Abstract
Introduction
The ideal treatment for a boxer’s fracture remains controversial, particularly the degree of volar dislocation considered acceptable for nonoperative treatment.
Patients and Methods
From December 2003 to December 2004, 25 patients who sustained a subcapital metacarpal fracture of the little finger with volar angulation between 30 to 75° were prospectively enrolled in the study. All patients were treated with a circular self-adherent wrap covering metacarpal bones II–V and buddy taping of the ring and little fingers for a period of 3 weeks while allowing immediate free range of motion.
Results
Final evaluation at a mean of 5 months revealed all patients to be satisfied without subjective functional impairment. All fractures healed, and the angulation of the fracture remained unchanged, but moderate shortening was observed. Active flexion of the metacarpophalangeal (MCP) joint was significantly lower on the fracture side, but as the median degree of MCP flexion was the same, this statistical difference was without clinical relevance. There was no loss in grip strength. A subjective long-term evaluation was performed by phone; at a median of 3 years, a QuickDash score gave a median of 0 point.
Conclusion
Treating a boxer’s fracture with angulation of up to 75° by soft wrap and buddy taping resulted in satisfied patients and good clinical results.
Keywords: Boxer’s fracture, Metacarpal fracture, Fifth metacarpal, Wrap, Buddy taping, Conservative treatment
Introduction
Subcapital fractures of the fifth metacarpal account for approximately 20% of all hand fractures [18]. These fractures are usually sustained by an axial blow on the metacarpophalangeal (MCP) joint in a flexed position, hence, the name boxer’s fracture. The degree of acceptable volar angulation varies from 20 to 70° [6, 9, 11, 15, 20, 22, 27, 30, 31, 34], and the ideal treatment for this fracture is still a matter of debate. Treatment options include operative procedures, splinting with or without closed reduction, and functional taping. Overall results are generally satisfactory. Follow-up is often difficult because of poor compliance [7, 22], and therefore, a simple, low-cost, and limited labor-intensive treatment would be ideal. At the University Hospital of Geneva, we commonly treat a boxer’s fracture with a self-adherent wrap covering metacarpal bones II–V and buddy taping of the ring and little fingers for a period of 3 weeks while allowing immediate free range of motion (ROM). This treatment is designed to limit patient activity and permit early motion of the little finger. The aim of our study is to prospectively evaluate the subjective and objective outcome of this treatment.
Patients and Methods
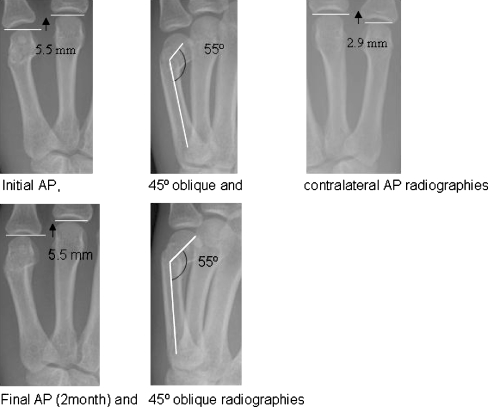
Between December 2003 and December 2004, all patients with subcapital fractures of the fifth metacarpal were evaluated in the outpatient clinic of the University Hospital of Geneva for possible inclusion in the study. Inclusion criteria were all subcapital, extra-articular, closed, and isolated fractures of the fifth digit with no rotational deformity. Radiographs of the fracture, and as well, the opposite hand, were taken on initial presentation in standard antero-posterior (AP) and 45° oblique views. Angulation was measured by using the angle between a line through the neck and center of the head, and a line through the axis of the shaft on the 45° oblique X-ray. Shortening was measured by the distance between lines tangential to the fourth and fifth metacarpal heads compared to the contralateral hand (Fig. 2).
Figure 2.
The figure shows initial, contralateral, and final (2-month) radiographies. Shortening was measured by the distance between tangential lines to the fourth and fifth metacarpal heads compared to the contralateral hand; in this case, 5.5–2.9 mm = 2.6 mm for initial and final shortening. Angulation was measured on 45° oblique radiographies; in this case, 55° on initial and final evaluation.
All patients were treated with a circular self-adherent wrap (Coban™) covering metacarpal bones II–V. The wrist and volar aspect of the MCP joints remained free of the wrap. The little finger was taped to the ring finger using Velcro™ straps (Fig. 1). Patients were encouraged to move the wrist and the fingers immediately and were instructed to remove the bandage and strap themselves after 3 weeks.
