Abstract
The skeletal architecture of the DRUJ provides minimal inherent stability, as the sigmoid notch is shallow and its radius of curvature is 50% greater than that of the ulnar head [Af Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg 1985;19(1):17–25]. Due to its incongruent articulation, the DRUJ relies strongly on the surrounding soft tissues for stability. The triangular fibrocartilage complex (TFCC) is generally accepted as the major soft tissue stabilizer of the DRUJ of which the volar and dorsal radioulnar ligaments are the primary components. Restoration of the radioulnar ligaments offers the best possibility to restore the normal DRUJ primary constraints and kinematics. This article presents an update of the procedure developed by the senior author that anatomically reconstructs the palmar and dorsal radioulnar ligaments at their anatomic origins and insertions.
Keywords: Distal radioulnar joint, Wrist instability, Ligament reconstruction, Distal radioulnar joint instability
DRUJ Biomechanics and Pathomechanics
In isolated posttraumatic DRUJ instability, the most common history is a traumatic event involving a fall on the outstretched hand or a forced rotation of the wrist such as recoil from a power drill, which is followed by ulnar-sided wrist swelling and pain aggravated by forearm and wrist motion. Pain-at-rest and swelling typically improve, but pain with use continues and may become associated with symptoms of mechanical instability including weakness and a joint clunk.
Reconstruction of the radioulnar ligaments offers the best possibility to restore the normal DRUJ primary constraints and kinematics. Although the precise roles of the radioulnar ligaments have been debated, the volar and dorsal ligaments act in concert with the rims of the sigmoid notch to constrain the joint, and both are necessary for normal stability in either direction [9, 13, 15]. Ligament tension peaks at the extremes of translation and rotation as the ulnar head simultaneously compresses against a rim of the notch creating an interactive, combined tether and buttress to dislocation. Despite one ligament possibly providing the dominant restraint under a specific condition, the other ligament provides a secondary restraint, and both must be injured to allow complete dislocation [9, 15]. In patients with bidirectional or severe unidirectional instability, both ligaments are likely injured. Therefore, reconstructing both ligaments would provide optimum restoration of normal DRUJ kinematics.
Historical Perspective
The first surgical option is repair of the triangular fibrocartilage complex (TFCC) to the fovea of the ulnar head [6, 12], which is the typical site of rupture [2]. If the TFCC is irreparable because of tissue damage, a reconstructive procedure is indicated. Numerous techniques have been described, which can be classified into three categories: (1) a direct radioulnar tether that is extrinsic to the joint [5], (2) an indirect radioulnar link via an ulnocarpal sling or a tenodesis [4, 7, 14], or (3) reconstruction of the radioulnar ligaments [1, 8, 11]. Although the techniques in the first two categories may improve symptoms, they have significant biomechanical deficiencies [10]. A radioulnar tether at the level of the ulnar neck does not guide the forearm along its normal axis of rotation. In addition, a tethering technique risks reducing forearm rotation. An ulnocarpal sling or a tenodesis uses the carpus to link the radius to the ulna. Although these techniques may restore ulnocarpal stability, the indirect radioulnar connection is inherently slack and thus suboptimal for restoring DRUJ stability.
Indications/Contraindications
The primary indication for DRUJ ligament reconstruction is DRUJ instability with an irreparable TFCC. DRUJ instability may coexist with other causes of ulnar-sided wrist pain, including ECU tendon subluxation, ulnar impaction syndrome, and DRUJ arthritis. These conditions, among others, must be considered before instability is attributed as the main cause of symptoms. If instability occurs, secondary to a previous malunion, ligament reconstruction may be performed in conjunction with a corrective osteotomy of the radius or ulna. In fact, any substantial skeletal malalignment must be corrected for a ligament reconstruction to restore stability.
If a previous distal radius fracture created deficiency of the sigmoid notch, or if the notch is developmentally flat, a notch osteoplasty is required as an adjunct to DRUJ reconstruction. If there is a question of damage or developmental flatness of the notch, a computed tomography (CT) scan should be obtained to determine the adequacy of the dorsal and volar rims. Ligament reconstruction is contraindicated in the presence of DRUJ arthritis. Although it could be performed in conjunction with a hemiresection of the distal ulna for an unstable and arthritic DRUJ, other procedures such as a tenodesis would likely be as effective and accomplished more efficiently in this situation.
Surgical Technique
A 5-cm dorsal incision is made between the fifth and sixth extensor compartments over the DRUJ.
The fifth compartment is opened over the distal radioulnar joint and the extensor digiti minimi tendon is retracted.
