Abstract
Intensive group training using principles of graded activity has been proven to be effective in occupational care for workers with chronic low back pain. Objective of the study was to compare the effects of an intensive group training protocol aimed at returning to normal daily activities and guideline physiotherapy for primary care patients with non-specific chronic low back pain. The study was designed as pragmatic randomised controlled trial with a setup of 105 primary care physiotherapists in 49 practices and 114 patients with non-specific low back pain of more than 12 weeks duration participated in the study. In the intensive group training protocol exercise therapy, back school and operant-conditioning behavioural principles are combined. Patients were treated during 10 individual sessions along 20 group sessions. Usual care consisted of physiotherapy according to the Dutch guidelines for Low Back Pain. Main outcome measures were functional disability (Roland Morris disability questionnaire), pain intensity, perceived recovery and sick leave because of low back pain assessed at baseline and after 6, 13, 26 and 52 weeks. Both an intention-to-treat analysis and a per-protocol analysis were performed. Multilevel analysis did not show significant differences between both treatment groups on any outcome measures during the complete follow-up period, with one exception. After 26 weeks the protocol group showed more reduction in pain intensity than the guideline group, but this difference was absent after 52 weeks. We finally conclude that an intensive group training protocol was not more effective than usual physiotherapy for chronic low back pain.
Keywords: Low back pain, Physiotherapy, Randomized controlled trial, Graded activity, Group training
Introduction
Non-specific low back pain is one of the most common and expensive disorders in industrialised countries. The 1-year prevalence is estimated at 44% in the general population [17]. Contrary to common belief, current literature suggests that the proportion of patients with persistent low back pain after 1 year is larger than 10% [7, 13, 21]. Therefore, there is a great need to identify efficient interventions for chronic low back pain patients. Systematic Cochrane reviews of the effectiveness of exercise therapy, behavioural therapy and back school programs have shown that these interventions are promising treatment options. [6, 8, 16]. The Low Back Pain Guideline of the Royal Dutch College for Physiotherapy for low back pain recommends adequate information and an active approach including behavioural principles [1]. As physiotherapists do not have specific knowledge of behavioural principles or are not specifically trained to provide behavioural therapy, physiotherapists in Amsterdam developed an intensive group training protocol based on the guideline. In two randomised controlled trials (RCTs) the effects of a behaviour-orientated physical exercise program were studied in occupational health care [12, 19]. The promising results of these studies led to the question whether a similar intervention would be as effective in a primary physiotherapy care setting. The aim of the current study was to compare the effectiveness of an intensive group training protocol to guideline physiotherapy in chronic low back pain patients. An extensive description of the design of this study has been reported elsewhere [22]. Although we initially focussed on patients with sub-acute and chronic low back pain, after a one year inclusion period only eight patients with sub-acute low back pain were recruited for this study. It was therefore decided to focus only on patients with chronic complaints.
Methods
Participants
Participating physiotherapists were asked to include patients with chronic low back pain. Inclusion criteria were: age 18–65 years, a new episode of non-specific low back pain lasting more than 12 weeks, inability to resume daily activities in the last 3 weeks, health insurance with one insurance company. This was the only company willing to reimburse the intensive group training protocol at the beginning of the trial. This company is one of the largest health insurance companies and the population is representative of the general population in The Netherlands. Exclusion criteria were specific low back pain, advice by general practitioner not to perform physically straining activities, pregnancy, pelvic girdle pain, legal involvement related to either low back pain or related to work disability.
Randomisation
Patients were randomly allocated to either the protocol group or guideline group. Nine local research centres were set up. For each research centre a randomisation list was prepared and permuted blocks of 4 patients were made to ensure equal distribution of patients for each research centre. An independent statistician (DLK) generated the randomisation lists, using series of random numbers. The principle investigator (NvdR), who was not involved in the recruitment of patients or treatment allocation, prepared opaque, sealed envelopes. After the baseline measurement the administrative assistant handed the next envelope to the patient who then opened the envelope guaranteeing concealed randomisation. Due to the pragmatic design both patients and physiotherapists could not be blinded for the interventions.
