Abstract
The determination of skeletal age is essential in the management of patients with scoliosis. One of the most frequently used techniques to determine skeletal maturity is the method described by Risser. However, repeated X-ray exposure in the follow-up examinations of scoliosis patients may increase the risk of cancer. We compared conventional radiological evaluation of the Risser grade with ultrasound evaluation. For scoliosis patients routine application of ultrasound in the follow-up examinations may significantly reduce radiation exposure. 46 adolescent idiopathic scoliosis patients (median age, 14.5 years) were investigated. Sonographic and radiographic assessment of Risser sign was carried out by two independent senior staff skeletal radiologists. Agreement of Risser Grade between the two diagnostic methods was determined by Kappa statistics. Coefficients <0.21, 0.21–0.40, 0.41–0.60, 0.61–0.80, and >0.80 were rated as poor, fair, moderate, good, and very good agreement. For Risser Grades I–III 100% agreement was found between the two methods. Disagreement between radiographic and sonographic evaluation was found in Risser Grades IV and V. In five patients, X-ray evaluation yielded Risser Grade V while ultrasound showed Risser Grade IV. In one patient, radiographic examination resulted in Risser Grade IV while Grade V was detected in ultrasound. Overall, the Kappa value showed very good agreement between the two diagnostic methods. Our findings suggest that ultrasound can be applied as an alternative method to X-ray evaluation in Risser Grade determination. It should be routinely used in clinical practice to reduce the patients exposure to radiation.
Keywords: Skeletal age, Risser grade, Ultrasound asessment, Adolescent idiopathic scoliosis
Introduction
The accurate assessment of skeletal maturity is crucial in the management of patients with adolescent idiopathic scoliosis (AIS) when deciding whether conservative or surgical treatment is indicated. As the chronologic age of the patient is assumed to be inaccurate [14, 16, 18, 22, 35] several parameters have been proposed in maturity determination, such as the rip apophysis, timing of menarche, peak height velocity, assessment of the olecranon, calendar and skeletal age of the hand or wrist, the Risser sign, and electromyography [8, 9, 14–16, 22, 23, 25, 26, 28, 31, 40]. Evaluating Risser Grades requires plain radiographs of the iliac apophysis. The combined radiation dose for a standard posterioanterior and lateral standing radiograph is approximately 1.0 mSv (milli Sievert) [1], which is among the highest in diagnostic radiography. During adolescence the patients mammary glands are particularly sensitive to radiation [10, 13]. Exposure to radiation should therefore be reduced to a minimum. A reduction of the radiation dose may be achieved by using ultrasound devices to estimate of the skeletal age.
The purpose of this study was to determine the accuracy of ultrasound evaluation of the Risser Grade as compared to plain radiography in patients with adolescent idiopathic scoliosis.
Methods
From August 2001 to July 2005, 46 patients (36 female, 8 male) with idiopathic adolescent scoliosis who had undergone iliac apophysis radiography for skeletal age determination according to Risser were enrolled into the study. The patients had a median age of 14.5 years (range, 7–17 years). Standard anteriorposterior radiographs of the iliac crest apophysis were made using a digital bucky system (Philips Digital Diagnost, Philips Medical Systems, Hamburg, Germany). The system is based on a 43 × 43 cm flat planel detector provided by Trixell (Moirans, France) which consists of a cesium iodide scintillation layer mounted on a 2,94 × 13,021-pixel readout matrix made of amorphous silicon. Each of these elements is connected to a tiny switch for readout. The detected signals are amplified and multiplexed and then transferred to a post processing workstation.