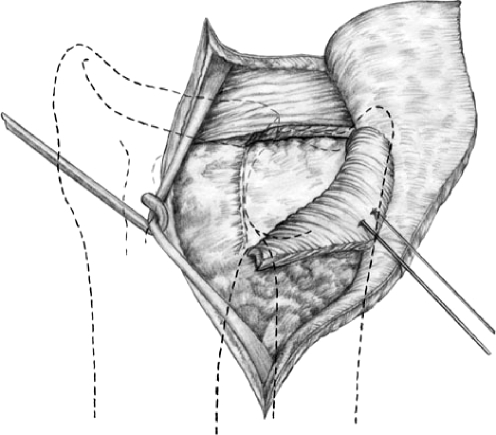
An L-shaped flap is created in the DRUJ capsule. One limb of the flap is longitudinal along the dorsal rim of the sigmoid notch. The other limb is transverse and located just proximal and parallel to the dorsal radioulnar ligament of the TFCC. This flap is then elevated proximally to expose the articular surface of the DRUJ and the proximal TFCC. Care is taken to preserve the uninjured portions of the TFCC; however, a tear in the disk can be debrided. (Fig. 1)
The integrity of the TFCC and its potential for repair is determined. If the TFCC is not reparable, then proceed to the reconstruction. Debride the granulation tissue from the fovea of the ulnar head but do not injure the ECU sheath or any remnant of the TFCC that reflects over the ulnar styloid.
The periosteum beneath the fourth dorsal extensor compartment is elevated from the dorsal margin of the sigmoid notch.
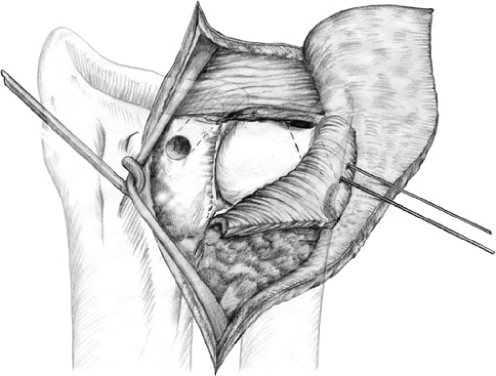
A guide wire for a 3.5 mm cannulated drill bit is driven through the radius several millimeters proximal to the lunate fossa and approximately 5 mm radial to the articular surface of the sigmoid notch. This site is chosen so that the tunnel can be enlarged if necessary to accommodate the graft without disrupting the subchondral bone of the lunate fossa or sigmoid notch. (Fig. 2)
After fluoroscopic views confirm proper guide wire position, the tunnel is made with a 3.5-mm cannulated drill. (Figs. 3 and 4)
A 4.5-mm drill hole is made in the ulnar neck at its subcutaneous border. A guide wire for a cannulated 3.5-mm drill bit is inserted in the hole and driven obliquely through the head to exit the fovea. Alternatively, the wrist is flexed and the guide wire may be driven through the fovea and out the ulnar neck without making the 4.5-mm hole first. (Fig. 5)
After fluoroscopic views confirm proper guide wire position, the tunnel is made with a 3.5-mm cannulated drill. Depending on graft size, the tunnel may need to be enlarged.
A palmaris longus or plantaris tendon graft is harvested. Alternatively, a strip of the flexor carpi ulnaris or a long toe extensor tendon can be used.
The volar opening of the radius tunnel is exposed through a 3- to 4-cm longitudinal incision extending proximally from the proximal wrist crease between the ulnar neurovascular bundle and finger flexor tendons.
A suture retriever is passed through the radius tunnel from dorsal to volar, and one end of the graft is pulled back through the tunnel.
A straight hemostat is passed over the ulnar head but proximal to the remaining TFCC and pushed through the volar DRUJ capsule. The other end of the graft is grasped with the hemostat and pulled back along this tract.
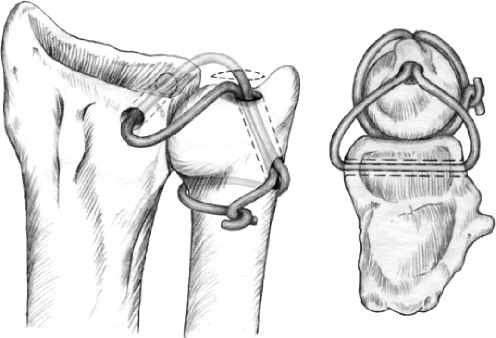
Both graft limbs are then passed through the ulnar tunnel to exit the ulnar neck. The limbs are passed in opposite directions around the ulnar neck, one passing deep to the ECU sheath. (Fig. 6)
With the forearm in neutral rotation and the DRUJ manually compressed, the limbs are pulled taut, tied together against the dorsum of the ulnar neck, and secured with sutures.
The dorsal DRUJ capsule and extensor retinaculum are closed in a single combined layer leaving the extensor digiti quinti (EDQ) subcutaneous.