Interventions
The intensive group training protocol combines exercise therapy, back school and behavioural principles. Physiotherapists in the protocol group received two intensive training sessions of 6 h each and were trained to work according to protocol, including behavioural principles. Patients received 10 individual sessions consisting of patient history, physical examination, providing information on the treatment, determining baseline level of functional capacity, setting treatment goals, signing a treatment contract and evaluating treatment goals. During the 20 group sessions patients trained according to operant-conditioning behavioural principles based on the baseline level of functional capacity.
Physiotherapists in the guideline group received two training sessions of three hours each. Background, content and recommendations of the guideline were discussed during the training sessions. Patients assigned to the guideline group were treated individually and the number of treatment sessions was at the discretion of the physiotherapists. The mean number of physiotherapy sessions per patient in this group was 13.
Outcome assessment
Patients completed questionnaires at baseline and 6, 13, 26 and 52 weeks after randomisation. Primary outcome measures were: (1) functional status assessed with the 24-item Roland Morris Disability Questionnaire (RDQ) [18]; (2) pain-intensity measured on an 11-point numerical rating scale (PI-NRS), ranging from 0 “no pain” to 10 “very severe pain” [3]; (3) global perceived effect (GPE) measured on a 6-point scale ranging from “much worse” to “completely recovered”; (4) work absenteeism, measured with the Short Form Health and Labour Questionnaire (HLQ) [5, 25]. Secondary outcomes were: (1) fear of movement/(re)injury using the 17-item Tampa scale [10]; (2) pain coping strategies assessed using the Pain Coping Inventory [11]; (3) self-efficacy beliefs are measured using the Pain Self-Efficacy Questionnaire [14].
Sample size calculation
Sample size was based on detecting a clinically relevant difference in functional disability (difference of 3 points on the RDQ after 52 weeks [2]) with a power (1 − β) of 90% and a significance level of 5%. This resulted in 60 patients per group.
Statistical analyses
Baseline similarity was assessed, using Chi-square tests, unpaired Student’s t tests or Mann–Whitney U tests. An intention-to-treat analysis was conducted for each follow-up moment using multilevel modelling. The included levels were: repeated measures (i.e. time), patient, physiotherapists and physiotherapy practices. Analyses were adjusted for patients’ characteristics that differed between the protocol group and the guideline group. Resulting regression coefficients can be interpreted as the difference on patient outcomes between both groups at a certain follow-up period corrected for the difference at baseline. Per-protocol analyses were performed additionally, excluding all participants who did not receive or complete the randomised intervention. Three subgroup analyses were performed for patients with elevated psychosocial scores at baseline (fear avoidance beliefs, median split; catastrophising, median split; self efficacy, median split). The analyses were performed in SPSS version 12.0 and MLwiN version 2.02.
Results
Participants
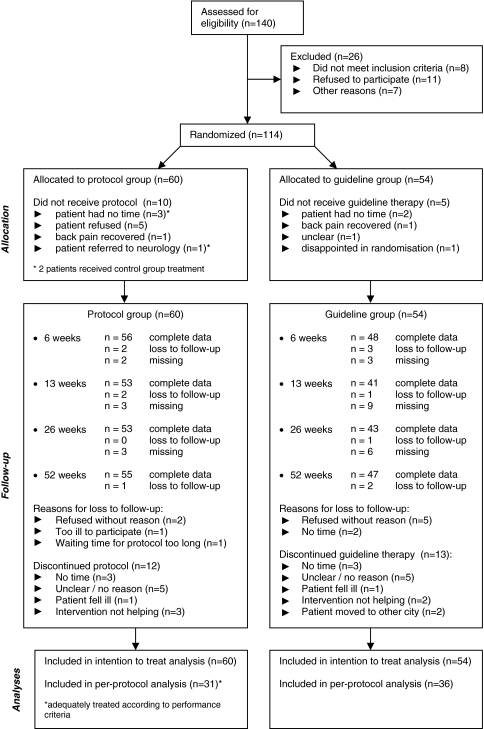
From October 2003 until April 2005 a total of 105 participating physiotherapists referred 140 patients with low back pain to a research centre; 114 patients met all inclusion criteria and signed informed consent. Figure 1 shows the trial profile. One patient enrolled should not have been, since this patient showed signs of specific low back pain and was later referred to a neurologist. Four patients in each group had sub-acute low back pain and were included in the analyses.