Figure 1.
Fracture treatment with self-adherent wrap and strapping of the fourth and fifth fingers.
Follow-up examinations were at 1, 4, and 12 weeks after the fracture. Final examination was performed up to 12 months after the initial trauma. ROM of the fifth MCP joint was assessed with a finger goniometer. Grip strength was measured with a Jamar™ model PC 5030JIA hand dynamometer. The mid-position was used as it reflects global strength. Maximum strength was then determined by the mean value of three successive attempts. Malrotation was assessed clinically. Subjective evaluation consisted of recording pain (visual analogue scale), limitation of daily activities, and overall satisfaction. The use of analgesics and return to work was also documented. The results were analyzed using Medcalc® (http://www.medcalc.be). Long-term evaluation by telephone was performed using the QuickDash score [3].
Results
Of 29 patients included in the study, 4 were lost to follow-up, thus, leaving 25 patients (24 male, 1 female) for final evaluation. The median age was 25 years (range, 17–61 years). Ten patients sustained a fracture of the non-dominant hand. Thirteen patients were manual workers, 9 were non-manual workers, and 3 unemployed at the time of the accident. Fifteen patients fractured their fifth metacarpal while fighting and the remainder during a fall on the hand. All patients gave a history of normal function and full motion before the fracture.
The median initial angulation noted on the 45° oblique radiograph was 50° (range, 30–75°). Median initial shortening on the AP radiograph was 2 mm (range, 0–5 mm; Table 2). Three metacarpal fractures were comminuted. The median time of final clinical and radiological evaluation was 5 months (range, 3–12 months). All patients were pain-free with no restriction of daily activities. Thirteen patients were very satisfied, and 12 were satisfied; no patient was unsatisfied. The mean time out from work was 30 days (range, 4–55 days). The final clinical evaluation is shown in Table 1. No soft-tissue complications were observed. Half of the patients did not regularly come for follow-up evaluation.
Table 2.
Angulation and shortening of the fifth metacarpal fractures at the beginning and at the end of treatment.
| Beginning of treatment | End of treatment | P value (test applied) | |
|---|---|---|---|
| Median (range) angulation in 45° oblique radiographies | 50° (30–75°) | 50° (35–75°) | NS |
| Median (range) shortening in AP radiographies | 2 mm (0–5 mm) | 2 mm (0–6 mm) | P = 0.023 (Wilcoxon) |
Table 1.
Clinical results concerning ROM and grip force at the end of the treatment comparing the fractured and the contralateral sides.
| Fractured side | Contralateral side | P value (test applied) | |
|---|---|---|---|
| Median (range) active extension | 0° (−10–+5°) | 0° (−10–0°) | NS (paired t test) |
| Median (range) active flexion | 90° (70–95°) | 90° (85–100°) | P = 0.001 (Wilcoxon) |
| Median (range) grip force | 40 kg (23–60 kg) | 42.5 kg (22–60 kg) | NS (Wilcoxon) |
Median final flexion of the fifth MCP joint was 90° (range, 70–95°), significantly lower (P = 0.001) compared to the contralateral side (median 90°; range, 85–100°). No difference (P = 0.18) was noted in the final extension of the fifth MCP joint (median 0°; range, −10–+5°) compared to the contralateral side (median, 0°; range, −10–0°).
The median final grip force on the affected side was 40 kg (range, 23–60 kg) and on the contralateral side, 42.5 kg (range, 22–60 kg). This difference was not significant. All fractures were healed at final evaluation, but because of poor patient compliance, it was impossible to determine the exact time of union. Radiological results are summarized in Table 2.
Median final angulation of the fifth metacarpal shaft was 50° (range, 35–75°) with a median final shortening of 2 mm (range, 0–6 mm). Final angulation of the fifth metacarpal did not significantly differ from the initial measurement. However, final shortening was significantly different in comparison to initial measurements (P = 0.023). Figure 2 shows an example of angulation and shortening at initial and final evaluation. The three comminuted fractures did not show greater collapse than the simple fractures.
Twenty-two patients (88%) could be reached by phone for a long-term evaluation after a median of 3 years (range, 2.4–3.4 years). A QuickDash was performed, which revealed a median score of 0 point (range, 0–36 points). No patient complained of any volar soreness.
