Abstract
Background
The Medical Outcomes General Health Survey (SF-36) is a widely used health status measure; however, limited evidence is available for its performance in orthopedic settings. The aim of this study was to examine the magnitude and meaningfulness of change and sensitivity of SF-36 subscales following orthopedic surgery.
Methods
Longitudinal data on outcomes of total hip replacement (THR, n = 255), total knee replacement (TKR, n = 103), arthroscopic partial meniscectomy (APM, n = 74) and anterior cruciate ligament reconstruction (ACL, n = 62) were used to estimate the effect sizes (ES, magnitude of change) and minimal detectable change (sensitivity) at the group and individual level. To provide context for interpreting the magnitude of changes in SF-36 scores, we also compared patients' scores with age and sex-matched population norms. The studies were conducted in Sweden. Follow-up was five years in THR and TKR studies, two years in ACL, and three months in APM.
Results
On average, large effect sizes (ES≥0.80) were found after orthopedic surgery in SF-36 subscales measuring physical aspects (physical functioning, role physical, and bodily pain). Small (0.20–0.49) to moderate (0.50–0.79) effect sizes were found in subscales measuring mental and social aspects (role emotional, vitality, social functioning, and mental health). General health scores remained relatively unchanged during the follow-up. Despite improvements, post-surgery mean scores of patients were still below the age and sex matched population norms on physical subscales. Patients' scores on mental and social subscales approached population norms following the surgery. At the individual level, scores of a large proportion of patients were affected by floor or ceiling effects on several subscales and the sensitivity to individual change was very low.
Conclusion
Large to moderate meaningful changes in group scores were observed in all SF-36 subscales except General Health across the intervention groups. Therefore, in orthopedic settings, the SF-36 can be used to show changes for groups in physical, mental, and social dimensions and in comparison with population norms. However, SF-36 subscales have low sensitivity to individual change and so we caution against using SF-36 to monitor the health status of individual patients undergoing orthopedic surgery.
Background
The Medical Outcomes Study Short Form Health Survey (SF-36) is a health status questionnaire that was developed almost 20 years ago for the assessment of functional status and well-being [1]. Its 36 items assess eight health-related concepts thought to be affected by disease and treatment interventions: physical functioning, role limitations due to physical health problems (role physical), bodily pain, general health, energy levels/fatigue (vitality), social functioning, role limitations due to emotional problems (role emotional), and psychological distress (mental health). The SF-36 has been applied in a variety of clinical settings [2-6] including orthopedic surgery where it has been frequently used to evaluate psychometric and clinometric properties of other self-report questionnaires [7-9].
The popularity of the SF-36 is in part related to accumulating support for its satisfactory validity and reliability across study settings and populations [10-13]. Population norms for SF-36, by age and sex, are available for several countries, allowing comparisons of the health status of the patient groups with the general population [1,14-16]. To be of practical use in clinical and research settings, measures that are used to assess outcomes of an intervention must have been shown to be able to detect change in health status. Given that statistical significance of change is sample-dependent (in large studies minute and clinically unimportant changes may be statistically significant and fallaciously regarded as clinically significant), the magnitude of change (effect size) following an intervention is more informative to clinical practitioners. Information on effect size is also useful in research settings, where it can be used to calculate the sample size required to detect changes of a certain magnitude.
An additional measurement issue associated with comparing pre- and post-intervention scores is that change scores may be due to random measurement error, real change in health status, or both. Therefore, an important characteristic of a sound measure is the ability to detect meaningful change in participants' health state. The ability of a questionnaire to detect a meaningful change is known as sensitivity, with instruments that are more sensitive being able to detect smaller changes. Ideally, the measurement properties of a questionnaire should be tested in the settings in which it will be used. However, relatively few studies have specifically examined the magnitude and meaningfulness of changes in SF-36 scores following orthopedic surgery, and mixed results have been reported in those that have [9,17,18].
The aim of this study was to assess the utility of SF-36 subscales in orthopedics by examining the magnitude and meaningfulness of change and sensitivity of SF-36 scores in orthopedic surgery. To provide context for interpreting the magnitude of changes in SF-36 scores, we also compared patients' pre- and post-operative scores with the age and sex adjusted population norms.
Methods
To estimate magnitude of change and sensitivity of SF-36 subscales in orthopedic settings, we utilized secondary data from prospective follow-up studies of outcomes in total hip replacement (THR), total knee replacement (TKR), arthroscopic partial meniscectomy (APM), and anterior cruciate ligament (ACL) reconstruction surgery. The methods of these studies have been previously published and are summarized here only briefly.
Total hip replacement (THR) groups
This group included 274 consecutive patients having THR for hip osteoarthritis at the Department of Orthopedics at Halmstad Central Hospital, Sweden and 110 controls, matched to the patients by age, sex and municipality [19]. Controls were identified from the Swedish National Population Records. In all, 258 eligible controls were identified, with 45% (n = 116) agreeing to take part in the study. After exclusion of those who reported hip complaints (pain or diminished range of motion) (n = 6), the remaining number (110) was regarded as sufficient for group comparisons. Patients' mean age was 70.5 years and 53% were women. Mean age of controls was 70.7 years and 55% were women. Patients were assessed before the surgery (baseline) and reassessed at six months and five years after the surgery. Controls were assessed at the time of recruitment, with follow-up assessments also at six months and five years. Five-year follow-up rates were 65% for both groups (Table 1).
Table 1.
Follow-up rates for the study groups
| Group | Number of participants (% of baseline) | |||||
| Baseline | 3 months | 6 months | 1 year | 2 years | 5 years | |
| Total hip replacement (controls) |
110 | - | 74 (67%) | - | - | 71 (65%) |
| Total hip replacement (patients) |
274 | - | 222 (81%) | - | - | 179 (65%) |
| Total knee replacement | 105 | - | 94 (90%) | 87 (83%) | - | 80 (76%) |
| Arthroscopic partial meniscectomy | 74 | 63 (85%) | - | - | - | - |
| Anterior cruciate ligament reconstruction | 62 | - | 62 (100%) | 55 (89%) | 46 (74%) | - |
Total knee replacement (TKR) group
This group included data from 105 consecutive patients having TKR for knee osteoarthritis at the Department of Orthopedics at Lund University Hospital, Sweden. Their mean age was 71.3 years and 63% were women [20]. Patients were assessed before the surgery (baseline), with follow-ups at six months, one year, and five years. At final follow-up data were available from 76% of patients.
Arthroscopic partial meniscectomy (APM) group
This group included 74 consecutive patients from Department of Orthopedics at Lund University Hospital, Sweden who received arthroscopic partial meniscectomy as the only intervention. Their mean age was 44.8 years and 32% were women [21]. The assessments were conducted before the surgery (baseline) and three months after the surgery (85% follow-up rate).
Anterior cruciate ligament (ACL) reconstruction group
This group included data from 62 Swedish patients randomized to an ACL reconstruction within a trial of surgical versus non-surgical treatment of acute ACL tear (ISRCTN 84752559). Inclusion criteria were age between 18 and 35 years, having a moderate to high physical activity level and no more than four weeks since ACL rupture at time of reconstruction. Their mean age was 25.9 years and 19% were women [22]. Patients were assessed before surgery (baseline), with follow-ups at six months, one year, and two years (74% follow-up rate).
Ethical approval and informed consent
Research carried out for the studies reported here complies with the Helsinki Declaration. Each study was approved by the Ethics Committee of the Medical Faculty of Lund University, Lund, Sweden. Written informed consent was obtained from the participants for the publication of results. Copies of the written consent are available for review by the Editor-in-Chief of this journal.
