Abstract
A retrospective study was conducted in 179 consecutive patients (48 males, 131 females; mean age: 72.0 ± 8.59 years; range: 51–93) with single symptomatic acute amyelic osteoporotic vertebral fracture presenting between September 2004 and September 2005 to the Santa Lucia Foundation in Rome, Italy. Vertebral fractures usually become manifest due to pain which can be debilitating. Treatment depends on the presence or absence of spinal cord involvement. In the first case, surgical stabilization is mandatory. In the second case, treatment may be performed either by conservative medical therapy (CMT) or percutaneous vertebroplasty (PVT). The aim of this study was to evaluate the effectiveness, costs and cost-effectiveness of percutaneous vertebroplasty. After 2 weeks of analgesic therapy, 153 patients presented refractory pain and were offered treatment by PVT. A total of 58 patients accepted and underwent PVT (PVT group), while 95 refused and underwent conservative medical therapy (CMT group). Follow-up was performed by specialist consults, spine radiography and MRI and a self-assessment questionnaire evaluating pain using a Visual Analogue Scale (VAS) and function using an ambulation and an Activities of Daily Living (ADL) scale. A 12-month follow-up was obtained in 86 of 95 (90.5%) CMT group patients and 54 of 58 (93.1%) PVT group patients. Significant reduction of VAS and improvement of ambulation and ADL was observed in both groups at 1 week and 3 and 12 months (P < 0.05; Wilcoxon signed rank test), however, these results were significantly superior in the PVT group at 1 week and 3 months (P < 0.05; Mann–Whitney U test). Average cost per patient at 1 week and 3 and 12 months were respectively 755.49 ± 661.96, 3791.95 ± 3341.97 and 4299.55 ± 3211.53 € (CMT group) and 3311.35 ± 0.32, 3745.30 ± 3.59 and 4101.05 ± 755.41 € (PVT group). PVT resulted significantly more cost-effective than CMT with regards to the three scales at 1 week (P < 0.05; Mann–Whitney U test). At 3 months PVT was more cost-effective than CMT with regards to the three scales, however, the difference was significant only with regards to ambulation. No significant differences in cost-effectiveness where found between the two groups at 12 months. PVT should be considered the treatment of first choice in symptomatic acute amyelic osteoporotic vertebral fractures with refractory pain after a short period of analgesic therapy.
Keywords: Percutaneous vertebroplasty, Vertebral fracture, Osteoporosis, Cost-effectiveness
Introduction
Vertebral fractures are the most common fractures associated to osteoporosis, although they often remain unidentified. It is calculated that of the 1.5 million osteoporotic fractures occurring yearly in the USA, 750,000 involve the spine, 250,000 the femur, 250,000 the wrist and the remaining 250,000 other sites [1].
Osteoporotic vertebral fractures are pathological bone fractures in which a force, otherwise unable to produce lesions in normal bone tissue, when exerted on a bone with a structure weakened by osteoporosis yields a fracture. Due to the peculiar kinetic of the spine, 80% of pathological vertebral fractures are located at the dorsal-lumbar passage. The most frequent sites of osteoporotic vertebral fractures are in decreasing order L1, D12 and L2 [18]. Vertebral fractures can be divided into myelic and amyelic fractures according to the presence or absence of a spinal cord involvement.
According to the International Osteoporosis Foundation, approximately 200 million persons worldwide are potentially at risk of an osteoporotic vertebral fracture [2].
Vertebral fractures usually become manifest due to pain which can have variable intensities and may affect radically the patient’s quality of life. Usually the intensity of the pain depends on the site of the fracture, the number of fractures and their severity, however approximately half of the patients refer no pain [14].
When pain is present, often even under analgesic drug therapy, it is debilitating and patients require assistance for the most elementary activities of daily living, such as personal care taking. Furthermore, an altered equilibrium caused by the progressive kyphosis results in a fear of falling, thus bringing the patient to social isolation.
Some patients present an intolerable and highly debilitating pain persisting for several weeks or months after the trauma and require hospitalization for continuous care. Furthermore, vertebral fractures are associated to an increased morbidity and mortality rate due to respiratory complications [8].
The treatment of a vertebral fracture depends on the presence or absence of involvement of the spinal cord. In the first case, surgical stabilization is mandatory. In the second case, treatment may be performed either by conservative medical therapy (CMT) or percutaneous vertebroplasty (PVT). Although the effectiveness of PVT has been already described in literature, to date there exist no studies evaluating its cost-effectiveness [5, 11, 12].
The aim of this study was to evaluate the cost-effectiveness of PVT compared to CMT in patients with acute osteoporotic amyelic symptomatic vertebral fractures.