Immobilize the extremity in a long-arm plaster splint with the forearm in neutral to slight supination or pronation depending on the most stable position.
Figure 1.
Techniques in hand and upper extremity. Dorsal exposure of the DRUJ for ligament reconstruction is obtained by incising the fifth compartment and raising a triangular capsular flap.
Figure 2.
Techniques in hand and upper extremity. Dorsal exposure of the DRUJ demonstrating capsular exposure and bone tunnels.
Figure 3.
Techniques in hand and upper extremity. Lateral x-ray demonstrating guide wire in distal radius. Note relationship of guide wire to the articular surface.
Figure 4.
Techniques in hand and upper extremity. PA radiograph of the distal radius demonstrating bone tunnel.
Figure 5.
Techniques in hand and upper extremity. PA radiograph demonstrating bone tunnels for graft with guide wire in ulnar tunnel.
Figure 6.
Techniques in hand and upper extremity. Tendon graft reconstruction through bone tunnels.
Rehabilitation
At 10 days postoperative, the sutures are removed and the patient’s cast is converted to a long arm cast extending to just above the elbow to control forearm rotation. At 3 weeks, the cast is changed to a short arm well-molded cast that partially limits forearm rotation for an additional 2 to 3 weeks.
The cast is then converted to a removable commercial or custom wrist brace to be used for at least 2 months, as motion and strength are recovered. Therapy begins with active and gentle passive wrist flexion, extension, pronation, and supination. No limitations are placed on active motion, but only gentle passive motion should be used during the first month of therapy. Strengthening is started at 3 months postoperative, but high forces with the arm in full pronation or supination are avoided. At 4 months postoperative, more aggressive passive ROM and strengthening are added with the goal to recover 85% of “normal” forearm rotation by 6 months. No unprotected use of the hand for sports or lifting greater than 10 lbs is allowed until at least 4 months postoperation.
Complications
Potential complications following reconstruction for DRUJ instability are persistent joint pain, recurrent instability, stiffness, and weakness. Pain and weakness may be related to previous surgery or caused by unrecognized DRUJ arthritis. Ulnocarpal impingement may also be a cause of persistent pain. A history of repeat trauma suggests possible disruption of the repair.
References
- 1.Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg [Am] 2002;27(2):243–51. [DOI] [PubMed]
- 2.Adams BD, Samani JE, Holley KA. Triangular fibrocartilage injury: a laboratory model. J Hand Surg [Am] 1996;21(2):189–93. [DOI] [PubMed]
- 3.Af Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg 1985;19(1):17–25. [DOI] [PubMed]
- 4.Breen TF, Jupiter J. Tenodesis of the chronically unstable distal ulna. Hand Clin 1991;7(2):355–63. [PubMed]
- 5.Fulkerson JP, Watson HK. Congenital anterior subluxation of the distal ulna. A case report. Clin Orthop 1978;131:179–82. [PubMed]
- 6.Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg [Am] 1991;16(2):340–6. [DOI] [PubMed]
- 7.Hui FC, Linscheid RL. Ulnotriquetral augmentation tenodesis: a reconstructive procedure for dorsal subluxation of the distal radioulnar joint. J Hand Surg [Am] 1982;7(3):230–6. [DOI] [PubMed]
- 8.Johnson Jones K, Sanders WE. Posttraumatic radioulnar instability: treatment by anatomic reconstruction of the volar and dorsal radioulnar ligaments. Orthop Trans 1995–1996;19:832.
- 9.Kihara H, Short WH, Werner FW, Fortino MD, Palmer AK. The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg [Am] 1995;20(6):930–6. [DOI] [PubMed]
- 10.Petersen MS, Adams BD. Biomechanical evaluation of distal radioulnar reconstructions. J Hand Surg [Am] 1993;18(2):328–34. [DOI] [PubMed]
- 11.Scheker LR, Belliappa PP, Acosta R, German OS, et al. Reconstruction of the dorsal ligament of the triangular fibrocartilage complex. J Hand Surg [Br] 1994;19(3):310–8. [DOI] [PubMed]
- 12.Sennwald GR, Lauterburg M, Zdravkovic V. A new technique of reattachment after traumatic avulsion of the TFCC at its ulnar insertion. J Hand Surg [Br] 1995;20(2):178–84. [DOI] [PubMed]
- 13.Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg [Am] 2000;25(4):689–99. [DOI] [PubMed]
- 14.Tsai TM, Stilwell JH. Repair of chronic subluxation of the distal radioulnar joint (ulnar dorsal) using flexor carpi ulnaris tendon. J Hand Surg [Br] 1984;9(3):289–94. [DOI] [PubMed]
- 15.Ward LD, Ambrose CG, Masson MV, Levaro F. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg [Am] 2000;25(2):341–51. [DOI] [PubMed]