Measures
All study groups were administered SF-36 at each assessment. The SF-36 is a self-report generic health status questionnaire comprised of eight subscales: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH) [23-25]. The scores range between 0 and 100, with higher scores representing better health.
Statistical analyses
The original data for each study were extracted for the analyses.
Effect sizes
Magnitude of change in SF-36 subscale scores was assessed using Cohen's d [26]. Cohen's d is a standardized measure of effect size (ES) and provides information on the amount of change in the measure relative to the variation within the measure. Cohen's d is computed as the difference between the baseline and follow-up scores divided by the standard deviation of baseline scores. Benchmarks to classify the importance of the change are available, with ES values of 0.20–0.49 considered small, values of 0.50–0.79 considered moderate, and values ≥ 0.80 considered large [26]. ES were calculated so that positive values represent improvement and negative values represent deterioration.
Given that questionnaire change scores cannot be reliably estimated for the participants with extreme scores, we also examined the presence of floor and ceiling effects at each assessment time. The subscales were deemed to have floor or ceiling effects if 15% of respondents or more reported the worst (0) or best (100) possible scores, respectively.
Sensitivity
Sensitivity of subscales was evaluated using Minimal Detectable Change (MDC), calculated at individual and group levels. While individual and group MDC are related concepts, they convey different information. Individual level MDC provide information on whether observed changes in the individual's health status are greater than chance variations [27] whereas group level MDC are useful for comparing meaningfulness of change across samples [28].
Differences in the scores on the same measure obtained on different occasions may be due to random error, real change in health status, or a combination of both [27]. Therefore, MDC used for this study was based on standard error of measurement (SEM). Since the smaller the measurement error, the smaller the changes can be de detected beyond random error, with lower values of SEM indicating more sensitive subscales. SEM was derived from within subjects analysis of variance [29] with time of assessment (i.e., baseline, follow-up) as the within subjects factor [30]. This study design partitions the within-person variations in SF-36 scores into between-assessment variance and the residual variance [30]. The former represents systematic differences between assessment times, such as intervention effects, while the latter represents residual variance due to random error and error from unknown systematic sources. SEM was calculated as a square root of this residual within person variance [30]. To determine with 95% confidence whether observed changes were larger than the random error, individual level MDC (MDCind) were calculated as 1.96*√2*SEM [29,31-33]. Group level MDC (MDCgrp) were based on standard errors of the sample means. Standard error of the mean is influenced by both the within-subjects variability and the sample size, therefore MDCgrp were calculated as (1.96*√ 2*SEM)/√n [32,34,35]. The differences in group scores between baseline and follow-ups were interpreted as 'real' change if they exceed values of MDC [28].
MDC reflects changes that are greater than measurement error (i.e., statistically significant change) and should not be equated with clinically important change (change that clinicians and patients regard as important). Since minimal clinically important changes (MCIC) for SF-36 subscales are not well studied in orthopedic settings, we utilized the published standards for minimal "clinically and socially relevant" change in group scores as a measure of MCIC at a group level [36]. The standards for clinically and socially relevant changes at a group level are based on Cohen's d, with minimal important change represented by a moderate effect size (0.50–0.79), which corresponds to at least 5-point change in scores on the 0–100 scale (5%) [36]. SF-36 subscales with MDCgrp less than five were considered to have acceptable sensitivity to change in group scores. To determine whether the observed changes in SF-36 scores were statistically and clinically meaningful, we also compared the average group changes with values of MDC group and MCIC, respectively.
Established standards for MCIC at an individual level are essential for interpretation of intra-individual change as they help to determine clinical meaningfulness of the observed change in individual scores. Estimates of individual level MCIC are also important for evaluating sensitivity of a measure since a scale can only be regarded as sufficiently sensitive to detect meaningful changes in individual health status if the values of MDCind do not exceed values of individual level MCIC [33,37]. However, generally accepted standards for individual level MCIC in orthopedic surgery currently do not exist. Since scale's sensitivity to change is affected by measurement error, we used values of 95% confidence intervals (CI; calculated as 1.96*SEM) around SF-36 scores from a normative population-based sample [36] to gauge measurement error in SF-36 scores in orthopedic settings. As the CI and MDC represent boundary for true score and boundary for change, respectively, change could not be regarded as 'real' if the amount of measurement error around the true score exceeded the amount of measurement error around the change score. Therefore, SF-36 subscales were regarded as sufficiently sensitive to detect real changes in individual scores if MDCind were smaller than the normative values of 95% CI: 12 points for PF, 23 points for RP, 15 points for BP, 18 points for GH, 16 points for VT, 26 points for SF, 28 points for RE, and 24 points for MH subscales [36]. It is important to note however that CI values were used as an external standard for the expected amount of measurement error in SF-36 scores and not as a substitute for individual level MCIC.
Proportion improved or deteriorated
MDCind was used to categorize change in participants' scores. Those who had scores that decreased by an amount greater than the MDCind were classified as 'worse'; those whose scores increased by an amount greater than the values of MDCind were classified as 'better', and those with change scores less than or equal to MDCind were classified as 'no change'.
Population norm comparisons
To provide context for interpreting changes in health status following orthopedic surgery, patients' SF-36 scores were compared with the published norms for SF-36 for the Swedish population of the same age and sex [1,15]. As the standard errors for the published norm scores were very small, the mean values of the normative scores were used to represent the 'real' values for the population of each age and sex group. Average group scores within +/- 5 points of the population norm were considered to be within the norm [1,36].
All statistical analyses were performed using SPSS Version 15. Longitudinal changes were calculated using data from participants with complete follow-up only.
Results
SF-36 baseline data were available for 515 patients who underwent orthopedic surgery, including 274 THR, 105 TKR, 74 APM, and 62 ACL reconstruction patients. In the THR study, there were also 110 age and sex matched controls. Follow-up rates for the patients varied between 81% (APM) and 100% (ACL) at first post-surgical assessment (three months in APM study and six months in THR, TKR, and ACL studies) and between 65% (THR) and 76% (TKR) at final follow-up (two years for the ACL and five years for THR and TKR studies), see Table 1. Demographic characteristics are in Table 2. The proportion of men varied from 37% in TKR study to 81% in ACL study. On average, patients in the ACL study were youngest (mean [sd] 25.9 [5.1] at baseline), while patients in TKR study were the oldest (71.3 [8.1] years at baseline).
Table 2.
Age and sex characteristics of the study groups at baseline
| Group | % male | Age | |
| M (SD) | Range | ||
| Total hip replacement (controls) | 44.6 | 70.7 (7.6) | 52–86 |
| Total hip replacement (patients) | 47.2 | 70.5 (8.9) | 41–96 |
| Total knee replacement | 37.1 | 71.3 (8.1) | 43–86 |
| Arthroscopic partial meniscectomy | 67.6 | 44.8 (12.2) | 14–75 |
| Anterior cruciate ligament reconstruction | 80.6 | 25.9 (5.1) | 18–35 |
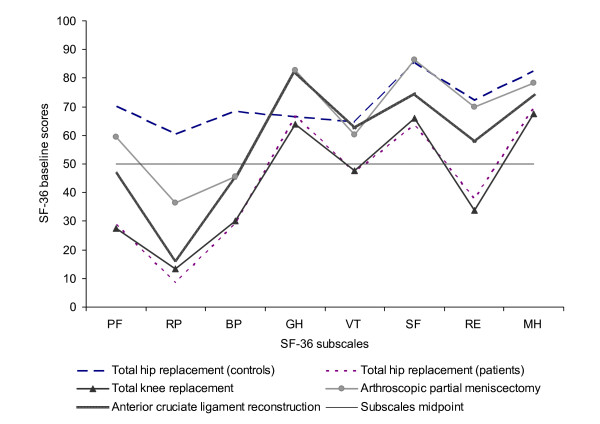
Baseline Scores
Average baseline scores are presented in Figure 1. The overall pattern of SF-36 subscale scores was similar across groups, with lowest scores recorded on RP subscale in all groups. The scores on GH, SF, and MH subscales tended to be similar within the groups and were generally better than the scores on other subscales. The greatest difference between the best and the worst subscale scores was observed for the ACL patients (GH versus RP subscales). THR and TKR patients had the worst baseline scores across all SF-36 subscales, and were well below the mid point (50 points) scores on PF, RP, BP, and SF subscales.