Materials and methods
Patient population
A retrospective study, with full institutional review board approval and waiver of informed consent, was performed on 179 consecutive patients (48 males, 131 females; mean age: 72.0 ± 8.59 years; range: 51–93) affected by symptomatic acute amyelic osteoporotic fracture of a single vertebral body presenting between September 2004 and September 2005 to the Centre for Prevention, Diagnosis and Cure of Osteoporosis of the Santa Lucia Foundation in Rome, Italy.
Diagnosis was made by spine radiography. The vertebral fracture was successively evaluated by magnetic resonance imaging. The osteoporotic condition was assessed by bone densitometry.
All patients presented an osteoporotic fracture of a single vertebral body, occurring no more than 3 months earlier, positive for bone marrow edema and negative for spinal cord involvement at magnetic resonance imaging.
A total of 34 patients (19.0%) with severe pain and disability, requiring bed immobilization and continuous care, were admitted to hospital while the remaining 145 (81.0%) patients were followed as outpatients.
All patients underwent 2 weeks of analgesic drug therapy by oral administration of 2,400 mg/day of ibuprofen (Brufen, Abbot), 200 mg/day of diclofenac (Voltaren, Innovex) and 500 mg of paracetamol + 30 mg of codeine × 4/day (Coefferalgan, Bristol-Myers Squibb Srl, Italia) for the first week followed by 5–15 mg × 2/day of oxycodone (Oxycontin, Mundipharma Pharmaceutic Srl) and 50–200 mg × 2/day of tramadol (Tradonal, Viatris) for the second week.
After 2 weeks of drug therapy, 153 patients (41 males and 112 females; mean age: 71.0 ± 9.95 years; range: 51–92 years) presented refractory pain.
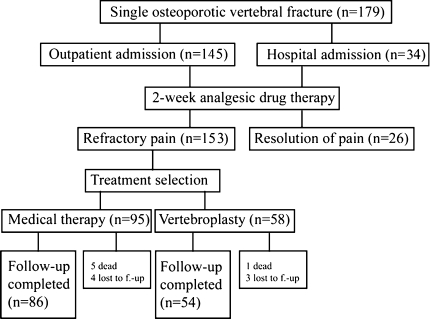
All patients with refractory pain were offered PVT. A total of 95 (62.1%) patients (25 males, 70 females; mean age: 70.2 ± 7.68 years; range: 56–90) refused this procedure and were treated by CMT (CMT group), while 58 (37.9%) patients (16 males, 42 females; mean age: 73.5 ± 8.90 years; range: 51–92) accepted and were treated by PVT (PVT group) at the Department of Diagnostic Imaging, Molecular Imaging, Interventional Radiology and Radiation Therapy of the University Polyclinic of Tor Vergata in Rome (Fig. 1).
Fig. 1.
Patient enrolment, treatment selection and follow-up
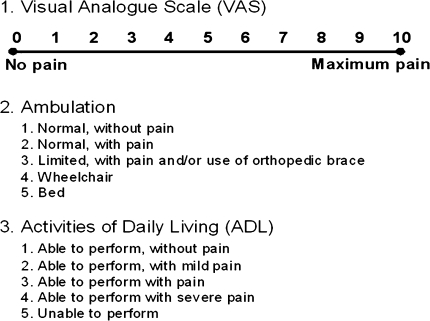
The degree of pain and function were evaluated in all patients prior to continuing with CMT or PVT using a self-assessment questionnaire completed in an examination room in presence of a physician. This questionnaire included a 0–10 points Visual Analogue Scale (VAS) for the evaluation of pain and a 1–5 points ambulation scale and Activities of Daily Living scale (ADL) for the evaluation of function (Fig. 2).
Fig. 2.
Self-assessment questionnaire for the degree of pain and ambulation and the ability to perform activities of daily living
Independently from the selected treatment, all patients continued the preexisting drug therapy for the osteoporotic condition. No substantial differences were found between the two groups in terms of the types of drugs used and their dosages.
Conservative medical therapy
Patients that refused PVT continued the preexisting analgesic drug therapy (oral administration of 5–15 mg × 2/day of oxycodone and 50–200 mg × 2/day of tramadol) for further 3 weeks.
The drug therapy protocol for patients with pain persisting after this period consisted of oral administration of 5–15 mg × 2/day of oxycodone, 50–200 mg × 2/day of tramadol and 300–800 mg × 3/day of gabapentin (Neurontin, Pfizer Italia) for 30 weeks. If pain still persisted, the same drug therapy was extended for additional 19 weeks.