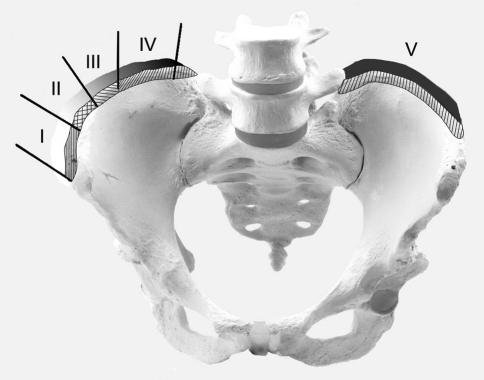
Subsequently, Risser Grade (0–V) (Fig. 1) was measured [22]. The Risser sign was defined by the extent of ossification of the apophysis from the anterolateral to the posteromedial aspect of the iliac crest. The absence of ossification of the iliac crest was defined as Risser Grade 0. Ossification within the first quarter was defined as Risser Grade I (0–25%). Ossification extending the second quarter of the iliac crest was recorded as Risser Grade II (25–50%). Risser Grade III represents an ossification progress into the third quarter (50–75%) while Grade IV was defined as an ossification into the fourth quarter of the crest (≥75%). Complete fusion of the apophysis to the ilium was rated as Risser Grade V. A senior staff radiologist evaluated all iliac apophysis radiographs and determined the Risser sign as defined above.
Fig. 1.
Risser Grades I–V
On the same day, sonographic examinations of the iliac apophysis were performed on an ATL HDI-5000 ultrasound scanner (Advanced Technologicaly Labor, Bothell, Washington) using a 12-MHz linear array. The patients were placed in a lateral decubitus position. The ossification center of the apophysis was scanned starting at the anterolateral aspect of the iliac crest and going on to the posteromedial aspect. The grades of the Risser sign (0–V) were assessed as defined above. The ultrasound examinations were carried out by another senior staff skeletal radiologist. Ultrasound evaluation was performed without knowledge of the radiographic results. The results of ultrasound assessment were compared to the radiographic findings. Plain digital radiography was taken as the gold standard to assess the Risser Grade.
Statistical methods
Agreement in Risser grading between the two diagnostic methods was determined by Kappa statistics. The coefficients <0.21, 0.21–0.40, 0.41–0.60, 0.61–0.80, and >0.80 were considered poor, fair, moderate, good, and very good agreement [2].
Results
Ultrasound and radiologic data were available for all patients. The results of radiographic and ultrasound evaluation are shown in Table 1. 100% agreement between the two examination techniques was found in 40 of 46 patients. According to the ultrasound evaluation, thirteen patients were classified as Risser Grade 0, three as Risser Grade I, six as Risser Grade II, three as Risser Grade III, eleven as Risser Grade IV, and ten as Risser Grade V. All patients sonographically classified as Risser Grades I–III showed identical radiographic Risser Grades. Disagreement between radiographic and ultrasound examination was observed in Risser Grades IV and V. In five patients, a radiographically assessed Risser Grade V was determined as Grade IV with ultrasound. In one patient, a radiographical Risser Grade IV was assessed Grade V with ultrasound. The Kappa value showed very good agreement between the two diagnostic methods. (κ = 0.835, P < 0.001).
Table 1.
Agreement matrix of two diagnostic methods and six Risser Grades
| Digital radiography | Sonography | ||||||
|---|---|---|---|---|---|---|---|
| Risser Grade | 0 | I | II | III | IV | V | Total |
| 0 | 13 | 0 | 0 | 0 | 0 | 0 | 13 |
| I | 0 | 3 | 0 | 0 | 0 | 0 | 3 |
| II | 0 | 0 | 6 | 0 | 0 | 0 | 6 |
| III | 0 | 0 | 0 | 3 | 0 | 0 | 3 |
| IV | 0 | 0 | 0 | 0 | 6 | 1 | 7 |
| V | 0 | 0 | 0 | 0 | 5 | 9 | 14 |
| Total | 13 | 3 | 6 | 3 | 11 | 10 | 46 |
6 = 0.835, P < 0.001
Discussion
Skeletal maturity needs to be considered when treating patients with scoliosis. Various indicators for assessing maturity and spinal growth have been described in literature, such as chronologic age [16, 23, 31, 40], the rip apophysis [14], the status of opened or closed triradiate cartilage [16], timing of menarche [14, 23], peak height velocity [22, 32, 34], the assessment of the olecranon [8], calendar and skeletal age of the hand or wrist [12, 14], the Risser sign [15, 28], and electromyography [9].