Figure 1.
Baseline SF-36 scores of the study groups. Note: PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
Changes in SF-36 Scores
Average SF-36 scores of the study groups at baseline and at first and final follow-ups are presented in Table 3. While the THR control group did not change or deteriorated slightly, the intervention groups generally improved in their SF-36 scores during the follow-up. One exception was the GH subscale, with small deteriorations relative to baseline scores recorded for THR and TKR groups at five years and for the APM group at three months follow-up.
Table 3.
Average SF-36 subscale scores and effect sizes for the study groups at first and final follow-up*
| SF-36 scores | Total hip replacement (controls) |
Total hip replacement (patients) |
Total knee replacement |
Arthroscopic partial meniscectomy |
Anterior cruciate ligament reconstruction |
|||||||||||
| N | M (SD) | ES | N | M (SD) | ES | N | M (SD) | ES | N | M (SD) | ES | N | M (SD) | ES | ||
| PF | Baseline | 44 | 79.6 (17.7) | 147 | 30.7 (20.1) | 68 | 30.0 (14.9) | 62 | 59.0 (21.8) | 46 | 44.2 (21.8) | |||||
| First follow-up | 44 | 78.2 (21.8) | -0.1 | 147 | 60.5 (22.0) | 1.5 | 68 | 60.6 (21.1) | 2.1 | 62 | 73.7 (21.9) | 0.7 | 46 | 79.6 (17.7) | 1.6 | |
| Final follow-up | 44 | 74.5 (24.1) | -0.3 | 147 | 57.6 (27.3) | 1.3 | 68 | 52.3 (24.1) | 1.5 | 46 | 83.4 (20.2) | 1.8 | ||||
| RP | Baseline | 42 | 68.5 (41.0) | 139 | 8.5 (20.2) | 64 | 12.6 (23.7) | 62 | 36.7 (38.3) | 46 | 14.1 (26.7) | |||||
| First follow-up | 42 | 69.6 (42.6) | 0.0 | 139 | 49 (42.6) | 2.0 | 64 | 42.7 (42.4) | 1.3 | 62 | 62.5 (42.2) | 0.7 | 46 | 64.7 (40.0) | 1.9 | |
| Final follow-up | 42 | 60.1 (42.4) | -0.2 | 139 | 49.6 (43.2) | 2.0 | 64 | 48.0 (43.9) | 1.5 | 46 | 80.4 (34.9) | 2.5 | ||||
| BP | Baseline | 50 | 75.7 (24.2) | 154 | 30.9 (17.2) | 66 | 30.6 (18.8) | 62 | 44.4 (19.2) | 46 | 41.8 (20.4) | |||||
| First follow-up | 50 | 73.0 (27.6) | -0.1 | 154 | 70.3 (23.6) | 2.3 | 66 | 70.9 (23.7) | 2.1 | 62 | 63.3 (24.9) | 1.0 | 46 | 74.4 (20.7) | 1.6 | |
| Final follow-up | 50 | 70.2 (28.0) | -0.2 | 154 | 67.1 (26.0) | 2.1 | 66 | 63.9 (25.1) | 1.8 | 46 | 75.8 (25.3) | 1.7 | ||||
| GH | Baseline | 46 | 70.2 (20.3) | 139 | 68.8 (19.1) | 59 | 66.0 (18.3) | 61 | 82.4 (15.1) | 46 | 81.5 (15.8) | |||||
| First follow-up | 46 | 68.6 (22.0) | -0.1 | 139 | 72.5 (20.7) | 0.2 | 59 | 70.0 (20.9) | 0.2 | 61 | 80.1 (19.4) | -0.2 | 46 | 85.0 (15.8) | 0.2 | |
| Final follow-up | 46 | 61.8 (22.7) | -0.4 | 139 | 63.6 (22.9) | -0.3 | 59 | 62.7 (24.0) | -0.2 | 46 | 83.4 (17.1) | 0.1 | ||||
| VT | Baseline | 45 | 69.8 (21.7) | 135 | 50.9 (20.1) | 59 | 50.3 (26.7) | 62 | 60.8 (22.1) | 46 | 59.5 (19.3) | |||||
| First follow-up | 45 | 69.1 (21.6) | 0.0 | 135 | 70.9 (19.2) | 1.0 | 59 | 67.3 (24.4) | 0.6 | 62 | 69.4 (22.3) | 0.4 | 46 | 71.6 (22.5) | 0.6 | |
| Final follow-up | 45 | 63.8 (22.6) | -0.3 | 135 | 64.3 (22.4) | 0.7 | 59 | 61.0 (27.7) | 0.4 | 46 | 72.1 (20.0) | 0.7 | ||||
| SF | Baseline | 49 | 87.8 (19.7) | 157 | 65.4 (26.2) | 66 | 72.7 (23.0) | 62 | 86.3 (18.6) | 46 | 72.6 (26.0) | |||||
| First follow-up | 49 | 84.9 (18.9) | -0.1 | 157 | 87.9 (19.5) | 0.9 | 66 | 86.7 (19.1) | 0.6 | 62 | 87.5 (22.6) | 0.1 | 46 | 90.8 (16.1) | 0.7 | |
| Final follow-up | 49 | 82.7 (24.0) | -0.3 | 157 | 84.3 (22.3) | 0.7 | 66 | 83.5 (25.2) | 0.5 | 46 | 94.3 (14.6) | 0.8 | ||||
| RE | Baseline | 37 | 76.1 (34.4) | 139 | 39.3 (43.6) | 56 | 40.5 (43.0) | 62 | 68.8 (38.1) | 46 | 52.9 (43.6) | |||||
| First follow-up | 37 | 76.6 (37.6) | 0.0 | 139 | 68.1 (39.7) | 0.7 | 56 | 64.0 (43.1) | 0.5 | 62 | 77.4 (36.6) | 0.2 | 46 | 81.9 (36.3) | 0.7 | |
| Final follow-up | 37 | 77.5 (40.9) | 0.0 | 139 | 65.5 (42.0) | 0.6 | 56 | 57.7 (42.4) | 0.4 | 46 | 92.0 (20.1) | 0.9 | ||||
| MH | Baseline | 45 | 86.6 (13.7) | 136 | 69.8 (21.6) | 59 | 71.0 (21.0) | 62 | 78.1 (18.4) | 46 | 71.8 (18.9) | |||||
| First follow-up | 45 | 85.2 (13.9) | -0.1 | 136 | 83.8 (17.7) | 0.6 | 59 | 80.0 (19.7) | 0.4 | 62 | 83.6 (17.6) | 0.3 | 46 | 84.3 (17.0) | 0.7 | |
| Final follow-up | 45 | 82.0 (15.6) | -0.3 | 136 | 80.6 (17.9) | 0.5 | 59 | 77.2 (20.1) | 0.3 | 46 | 86.2 (12.8) | 0.8 | ||||
*Note: First follow-up was three months for APM and six months for THR, TKR, and ACL groups; Final follow-up was five years for THR and TKR groups and two years for ACL.
PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
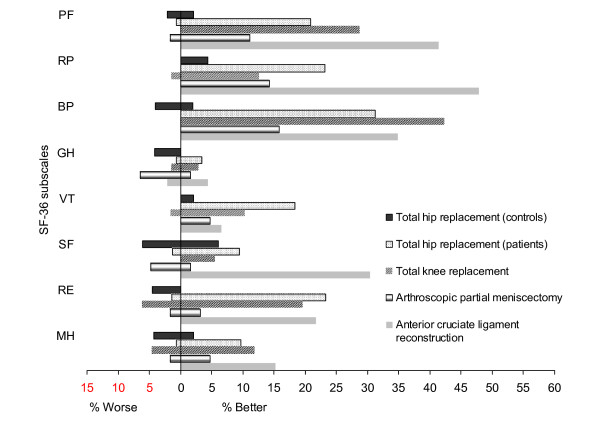
Effect sizes
ES for the first follow-up are presented in Figure 2 and in Table 3. Generally, the magnitude of changes in SF-36 was similar for patients in THR, TKR, and ACL groups, with smaller changes in the APM group. In the THR study, large improvements (ES≥0.80) at first follow-up occurred in PF, RP, BP, VT and SF scores, moderate improvements (ES 0.50–0.79) in RE and MH scores and small change in GH scores (ES = 0.20). For TKR patients, improvements at first follow-up were large in PF, RP, and BP scores, moderate in VT, SF, and RE scores and small in GH and MH scores. Improvements for APM patients could be classified as large on BP subscale only, with moderate improvements on PF and RP, small improvements on VT, RE, and MH, no change on SF, and a small deterioration on GH subscale. In the ACL study, improvements at first follow-up were large in PF, RP, and BP scores, moderate in VT, SF, RE, and MH scores, and small in GH scores.
Figure 2.
Effect sizes for SF-36 subscales across the study groups at first follow-up*. * Note: First follow-up was three months for APM and six months for TKR, THR, and ACL groups. PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
The ES across SF-36 subscales have changed only slightly over time, with similar values recorded for fist and final follow-ups (see Table 3). In the studies where data were available on intermediate follow-up (one year after the surgery in TKR and the ACL groups) ES were generally highest at one year (data not shown).
Floor and ceiling effects
Baseline floor effects, indicating worst possible scores, were present in the RP subscale for all groups and the RE subscale for THR, TKR, and ACL groups (see Table 4). More troublesome for documenting potential improvements in scores were ceiling effects at baseline, which were observed in the SF and RE subscales for all groups and in the RP and GH subscales for APM group. Ceiling effects generally increased during the follow-up. PF and VT were the only subscales that displayed no ceiling effects at baseline or at follow-ups across all surgical groups.
Table 4.
Floor and ceiling effects for SF-36 subscale scores for the study groups at first and final follow-up*
| SF-36 scores | Total hip replacement (controls) |
Total hip replacement (patients) |
Total knee replacement |
Arthroscopic partial meniscectomy |
Anterior cruciate ligament reconstruction |
||||||
| % scoring 0 |
% scoring 100 |
% scoring 0 |
% scoring 100 |
% scoring 0 |
% scoring 100 |
% scoring 0 |
% scoring 100 |
% scoring 0 |
% scoring 100 |
||
| PF | Baseline | - | 12.0 | 8.3 | - | 1.4 | - | 1.6 | 0.0 | 2.2 | - |
| First follow-up | - | 13.6 | 1.3 | 0.7 | - | 1.4 | - | 6.3 | - | 4.3 | |
| Final follow-up | 2.2 | 8.7 | 3.9 | - | 2.7 | - | - | 28.3 | |||
| RP | Baseline | 19.6 | 54.3 | 80.8 | 2.0 | 70.4 | 2.8 | 39.7 | 19.0 | 76.1 | - |
| First follow-up | 21.4 | 61.9 | 35.3 | 31.7 | 40.8 | 26.8 | 20.6 | 50.8 | 19.6 | 45.7 | |
| Final follow-up | 26.2 | 42.9 | 35.3 | 35.3 | 38.0 | 19.4 | 10.9 | 71.7 | |||
| BP | Baseline | - | 40.0 | 9.0 | 1.3 | 8.3 | 1.4 | - | 1.6 | - | 2.2 |
| First follow-up | - | 36.0 | 0.6 | 27.1 | - | 26.4 | - | 12.7 | - | 21.7 | |
| Final follow-up | 2.0 | 38.0 | 0.6 | 25.8 | - | 19.4 | 2.2 | 41.3 | |||
| GH | Baseline | - | 8.7 | - | 4.3 | - | 1.5 | - | 16.1 | - | 8.7 |
| First follow-up | - | 13.0 | 0.7 | 5.7 | - | 8.8 | - | 27.4 | - | 13.0 | |
| Final follow-up | - | 6.5 | 1.4 | 4.3 | - | 8.8 | - | 21.7 | |||
| VT | Baseline | - | 4.4 | 2.2 | 0.7 | 3.0 | 4.5 | - | 3.2 | - | - |
| First follow-up | - | 11.1 | 0.7 | 5.1 | - | 7.6 | - | 7.9 | - | 13.0 | |
| Final follow-up | 2.2 | 4.4 | 0.7 | 4.4 | 3.0 | 4.5 | - | 6.5 | |||
| SF | Baseline | - | 64.0 | 3.2 | 17.7 | - | 22.5 | - | 52.4 | 2.2 | 32.6 |
| First follow-up | - | 53.1 | 0.6 | 60.8 | - | 57.7 | - | 68.3 | - | 67.4 | |
| Final follow-up | 2.0 | 52.0 | 1.9 | 55.7 | 2.8 | 53.5 | - | 84.8 | |||
| RE | Baseline | 10.8 | 59.5 | 47.5 | 30.2 | 46.9 | 28.1 | 14.3 | 54.0 | 30.4 | 41.3 |
| First follow-up | 13.5 | 67.6 | 17.3 | 55.4 | 28.1 | 53.1 | 12.7 | 68.3 | 15.2 | 76.1 | |
| Final follow-up | 18.9 | 75.7 | 23.0 | 54.0 | 26.6 | 43.8 | - | 84.8 | |||
| MH | Baseline | - | 20.0 | - | 6.6 | - | 12.1 | - | 9.5 | - | - |
| First follow-up | - | 15.6 | 0.7 | 24.1 | - | 21.2 | - | 22.2 | - | 21.7 | |
| Final follow-up | - | 13.3 | - | 19.0 | - | 16.7 | - | 15.2 | |||
*Note: First follow-up was three months for APM and six months for THR, TKR, and ACL groups; Final follow-up was five years for THR and TKR groups and two years for ACL.
PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
Values indicating floor (15% or more with a score of 0) and ceiling (15% or more with a score of 100) effects are bolded.
Sensitivity: Group changes
The values of MDCgrp varied across the study groups and across the subscales but were generally lager than or equal to the values of MCIC (5 points or more), see Table 5. This suggests that at least some of the meaningful changes in group scores could not be detected with 95% confidence. The observed changes in the average SF-36 subscale scores however were larger than either the values of MDCgrp or MCIC across all intervention groups, indicating that statistically and clinically meaningful change in subscale scores had occurred following orthopedic surgery. Overall, GH subscale had the best ability to detect MCIC in orthopedic surgery, with MDCgrp values of five or less in all intervention groups (Table 5). RP and RE subscales had the worst ability to detect MCIC in group scores, with values of MDCgrp ranging from 8 (THR patients) to 12 (TKR and ACL) and from 9 (THR and APM) to 14 (TKR), respectively.
