Abstract
This study is a retrospective multi-centre analysis of changes in spino-pelvic sagittal alignment after surgical correction of L5–S1 developmental spondylolisthesis. The purpose of this study was to determine how sagittal spino-pelvic alignment is affected by surgery, with the hypothesis that surgical correction at the lumbo-sacral level is associated with an improvement in the shape of the spine and in the orientation of the pelvis. Whether L5–S1 high grade spondylolisthesis should or should not be reduced remains a controversial subject. A popular method of treatment has been in situ fusion, but studies have reported a high rate of pseudarthrosis, slip progression and persistent cosmetic deformity. Spinal instrumentation with pedicle screws has generated a renewed interest for reduction, but the indications for this treatment and its effect on spino-pelvic alignment remain poorly defined. Recent evidence indicates that reduction might be indicated for subjects with an unbalanced (retroverted or vertical) pelvis. This is a retrospective multi-centre analysis of 73 subjects (mean age 18 ± 3 years) with developmental spondylolisthesis and an average follow-up of 1.9 years after reduction and posterior fusion with spinal instrumentation or cast immobilisation. Spinal and pelvic alignment were measured on standing lateral digitised X-rays using a computer software allowing a very high inter and intra observer reliability. Pelvic incidence was unaffected by surgery. The most important changes were noted for grade, L5 Incidence, lumbo-sacral-angle, and lumbar lordosis, which all decreased significantly towards normal adult values. At first evaluation, pelvic tilt, sacral slope and thoracic kyphosis appeared minimally affected by surgery. However, after classifying subjects into balanced and unbalanced pelvis, significant improvements were noted in pelvic alignment in both the sub-groups, with 40% of cases switching groups, the majority from an unbalanced to a balanced pelvis alignment. The direction and magnitude of these changes were significantly different by sub-group: sacral slope decreased in the balanced pelvis group but increased in the unbalanced group, while pelvic tilt values did the opposite. While pelvic shape is unaffected by attempts at surgical reduction, proper repositioning of L5 over S1 significantly improves pelvic balance and lumbar shape by decreasing the abnormally high lumbar lordosis and abnormal pelvic retroversion. These results emphasise the importance of sub-dividing subjects with high grade developmental spondylolisthesis into unbalanced and balanced pelvis groups, and further support the contention that reduction techniques might be considered for the unbalanced retroverted pelvis sub-group.
Keywords: Spondylolisthesis, Surgery, Sagittal alignment, Posture
Introduction
The question of whether L5–S1 developmental spondylolisthesis should or should not be reduced by surgery remains a very controversial subject. Historically, a popular method of treatment for a high grade L5–S1 spondylolisthesis has been to perform a postero-lateral in situ fusion. Many retrospective studies have shown that this treatment will be satisfactory in 75–80% of subjects [5, 10, 24], but others [3] have reported a high rate of pseudarthrosis, further progression of the slip as well as persistent cosmetic deformity of the trunk and sagittal imbalance. Over the past decade, more liberal use of pedicle screws has generated a renewed interest for reduction, but the indications for this treatment and its effect on spino-pelvic alignment remain poorly defined. Many retrospective studies [17, 19] indicate that obtaining a reduction is possible, but at the expense of an increased neurological risk and of some loss of reduction in the post-operative period.