An orthopedic back brace was applied to all patients. Finally, all patients underwent physical therapy. This consisted of 30–40 sessions of massotherapy and rehabilitation gymnastic and 20 sessions of postural restoration and hydrokinesitherapy in inpatients and 20 sessions of massotherapy, rehabilitation gymnastic, analgesic electrotherapy and magnetotherapy in outpatients. Physical therapy was repeated in patients with persisting pain.
Percutaneous vertebroplasty
Patients who accepted treatment by PVT continued the preexisting drug therapy (oral administration of 5–15 mg × 2/day of oxycodone and 50–200 mg × 2/day of tramadol) for another week, during which the procedure was performed. The technical features of the procedure have been previously described [10].
Patients with pain persisting after this period were treated by oral administration of 5–15 mg × 2/day of oxycodone, 50–200 mg × 2/day of tramadol and 300–800 mg × 3/day of gabapentin for additional 2 weeks.
Signed informed consent was obtained in all patients prior to the procedure.
Follow-up
Follow-up was performed at 1 week and at 3 and 12 months by physiatric and radiological consult and by compilation of the self-assessment questionnaire, at 1, 3 and 12 months by full spine radiography and at 3 months by magnetic resonance imaging of the involved spinal segment.
An additional physiatric consult was performed at 8 months in patients with persisting pain requiring a revision of the analgesic drug therapy.
Endpoints and statistical analyses
The endpoints of our study were the assessment of effectiveness, costs and cost-effectiveness of PVT compared to CMT in patients with osteoporotic fracture of a single vertebral body completing a 12-month follow-up.
Effectiveness was evaluated in terms of the reduction of pain (VAS) and the improvement of ambulation (ambulation scale) and ability to perform the activities of daily living (ADL scale) at 1 week and at 3 and 12 months.
Costs were evaluated for each group by adding hospital care costs (daily tariff1 or DRG2) to all outpatient costs. Finally, an average patient cost was calculated for each group at 1 week and at 3 and 12 months.
Data on resource use were obtained through medical record review.
Direct non-sanitary patient costs (travel to receive care, time off usual activities) were not included in this study.
Cost-effectiveness was measured as the average cost per patient per reduction of one point in the VAS, ambulation or ADL scale.
All data are expressed as mean ± SD (range). Categorical data are expressed as percentages. Several times the variances between groups were not homogenous (we used Bartlett’s Chi square test for Inequality of Population Variances), thus we preferred to use Mann–Whitney U test to check differences of numeric variables between groups. The Wilcoxon signed rank test was used to evaluate statistically significant differences before and after treatment. Categorical differences were tested by the Fischer exact method. All P values were two-tailed and a value less than 0.05 was considered statistically significant. Input data and statistical analysis was performed using the Epi Info 3.4.4 software (CDC, Atlanta, USA).
Results
Conservative medical therapy
A total of 95 (62.1%) patients (25 males, 70 females; mean age: 70.2 ± 7.68 years; range: 56–90) refused to be treated by PVT and continued CMT. Twenty (21.1%) of these patients had been already hospitalized and no further hospital admissions were required. The site of the vertebral fracture was lumbar in 55 (57.9%) cases and thoracic in 40 (42.1%) cases.
During the 12-month follow-up period, 5 (5.3%) patients died and 4 (4.2%) patients were lost to follow-up (Fig. 1). The cause of death was related to the vertebral fracture in three patients. In two cases, for pulmonary embolism caused by deep venous thrombosis secondary to prolonged immobilization and in one case for pneumonia complicating a respiratory insufficiency worsened by the vertebral fracture. The cause of death was not related to the vertebral fracture in the other two deaths occurring (1 acute myocardial infarction and 1 stroke).
A 12-month follow-up was thereby obtained in 86 (90.5%) patients (21 males, 65 females; mean age: 69.7 ± 7.54 years; range: 56–90). Twenty (23.3%) of these patients had been already hospitalized at the time of treatment selection.
The mean hospitalization time in the patients completing the 12-month follow-up period was 33.45 ± 6.06 days.
Percutaneous vertebroplasty
A total of 58 (37.9%) patients (16 males, 42 females; mean age: 73.5 ± 8.90 years; range: 51–92) accepted treatment by PVT. Fourteen (24.1%) of these patients, had been already hospitalized. PVT was performed in an inpatient setting in all patients.
Technical success was obtained in all patients in absence of major complications. In nine (15.5%) patients a mild, asymptomatic, disk space leakage of PMMA cement was observed, which required no additional therapy. A total of 32 (55.2%) lumbar and 26 (44.8%) thoracic levels were treated with 41 (70.7%) monolateral and 17 (29.3%) bilateral accesses.