Table 5.
Change in SF-36 subscales across study groups
| Norm 95%CI¶ |
Total hip replacement (controls) |
Total hip replacement (patients) |
Total knee replacement |
Arthroscopic partial meniscectomy |
Anterior cruciate ligament reconstruction |
||||||||||||||||
| SEM* | MDC# | ΔM (SD) | SEM | MDC | ΔM (SD) | SEM | MDC | ΔM (SD) | SEM | MDC | ΔM (SD) | SEM | MDC | ΔM (SD) | |||||||
| Ind | Grp | Ind | Grp | Ind | Grp | Ind | Grp | Ind | Grp | ||||||||||||
| PF | 12 | 12 | 34 | 5 | -2 (12) | 18 | 49 | 4 | 27 (23) | 15 | 41 | 6 | 29 (17) | 16 | 45 | 6 | 15 (23) | 14 | 40 | 6 | 34 (21) |
| RP | 23 | 21 | 57 | 10 | -2 (26) | 33 | 91 | 8 | 33 (33) | 30 | 84 | 12 | 35 (34) | 32 | 88 | 11 | 27 (45) | 29 | 81 | 12 | 50 (30) |
| BP | 15 | 15 | 41 | 6 | -3 (16) | 20 | 54 | 5 | 37 (23) | 19 | 51 | 7 | 36 (27) | 17 | 46 | 6 | 20 (24) | 17 | 48 | 7 | 31 (22) |
| GH | 18 | 13 | 36 | 6 | -4 (13) | 14 | 39 | 4 | 0 (17) | 13 | 35 | 5 | 3 (14) | 10 | 27 | 3 | -3 (14) | 11 | 31 | 5 | 2 (12) |
| VT | 16 | 12 | 34 | 6 | -2 (14) | 16 | 44 | 4 | 17 (20) | 18 | 50 | 7 | 16 (22) | 14 | 39 | 5 | 9 (20) | 12 | 34 | 5 | 11 (14) |
| SF | 26 | 17 | 48 | 7 | -3 (21) | 19 | 53 | 5 | 19 (24) | 19 | 52 | 7 | 14 (25) | 14 | 38 | 5 | 1 (19) | 17 | 46 | 7 | 19 (26) |
| RE | 28 | 28 | 79 | 14 | 3 (31) | 35 | 97 | 9 | 25 (43) | 34 | 94 | 14 | 24 (47) | 27 | 74 | 9 | 9 (38) | 28 | 78 | 11 | 30 (43) |
| MH | 24 | 12 | 33 | 5 | -3 (14) | 15 | 40 | 4 | 12 (17) | 14 | 39 | 6 | 8 (18) | 12 | 33 | 4 | 5 (17) | 12 | 34 | 5 | 12 (17) |
Note: ¶ 95%CI for population-based normative scores on SF-36 subscales [36].
* SEM (Standard error of measurement) = √within subjects variance; Derived from ANOVA model with 'time of follow-up' as the within subjects factor.
# MDCind (Minimal detectable change at individual level) = 1.96*√2*SEM; MDCgrp (Minimal detectable change at group level) = (1.96*√2*SEM)/√n.
PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
Sensitivity: Individual changes
Sensitivity of SF-36 subscales to individual change was very low, as indicated by the high values of SEM and MDCind (Table 5). The MDCind in all study groups far exceeded the normative values of 95% CI (Table 5), indicating much greater amount of measurement error in SF-36 subscale in orthopedic settings than in the normative sample. Across all surgical groups, the GH subscale had the best sensitivity, with lowest values of MDCind in all intervention groups. However a change as large as 27% or greater needed to occur on this subscale before it could be considered 'real'. RP and RE subscales were least sensitive to individual change with values of MDCind ranging from 81 (ACL) to 91 (THR patients) and from 74 (APM) to 97 (THR patients), respectively.
Proportion improved or deteriorated
The proportion of participants who could be classified as either improved or deteriorated during the follow-up is presented in Figure 3. Participants in the control group of the THR study were approximately equally likely to deteriorate or improve while in the intervention groups, the participants were more likely to improve. An exception was the GH subscale, with the vast majority classified as unchanged: 96% in THR (patients) and TKR groups, 93% in ACL group, and 92% in APM group. Overall, surgical group with the greatest proportion of patients who improved was ACL, followed by TKR and THR groups, with APM patients being generally least likely to improve.
Figure 3.
Proportion improved or deteriorated on SF-36 subscales across the study groups at first follow-up*. * Note: First follow-up was three months for APM and six months for TKR, THR, and ACL groups. PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
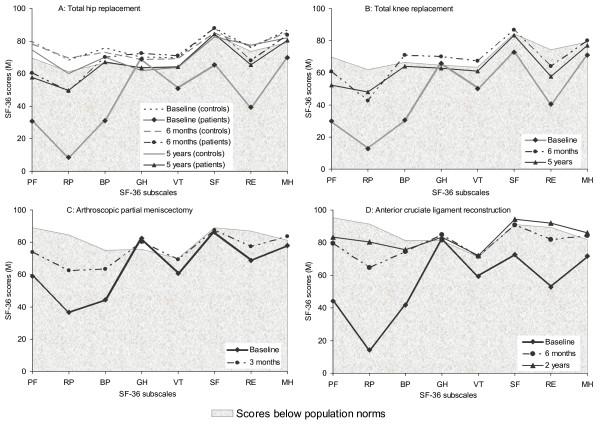
Population norm comparisons
Figure 4 indicates that at baseline, all the surgical groups deviated most from the population norms on the RP subscale and were most similar to the norms on the GH subscale. As expected, the controls in the THR study changed little throughout the follow-up and were comparable to population norms at each assessment. At baseline, only GH scores were within the population norms for THR and TKR patients. The THR patients generally improved but were still below the population norms on PF, RP, and RE subscales at six months and five years follow-up (Figure 4a). TKR patients also generally improved, scoring slightly above the norm on the GH, BP, and VT subscales (Figure 4b), but below the norms on PF, RP, and RE at six months. At five years follow-up, TKR patients had a slight drop in their PF, BP, VT, and RE scores and were still below the norm on PF, RP, and RE subscales.
Figure 4.
Comparisons of SF-36 subscale scores of the study groups with population norms. PF = Physical Functioning, RP = Role Physical, BP = Bodily Pain, GH = General Health, VT = Vitality, SF = Social Functioning, RE = Role Emotional, MH = Mental Health.
In the APM study, patients' baseline scores were slightly above the norm on the GH subscale and within the norm on SF and MH subscales. At three months follow-up, patients improved on PF, RP, BP, VT, and RE subscales but reached population norms on VT subscale only (Figure 4c). The ACL group had lower baseline scores than the norm on all subscales except GH. At six months, patients generally improved, but stayed below the norm on PF, RP, BP, and RE subscales. At two years follow-up, further improvements were recorded on RP and RE subscales, with patients scoring slightly above the norm on RE, but remaining below the norm on RP subscale (Figure 4d).