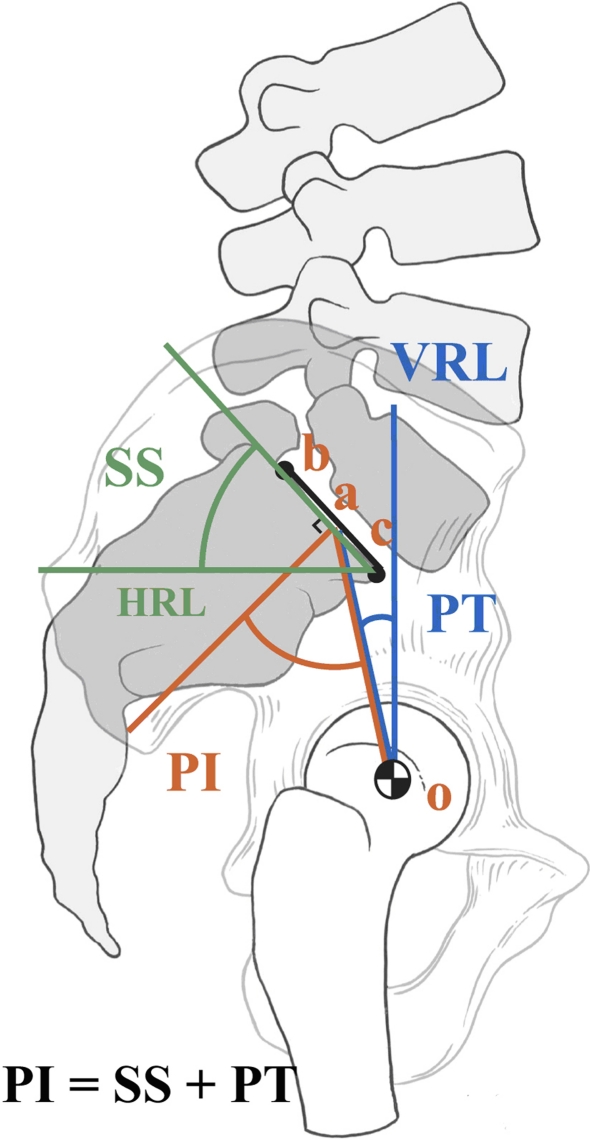
In order to decide which patients should be treated by reduction, a number of radiological measurements that describe the relationship between L5 and S1 have been used, such as percentage of slip, slip angle or lumbo-sacral kyphosis [22, 25]. These measurements are improved after reduction, but the effect of these local L5–S1 changes on the global spino-pelvic alignment has not been reported. Duval-Beaupère and colleagues [11] have proposed pelvic incidence as a fundamental anatomic parameter, which is specific and constant for each individual and is a strong determinant of pelvic orientation and lumbar lordosis. It is defined as the angle between a line perpendicular to the sacral plate and a line joining the sacral plate to the axis of the femoral heads, and is the arithmetic sum of sacral slope (SS) + pelvic tilt (PT), two position-dependant variables which are used to describe pelvic orientation in the sagittal plane (Fig. 1). Many studies [6, 8, 16, 21] have shown that these relationships are clearly disturbed in L5–S1 spondylolisthesis, but again, the effect of surgery on spino-pelvic alignment remains poorly understood. Recently, in an analysis of patients with high grade spondylolisthesis, Hresko et al. [7] have reported two distinct groups named “balanced” and “unbalanced” pelvis. Patients with an unbalanced pelvis had a sagittal spinal alignment that differed from those with a balanced pelvis and a control group, suggesting that reduction techniques might be considered in patients with an unbalanced pelvis.
Fig. 1.
Sagittal pelvic parameters based on standing radiograph. The pelvic incidence (PI) is constant for each person. Sacral slope (SS) and pelvic tilt (PT) are variable dependent on the version of the pelvis about the hip axis (O). VRL vertical reference line; HRL horizontal reference line (reproduced with permission from O’Brien et al. (2004) Radiographic measurement manual. Medtronic Sofamor Danek, Memphis, TN)
Therefore, the purpose of this study was to determine how sagittal spino-pelvic alignment is affected after surgical reduction of L5–S1 spondylolisthesis, with the hypothesis that surgical correction at the lumbo-sacral level is associated with an improvement in the shape of the spine and in the orientation of the pelvis.
Material and methods
A retrospective multi-centre study of 73 subjects recruited from 10 medical institutions in North America and France was conducted with the following inclusion criteria: (1) a diagnosis of developmental L5–S1 spondylolisthesis according to the classification of Marchetti and Bartholozzi [15], (2) an age between 10 and 30 years, (3) the availability of a standing lateral radiograph of the spine and pelvis in which the spine from T1 to S1 and both femoral heads were visible, and (4) an indication for surgical reduction, as determined by the treating physician. Subjects with any previous spine surgery, associated musculo-skeletal syndrome, or significant lower limb discrepancy (>2 cm) were excluded from the study.
For each subject, the following information was obtained: age at baseline and last follow-up, sex, type of surgery performed, age at surgery, lateral standing radiographs of the spine and pelvis before and at the last available follow-up after surgery.