A cost analysis comparing the conservative and operative treatment regime according to the Swiss tax point system (TARMED [33]) is given in Table 3.
Table 3.
Costs of different treatment regimes, following the Swiss tax point system [33].
| Conservative treatment with elastic wrap | Operative treatment with K-wires |
|---|---|
| First evaluation with X-rays, 113.66 TARMED points | First evaluation with X-rays, 113.66 TARMED points |
| Anesthesia, surgery, and cast, 647.89 TARMED points | |
| Two-week evaluation with X-rays, 113.66 TARMED points | Two-week evaluation with X-rays, 113.66 TARMED points |
| Six-week evaluation with X-rays, 113.66 TARMED points | Six-week evaluation with X-rays, 113.66 TARMED points |
| Evaluation, anesthesia, hardware removal, and surgery, 467.22 TARMED points | |
| Two-week evaluation after hardware removal, 113.66 TARMED points | |
| 340.98 TARMED points | 1,447.19 TARMED points |
Discussion
The ideal treatment for a boxer’s fracture, surgical or nonoperative, remains controversial. It is also unclear as to what amount of volar angulation and axial shortening is acceptable [6, 9, 11, 15, 20, 22, 27, 30, 31, 34]. In the present study, we obtained subjectively good results with no pain and objectively good mobility and strength, at a mean of 5 months after the fracture. A long-term evaluation after 3 years gave a median QuickDash score of 0 point; we counted two re-fractures that were treated once more by wrap and buddy taping. In addition, the short amount of time lost from work (mean of 3 weeks) supports the use of a functional treatment for these fractures, as has been noted in previous reports [6, 7, 20, 22, 30, 31].
An anatomical study [32] demonstrated that, for every 2 mm of metacarpal shortening, there was a corresponding 7° extension deficit. However, its clinical relevance is uncertain, and Lumplesch [24] reported no extension deficit for shortening up to 6 mm. This is similar in our patients where shortening of up to 5 mm did not result in extension deficits. A biomechanical study [1] with cadaver hands concluded that 30° of angulation is the acceptable upper limit; otherwise, the ROM of the MCP joint of the little finger could diminish and weaken the finger’s initiation of grip. Several clinical studies [23, 26, 31] do not support these findings. We found that, even at 75°of angulation, the grip strength does not differ between the fracture and contralateral side. A more specific evaluation of the isolated grip strength of the fifth digit is of academic interest and does not affect the final subjective result. A loss of intrinsic strength, theoretically possible because of the shortening of the fifth metacarpal, cannot be excluded because it was not part of our examination protocol.
Active flexion of the MCP joint was significantly lower on the fracture side, but as the median degree of MCP flexion was the same, this statistical difference was without clinical relevance.
Reduction of MCP motion can be compensated for by greater mobility in the adjacent carpometacarpal (CMC) and interphalangeal (IP) joints [12, 18]. Whether this compensation will lead to early degenerative changes in the carpometacarpal joint needs to be further assessed in a long-term follow-up. In any event, arthritis involving the small finger CMC or IP joints because of malunion of a subcapital fracture has not been reported and might not occur because of the relatively unconstrained nature of this joint [21]. On the other hand, limitation of motion, reduction in grip ability, or pain after digito-palmar grasping movements has been previously stated [8, 28] and seems to be related to initial immobilization [8, 28].
Early arthritic changes in the MCP joint secondary to a malunited subcapital fracture cannot be excluded, but even so, there have been no osteoarthritic changes reported with late osteotomies for metacarpal malunions [8].
The median angulation of the fifth metacarpal did not differ significantly between the initial and the final evaluation. By contrast, the median shortening did differ significantly, but as the median remained the same, the difference is without relevance. This observation suggests that these fractures were stable. Closed reduction might displace a stable fracture, and in other studies, all fractures that had been reduced lost reduction irrespective of the type of immobilization [5, 14, 19, 20, 22, 23]. Consequently, reduction of a subcapital fracture of the fifth metacarpal is not necessary, and early mobilization is not harmful. Interestingly, in an animal model, early controlled passive motion for metacarpal fractures in a rabbit led to significant improvement in the ability of early callus to resist and bear loads [10].