Discussion
Orthopedic surgery is performed in response to a broad spectrum of conditions, including degenerative disorders and sports injury. We examined the magnitude and meaningfulness of changes in SF-36 subscales in four orthopedic populations and compared changes in patients' health status with the age and sex matched population norms. Large improvements (ES≥0.80) were observed on physical dimensions of the SF-36 (PF, RP, and BP subscales). Improvements on the mental and social dimensions (SF, RE, VT, and MH subscales) were small to moderate, while GH scores remained relatively unchanged during the study period. Group changes on all subscales but GH were clinically and statistically meaningful. Despite improvements, patients were still below the age and sex matched population norms on physical dimensions but scores on mental and social dimensions generally approached population norms following the surgery. On an individual level, floor and ceiling effects were observed on several subscales and the sensitivity to individual change was very low. Of the eight SF-36 subscales, the GH subscale had the best sensitivity to detect changes in health status of individual patients, although values of MDCind were very high even on this subscale. PF subscale generally performed best, with no floor or ceiling effects and large changes in patients' scores following surgery however it had low sensitivity to change in individual or group scores.
Our results also indicate that overall, patients who underwent THR, TKR, APM, and ACL reconstruction surgery showed improvements in the health domains assessed by the SF-36 subscales. While the magnitude of the changes in SF-36 domains varied between the surgical groups, generally, greatest improvements were recorded for the physical dimensions, including physical function, role physical, and bodily pain, with more moderate changes in vitality, social functioning, role emotional, and mental health. Although no comparable data are currently available for APM, previous studies with THR, TKR, and ACL patients also documented greatest changes in the physical domains [18,38-42]. This study supports findings of past studies and extends them to a wider range of orthopedic surgery types.
Several researchers have previously recommended that interventions conducted with orthopedic populations should include at least one generic health status questionnaire in addition to condition-specific measures [8,41,43-45]. Disease-specific instruments, such as the Knee Injury and Osteoarthritis Outcome Score (KOOS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and Arthritis Impact Measurement Scales (AIMS) for example, have been found reliable, valid, and sensitive measures of patient-reported outcomes in arthritis [20,46,47]. Disease-specific measures were also reported to be more sensitive in detecting change following surgical interventions than the generic instruments [8]. However, generic health status measures, such as SF-36, provide a broader insight into patients' quality of life and allow comparisons across conditions. Our results provide some support for the use of SF-36 to evaluate outcomes of THR, TKR, and ACL surgery, as improvements in vitality, social functioning, role emotional, and mental health of these surgical groups would have been missed if only disease-specific instruments were used.
In APM surgery, the changes in SF-36 scores were smaller than in other surgical groups. The mean age in the meniscectomy group was 45 years, implying a large proportion of degenerative meniscus tears in this group. Degenerative tear is a strong risk factor for future radiographic osteoarthritis and have been suggested to signal incipient knee OA [48]. Thus, the modest improvements seen in this group might be due to the surgery being performed for the wrong reason. A recent RCT in subjects with an MRI-verified meniscal tear compared meniscectomy and exercise with exercise alone and found no superior effect of meniscectomy, further questioning the effectiveness of meniscectomy in middle-aged people [49].
Another important finding in this study was that observed changes on all SF-36 subscales except GH were clinically and statistically meaningful at a group level. However, values of MDCgrp in our study where higher than the established values of MCIC [36] for almost all subscales, indicating that at least some of the meaningful changes in group scores of orthopedic patients could not be detected with 95% confidence due to measurement error. Sensitivity of SF-36 subscales was even lower at an individual level, with very large changes in scores needed to occur before such changes could be classified as real with 95% confidence. The disparities in the amount of measurement error between ours and the normative samples [36] highlight the importance of evaluating outcome measures in the populations and settings for which these measures will be used. Poor sensitivity of SF-36 to individual change was previously observed in an analytical review of health status measures, with confidence intervals unacceptably wide to be of practical use for individual assessment [50] and in prospective follow-up of THR patients [17], raising concerns about the ability of SF-36 to reliably detect meaningful changes in health status of individuals. Information on sensitivity of a measure can potentially be used by clinicians and researchers to determine whether observed changes in the health status of individual patients or groups of patients reflect real changes as opposed to random variations. However, since our results suggest poor sensitivity of SF-36 subscales to individual change, we advise against using this questionnaire to monitor individual patients.
Previous studies with TKR, THR, and ACL patients reported that the GH subscale of SF-36 showed very little change in group scores after the surgery [17,39,40,42]. Similar findings were obtained in our study, with GH subscale showing little or no change across the study groups. However, group results are not necessarily a valid indicator of changes in health state of individuals, especially in situations where there are as many patients deteriorating as improving: when averaged for the whole group, the results may appear to suggest no change. Examination of individual scores in our study indicated that very few individuals could be classified as changed across the intervention groups on GH subscale. This finding extends the results of previous studies and underscores the importance of taking into account individual as well as group changes when evaluating outcomes in longitudinal studies [51].
Our results also indicate that patients in all intervention groups had general health scores comparable with the age and sex adjusted population norms. Lack of improvement in GH scores across the study groups is therefore not surprising as the participants were already in very good general health before the surgery. We also found that despite substantial improvements in health status over the study period, patients in the THR, TKR, APM, and ACL studies remained below the age and sex norms for the general population on several SF-36 subscales. While no data is currently available that compares outcomes of APM with the population norms, at least two previous investigations with THR and TKR patients [39,52] reported that patients who undergo these surgical interventions still fall short of age and sex adjusted population norms on health domains measured by SF-36.
We also found that floor and/or ceiling effects were present in most SF-36 subscales for nearly all intervention groups; hence the results of magnitude of changes (effect sizes) following orthopedic surgery need to be interpreted with caution, as changes can not be reliably estimated for individuals with extreme scores. The presence of floor and ceiling effects also indicates that SF-36 is not covering the full continuum of impairment and recovery in orthopedic populations. Substantial floor and ceiling effects for SF-36 scores were previously reported in other investigations [2,40], further indicating poor utility of SF-36 in orthopedics.
This study is subjected to some limitations. Firstly, it was not specifically designed to assess performance of SF-36 in different types of orthopedic surgery. Different methodologies were used and the study groups differed on some demographic variables. Therefore, some differences across groups may be related to study effects. Secondly, MCIC in the SF-36 domains are not well studied in orthopedic surgery, therefore we have used established population norms to gauge the amount of measurement error around individual change scores in orthopedic surgery settings. While the results indicate low sensitivity of SF-36 to individual change, future studies need to compare the MDC values with empirically derived estimates of MCIC following different types of orthopedic surgery. Finally, the presence of floor and ceiling effects on several SF-36 subscales suggests that the amount of change that could potentially occur for individual participants during the follow-up may have been influenced by their baseline scores, with greater possible range of change scores for individuals with midrange scores at baseline than for those who had more extreme baseline scores. As a result, within-subjects variability may have been underestimated, potentially distorting estimates of MDC [29,53].
One of the major strengths of this study is the use of data from four different types of orthopedic surgery. While several past studies investigated measurement properties of SF-36 in joint replacement surgery [7,9,17,38,45,54], to the best of our knowledge, ours is the first study to consider performance of SF-36 in THR, TKR, APM, and ACL reconstruction surgery simultaneously. Additional strengths of this study are the prospective design of the studies included and the high follow-up rates (65–100%). These aspects of study methodology serve to reduce bias and improve generilizability of results. Finally, we presented estimates of change in SF-36 subscale scores expressed in standardized units (ES) and in the original scale of measurement (MDC and SEM). While estimates of change in original scale of measurement have the advantage of being conceptually easy to interpret, ES can be used by clinicians and researchers to compare changes in patients' health status on different measures obtained in the same study, to evaluate efficacy of different interventions, or to compare results of different studies.