A similar radiological protocol was used at all participating institutions, with a 30 × 90 cm lateral radiograph of each subject standing in a comfortable position with the knees fully extended. For the upper limbs, the arms were held in slight forward flexion for all subjects, but the forearms were extended and were resting on an arm support at one centre, while they were fully flexed with the hands touching the shoulders at the other centres. Digital radiographs were available at one institution, while standard radiographs were obtained at the other institutions and were subsequently digitised using a VIDAR VXR8 X-ray film scanner. All radiographs were then measured by the same experienced individual (E.B.) using SagittalSpine® (Optimage, Lyon, France), a dedicated software to assess sagittal alignment of the spine and pelvis. This software has been described in detail previously by Berthonnaud et al. [2]: it allows fast and accurate calculation of the following parameters by interactive digitization of various anatomical landmarks of the spine and pelvis on a lateral radiograph:
Thoracic kyphosis (TK): the sagittal shape of the spine is modelised by the software as a succession of curved segments representing thoracic kyphosis and lumbar lordosis. Kyphosis is represented by two arcs of circle tangent at the apex of the curve, and thoracic kyphosis is the sum of the kyphosis above and below the apex.
Lumbar lordosis (LL): likewise, lordosis is represented by two arcs of circle tangent at the apex of the curve, and lumbar lordosis is the sum of the lordosis above and below the apex.
The number of vertebrae included in the lordosis was also recorded as length of lumbar lordosis
Pelvic incidence (PI), defined as the angle between a line joining the centre of the upper endplate of S1 to the axis of the femoral heads and a line perpendicular to the upper end plate of S1 (Fig. 1).
Sacral slope (SS), defined as the angle between the endplate of S1 and a horizontal line (Fig. 1).
Pelvic tilt (PT), defined as the angle between a vertical line and the line joining the middle of the sacral plate and the axis of the femoral heads. It is positive when the hip axis lies in front of the middle of the sacral plate (Fig. 1).
Grade of spondylolisthesis, as measured by the Newman technique [18].
Incidence of L5 (IL5), defined as the angle between a line joining the centre of the upper endplate of L5 to the axis of the femoral heads and a line perpendicular to the upper end plate of L5.
Lumbosacral angle (LSA), or slip angle, defined as the angle between a line joining the lower endplate of L5 to a line joining the upper endplate of S1.
The inter and intra observer variability of these measurements is ±1° with an ICC between 0.92 and 0.99, as reported by Berthonnaud et al. [1] in a study evaluating radiographs of 15 normal and 15 scoliotic subjects. Two recent studies [13, 20] have demonstrated that the technique of measurement of TK and LL used with this software is very highly correlated to the Cobb angle technique, but more reliable and less variable in the thoracic area (Fig. 2).
Fig. 2.
The two subgroups of patients with high-grade spondylolisthesis based on their pelvic balance (reproduced with permission from Hresko et al. [7])
In the presence of a dome shaped sacrum, the technique recommended by the Spinal Deformity Study Group was used to measure PI, SS and PT [8].
Finally, all subjects were sub-divided into either the balanced pelvis group (high SS and low PT) or the unbalanced retroverted pelvis (high PT and low SS) according to the method described by Hresko et al. [7]. Briefly, the measurement of the PT and SS is performed from a standing lateral radiograph centred on the lumbosacral spine, which includes the hips and the spine. The subclassification of high-grade spondylolisthesis, based on version of the pelvis can be obtained by plotting the SS and PT on a graph provided in their publication. Patients with a “balanced” high-grade spondylolisthesis have pelvic parameters similar to that of asymptomatic controls with high PI. High-grade spondylolisthesis patients with “unbalanced” retroverted pelvis differ from asymptomatic controls and “balanced” pelvis patients in sagittal spinal alignment.
A statistical software package (SPSS for Windows 12.0, SPSS, Chicago, IL) was used to analyse the pre and post-operative values, which included nominal/ordinal and continuous variables. Paired two-sided Student t tests and repeated measures analysis of variance were used to compare the radiological measurements before and after surgery in the entire cohort and in the two subgroups.
Results
The mean age of the 73 subjects recruited before surgery was 18 ± 3 years with a range of 10–30 years. The male to female ratio was 0.71. The average follow-up period was 1.9 years, ranging from 1 to 5 years. Before the surgery, the cohort included 17 grade II, 40 grade III, 13 grade IV and 3 grade V developmental spondylolisthesis. The majority of patients (n = 62) were treated by a one stage surgical attempt at reduction with posterior instrumentation using bilateral contoured rods, pedicles and sacral/iliac screws with autogenous postero-lateral bone graft fusion. In seven cases, the fusion and instrumentation was limited to L5–S1, while in 55 cases, it was carried up to L4. Five patients underwent a one stage L5–S1 anterior interbody fusion with a cage or graft and a posterior instrumentation using bilateral contoured rods, pedicles and sacral screws with autogenous postero-lateral bone graft fusion. Finally, the remaining 6 subjects were treated by posterolateral autogenous bone graft fusion followed by reduction and immobilization in a spica cast.