The stage of ossification of the iliac apophysis (Risser sign) is the most commonly used method of determining skeletal maturation in patients with idiopathic scoliosis [4, 5, 11, 17, 19–21, 27, 30, 31, 37–39]. Risser Grade determination is a simple and readily available method and therefore it is frequently used. However, radiation exposure is a significant problem in these young patients. The patients mammary glands are directly exposed to ionizing radiation. The combined radiation dose for a standard posterioanterior and lateral standing is approximately 1.0 mSv and among the highest in diagnostic radiography [1]. Due to the necessity of frequent follow-up radiographs, the cumulative radiation dose may become significant, which has been associated with a higher risk of developing breast cancer [10, 13].
Various studies have been published highlighting this problem. Izumi [15] compared Risser Grade determination performed on an AP X-ray view with posteroanterior (PA) radiographs. Since the incidence of breast cancer has been reported to be higher in scoliotic patients, he tried to introduce the PA view of the pelvis in the routine follow-up of patients with scoliosis. He concluded that the appearance of the iliac apophysis on the PA radiographs cannot be established as a reliable indicator of skeletal bone age because 42% of the PA views produced a contorted image of the iliac apophysis without visualizing the medial and lateral aspects of the apophysis.
Since it was assumed that the entire excursion of the iliac crest could be imaged on AP oblique views, Shuren et al. [33] compared the iliac apophysis in PA and AP oblique views in 34 patients. The authors did not find any significant differences between Risser Grade assessed on PA and AP oblique, but pointed out that the differentiation between Risser IV and V may become difficult on the PA radiographs since the ilium may overlap the apophysis.
Only few studies have mentioned sonography as an image-guided alternative to examine bone age [3, 6, 7, 24, 36]. Wagner et al. [36] described a high correlation between sonographic and radiological Risser Grade evaluation. Wagner concluded that the sonographic differentiation between Risser Grades III and IV to be demanding, especially in overweight patients. In this study, an overall accuracy of 89.2% (25 of 28 measurements) was achieved. However, Wagner’s study group was smaller than the current and the ultrasound equipment was less sophisticated. In addition, radiological equipment has improved considerably, particularly with respect to magnification capacities and resolution. Furthermore, additional anatomical settings for ultrasound are now available.
Castriota-Scanderbeg et al. [7] investigated sonographic bone age determination in patients with proven or suspected growth disorder by measuring the thickness of the articular cartilage of the femoral head and compared it with the Greulich and Peyle and the Tanner–Whitehouse method. His ultrasound method agreed the least (difference in 4.19–5.13 years) with the other methods. The ultrasound method provided 85.8% (ultrasound vs. Tanner–Whitehouse) to 91.3% (ultrasound vs. Greulich and Peyle) concordant results in recognizing differences between skeletal and chronological age, and showed a 72.5% sensivity and 56.8% specificity. As a consequence of the inaccuracy of Castriota-Scanderbegs assessments, he suggested not using ultrasound evaluation in routine diagnostics.
Mentzel [24] performed a study to compare the Greulich and Pyle method with the sonographic evaluation of the same hand. He applied a sonographic method evaluating the relationship between the velocity of sound passing through the distal radial and ulna epiphysis, and growth, using gender- and ethnicity-based algorithms. The averaged accuracy (i.e., absolute difference in years between the Greulich an Pyle method and the ultrasound method) for the left hand was 1.0 ± 0.8 years and for the distal radius was 0.8 ± 0.7 for boys and 0.9 ± 0.7 for girls. Moreover, Mentzel’s technique requires a special ultrasound device.
The sonography-based techniques such as the ultrasonographic version of the Greulich and Pyle atlas demonstrated by Bilgili [3] are available, but they are time consuming (average time; 3 min, 45 s) and may not be useful in routine. Bilgili compared hand and wrist plain radiographs and compared the findings with sonographic evaluation. He reported a correlation of 71.1% for boys and of 65.5% for girls. However, Sanders et al. [29, 30] confirmed that morphological changes in the wrist, radius and ulna did not correlate with curve progression during peak height velocity.