Conclusion
Large to moderate meaningful changes in group scores were observed in all SF-36 subscales except GH across the intervention groups. Therefore, in orthopedic settings, the SF-36 can be used at a group level to show change in physical, mental, and social dimensions following different types of surgery and to make comparisons of the surgical groups with population norms. At an individual level however, SF-36 subscale had low sensitivity to individual change. Although further research is needed to establish the minimal clinically important change in SF-36 scores in orthopedic settings, we caution against using SF-36 to monitor health status of individual patients undergoing orthopedic surgery.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LB participated in study design, performed the statistical analysis, and drafted the manuscript. RHO participated in study design and helped to draft the manuscript. AN carried out data collection (THR study). RB participated in study design and helped to draft the manuscript. EMR conceived of the study, participated in the design of the study, carried out data collection,TKR, APM, and ACL studies, and helped to draft the manuscript. All authors read and approved the final manuscript.
Acknowledgments
Acknowledgements
Lucy Busija's work was supported by a University of Melbourne Postgraduate Research Scholarship and a Universitas 21 Solander Travel Scholarship.
Richard H Osborne was supported in part by an Australian National Health and Medical Research Council (NHMRC) Population Health Career Development Award, a Universitas 21 Solander Travel Fellowship, and a Bone and Joint Decade Fellowship.
Anna Nilsdotter's work was supported by Halmstad Central Hospital.
Rachelle Buchbinder was supported in part by an Australian NHMRC Practitioner Fellowship.
Ewa M Roos' work was supported by The Swedish Research Council, the Swedish Rheumatism Association, the Faculty of Medicine Lund University, and Region Skåne.
We would like to thank the steering group of the KANON-study for generously allowing the use of data from the KANON-study.
The KANON study was funded by Pfizer Global Research, Thelma Zoegas fund, Stig & Ragna Gorthon research foundation, The Swedish National Centre for Research in Sports, The Swedish Research Council, the Medical Faculty Lund University (ALF) and Region Skåne.
We wish to thank Professor Peter Fayers, Department of Public Health, the University of Aberdeen, for his practical and insightful statistical advice.
Contributor Information
Lucy Busija, Email: l.busija@pgrad.unimelb.edu.au.
Richard H Osborne, Email: richardo@unimelb.edu.au.
Anna Nilsdotter, Email: Anna.Nilsdotter@lthalland.se.
Rachelle Buchbinder, Email: Rachelle.Buchbinder@med.monash.edu.au.
Ewa M Roos, Email: eroos@health.sdu.dk.
References
- Ware JE, Kosinski M, Gandek B. SF-36 Health Survey: Manual and interpretation guide 2000 edn. Lincoln: Quality Metric Inc; 1993. [Google Scholar]
- Baron R, Elashaal A, Germon T, Hobart J. Measuring outcomes in cervical spine surgery: Think twice before using the SF-36. Spine. 2006;31:2575–2584. doi: 10.1097/01.brs.0000240694.83621.52. [DOI] [PubMed] [Google Scholar]
- Coster WJ, Haley SM, Jette AM. Measuring patient-reported outcomes after discharge from inpatient rehabilitation settings. J Rehabil Med. 2006;38:237–242. doi: 10.1080/16501970600609774. [DOI] [PubMed] [Google Scholar]
- Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis. 2001;60:834–840. [PMC free article] [PubMed] [Google Scholar]
- Strine TW, Hootman JM, Chapman DP, Okoro CA, Balluz L. Health-related quality of life, health risk behaviors, and disability among adults with pain-related activity difficulty. Am J Public Health. 2005;95:2042–2048. doi: 10.2105/AJPH.2005.066225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne RH, Hawthorne G, Lew EA, Gray LC. Quality of life assessment in the community-dwelling elderly: Validation of the Assessment of Quality of Life (AQoL) Instrument and comparison with the SF-36. J Clin Epidemiol. 2003;56:138–147. doi: 10.1016/S0895-4356(02)00601-7. [DOI] [PubMed] [Google Scholar]
- Blanchard C, Feeny D, Mahon JL, Bourne R, Rorabeck C, Stitt L, Webster-Bogaert S. Is the Health Utilities Index valid in total hip arthroplasty patients? Qual Life Res. 2004;13:339–348. doi: 10.1023/B:QURE.0000018479.52075.bf. [DOI] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Munro J, Walters SJ, Snaith ML. Generic and condition-specific outcome measures for people with osteoarthritis of the knee. Rheumatology (Oxford) 1999;38:870–877. doi: 10.1093/rheumatology/38.9.870. [DOI] [PubMed] [Google Scholar]
- Nilsdotter AK, Roos EM, Westerlund JP, Roos HP, Lohmander LS. Comparative responsiveness of measures of pain and function after total hip replacement. Arthritis Rheum. 2001;45:258–262. doi: 10.1002/1529-0131(200106)45:3<258::AID-ART258>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Kosinski M, Keller SD, Ware JE, Jr, Hatoum HT, Kong SX. The SF-36 Health Survey as a generic outcome measure in clinical trials of patients with osteoarthritis and rheumatoid arthritis: Relative validity of scales in relation to clinical measures of arthritis severity. Med Care. 1999;37:MS23–39. doi: 10.1097/00005650-199905001-00003. [DOI] [PubMed] [Google Scholar]
- Yost KJ, Haan MN, Levine RA, Gold EB. Comparing SF-36 scores across three groups of women with different health profiles. Qual Life Res. 2005;14:1251–1261. doi: 10.1007/s11136-004-6673-8. [DOI] [PubMed] [Google Scholar]
- Sanson-Fisher RW, Perkins JJ. Adaptation and validation of the SF-36 Health Survey for use in Australia. J Clin Epidemiol. 1998;51:961–967. doi: 10.1016/S0895-4356(98)00087-0. [DOI] [PubMed] [Google Scholar]
- Ruta DA, Hurst NP, Kind P, Hunter M, Stubbings A. Measuring health status in British patients with rheumatoid arthritis: reliability, validity and responsiveness of the short form 36-item health survey (SF-36) Br J Rheumatol. 1998;37:425–436. doi: 10.1093/rheumatology/37.4.425. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics . National Health Survey: SF36 Population Norms, Australia, 1995. Cat. no. 4399.0. Canberra: ABS; 1997. [Google Scholar]
- Sullivan M, Karlsson J, Ware JE. SF-36 Swedish Manual and Interpretation Guide. Gothenburg: Gothenburg University; 1994. [Google Scholar]
- Ware JE, Kosinski M, Dewey JE. How to score version 2 of the SF-36 Health Survey. Lincoln: Quality Metric Inc; 2000. [Google Scholar]
- Quintana JM, Escobar A, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after hip joint replacement. Osteoarthritis Cartilage. 2005;13:1076–1083. doi: 10.1016/j.joca.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Escobar A, Quintana JM, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2006;15:273–280. doi: 10.1016/j.joca.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: A prospective study. Ann Rheum Dis. 2003;62:923–930. doi: 10.1136/ard.62.10.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) – Validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17. doi: 10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos EM, Roos HP, Ryd L, Lohmander LS. Substantial disability 3 months after arthroscopic partial meniscectomy: A prospective study of patient-relevant outcomes. Arthroscopy. 2000;16:619–626. doi: 10.1053/jars.2000.4818. [DOI] [PubMed] [Google Scholar]