Fig. 1.
Flowchart
Baseline characteristics
Baseline characteristics of the patients were largely similar in both groups (Table 1). There was a difference at baseline in the percentage of patients with paid work and ethnic background. Patients who were lost to follow-up (n = 12) were significantly younger at baseline than completers (mean age 34.1 vs. 42.6).
Table 1.
Baseline characteristics of the two intervention groups
| Variable | Protocol group (n = 60) | Guideline group (n = 54) |
|---|---|---|
| Age in years (mean; SD) | 41.5 (8.8) | 42.0 (9.9) |
| Women | 33 (55%) | 26 (48%) |
| Paid work (% yes) | 42 (70%) | 31 (57%) |
| Ethnic background | ||
| Dutch | 29 (48%) | 19 (35%) |
| Immigrant (European) | 3 (5%) | 2 (4%) |
| Immigrant (non-European) | 28 (47%) | 33 (61%) |
| Education level | ||
| Low | 17 (28%) | 15 (28%) |
| Middle | 30 (50%) | 28 (52%) |
| High | 13 (22%) | 11 (20%) |
| Duration current episode in weeks (mean; SD) | 53.9 (70.6) | 47.2 (64.3) |
| Previous complaints of LBP | 47 (78%) | 43 (80%) |
| # LBP episodes in the last 12 months | ||
| 0 episodes | 13 (22%) | 14 (26%) |
| 1–2 episodes | 6 (10%) | 4 (7%) |
| 3–5 episodes | 11 (18%) | 9 (17%) |
| More than 5 episodes | 8 (13%) | 3 (6%) |
| Nonstop complaints | 22 (37%) | 24 (44%) |
| Preference for treatment | ||
| Preference for protocol | 5 (8%) | 4 (7%) |
| Preference for guideline | 23 (38%) | 19 (35%) |
| No preference | 32 (53%) | 31 (57%) |
Data are number of patients (%) unless otherwise indicated
Effect of the intervention
The multilevel analyses showed that all analyses had to be adjusted for the correlation of repeated measures within patients and physiotherapists. The variation of the physiotherapy practices level was 0% and this level was, therefore, excluded from the final multilevel models. Table 2 shows the means, regression coefficients and odds ratios for the primary and Table 3 for the secondary outcome measures estimated with multilevel modelling. No statistically significant differences were found for functional status. At 26 weeks, patients in the protocol group reported significantly lower pain intensity, however this difference was absent after 1 year follow-up.
Table 2.
Multilevel model-based mean scores at baseline and follow-up and the regression coefficients and odds ratios (95% CI) for the primary outcome measures
| Primary outcome measure | Protocol group | Guideline group | Regression coefficients (95% CI)a |
|---|---|---|---|
| Functional status (RDQ) | |||
| Baseline | 11.6 | 12.1 | |
| 6 weeks | 10.2 | 10.2 | 0.35 (−1.29; 1.98) |
| 13 weeks | 7.9 | 7.5 | 0.85 (−1.36; 3.06) |
| 26 weeks | 7.4 | 7.7 | 0.13 (−2.24; 2.50) |
| 52 weeks | 6.7 | 7.1 | 0.06 (−2.22; 2.34) |
| Overall effect: χ2 = 0.980; 4df (P = 0.91) | |||
| Regression coefficients (95% CI)b | |||
| Pain intensity (PI-NRS) | |||
| Baseline | 6.2 | 5.9 | |
| 6 weeks | 5.3 | 5.4 | −0.42 (−1.29; 0.46) |
| 13 weeks | 4.4 | 4.9 | −0.76 (−1.74; 0.23) |
| 26 weeks | 4.1 | 4.8 | −0.97 (−1.88; −0.06)* |
| 52 weeks | 3.9 | 4.6 | −1.02 (−2.14; 0.09) |
| Overall effect: χ2 = 5.212; 4df (P = 0.27) | |||
| Odds ratios (95% CI) | |||
| Perceived effect (GPE) (% yes) | |||
| 6 weeks | 14.2% | 20.4% | 0.65 (0.21; 2.01) |
| 13 weeks | 29.9% | 29.6% | 1.02 (0.37; 2.80) |
| 26 weeks | 38.2% | 39.8% | 0.93 (0.36; 2.43) |
| 52 weeks | 45.0% | 32.3% | 1.71 (0.67; 4.38) |
| Overall effect: χ2 = 4.968; 4df (P = 0.29) | |||
RDQ Roland Morris Disability Questionnaire, PI-NRS Pain Intensity Numerical Rating Scale, GPE general perceived effect, df degrees of freedom, CI confidence intervals
* P < 0.05
aAdjusted for baseline, ethnic background and work status
bAdjusted for baseline and ethnic background
Table 3.