During the 12-month follow-up period, one (1.7%) patient died and three (5.2%) patients were lost to follow-up (Fig. 1). The cause of the only death occurred was not related to the vertebral fracture (acute myocardial infarction).
A 12-month follow-up was thereby obtained in 54 (93.1%) patients (15 males, 39 females; mean age: 73.0 ± 8.87 years; range: 51–92). Thirteen (24.1%) of these patients had been already hospitalized at the time of treatment selection.
The mean hospitalization time in the patients completing the 12-month follow-up period was 2.46 ± 0.60 days.
Follow-up
A total of 140 patients (36 males and 104 females; mean age: 71.0 ± 8.24 years; range: 51–92 years) completed the 12-month follow-up period: 86 (61.4%) patients (21 males, 65 females; mean age: 69.7 ± 7.54 years; range: 56–90) in the CMT group and 54 (38.6%) patients (15 males, 39 females; mean age: 73.0 ± 8.87 years; range: 51–92) in the PVT group.
The results of the VAS, the ambulation scale and the ADL scale at 1 week and at 3 and 12 months from treatment selection, in patients who have completed the entire follow-up, are summarized in Table 1.
Table 1.
Results of the VAS, the ambulation scale and the ADL scale at 1 week and at 3 and 12 months
| Treatment | Pre-treament | 1 week | 3 months | 12 months |
|---|---|---|---|---|
| VAS mean ± SD (range) | ||||
| Medical therapy | 8.6 ± 0.87 (7–10) | 7.9 ± 0.67* (7–9) | 4.2 ± 1.27* (1–7) | 1.8 ± 1.14* (0–5) |
| Vertebroplasty | 8.7 ± 1.20 (6–10) | 1.1 ± 1.53*,** (0–6) | 0.9 ± 1.44*,** (0–5) | 1.1 ± 1.79* (0–5) |
| Ambulation mean ± SD (range) | ||||
| Medical therapy | 3.6 ± 0.89 (2–5) | 3.2 ± 0.81* (1–5) | 2.7 ± 0.80* (1–4) | 1.6 ± 0.62* (1–3) |
| Vertebroplasty | 3.6 ± 0.87 (3–5) | 1.2 ± 0.37*,** (1–2) | 1.2 ± 0.46*,** (1–3) | 1.4 ± 0.53* (1–3) |
| ADL mean ± SD (range) | ||||
| Medical therapy | 4.0 ± 0.75 (3–5) | 3.7 ± 0.79* (2–5) | 2.8 ± 0.78* (1–4) | 1.7 ± 0.60* (1–3) |
| Vertebroplasty | 3.9 ± 0.79 (2–5) | 1.2 ± 0.46*,** (1–3) | 1.4 ± 0.63*,** (1–3) | 1.5 ± 0.66* (1–3) |
* Significant difference with pre-treatment scores (P < 0.05; Wilcoxon signed rank test)
** Significant difference between groups (P < 0.05 Mann–Whitney U test)
Table 2.
Detailed analysis of the medical activities performed in the CMT and PVT groups
| Element | CMT group | PVT group |
|---|---|---|
| Analgesic therapy | In 86 (100%) patients: 5–15 (9.2 ± 3.70) mg × 2/day oxycodone (Oxycontin, Mundipharma Pharmaceutic Srl) and 50–200 (118.6 ± 54.48) mg × 2/day tramadol (Tradonal, Viatris) for 3 weeks In 46 (53.5%) patients: 5–15 (7.8 ± 3.07) mg × 2/day oxycodone, 50–200 (89.1 ± 46.52) mg × 2/day tramadol and 300–800 (458.7 ± 156.84) mg × 3/day gabapentin (Neurontin, Pfizer Italia) for 30 weeks In 30 (34.9%) patients with persisting pain: 5–15 (7.50 ± 2.50) mg × 2/day oxycodone, 50–200 mg (88.3 ± 40.17) × 2/die tramadol and 300–800 (413.3 ± 111.75) × 3 mg/day gabapentin for additional 19 weeks |
In 54 (100%) patients: 5–15 (9.7 ± 3.52) mg × 2/day oxycodone and 50–200 (127.8 ± 51.52) mg × 2/day tramadol for 1 week In 7 (13.0%) patients with persisting pain: 5–15 (6.4 ± 2.26) mg × 2/day oxycodone and 50–200 (57.4 ± 17.50) mg × 2/day tramadol for 2 weeks In 2 (3.7%) patients with new symptomatic vertebral fracture after 3 months: 5–15 (12.5 ± 2.5) mg × 2/day oxycodone and 50–200 (175.0 ± 25.00) mg × 2/day tramadol for 1 week |
| Hospitalization | Twenty (23.3%) patients hospitalized for a mean of 33.45 ± 6.06 days | Fifty-eight (100%) patients hospitalized for a mean of 2.46 ± 0.60 days Two (3.4%) patients with new symptomatic vertebral fractures hospitalized for a mean of 2.50 ± 0.50 days |