- Frobell RB, Lohmander LS, Roos EM. The challenge of recruiting patients with anterior cruciate ligament injury of the knee into a randomized clinical trial comparing surgical and non-surgical treatment. Contemp Clin Trials. 2007;28:295–302. doi: 10.1016/j.cct.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Keller SD, Majkut TC, Kosinski M, Ware JE., Jr Monitoring health outcomes among patients with arthritis using the SF-36 Health Survey: overview. Med Care. 1999;37:MS1–9. doi: 10.1097/00005650-199905001-00001. [DOI] [PubMed] [Google Scholar]
- Kosinski M, Keller SD, Hatoum HT, Kong SX, Ware JE., Jr The SF-36 Health Survey as a generic outcome measure in clinical trials of patients with osteoarthritis and rheumatoid arthritis: Tests of data quality, scaling assumptions and score reliability. Med Care. 1999;37:MS10–22. doi: 10.1097/00005650-199905001-00002. [DOI] [PubMed] [Google Scholar]
- McCallum J. The SF-36 in an Australian sample: Validating a new, generic health status measure. Aust J Public Health. 1995;19:160–166. doi: 10.1111/j.1753-6405.1995.tb00367.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for Social and Behavioural Sciences. New York: Academic Press; 1977. [Google Scholar]
- de Vet HC, Bouter LM, Bezemer PD, Beurskens AJ. Reproducibility and responsiveness of evaluative outcome measures: Theoretical considerations illustrated by an empirical example. Int J Technol Assess Health Care. 2001;17:479–487. doi: 10.1017/S0266462301106148. [DOI] [PubMed] [Google Scholar]
- Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Measurement error. BMJ. 1996;313:744. doi: 10.1136/bmj.313.7059.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masse J, Bland JM, Doyle JR, Doyle JM. Measurement error. BMJ. 1997;314:147. [PMC free article] [PubMed] [Google Scholar]
- Beckerman H, Roebroeck ME, Lankhorst GJ, Becher JG, Bezemer PD, Verbeek AL. Smallest real difference, a link between reproducibility and responsiveness. Qual Life Res. 2001;10:571–578. doi: 10.1023/A:1013138911638. [DOI] [PubMed] [Google Scholar]
- de Boer MR, de Vet HC, Terwee CB, Moll AC, Volker-Dieben HJ, van Rens GH. Changes to the subscales of two vision-related quality of life questionnaires are proposed. J Clin Epidemiol. 2005;58:1260–1268. doi: 10.1016/j.jclinepi.2005.04.007. [DOI] [PubMed] [Google Scholar]
- de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, Bouter LM. Minimal changes in health status questionnaires: Distinction between minimally detectable change and minimally important change. Health Qual Life Outcomes. 2006;4:54. doi: 10.1186/1477-7525-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Standard deviations and standard errors. BMJ. 2005;331:903. doi: 10.1136/bmj.331.7521.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spies-Dorgelo MN, Terwee CB, Stalman WAB, Windt DAWM van der. Reproducibility and responsiveness of the Functional Handicap Score (FHS) and Dutch Arthritis Impact Score (Dutch-AIMS2) for patients with wrist or hand problems in primary care. Health Qual Life Outcomes. 2006;10:87. doi: 10.1186/1477-7525-4-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinski MA, Gandek B. SF-36 Health Survey: Manual and interpretation guide. Lincoln: Quality Metric Inc; 2005. [Google Scholar]
- Wyrwich K, Tierney W, Wolinsky F. Using the standard error of measurement to identify important changes on the Asthma Quality of Life Questionnaire. Qual Life Res. 2002;11:1–7. doi: 10.1023/A:1014485627744. [DOI] [PubMed] [Google Scholar]
- Bachmeier CJ, March LM, Cross MJ, Lapsley HM, Tribe KL, Courtenay BG, Brooks PM. A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage. 2001;9:137–146. doi: 10.1053/joca.2000.0369. [DOI] [PubMed] [Google Scholar]
- Jones CA, Voaklander DC, Johnston DW. The effect of age on pain, fuction, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161:454–460. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- Marx RG, Jones EC, Atwan NC, Closkey RF, Salvati EA, Sculco TP. Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J Bone Joint Surg Am. 2005;87-A:1999–2005. doi: 10.2106/JBJS.D.02286. [DOI] [PubMed] [Google Scholar]
- Salaffi F, Carotti M, Grassi W. Health-related quality of life in patients with hip or knee osteoarthritis: Comparison of generic and disease-specific instruments. Clin Rheumatol. 2005;24:29–37. doi: 10.1007/s10067-004-0965-9. [DOI] [PubMed] [Google Scholar]
- Shapiro ET, Richmond JC, Rockett SE, McGrath MM, Donaldson WR. The use of generic, patient-based health assessment (SF-36) for evaluation of patients with anterior cruciate ligament injuries. Am J Sports Med. 1996;24:196–200. doi: 10.1177/036354659602400214. [DOI] [PubMed] [Google Scholar]
- Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ. 2004;13:873–884. doi: 10.1002/hec.866. [DOI] [PubMed] [Google Scholar]
- Dieppe P. Recommended methodology for assessing the progression of osteoarthritis of the hip and knee joints. Osteoarthritis Cartilage. 1995;3:73–77. doi: 10.1016/S1063-4584(05)80040-8. [DOI] [PubMed] [Google Scholar]
- Kreibich DN, Vaz M, Bourne RB, Rorabeck CH, Kim P, Hardie R, Kramer J, Kirkley A. What is the best way of assessing outcome after total knee replacement? Clin Orthop Relat Res. 1996:221–225. doi: 10.1097/00003086-199610000-00031. [DOI] [PubMed] [Google Scholar]
- de Groot IB, Favejee MM, Reijman M, Verhaar JAN, Terwee CB. The Dutch version of the knee injury and osteoarthritis outcome score: A validation study. Health Qual Life Outcomes. 2008;6 doi: 10.1186/1477-7525-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosemann TT, Joos SS, Koerner TT, Szecsenyi JJ, Laux GG. Comparison of AIMS2-SF, WOMAC, x-ray and a global physician assessment in order to approach quality of life in patients suffering from osteoarthritis. BMC Musculoskelet Disord. 2006;7:6. doi: 10.1186/1471-2474-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50:2811–2819. doi: 10.1002/art.20489. [DOI] [PubMed] [Google Scholar]
- Herrlin S, Hållander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: A prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15:393–401. doi: 10.1007/s00167-006-0243-2. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: Are available health status surveys adequate? Qual Life Res. 1995;4:293–307. doi: 10.1007/BF01593882. [DOI] [PubMed] [Google Scholar]
- Paradowski PT, Englund M, Roos EM, Lohmander LS. Similar group mean scores, but large individual variations, in patient-relevant outcomes over 2 years in meniscectomized subjects with and without radiographic knee osteoarthritis. Health Qual Life Outcomes. 2004;2:38. doi: 10.1186/1477-7525-2-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March LM, Cross MJ, Lapsley H, Brnabic AJM, Tribe KL, Bachmeier CJM, Courtenay BG, Brooks PM. Outcomes after hip or knee replacement surgery for osteoarthritis – A prospective cohort study comparing patients' quality of life before and after surgery with age-related population norms. Med J Aust. 1999;171:235–238. [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric Theory. New York: McGraw Hill; 1994. [Google Scholar]
- Soderman P, Malchau H. Validity and reliability of Swedish WOMAC osteoarthritis index: a self-administered disease-specific questionnaire (WOMAC) versus generic instruments (SF-36 and NHP) Acta Orthop Scand. 2000;71:39–46. doi: 10.1080/00016470052943874. [DOI] [PubMed] [Google Scholar]