Twenty-four patients (96%) were asymptomatic at final evaluation. Because patients with a boxer’s fracture are frequently known to be noncompliant [4, 7, 22, 34], it is doubtful that they closely followed the treatment protocol, although all patients presented with the wrap and buddy taping. One might argue that no treatment could be a treatment option as well. Our patients lost a mean time from work of 30 days, which is not different from that in similar studies [16, 31]. Whether functional treatment as compared to bracing leads to a shorter time lost from work is still under debate [16, 20, 27, 35]. The initial pain relief with the use of braces as compared to functional taping [15, 31] did not influence the length of time off from work. However, because of the compliance issue, we prefer to avoid bracing because of the risk of skin necrosis over the metacarpal [7, 13, 17, 29] and as well the need to control the brace on a regular basis. The patients themselves prefer buddy taping to casting and no follow-up evaluations [2].
As both fracture angulation and shortening can impair force and mobility, the same fracture angulation in combination with different amounts of shortening may lead to different clinical results. Thus, angulation and shortening should not be viewed independently, but rather as two components in a mathematical model helpful in decision making. However, more data is required to investigate this hypothesis. Besides medical importance, such a model is of economical interest, as the direct costs of operative treatment (e.g., intramedullary wiring inclusive of removal of hardware [9]) are about four times greater than treatment by soft wrap and buddy tapping (Table 3) [33]. Complications after intramedullary Kirschner wiring in noncompliant patients, such as wound infection, articular stiffness, tendon adhesion and non-union can even further raise the costs. As with indirect costs, it is vital to mention that time lost from work after operative procedures are generally twice [9, 25] as long as in our patients. When we take into account our good results from nonoperative treatment and the possible complications of surgery and their cost, we believe that surgery should be proposed only in selective cases.
Conclusion
As noncompliance is high among patients with subcapital fractures of the fifth metacarpal (boxer’s fracture), a simple and efficient treatment is required. We employed a self-adherent wrap combined with buddy taping of the ring and little fingers for a period of 3 weeks, allowing immediate motion. In patients with nondisplaced fractures that were not rotated or angulated greater than 75°, we obtained pain-free and satisfied patients with symmetrical grip strength and functional ROM of the fifth MCP joint. According to the Swiss tax point system [33], treatment by wrap and buddy taping is approximately four times less expensive than operative treatment.
References
- 1.Ali A, Hamman J, Mass DP. The biomechanical effects of angulated boxer’sfractures. J Hand Surg (Am) 1999;24:835–44. [DOI] [PubMed]
- 2.Bansal R, Craigen MA. Fifth metacarpal neck fractures: is follow-up required? J Hand Surg [Br] 2007;32:69–73. [DOI] [PubMed]
- 3.Beaton DE, Wright JG, Katz JN. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am 2005;87:1038–46. [DOI] [PubMed]
- 4.Borgeskov S. Conservative treatment of phalangeal and metacarpal fractures. Ugeskr Laeger 1967;129:349–53. [PubMed]
- 5.Braakman M. Is anatomical reduction of fractures of the fourth and fifth metacarpals useful? Acta Orthop Belg 1997;63:106–9. [PubMed]
- 6.Braakman M, Oderwald EE, Haentjens MH. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury 1998;29:5–9. [DOI] [PubMed]
- 7.Breddam M, Hansen TB. Subcapital fractures of the fourth and fifth metacarpals treated without splinting and reposition. Scand J Plast Reconstr Surg Hand Surg 1995;29:269–70. [DOI] [PubMed]
- 8.Ceroni D, Della Santa D. Extension osteotomy of the long metacarpal bones. A therapeutic solution to repairing flexion defects. Apropos of 14 cases. Chir Main 2000;19:100–8. [DOI] [PubMed]
- 9.Della Santa D, Chamay A, Blanco F, Marti MC. Fractures of the long metacarpals. Long-term results. Ann Chir Main 1985;4:175–80. [DOI] [PubMed]