| Follow-up | At 1 and 3 weeks and at 3 and 12 months: physiatric consult At 1 week and at 1, 3 and 12 months: radiological consults At 1, 3 and 12 months full spine X-ray. At 3 months MRI of the involved spinal segment In 46 (53.5%) patients with persisting pain: physiatric consult at 8 months Additional specialist consults and radiological examinations in 3 (3.5%) patients with new symptomatic vertebral fracture, respectively, one at 3 months and two at 6 months At 1 week and at 1 and 3 months, physiatric and radiological consult At 1 and 3 months full spine X-ray At 3 months MRI of the involved spinal segment |
At 1 and 3 weeks and at 3 and 12 months: physiatric consult At 1 week and at 1, 3 and 12 months: radiological consult At 1, 3 and 12 months full spine X-ray At 3 months MRI of the involved spinal segment Additional specialist consults and radiological examinations in 2 (3.7%) patients new symptomatic vertebral fracture after 3 months At 1 week and at 1 and 3 months physiatric and radiological consult At 1 and 3 months full spine X-ray. At 3 months MRI of the involved spinal segment |
| Physical therapy | In 20 (23.3%) hospitalized patients: 30–40 sessions of massotherapy and rehabilitation gymnastic and 20 sessions of postural restoration and hydrokinesitherapy In 66 (76.7%) outpatients: 20 sessions of massotherapy, rehabilitation gymnastic, analgesic electrotherapy and magnetotherapy In 46 (53.5%) patients with persisting pain: 20 sessions of massotherapy, rehabilitation gymnastic, analgesic electrotherapy and magnetotherapy In 100 (100%) patients back brace: C35 Camp in 61 (70.9%) patients and MZ in 25 (29.1%) patients Additional physical therapy in 3 (3.5%) patients with new symptomatic vertebral fracture (not hospitalized) Twenty sessions of massotherapy, rehabilitation gymnastic, analgesic electrotherapy and magnetotherapy |
There were no statistically significant differences between the pre-treatment scores of the two groups. In both groups, a statistically significant reduction of the scores of the three scales was observed at 1 week and at 3 and 12 months. A significantly higher reduction of the three scores was observed in the PVT group at 1 week and at 3 months, while there was no statistically significant difference between the scores of the two groups at 12 months.
The detailed analysis of the medical activities performed after treatment selection is summarized in Table 2.
Table 3.
Detailed cost analysis of the medical activities performed in the CMT and PVT groups
| Period | CMT group | PVT group |
|---|---|---|
| 1 week | Hospitalization (daily tariffa = € 244.00/day): 20 patients → 34 160.00 € Outpatient drug therapy: 66 patients → 466.98 € Outpatient specialist consults: 66 patients → 1799.16 € Outpatient physical therapy: 66 patients → 7 046.16 € Back brace:86 patients → 21 500.00 € Total 1-week cost: 64 972.30 € Average 1-week patient cost: 755.49 ± 661.96 € (range: 391.10–1 958.00) |
Procedure (DRG 215b = 3 729.50 €): 54 patients → 177 093.00 € Outpatient drug therapy: 4.54 ± 0.60 days (of 1-week drug therapy started during hospitalization) for 54 patients → 247.85 € Outpatient specialist consults: 54 patients → 1472.04 € Total 1-week cost: 178 812.89 € Average 1-week patient cost: 3 311.35 ± 0.32 € (range: 3 310.80–3 311.81) |
| 3 months | 1st week total cost: 64 972.30 € Hospitalization (daily tariff = 244.00/day €): 26.45 days (total: 33.45 ± 6.06; range: 21–47) for 20 patients → 129 236.00 € Outpatient drug therapy: 14 days (of 3-week drug therapy) for 66 patients → 933.96 € 70 days (of 30-week drug therapy) for 27 patients → 3 664.52 € 57.55 ± 2.5 days (of 30-week drug therapy stared during hospitalization) for 19 patients → 2 120.09 € Outpatient specialist consults and radiological examinations: 3rd week control for 67 patients → 899.58 € 1st month control for 72 patients → 202.65 € 3rd month control for 86 patients → 18 600.08 € Outpatient physical therapy: 66 patients → 56 369.28 € 46 patients with persistent pain → 49 109.60 € Total 3-month cost: 326 108.06 € Average 3-month patient cost: 3 791.95 ± 3341.97 (range: 1 106.68–11 129.19) |