Shortcomings of the current study are that there was only one observer per method. Because the sonographic evaluation is a dynamic assessment technique, multiple evaluations would be needed to get an appropriate result. A second or even third investigation would be very straining for adolescent patients and was therefore not performed. Another shortcoming is that a three-dimensional method (sonographic evaluation) is compared with a one dimensional method (conventional X-rays). However, the aim of our study was to investigate the comparison between two methods with different radiation doses. Nowadays, with modern digital technology, a total visualization of the spine and pelvis can be obtained without the need of extra images. In addition, new X-ray machines are available to illustrate the Risser sign with a radiation of 9–10% compared to a standard radiation dose.
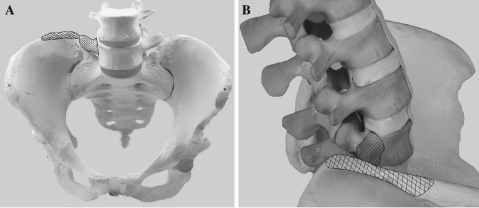
In our study, 100% agreement of the radiological and ultrasound assessments of the Risser Sign was found for Risser Grades I–III using a standard ultrasound device. The disagreement for Risser Grades IV and V may be explained by the overlap of the transverse process of the fifth lumbar vertebra and the medial iliac apophysis in ultrasound. By using ultrasound it was different in some patients to already distinguish between a medially ossified iliac crest (Risser Grade IV) and the bony structure of the transverse process of the fifth lumbar vertebra. (Fig. 2) Therefore, a Risser Grade IV without a complete ossification of the medial aspect of the iliac crest may be falsely noted as Risser Grade V.
Fig. 2.
a Picture showing the transverse process of the fifth lumbar vertebra (striped marking) in relation to the posteromedial iliac apophysis (checkered marking) from anterior-posterior. b Picture showing the transverse process of the fifth lumbar vertebra (striped marking) in relation to the posteromedial iliac apophysis (checkered marking) from lateral
In conclusion, ultrasound evaluation of the Risser Grade has proved to be an accurate technique compared to radiographic techniques. The technique is cheap, easy to use, fast and easy accessibility. Routine use of this ultrasound method may significantly reduce radiation exposure for patients followed for scoliosis.
References
- 1.Adam CJIM, Harvey JR, Askin GN. Variability in Cobb angle measurements using reformatted computerized tomography scans. Spine. 2005;30:1664–1669. doi: 10.1097/01.brs.0000169449.68870.f8. [DOI] [PubMed] [Google Scholar]
- 2.Altman D. Practical statistics for medical research. Boca Raton: Chapman & Hall/CRC; 1991. [Google Scholar]
- 3.Bilgili YHS, Kara SA, Sanli C, Erdal HH, Altinok D. Accuracy of skeletal age assessment in children from birth to 6 years of age with the ultrasonographic version of the Greulich–Pyle atlas. J Ultrasound Med. 2003;22:683–690. doi: 10.7863/jum.2003.22.7.683. [DOI] [PubMed] [Google Scholar]
- 4.Bjerkreim ISH, Brox JI. Idiopathic scoliosis treated with Cotrel-Dubousset instrumentation: evaluation 10 years after surgery. Spine. 2007;32:2103–2110. doi: 10.1097/BRS.0b013e318145a54a. [DOI] [PubMed] [Google Scholar]
- 5.Bulthuis GJVA, Nijenbanning G. Clinical effect of continuous corrective force delivery in the non-operative treatment of idiopathic scoliosis: a prospective cohort study of the TriaC-brace. Eur Spine J. 2008;17:231–239. doi: 10.1007/s00586-007-0513-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castriota-Scanderbeg ADMV. Ultrasound of femoral head cartilage: a new method of assessing bone age. Skeletal Radiol. 1995;24:217–420. doi: 10.1007/BF00228922. [DOI] [PubMed] [Google Scholar]