Multilevel model based mean scores at baseline and follow-up and the regression coefficients (95% CI) for the secondary outcome measures
| Secondary outcome measure | Protocol group | Control group | Regression coefficients (95% CI) |
|---|---|---|---|
| Fear avoidance (Tampa)a | |||
| Baseline | 37.9 | 39.6 | |
| 6 weeks | 37.2 | 39.1 | −0.29 (−2.64; 2.07) |
| 13 weeks | 35.6 | 38.6 | −1.34 (−4.06; 1.39) |
| 26 weeks | 35.7 | 38.1 | −0.78 (−3.46; 1.91) |
| 52 weeks | 37.9 | 39.3 | 0.23 (−2.78; 3.25) |
| Overall effect: χ2 = 1.833; 4df (P = 0.77) | |||
| Active coping (PCI-A)a | |||
| Baseline | 6.4 | 6.6 | |
| 6 weeks | 6.1 | 6.6 | −0.14 (−0.59; 0.31) |
| 13 weeks | 5.9 | 6.3 | −0.10 (−0.59; 0.38) |
| 26 weeks | 5.9 | 6.5 | −0.31 (−0.80; 0.17) |
| 52 weeks | 5.9 | 6.0 | −0.13 (−0.42; 0.69) |
| Overall effect: χ2 = 4.535; 4df (P = 0.34) | |||
| Passive coping (PCI-P)a | |||
| Baseline | 6.1 | 6.4 | |
| 6 weeks | 5.8 | 6.3 | −0.33 (−0.75; 0.09) |
| 13 weeks | 5.3 | 6.1 | −0.61 (−1.10; −0.12)* |
| 26 weeks | 5.4 | 5.9 | −0.24 (−0.72; 0.24) |
| 52 weeks | 5.5 | 5.9 | −0.09 (−0.65; 0.47) |
| Overall effect: χ2 = 8.751; 4df (P = 0.07) | |||
| Self-efficacy (SES)b | |||
| Baseline | 37.5 | 37.7 | |
| 6 weeks | 40.1 | 37.9 | 2.41 (−0.80; 5.61) |
| 13 weeks | 43.4 | 40.1 | 3.55 (−0.49; 7.59) |
| 26 weeks | 41.4 | 41.8 | −0.16 (−4.42; 4.11) |
| 52 weeks | 43.8 | 41.2 | 2.80 (−1.86; 7.46) |
| Overall effect: χ2 = 7.037; 4df (P = 0.13) | |||
PCI-A Pain coping inventory, items active coping; PCI-P pain coping inventory, items passive coping; SES Self-efficacy scale; df degrees of freedom; CI confidence intervals
* P < 0.05
aAdjusted for baseline and ethnic background
bAdjusted for baseline, ethnic background and work status
Registration forms regarding treatment goals, content of the different sessions and evaluation of the treatment were completed by physiotherapists in both groups. The forms of the protocol group were also used to determine whether the protocol was followed adequately. We applied 18 performance criteria which are summarised in Table 4. Despite the training sessions the protocol physiotherapists received, we found that in 18% of the patients the protocol was not adequately followed. The results of the per-protocol analyses were similar to the intention-to-treat analyses (data not shown). Subgroup analyses showed that the protocol group was more effective in reducing pain intensity at 52 weeks follow-up for patients with elevated fear avoidance scores at baseline (Table 5). No multilevel analyses were performed for sick leave since less than 14, 8 and 5% of the workers were on sick leave at 13, 26 and 52 weeks, respectively, after randomisation.