Table 1 provides the mean and standard deviations in the entire cohort for all radiological variables measured before and after surgery at last available follow-up. With the exception of pelvic incidence and thoracic kyphosis, all other variables were significantly different after surgery (P < 0.01). The most important changes were noted for IL5, LSA, and LL which all decreased significantly towards normal adult values, while grade was significantly improved from 67 to 40% in subjects with a dome shaped sacrum and from 58 to 28% in the remaining subjects with a flat shaped endplate of S1.
Table 1.
Pre and post-operative results for all measurements in the entire cohort, prior to sub grouping by pelvic balance
| Variable | Pre-op | Post-op |
|---|---|---|
| Pelvic incidence (PI) | 79° ± 11 | 78° ± 11 |
| L5 Incidence (IL5)* | 66° ± 21 | 51° ± 16 |
| Lumbo-sacral angle (LSA)* | 21° ± 19 | 4° ± 11 |
| Grade (dome)* | 67% ± 17 | 40% ± 21 |
| Grade (flat)* | 58% ± 18 | 28% ± 17 |
| Sacral slope (SS)* | 50° ± 11 | 53° ± 10 |
| Pelvic tilt (PT)* | 30° ± 10 | 26° ± 8 |
| Lumbar lordosis (LL)* | 77° ± 16 | 66° ± 13 |
| Length of LL* | 6 ± 2 | 5 ± 1 |
| Thoracic kyphosis (TK) | 38° ± 12 | 40° ± 10 |
Grade is expressed as percentage of displacement and provided for subjects with a flat and domed sacrum. Length of lumbar lordosis is determined by the number of vertebrae included in the lordotic segment
* Indicates a statistically significant difference (P < 0.01)
At first glance, changes in SS and PT appeared relatively small when considering the entire cohort. However, changes became very significant when considering the two pelvic sub-groups. Forty-one subjects were classified in the unbalanced retroverted pelvis (high PT and low SS), while 32 were classified in the balanced pelvis group (high SS and low PT). After surgery, the number of patients with a balanced pelvis increased from 32 to 49, while the number of patients with an unbalanced pelvis decreased from 41 to 24. Overall, 27 patients (40%) changed classification following surgery. The majority, 22 (70%), went from the unbalanced to the balanced group. Five went from the balanced to the unbalanced group.
Overall, sacral slope increased slightly but significantly following surgery. However, the direction and magnitude of change were significantly different by SS/PT group (Table 2). For the balanced pelvis group (high SS, low PT), sacral slope decreased. For the unbalanced retroverted pelvis group, sacral slope increased. Overall, pelvic tilt decreased slightly but significantly following surgery. As for SS, the direction and magnitude of change were significantly different by SS/PT group (Table 3). For the balanced pelvis group, pelvic tilt increased slightly. For the unbalanced pelvis group, pelvic tilt decreased significantly.
Table 2.
Sacral slope (SS) changes by pre-op classification
| Pre-op classification | Mean | SD | N |
|---|---|---|---|
| Pre-op SS | |||
| Unbalanced pelvis | 42.9 | 8.4 | 41 |
| Balanced pelvis | 58.5 | 8.3 | 32 |
| Total | 49.7 | 11.4 | 73 |
| Post-op SS | |||
| Unbalanced pelvis | 50.8 | 9.4 | 41 |
| Balanced pelvis | 55.3 | 9.4 | 32 |
| Total | 52.8 | 9.6 | 73 |
Table 3.
Pelvic tilt (PT) changes by pre-op classification
| Pre-op classification | Mean | SD | N |
|---|---|---|---|
| Pre-op SS | |||
| Unbalanced pelvis | 35.7 | 8.8 | 41 |
| Balanced pelvis | 22.1 | 6.7 | 32 |
| Total | 29.7 | 10.5 | 73 |
| Post-op SS | |||
| Unbalanced pelvis | 28.7 | 7.3 | 41 |
| Balanced pelvis | 22.6 | 7.5 | 32 |
| Total | 26.0 | 7.9 | 73 |
Overall, lumbosacral angle decreased significantly following surgery. LSA was significantly greater in the unbalanced group (28° ± 20) when compared to the balanced group before surgery (12° ± 14). The direction was the same for both the groups, but the magnitude of change was significantly different by SS/PT group. For the unbalanced group, lumbosacral angle decreased at a greater rate than for the balanced group. Following surgery, the unbalanced group still had a greater magnitude of lumbosacral angle (6° ± 11 vs. 4° ± 11).