- 7.Castriota-Scanderbeg ASM, Emberti-Gialloreti L, Fraracci L. Skeletal age assessment in children and young adults: comparison between a newly developed sonographic method and conventional methods. Skeletal Radiol. 1998;27:271–277. doi: 10.1007/s002560050380. [DOI] [PubMed] [Google Scholar]
- 8.Charles YP, Canavese DA, Daures F. Skeletal age assessment from the olecranon for idiopathic scoliosis at Risser Grade 0. J Bone Joint Surg Am. 2007;89:2737–2744. doi: 10.2106/JBJS.G.00124. [DOI] [PubMed] [Google Scholar]
- 9.Cheung JVA, Halbertsma JPK, Maurits NM, Sluiter WJ, Cool JC, Horn JR. The relation between electromyography and growth velocity of the spine in the evaluation of curve progression in idiopathic scoliosis. Spine. 2004;29:1011–1016. doi: 10.1097/00007632-200405010-00012. [DOI] [PubMed] [Google Scholar]
- 10.Smet AAFS, Asher MA. A method for minimizing the radiation exposure from scoliosis radiographs. J Bone Joint Surg Am. 1981;63:156–158. [PubMed] [Google Scholar]
- 11.Dolan LAWS. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine. 2007;32:S91–S100. doi: 10.1097/BRS.0b013e318134ead9. [DOI] [PubMed] [Google Scholar]
- 12.Greulich WPS. Radiographic atlas of skeletal development of the hand and wrist. 2. Stanford: Stanford University Press; 1959. [Google Scholar]
- 13.Hoffman DALJ, Morin MM, Visscher W, Harris BS, 3rd, Boice JD., Jr Breast cancer in women with scoliosis exposed to multiple diagnostic X-rays. J Natl Cancer Inst. 1989;81:1307–1312. doi: 10.1093/jnci/81.17.1307. [DOI] [PubMed] [Google Scholar]
- 14.Hoppenfeld SLB, Murthy V, Yun G. The rip epiphysis and other growth centers as indicators of the end of spinal growth. Spine. 2003;29:47–50. doi: 10.1097/01.BRS.0000103941.50129.66. [DOI] [PubMed] [Google Scholar]
- 15.Izumi Y. The accuracy of Risser staging. Spine. 1995;20:1868–1871. doi: 10.1097/00007632-199509000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Karol LAJC, Browne RH, Madison M. Progression of the curve in boys who have idiopathic scoliosis. J Bone Joint Surg Am. 1993;75:1804–1810. doi: 10.2106/00004623-199312000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Kim YJLL, Bridwell KH, Cheh G, Whorton J, Sides B. Prospective pulmonary function comparison following posterior segmental spinal instrumentation and fusion of adolescent idiopathic scoliosis: is there a relationship between major thoracic curve correction and pulmonary function test improvement? Spine. 2007;32:2685–2693. doi: 10.1097/BRS.0b013e318074c3ce. [DOI] [PubMed] [Google Scholar]
- 18.Kohashi Y, Oga M, Sugioka Y (1996) A new method using top views of the spine to predict the progression of curves in idiopathic scoliosis during growth. Spine 21:212–217. doi:10.1097/00007632-199601150-00010 [DOI] [PubMed]
- 19.Kotwicki TDJ, Padovani JP. Correction of flexible thoracic scoliosis below 65 degrees—a radiological comparison of anterior versus posterior segmental instrumentation applied to similar curves. Eur Spine J. 2006;15:972–981. doi: 10.1007/s00586-005-0991-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuklo TPB, Polly D, O’Brian F, Schroeder T, Lenke L. Reliability analysis for manual adolescent idiopathic scoliosis measurements. Spine. 2005;30:444–454. doi: 10.1097/01.brs.0000153702.99342.9c. [DOI] [PubMed] [Google Scholar]
- 21.Kuklo TRPB, Schroeder TM, O’Brien MF. Comparison of manual and digital measurements in adolescent idiopathic scoliosis. Spine. 2006;31:1240–1246. doi: 10.1097/01.brs.0000217774.13433.a7. [DOI] [PubMed] [Google Scholar]