Table 4.
Criteria list used to assess the quality of the intensive group training protocol
| 1 | At least two or more criteria have been set (focussed on activities or participation) |
| 2 | Duration, intensity, frequency etc. were formulated in the treatment goals |
| 3 | Reducing pain was not adopted as a treatment goal |
| 4 | The treatment goals were evaluated (whether goals are met is registered) |
| 5 | A minimum of two baseline measurements were performed |
| 6 | A treatment agreement (with goals) was signed by patient and physiotherapist |
| 7 | Information on dealing with (chronic) pain was provided |
| 8 | A minimum of 15 group training sessions (75%) were attended |
| 9 | Patient trained in a group |
| 10 | Graphs were used during training sessions and evaluations |
| 11 | A gradually progressive exercise scheme was prepared |
| 12 | There was/were plausible reason(s) for not following the progressive exercise scheme |
| 13 | At least one aerobic exercise was included in the scheme |
| 14 | At least one back exercise was included in the scheme |
| 15 | At least one abdominal exercise was included in the scheme |
| 16 | At least one buttock exercise was included in the scheme |
| 17 | A minimum of two evaluations were performed |
| 18 | No other (manual) therapies for low back pain were performed |
One point was assigned to each positively assessed Item; the maximum score was 18. For adoption in the per protocol analysis a minimum of 14 points were necessary
Table 5.
Three subgroup analyses with regression coefficients and odds ratios (95% CI) for the difference between the two groups 52 weeks after baseline
| Functional status (RDQ)a | Pain Intensity (NRS)a | Perceived recovery (GPE)b | ||||
|---|---|---|---|---|---|---|
| Fear-avoidance (17–68) | ||||||
| Tampa > 38 (n = 54) | 1.91 | (−1.31; 5.13) | −1.91 | (−3.42; −0.39)* | 2.83 | (0.76; 10.59) |
| Tampa ≤ 38 (n = 60) | −1.53 | (−4.65; 1.60) | −0.02 | (−1.58; 1.54) | 0.93 | (0.23; 3.71) |
| Catastrophising (9–36) | ||||||
| PCI_C > 20 (N = 52) | 1.80 | (−1.49; 5.09) | −0.52 | (−2.13; 1.10) | 2.48 | (0.03; 223.63) |
| PCI_C ≤ 20 (N = 60) | −0.72 | (−3.82; 2.39) | −1.19 | (−2.71; 0.33) | 4.03 | (1.06; 15.29) |
| Self-efficacy (0–60) | ||||||
| SES > 38 (N = 53) | −1.44 | (−4.78; 1.91) | −0.67 | (−2.28; 0.94) | 2.92 | (0.70; 11.82) |
| SES ≤ 38 (N = 61) | 1.52 | (−1.50; 4.54) | −1.05 | (−2.51; 0.41) | 0.81 | (0.20; 3.27) |
RDQ Roland Morris Disability Questionnaire, VAS Visual Analogue Scale, GPE general perceived effect, PCI_C pain coping inventory (scale items catastrophising), SES self-efficacy scale
* P < 0.05
aRegression coefficients
bOdds ratios
Adverse events
No serious adverse events (an event resulting in admission to hospital or permanent disability, or both, or death) were reported by patients in either of the groups.
Cost effectiveness
A detailed report of the economic evaluation is provided in a separate paper [24]. After 52 weeks the direct health care costs were significantly higher for patients in the protocol group (€ 1003) compared with the control group (€ 527), largely due to the costs of the intervention. The mean difference in total costs amounted to € 233 (95% CI € −2.185 and 2.764). The cost-effectiveness planes indicated no significant differences in cost-effectiveness between the two groups.