Overall, L5 incidence decreased significantly following surgery. The direction and magnitude of change were similar for both the groups. The unbalanced group had higher values for L5 incidence, both pre-operatively and post-operatively (72° ± 20 and 55° ± 14), than the balanced group (58° ± 19 and 46° ± 16).
Overall, lumbar lordosis decreased significantly following surgery. Neither the direction nor magnitude was significantly different for one group when compared to the other. Overall, length of lordosis changed significantly following surgery. The direction and magnitude were similar for both the groups. Similarly, the change in thoracic kyphosis from pre-op to post-op was not significant overall, and neither the magnitude nor direction of change varied significantly by group.
Discussion
Duval-Beaupère and co-workers [4, 11, 16] have demonstrated that pelvic incidence is an important anatomic parameter that describes the anatomical shape of the pelvis and greatly influences the positional configuration of the spine and pelvis, and thus of sagittal spino-pelvic alignment. Many studies [12, 14, 23] have also suggested that normal sagittal spino-pelvic alignment is a combination of balance between spino-pelvic shape and position parameters, which are interrelated and interdependent. The pelvic shape, best quantified by PI, determines the position of the pelvis (PI = SS + PT) and of the sacrum. The spine reacts to this position by adapting through lumbar lordosis, the amount of lordosis increasing as the sacral slope increases in order to balance the trunk in the upright position.
An association between PI and spondylolisthesis has been reported in many publications [6, 9, 16, 21]. All authors have noted a greater pelvic incidence and sacral slope, and postulated that a specific pelvic shape with increased PI could predispose to spondylolisthesis. Recently, Hresko et al. [7] analysed sagittal alignment in high grade spondylolisthesis patients and reported two distinct groups termed “balanced” and “unbalanced” pelvis. PT and SS were similar in balanced pelvis patients and control population with high PI. Unbalanced pelvis patients had a sagittal spinal alignment that differed from the balanced pelvis and control groups, suggesting that reduction techniques might be considered in this group. Mac-Thiong et al. [14] have proposed a postural model of sagittal alignement of spondylolisthesis incorporating this new knowledge and report that children and adolescents stand with a relatively constant global sagittal spino-pelvic alignment, regardless of the local lumbosacral deformity. A normal posture is maintained in low-grade and high-grade spondylolisthesis with a balanced pelvis. However, posture is abnormal in high-grade spondylolisthesis with an unbalanced pelvis, again suggesting that surgical reduction of the local lumbosacral deformity in these patients could be attempted to restore a normal posture.
The effect of surgical reduction on spino-pelvic alignment remains poorly defined. Percentage of slip, slip angle or lumbo-sacral kyphosis [22, 25] have been used to quantify reduction of L5 over S1, but the effect of these changes on the global spino-pelvic alignment has rarely been reported.
The present study provides a critical analysis of sagittal spino-pelvic alignment after surgical correction of spondylolisthesis, taking into account the recent advances in our understanding of this disorder. It indicates that surgical correction of developmental spondylolisthesis has a significant and profound effect on sagittal alignment of the spine and pelvis, and confirms our hypothesis that surgical correction produces an improvement in the shape and alignment of the spine as well as in the orientation of the pelvis. In addition to an improvement in L5–S1 relationship, the key to the changes observed is the improvement in pelvic orientation which could only be adequately documented by sub-dividing our cohort into balanced and unbalanced pelvis, thus supporting the findings of Hresko et al. [7]. The direction and magnitude of changes were significantly different by sub-group, with a significant improvement of pelvic balance towards normal values and a majority of subjects switching from one group to another and doing so in a favourable manner, that is changing pelvic balance from the unbalanced retroverted position to the balanced group which shares the same pelvic configuration as control population with high pelvic incidence. This would explain why PT is decreased and SS is increased in the high PT/low SS unbalanced pelvis group, a favourable change towards normal values, while SS is decreased and PT is slightly increased in the high SS/low PT balanced pelvis group, also a favourable improvement towards more normal values. It should be noted that although a majority of subjects switched from the unbalanced to the balanced group, five patients did the opposite and moved from the balanced to the unbalanced pelvis sub-group. The clinical outcome of these five patients could unfortunately not be determined with certainty from this retrospective study.