Total cost: 178 812.89 € Outpatient drug therapy: 14 days (of 2-week drug therapy) in 7 patients → 74.82 € Outpatient specialist consults and radiological examinations: 3rd week and 1st, 3rd month control for 54 patients → 23 358.24 € Total 3-month cost: 202 245.95 € Average 3-month patient cost: 3 745.30 ± 3.59 € (range: 3 743.36–3 755.06) |
| 12 months | Total 3-month cost: 326 108.06 € Outpatient drug therapy: 140 days (of 30-day drug therapy) for 27 patients → 7 329.04 € 140 days (of 30-week drug therapy stared during hospitalization) for 19 patients → 5 157.47 € 133 days (of 19-week drug therapy) in 30 patients → 7 736.19 € Outpatient specialist consults and radiological examinations: 8th month control in 46 patients with persisting pain → 626.98 € 12th month control in 86 patients → 18 600.08 € Three new vertebral fractures Additional outpatient specialist consults, radiological examinations and physical therapy: 1st and 3rd week and 1st and 3rd month control and physical therapy → 4 203.50 € Total 12-month cost: 369 761.32 € Average 12-month patient cost: 4 299.55 ± 3 211.53 € (range: 1322.96–11874.79) |
Total 3-month cost: 202 245.95 € Outpatient specialist consults and radiological examinations: 12th month control for 54 patients → 11 679.12 € Two new vertebral fractures Procedure (DRG 215 = 3 279.50 €): 2 patients → 6 559.00 € Outpatient drug therapy: 14 days (before admission) for 2 patients → 39.81 € 4.5 ± 0.5 days (after discharge) for 2 patients → 13.44 € Outpatient specialist consults and radiological examinations: 2 patients → 919.64 € Total 12-month cost: 221 456.96 € Average 12-month patient cost: 4 101.05 ± 755.41 € (range: 3 959.64–7 726.33) |
aDaily Tariff of the Santa Lucia Foundation in Rome, Italy
bNational Disease Related Groups 215 (Italian Health Ministry Decree 30/06/1997)
During follow-up, eight new amyelic vertebral fractures were observed, five in four (4.7%) patients of the CMT group (3 lumbar and 2 thoracic) and three in two (3.7%) patients of the PVT group (2 lumbar and 1 thoracic) completing follow-up. There was no statistically significant difference between the frequencies of new vertebral fractures in the two groups (P = 0.9). The new vertebral fractures were adjacent to the initial treated level in two cases in the CMT group and in one case in the PVT group. Five of these fractures were symptomatic, three fractures in three (3.5%) patients of the CMT group and two fractures in two (3.7%) patients of the PVT group.
In the CMT group, the three new symptomatic vertebral fractures occurred respectively 1 at 3 months and 2 at 6 months from treatment selection, in patients still under analgesic drug therapy for persisting pain. The same treatment protocol previously described for patients undergoing CMT was applied.
The two new symptomatic vertebral fractures of the PVT group occurred 3 months after treatment selection and were treated by PVT. The same treatment protocol previously described for patients undergoing PVT was applied.
Cost analysis
Average cost per patient at 1 week and at 3 and 12 months in the patients completing follow-up were respectively 755.49 ± 661.96 (391.10–1958.00), 3791.95 ± 3341.97 (1106.68–11129.19) and 4299.55 ± 3211.53 (1322.96–11874.79) euros for the CMT group and 3311.35 ± 0.32 (3310.80–3311.81), 3745.30 ± 3.59 (3743.36–3755.06) and 4101.05 ± 755.41 (3959.64–7726.33) euros for the PVT group.
The large standard deviations of the mean costs of the CMT group are attributable to the large difference existing between the costs for hospitalized patients and outpatients.
The detailed cost analysis in the CMT and PVT groups is summarized in Table 3.
Table 4.