Discussion
The intensive group training protocol tended to be more effective in reducing pain intensity, coping and self-efficacy and more patients in this group (45%) indicated that they had improved compared to the guideline group (32%). However, the differences were small and not statistically significant during 1 year follow-up. The lack of statistical differences between the groups does not imply that patients did not improve. The minimal clinically important change (MCIC) in patients has been estimated to be at least 2 points on a Pain Intensity Numerical Rating Scale (PI-NRS) [4, 23]. In the protocol group 48% of the patients scored at least the MCIC score versus 37% in de guideline group. Applying 30% change from the baseline score [9] for the RDQ, results in 57% of the patients in the protocol group versus 48% in the guideline group experiencing a MCIC in functional status.
The strength of the study is the randomised design of the trial, reducing the chance of confounding. The relatively similar baseline characteristics of the patients in both groups indicate the successful randomisation. The number of patients that were lost to follow-up was comparable in both groups indicating non-selective drop-out.
This study had some limitations. Three months after the start of the inclusion period the Dutch government passed new legislation which de-listed physical therapy from basic health care insurance. In the first 2 months of 2004 the total number of visits to all physiotherapists in The Netherlands dropped with 14.6% compared to 2003; over the whole year the number of visits dropped with 6.1% [20]. The inclusion period of 1 year was therefore extended to 1 year and 6 months. Additionally, we recruited and trained 25 additional physiotherapists in two cities outside Amsterdam. This resulted in inclusion of a total of 114 patients. Although we aimed at inclusion of 120 patients, we believe that the power is sufficient and that an additional 6 participants would not have changed the results of this study.
Furthermore, the participating physiotherapists may not have delivered the intensive group training protocol adequately. Ideally, all group training sessions should be audio-taped and assessed by experts. Unfortunately, no means were available for this purpose; instead we used registration forms and regularly visited the group trainings. Participating physiotherapists were not selected on the basis of their skills or knowledge of behavioural therapies. It is possible that the used training method for the physiotherapists was insufficient for adequate performance of the therapy. We used the Pain Attitudes and Beliefs Scale for Physiotherapists (PABS-PT) [15] before and after training the physiotherapists in both groups to examine the effects of the training. We found that the scores on ‘behavioural orientation’ did not significantly increase after the training in the protocol group. This may have reduced the contrast between both interventions.
In contrast to previous studies in occupational care, our study did not find that an intensive group training protocol based on principles of graded activity was more effective than usual physiotherapy guideline care. The reduction in sick leave seen in occupational populations was not confirmed in a primary care population. Therefore, we conclude that the intensive group training protocol was not more effective than usual care and need not to be implemented in primary care physiotherapy.
Acknowledgments
The Medical Ethics Committee of VU University Medical Centre has approved the study design, protocols and informed consent procedures. This study was funded by the Netherlands Organisation for Health Research and Development (ZONMW) grant no: 945-03-023. This organisation was not directly involved in the research project and researchers were free to publish results from the study.