- 10.Feehan LM, Tang CS, Oxland TR. Early controlled passive motion improves early fracture alignment and structural properties in a closed extra-articular metacarpal fracture in a rabbit model. J Hand Surg [Am] 2007;32:200–8. [DOI] [PubMed]
- 11.Ford DJ, Ali MS, Steel WM. Fractures of the fifth metacarpal neck: is reduction or immobilisation necessary? J Hand Surg [Br] 1989;14:165–7. [DOI] [PubMed]
- 12.Freeland AE, Geissler WB, Weiss AP. Surgical treatment of common displaced and unstable fractures of the hand. Instr Course Lect 2002;51:185–201. [PubMed]
- 13.Geiger KR, Karpman RR. Necrosis of the skin over the metacarpal as a result of functional fracture-bracing. A report of three cases. J Bone Joint Surg Am 1989;71:1199–202. [PubMed]
- 14.Gonzalez MH, Igram CM, Hall RF Jr. Flexible intramedullary nailing for metacarpal fractures. J Hand Surg [Am] 1995;20:382–7. [DOI] [PubMed]
- 15.Hansen PB, Hansen TB. The treatment of fractures of the ring and little metacarpal necks. A prospective randomized study of three different types of treatment. J Hand Surg [Br] 1998;23:245–7. [DOI] [PubMed]
- 16.Harding IJ, Parry D, Barrington RL. The use of a moulded metacarpal brace versus neighbour strapping for fractures of the little finger metacarpal neck. J Hand Surg [Br] 2001;26:261–3. [DOI] [PubMed]
- 17.Harvie KW. Necrosis of the skin over the metacarpal as a result of functional fracture-bracing. J Bone Joint Surg Am 1990;72:1114–5. [PubMed]
- 18.Hunter JM, Cowen NJ. Fifth metacarpal fractures in a compensation clinic population. A report on one hundred and thirty-three cases. J Bone Joint Surg Am 1970;52:1159–65. [PubMed]
- 19.Jabaley ME, Freeland AE. Rigid internal fixation in the hand: 104 cases. Plast Reconstr Surg 1986;77:288–98. [DOI] [PubMed]
- 20.Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures 100 randomized cases with or without fixation. Acta Orthop Scand 1990;61:531–4. [DOI] [PubMed]
- 21.Kraus VB, Li YJ, Martin ER, Jordan JM, Renner JB, Doherty M, et al. Articular hypermobility is a protective factor for hand osteoarthritis. Arthritis Rheum 2004;50:2178–83. [DOI] [PubMed]
- 22.Kuokkanen HO, Mulari-Keranen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Reconstr Surg Hand Surg 1999;33:315–7. [DOI] [PubMed]
- 23.Lowdon IM. Fractures of the metacarpal neck of the little finger. Injury 1986;17:189–92. [DOI] [PubMed]
- 24.Lumplesch R, Zilch H, Friedebold G. Fractures of the metacarpal bones II to V-conservative and surgical treatment. Unfallchirurgie 1985;11:115–8. [DOI] [PubMed]
- 25.Manueddu CA, Della Santa D. Fasciculated intramedullary pinning of metacarpal fractures. J Hand Surg [Br] 1996;21:230–6. [DOI] [PubMed]
- 26.McKerrell J, Bowen V, Johnston G, Zondervan J. Boxer’s fractures—conservative or operative management? J Trauma 1987;27:486–90. [PubMed]
- 27.McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. A controlled comparison of compression glove and splintage. J Hand Surg [Br] 1994;19:597–600. [DOI] [PubMed]
- 28.Moutet F, Frere G. Metacarpal fractures. Ann Chir Main 1987;6:5–14. [DOI] [PubMed]
- 29.Nossaman BC, Rayan GM. Skin necrosis complicating functional bracing. Am J Orthop 1998;27:371–2. [PubMed]
- 30.Sorensen JS, Freund KG, Kejla G. Functional fracture bracing in metacarpal fractures: the Galveston metacarpal brace versus a plaster-of-Paris bandage in a prospective study. J Hand Ther 1993;6:263–5. [DOI] [PubMed]
- 31.Statius Muller MG, Poolman RW, van Hoogstraten MJ, Steller EP. Immediate mobilization gives good results in boxer’s fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Arch Orthop Trauma Surg 2003;123:534–7. [DOI] [PubMed]
- 32.Strauch RJ, Rosenwasser MP, Lunt JG. Metacarpal shaft fractures: the effect of shortening on the extensor tendon mechanism. J Hand Surg [Am] 1998;23:519–23. [DOI] [PubMed]
- 33.TARMED Suisse, volume 2006. Bern: TARMED Suisse; 2006.
- 34.Theeuwen GA, Lemmens JA, van Niekerk JL. Conservative treatment of boxer’s fracture: a retrospective analysis. Injury 1991;22:394–6. [DOI] [PubMed]
- 35.Viegas SF, Tencer A, Woodard P, Williams CR. Functional bracing of fractures of the second through fifth metacarpals. J Hand Surg [Am] 1987;12:139–43. [DOI] [PubMed]