Cost-effectiveness in the CMT and PVT group, with regards to the VAS and the ambulation and ADL scales at 1 week and at 3 and 12 months from treatment selection
| Type of treatment | 1 week | 3 months | 12 months |
|---|---|---|---|
| Cost-effectiveness VAS mean ± SD (range) | |||
| Medical therapy | 1079.27 ± 951.20*(195.55–1958.00) | 861.810 ± 639.94(122.96–1589.88) | 632.29 ± 528.32(165.37–1484.35) |
| Vertebroplasty | 435.70 ± 6.47*(413.85–473.12) | 480.17 ± 14.36(416.14–536.44) | 539.61 ± 39.23(439.96–772.63) |
| Cost-effectiveness ambulation mean ± SD (range) | |||
| Medical therapy | 1888.73 ± 1664.60*(391.10-N/A) | 4213.28 ± 3764.88*(553.34–11129.19) | 2149.78 ± 2013.23(440.99–5937.40) |
| Vertebroplasty | 1379.73 ± 50.36*(1103.60–1655.91) | 1560.54 ± 62.85*(1247.79–1877.53) | 1864.11 ± 84.71(1319.88–2575.44) |
| Cost-effectiveness ADL mean ± SD (range) | |||
| Medical therapy | 2518.30 ± 2219.47*(391.10-N/A) | 3159.96 ± 2615.63(1106.68–11129.19) | 1869.37 ± 1134.28(440.99–3958.26) |
| Vertebroplasty | 1226.43 ± 65.49*(827.70–1655.40) | 1498.12 ± 54.18(1247.79–1877.53) | 1708.77 ± 90.03(1319.88–2575.44) |
* Significant difference between groups (P < 0.05; Mann–Whitney U test)
N/A Data not available as one or more patients presented no reduction of the scale’s value
Cost-effectiveness
At 1 week from treatment selection, PVT resulted significantly more cost-effective than CMT with regards to the VAS, the ambulation and ADL scales. At 3 months PVT was more cost-effective than CMT with regards to the three scales, however, the difference was statistically significant only with regards to the ambulation scale. At 12 months, PVT remained more cost-effective than CMT with regards to the three scales, however, the difference was not significant.
The cost-effectiveness data for the CMT and PVT groups at 1 week and at 3 and 12 months from treatment selection are summarized in Table 4.
Discussion
Osteoporotic vertebral fracture is a highly invalidating disease that is associated to an increased mortality rate, reaching 10% during the 5 years which follow the fracture [3, 16, 17].
In Europe, the frequency of this disease in subjects older than 50 years, is approximately 12% [13], while it is estimated that approximately 200 million adults are at risk of osteoporotic vertebral fracture worldwide [2]. Patients with vertebral fracture, furthermore, show a five-fold increase of the risk of new fractures in the adjacent vertebral bodies [3, 15].
In the European Union, vertebral fractures are responsible of 8% of the hospital costs of all osteoporotic fractures with an estimated yearly expense of 377 million euros. The hospital cost of a vertebral fracture treated by CMT is approximately 63% of the mean hospital cost of a femoral fracture [6].
A global evaluation approach to the assessment of the validity of a treatment cannot prescind from the evaluation of its costs and its cost-effectiveness.
The efficacy of PVT, with regards to pain and function, in patients with acute vertebral fractures has been amply described in literature [5, 11, 12].
There exists only one study in literature comparing the efficacy of treatment in a group of patients treated by PVT with that of a control group treated by CMT [4]. According to this study by Diamond et al., PVT, differently from CMT, is associated to a significant improvement of pain 24 h after the procedure. CMT is associated to a significant improvement of pain only after 6 weeks, however, the efficacy of the two treatments is comparable (absence of statistically significant differences) only after 12 months. The authors observed similar results for function with a statistically significant improvement after 24 h only in patients treated by PVT, while the data between the two treatment groups became similar after 6 weeks.
Our results show that the treatment of symptomatic acute amyelic osteoporotic vertebral fractures by PVT is associated to an early drastic, and statistically significant, reduction of pain and improvement of ambulation and ability to perform activities of daily living. These results are substantially in accordance with data reported in literature [5, 7, 9, 11, 12].
Similarly to the study of Diamond et al., our study demonstrates a significantly higher improvement of pain and functionality in the group of patients treated by PVT on the short-term (at 1 week and at 3 months) and comparable result in the two groups on the long-term (at 12 months).
In our series, PVT resulted more cost-effective than CMT regardless of the scale used to evaluate effectiveness. However, the difference between the cost-effectiveness ratios of the two treatment alternatives was statistically significant with regards to all scales only at 1 week, whereas at 3 months it was statistically significant only for the ambulation scale.
The factors which had mostly influenced costs in the CMT group were the days of hospitalization, physical therapy and the back brace. On the other hand, in the PVT group, costs were mainly affected by the DRG of the procedure.
In our study, three deaths occurred in the group treated by CMT were directly relatable to the vertebral fracture. Moreover, there was no substantial difference between the rates of vertebral fracture recurrence between the two groups.
We may conclude that from a clinical point of view, the early and high effectiveness, the low incidence of major complications and the reduced mortality rate validate the use of PVT. On the other hand, the lower cost-effectiveness ratio of PVT on the short-term and its comparable cost-effectiveness ratio with that of CMT on the long-term validate the use of this procedure also from an economic point of view.
According to our knowledge, this is the first non-randomized retrospective study evaluating the cost-effectiveness of PVT compared to CMT.