Conflict of interests
The authors have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Bekkering GE, Hendriks HJM, Koes BW, Oostendorp RAB, Ostelo RWJG, Thomassen JMC, van Tulder MW. National Practice Guideline for the physiotherapeutic management of patients with low back pain. Physiotherapy. 2003;89:82–96. doi: 10.1016/S0031-9406(05)60579-2. [DOI] [Google Scholar]
- 2.Bombardier C, Hayden J, Beaton DE. Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol. 2001;28:431–438. [PubMed] [Google Scholar]
- 3.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–381. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 5.Hakkaart-van Roijen L, van Straten A, Donker M, Tiemens M. Manual trimbos/iMTA questionnaire for costs associated with psychiatric illness (TiC-P) Rotterdam: Rotterdam Institute for Medical Technology Assessment, Erasmus University; 2002. [Google Scholar]
- 6.Hayden JA, Van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–775. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 7.Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003;12:149–165. doi: 10.1007/s00586-002-0508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2005;30(19):2153–2163. doi: 10.1097/01.brs.0000182227.33627.15. [DOI] [PubMed] [Google Scholar]
- 9.Jordan K, Dunn KM, Lewis M, Croft P. A minimal clinically important difference was derived for the Roland-Morris Disability Questionnaire for low back pain. J Clin Epidemiol. 2006;59:45–52. doi: 10.1016/j.jclinepi.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Kori SH, Miller RP, Todd DD. Kinesiophobia: a new view of chronic pain behaviour. Pain Management. 1990;3:35–42. [Google Scholar]
- 11.Kraaimaat FW, Evers AW. Pain-coping strategies in chronic pain patients: psychometric characteristics of the pain-coping inventory (PCI) Int J Behav Med. 2003;10(4):343–363. doi: 10.1207/S15327558IJBM1004_5. [DOI] [PubMed] [Google Scholar]
- 12.Lindstrom I, Ohlund C, Eek C, Wallin L, Peterson LE, Fordyce WE. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant-conditioning behavioral approach. Phys Ther. 1992;72:279–290. doi: 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 13.Manek NJ, MacGregor AJ. Epidemiology of back disorders: prevalence, risk factors, and prognosis. Curr Opin Rheumatol. 2005;17:134–140. doi: 10.1097/01.bor.0000154215.08986.06. [DOI] [PubMed] [Google Scholar]
- 14.Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11(2):153–163. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Ostelo RW, Stomp-van den Berg SG, Vlaeyen JW, Wolters PM, de Vet HC. Health care provider’s attitudes and beliefs towards chronic low back pain: the development of a questionnaire. Man Ther. 2003;8:214–222. doi: 10.1016/S1356-689X(03)00013-4. [DOI] [PubMed] [Google Scholar]
- 16.Ostelo R, Tulder M, Vlaeyen J, Linton S, Morley S, Assendelft W (2005) Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev CD002014 [DOI] [PubMed]
- 17.Picavet HS, Schouten JS. Musculoskeletal pain in The Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain. 2003;102:167–178. doi: 10.1016/s0304-3959(02)00372-x. [DOI] [PubMed] [Google Scholar]
- 18.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Staal JB, Hlobil H, Twisk JW, Smid T, Koke AJ, van Mechelen W. Graded activity for low back pain in occupational health care: a randomized, controlled trial. Ann Intern Med. 2004;140:77–84. doi: 10.7326/0003-4819-140-2-200401200-00007. [DOI] [PubMed] [Google Scholar]
- 20.Swinkels I, van Sonsbeeck D, de Bakker D. Daling in de vraag naar fysiotherapie en oefentherapie in het jaar 2004. Utrecht: NIVEL; 2005. [Google Scholar]
- 21.Thomas E, Silman AJ, Croft PR, Papageorgiou AC, Jayson MI, Macfarlane GJ. Predicting who develops chronic low back pain in primary care: a prospective study. BMJ. 1999;318:1662–7. doi: 10.1136/bmj.318.7199.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Roer N, Van Tulder MW, Barendse JM, van Mechelen W, Franken WK, Ooms AC (2004) Cost-effectiveness of an intensive group training protocol compared to physiotherapy guideline care for sub-acute and chronic low back pain: design of a randomised controlled trial with an economic evaluation. [ISRCTN45641649]. BMC Musculoskelet Disord;5:45 [DOI] [PMC free article] [PubMed]
- 23.van der Roer N, Ostelo RW, Bekkering GE, Van Tulder MW, de Vet HC. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine. 2006;31:578–582. doi: 10.1097/01.brs.0000201293.57439.47. [DOI] [PubMed] [Google Scholar]
- 24.van der Roer N, van Tulder M, van Mechelen W, de Vet H. Economic evaluation of an intensive group training protocol compared with usual care physiotherapy in patients with chronic low back pain. Spine. 2008;33:445–451. doi: 10.1097/BRS.0b013e318163fa59. [DOI] [PubMed] [Google Scholar]
- 25.van Roijen L, Essink-Bot ML, Koopmanschap MA, Bonsel G, Rutten FF. Labor and health status in economic evaluation of health care. The Health and Labor Questionnaire. Int J Technol Assess Health Care. 1996;12:405–415. doi: 10.1017/s0266462300009764. [DOI] [PubMed] [Google Scholar]