Our findings support the contention that attempts at surgical correction may be best directed at patients with an unbalanced pelvis. Figure 3 is an example of a patient who switched from the unbalanced to the balanced pelvis group and summarises the most common pattern of changes noted in spino-pelvic alignment: after surgical reduction, the position of L5 over S1 is clearly improved with reduction of slip, IL5 and LSA. These changes at the lumbo-sacral area produce a secondary adaptation of pelvic orientation in the standing position, presumably to maintain a stable posture, with a significant decrease of pelvic tilt and increase of sacral slope. This change from a retroverted unbalanced to a more balanced pelvic position induces a change in shape of the lumbar spine, which adapts to the new position of the sacrum and of the sacral plate. In this particular example, the Cobb angle value of LL is unchanged, but the length of LL is significantly decreased. In addition, thoracic kyphosis is significantly increased, although this effect could not be documented in the entire cohort. This example demonstrates that shape and position parameters of the pelvis and spine are strongly correlated. A change in one positional variable will affect and change the other spine and pelvic variables. PI is the only variable that remained unchanged: this is not surprising, since PI is a descriptor of pelvic shape rather than a positional variable. Consequently, it will not be affected by a surgical procedure unless some modification to the sacral plate has been done during surgery or unless some remodelling of the sacro-iliac joints or of a dome shaped sacrum has occurred at follow-up, which was not the case in our cohort.
Fig. 3.
Example of a patient switching from the unbalanced to the balanced pelvis group after surgical correction
The retrospective nature of this multi-centre study and the possible biases associated with this design bring some limitations to our study. Although the results support the concept that spino-pelvic alignment is improved after surgery, the effect of this finding on the clinical outcome remains to be determined. Even if restoration of a normal posture would appear as a logical goal of treatment, there is no clear evidence that improving spino-pelvic alignment will have any impact on the outcome for patients. We fully recognise that the clinical usefulness of the measured changes will need to be confirmed by a prospective study correlating spino-pelvic alignment to appropriate and validated clinical outcome measurement tools, such as the SF-12, SF-36 or the SRS-30 patient questionnaire. In addition, a similar study should be done for subjects treated by in situ fusion, since secondary adaptive changes in spino-pelvic alignment may also occur after this treatment.
Conclusions
While pelvic shape is unaffected by attempts at surgical reduction, proper repositioning of L5 over S1 significantly improves pelvic balance and lumbar shape in L5–S1 developmental spondylolisthesis. Changes in pelvic balance can only be detected if sub grouping into balanced and unbalanced pelvis is done. These results support the rationale of sub-dividing subjects with high grade spondylolisthesis into unbalanced and balanced pelvis groups to analyse the results of surgery, and further support the contention that reduction techniques might be considered for the unbalanced retroverted pelvis sub-group.
Acknowledgments
The authors wish to thank Mike Shainline from PhDx for data analysis, and the following members of the Spinal Deformity Study Group for contributing cases to this study: Lawrence G. Lenke, Keith Bridwell, Tom Lowe, Courtney Brown, Peter Newton, Ensor Transfeldt.
Footnotes
This research was assisted by support from the Spinal Deformity Study Group. This research was funded by an educational/research grant from Medtronic Sofamor Danek.