- 22.Little DGSK, Katz D, Herring JA. Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J Bone Joint Surg Am. 2000;82:685–693. doi: 10.2106/00004623-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Lonstein JCJ. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66:1061–1071. [PubMed] [Google Scholar]
- 24.Mentzel HJVC, Eulenstein M, Schwartz T, Vogt S, Böttcher J, Yaniv I, et al. Assessment of skeletal age at the wrist in children with a new ultrasound device. Pediatr Radiol. 2005;35:429–433. doi: 10.1007/s00247-004-1385-3. [DOI] [PubMed] [Google Scholar]
- 25.Noordeen MHHF, Edgar MA, Pringle J. Spinal growth and a histological evaluation of the Risser grade in idiopathic scoliosis. Spine. 1999;24:535–538. doi: 10.1097/00007632-199903150-00006. [DOI] [PubMed] [Google Scholar]
- 26.Peterson LNA. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. J Bone Joint Surg Am. 1995;77:823–827. doi: 10.2106/00004623-199506000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Richards BSBR, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30:2068–2075. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 28.Risser J. The Iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop Relat Res. 1958;11:111–119. [PubMed] [Google Scholar]
- 29.Sanders JOBR, Cooney TE, Finegold DN, McConnell SJ. Correlates of the peak high velocity in girls with idiopathic scoliosis. Spine. 2006;31:2289–2295. doi: 10.1097/01.brs.0000236844.41595.26. [DOI] [PubMed] [Google Scholar]
- 30.Sanders JOBR, McConnell SJ, Margraf SA, Cooney TE. Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am. 2007;89:64–73. doi: 10.2106/JBJS.F.00067. [DOI] [PubMed] [Google Scholar]
- 31.Sanders JOHJ, Brown RH. Posterior arthrodesis and instrumentation in the immature spine in idiopathic scoliosis. J Bone Joint Surg Am. 1995;77:39–45. doi: 10.2106/00004623-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Sanders JOLD, Richards BS. Prediction of the crankshaft phenomenon by peak height velocity. Spine. 1997;22:1352–1356. doi: 10.1097/00007632-199706150-00013. [DOI] [PubMed] [Google Scholar]
- 33.Shuren NKJ, Emans J, Rand F. Reevaluation of the use of the Risser sign in idiopathic scoliosis. Spine. 1991;17:359–361. doi: 10.1097/00007632-199203000-00020. [DOI] [PubMed] [Google Scholar]
- 34.Song KMLD. Peak high velocity as a maturity indicator for males with idiopathic scoliosis. J Pediatr Orthop. 2000;20:286–288. doi: 10.1097/00004694-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Suh PBMEG. Idiopathic scoliosis in males: a natural history study. Spine. 1997;22:1352–1357. doi: 10.1097/00007632-199706150-00013. [DOI] [PubMed] [Google Scholar]
- 36.Wagner UADV, Schmitt O (1995) Determination of skeletal maturity by ultrasound: a preliminary report. Skeletal Radiol 24:417–420. doi:10.1007/BF00941236 [DOI] [PubMed]
- 37.Wong HKHJ, Rajan U, Chia HP. Idiopathic scoliosis in Singapore schoolchildren: a prevalence study 15 years into the screening program. Spine. 2005;30:1188–1196. doi: 10.1097/01.brs.0000162280.95076.bb. [DOI] [PubMed] [Google Scholar]
- 38.Wu JQY, Zhang L, Sun Q, Qiu X, He Y. Association of estrogen receptor gene polymorphisms with susceptibility to adolescent idiopathic scoliosis. Spine. 2006;31:1131–1136. doi: 10.1097/01.brs.0000216603.91330.6f. [DOI] [PubMed] [Google Scholar]
- 39.Yrjönen TYM, Schlenzka D, Poussa M. Results of brace treatment of adolescent idiopathic scoliosis in boys compared with girls: a retrospective study of 102 patients treated with the Boston brace. Eur Spine J. 2007;16:393–397. doi: 10.1007/s00586-006-0167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zapussis ALJJ. The iliac apophysis and the evolution of curves in scoliosis. J Bone Joint Surg Br. 1958;40:442–453. doi: 10.1302/0301-620X.40B3.442. [DOI] [PubMed] [Google Scholar]