Limitations to our study are its single-center nature and the non-randomized patient enrollment. Multi-centric randomized trials enrolling larger patient populations are necessary to confirm our results.
Percutaneous vertebroplasty should be considered as a valid therapeutic option in symptomatic acute amyelic osteoporotic vertebral fractures with refractory pain after a short period of analgesic drug therapy.
Footnotes
Daily Tariff of the Santa Lucia Foundation in Rome, Italy.
National Disease Related Groups 215 (Italian Health Ministry Decree 30/06/1997).
References
- 1.Barth RW, Lane JM. Osteoporosis. Orthop Clin North Am. 1998;19:845–858. [PubMed] [Google Scholar]
- 2.Cooper C. Epidemiology of osteoporosis. Osteoporosis Int. 1999;9:S2–S8. doi: 10.1007/PL00004156. [DOI] [PubMed] [Google Scholar]
- 3.Coumans JV, Reinhardt MK, Lieberman IH. Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg. 2003;99:44–50. doi: 10.3171/jns.2003.99.1.0044. [DOI] [PubMed] [Google Scholar]
- 4.Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med. 2003;114:257–265. doi: 10.1016/S0002-9343(02)01524-3. [DOI] [PubMed] [Google Scholar]
- 5.Evans AJ, Jensen ME, Kip KE, et al. Vertebral compression fractures: pain reduction and improvements in functional mobility after percutaneous polymethylmethacrylate vertebroplasty: retrospective report of 245 scases. Radiology. 2003;226:366–372. doi: 10.1148/radiol.2262010906. [DOI] [PubMed] [Google Scholar]
- 6.Finnern HW, Sykes DP. The hospital cost of vertebral fractures in the EU: estimates using national datasets. Osteoporos Int. 2003;14:429–436. doi: 10.1007/s00198-003-1395-2. [DOI] [PubMed] [Google Scholar]
- 7.Grados F, Depriester C, Cayrolle G, et al. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology. 2000;39:1410–1414. doi: 10.1093/rheumatology/39.12.1410. [DOI] [PubMed] [Google Scholar]
- 8.Kado DM, Browner WS, Palermo L, Al E. Vertebral fractures and mortality in older women: the study of osteoporotic fracture. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 9.Legroux-Gerot I, Lormeau C, Boutry N, et al. Long-term follow up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol. 2004;23:310–317. doi: 10.1007/s10067-004-0914-7. [DOI] [PubMed] [Google Scholar]
- 10.Masala S, Fiori R, Massari F, Simonetti G. Vertebroplasty and kyphoplasty: new equipment for malignant vertebral fractures treatment. J Exp Clin Cancer Res. 2003;22:75–79. [PubMed] [Google Scholar]
- 11.McGraw JK, Lippert JA, Minkus KD, et al. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol. 2002;13:883–886. doi: 10.1016/S1051-0443(07)61770-9. [DOI] [PubMed] [Google Scholar]
- 12.McKiernan F, Faciszewski T, Jensen R. Quality of life following vertebroplasty. J Bone Joint Surg Am. 2004;86:2600–2606. doi: 10.2106/00004623-200412000-00003. [DOI] [PubMed] [Google Scholar]
- 13.O’Neill TW, Felsenberg D, Varlow J, et al. The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res. 1999;11:1010–1018. doi: 10.1002/jbmr.5650110719. [DOI] [PubMed] [Google Scholar]
- 14.Ross PD. Clinical consequences of vertebral fractures. Am J Med. 1997;103:S30–S43. doi: 10.1016/S0002-9343(97)90025-5. [DOI] [PubMed] [Google Scholar]
- 15.Silverman SL. The clinical consequences of vertebral compression fracture. Bone. 1992;13:S27–31. doi: 10.1016/8756-3282(92)90193-Z. [DOI] [PubMed] [Google Scholar]
- 16.Stallmeyer MJ, Zoarski GH, Obuchowski AM. Optimizing patient selection in percutaneous vertebroplasty. J Vasc Interv Radiol. 2003;14:683–696. doi: 10.1097/01.rvi.0000064859.87207.fa. [DOI] [PubMed] [Google Scholar]
- 17.Watts NB. Osteoporotic vertebral fractures. Neurosurg Focus. 2001;10:1–3. doi: 10.3171/foc.2001.10.4.13. [DOI] [PubMed] [Google Scholar]
- 18.Wu SS, Lachmann E, Nagler W. Current medical, rehabilitation, and surgical management of vertebral compression fractures. J Womens Health. 2003;12:17–26. doi: 10.1089/154099903321154103. [DOI] [PubMed] [Google Scholar]