References
- 1.Berthonnaud E, Labelle H, Roussouly P, Grimard G, Vaz G, Dimnet J. A variability study of computerised sagittal spino-pelvic radiological measures of trunk balance. J Spinal Disord Tech. 2005;18(1):66–71. doi: 10.1097/01.bsd.0000128345.32521.43. [DOI] [PubMed] [Google Scholar]
- 2.Berthonnaud E, Roussouly P, Dimnet J. The parameters describing the shape and the equilibrium of the set back pelvis and femurs in sagittal view. Innov Tech Biol Med. 1998;19(6):411–426. [Google Scholar]
- 3.Bradford DS, Gotfried Y. Staged salvage reconstruction of grade IV and grade V spondylolisthesis. J Bone Joint Surg (A) 1987;69:191–202. [PubMed] [Google Scholar]
- 4.Descamps H, Commare-Nordmann MC, Marty C, et al. Modification of pelvic angle during the human growth (in French) Biom Hum Anthropol. 2001;17:59–63. [Google Scholar]
- 5.Frennered AK, Danielson BI, Nachemson Al, et al. Midterm follow-up of young patients fused in situ for spondylolisthesis. Spine. 1991;16:409–416. doi: 10.1097/00007632-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Hanson DS, Bridwell KH, Rhee J, et al. Correlation of pelvic incidence with low and high-grade isthmic spondylolisthesis. Spine. 2002;27(18):2026–2029. doi: 10.1097/00007632-200209150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high grade spondylolistheses based on pelvic version and spinal balance: possible rationale for reduction. Spine. 2007;32(20):2208–2213. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 8.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5–S1 developmental spondylolisthesis: a review of pertinent radiological measurements. Spine. 2005;30(6):S27–S34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 9.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Hresko T, Chopin D, Dimnet J. Spondylolisthesis, pelvic incidence and sagittal spino-pelvic balance: a correlation study. Spine. 2004;29(18):2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 10.Lamberg T, Remes V, Helenius I, Schlenzka D, Seitsalo S, Poussa M. Uninstrumented in situ fusion for high-grade childhood and adolescent isthmic spondylolisthesis: long-term outcome. J Bone Joint Surg (A) 2007;89:512–518. doi: 10.2106/JBJS.E.00545. [DOI] [PubMed] [Google Scholar]
- 11.Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for the 3D regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2007;16(2):227–234. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mac-Thiong JM, Pinel-Giroux F-M, Guise J, Labelle H. Comparison between constrained and non-constrained Cobb techniques for the assessment of thoracic kyphosis and lumbar lordosis. Eur Spine J. 2007;16:1325–1331. doi: 10.1007/s00586-007-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mac-Thiong JM, Wang Z, de Guise J, Labelle H (2008). Postural model of sagittal spino-pelvic alignment and its relevance for lumbosacral developemental spondylolisthesis. Spine (accepted for publication) [DOI] [PubMed]
- 15.Marchetti PG, Bartolozzi P. Classification of spondylolisthesis as a guideline for treatment. In: Bridwell KW, Wald RI, editors. The textbook of spinal surgery. 2. Philadelphia: Lippincott-Raven Publishers; 1997. pp. 1211–1254. [Google Scholar]
- 16.Marty C, Boisaubert B, Descamps H, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002;11:119–125. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mushik M, Zippel H, Perka C. Surgical management of severe spondylolisthesis in children and adolescents. Spine. 1997;22:2036–2043. doi: 10.1097/00007632-199709010-00020. [DOI] [PubMed] [Google Scholar]
- 18.Newman PH. A clinical syndrome associated with severe lumbo-sacral subluxation. J Bone Joint Surg (B) 1965;47:472–481. [PubMed] [Google Scholar]
- 19.O’Brien J, Mehdian H, Jaffray D. Reduction of severe lumbo-sacral spondylolisthesis: a report of 22 cases with a ten year follow-up period. Clin Orthop Relat Res. 1994;300:64–69. [PubMed] [Google Scholar]
- 20.Pinel-Giroux F-M, Mac-Thiong J-M, Guise JA, Berthonnaud E, Labelle H. Computerised assessment of sagittal curvatures of the spine. comparison between cobb and tangent circles techniques. J Spinal Disord Tech. 2006;19:507–512. doi: 10.1097/01.bsd.0000211206.15997.dd. [DOI] [PubMed] [Google Scholar]
- 21.Rajnics P, Templier A, Skalli W, et al. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord. 2002;15:24–30. doi: 10.1097/00024720-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Schwab F, Farcy JP, Roye D. The sagittal pelvic tilt index as a criterion in the evaluation of spondylolisthesis. Spine. 1997;22:1661–1667. doi: 10.1097/00007632-199707150-00026. [DOI] [PubMed] [Google Scholar]
- 23.Vaz G, Roussouly P, Berthonnaud E, et al. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velikas EP, Blackburne JS. Surgical treatment of spondylolisthesis in children and adolescents. J Bone Joint Surg (B) 1981;63:67–70. doi: 10.1302/0301-620X.63B1.7204476. [DOI] [PubMed] [Google Scholar]
- 25.Wright JG, Bell D. Lumbosacral joint angles in children. J Pediatr Orthop. 1991;11:748–51. doi: 10.1097/01241398-199111000-00009. [DOI] [PubMed] [Google Scholar]