Abstract
This study assesses the contribution of smoking to all-cause mortality among a primarily minority cohort of urban transit operators. Survey and medical exam data, obtained from 1,785 workers (61% African American; 9% female) who participated in the 1983–1985 San Francisco MUNI Health and Safety Study, were matched against state and national death records through 2000. At baseline, approximately 45% of the workers were current smokers, 30% were former smokers, and 25% had never smoked. Covariates were demographic factors (gender, age, race/ethnicity) and alcohol use (average number of drinks per week). There were 198 deaths during the follow-up period. Kaplan–Meier survival analysis indicated that the probability of survival did not differ between former and current smokers, but was significantly lower compared to never smokers (p < 0.001). Data were further analyzed using Cox regression with age, gender, race/ethnicity, years of smoking, and average weekly number of drinks as predictors of mortality. The results showed that years of smoking significantly contributed to mortality (hazard ratio [HR] = 1.023; p < 0.001). Compared to Asian-American transit operators, elevated mortality risk was observed for African-American operators (HR = 2.78, p < 0.01) and white operators (HR = 2.93, p < 0.01). Gender and average weekly number of drinks were not significantly associated with mortality. Although rates of smoking have declined over the past two decades among blue-collar workers, elevated prevalence of former smoking will likely contribute to excess mortality among blue-collar populations.
Keywords: Smoking, Alcohol, Mortality, Blue collar, Cohort, Urban transit
Introduction
In this study, we analyze a cohort of San Francisco municipal transit operators, followed for approximately 15 years, to determine differences in mortality over time in regard to smoking history, alcohol consumption, and possibly related covariates. Bus drivers, in general, have higher rates of mortality, morbidity, and absence because of illness when compared to employees from a wide range of other occupational groups.1–4 Specifically, morbidity and mortality were found to be higher for bus drivers compared to other occupations in three general areas: cardiovascular disease, gastrointestinal disease, and musculoskeletal problems.1,3 Increased disease rates have been found for drivers regardless of the use of different research methodologies, measurement techniques, and comparison groups.1 The possibility of a “healthy worker effect” may actually help to underestimate this result.4 Such findings have been found for bus driving in different countries and driving contexts.2,5 Issues such as job stress, both physical and psychological, and the sedentary nature of the job may have some role to play.6,7
Alcohol consumption has been shown to both be a risk factor for heart disease and preventative for heart disease as well as mortality.8–11 It is difficult to disentangle the exact point in which consumption amounts and behavior shifts from being protective to a risk factor for heart disease and mortality.10 In addition, the positive coping effects of alcohol may exist in parallel to more negative effects. At present, the literature showing that problem drinking is associated with higher levels of heart disease and mortality is much less ambiguous than that showing any protective effects of alcohol on overall health.12 This is of particular relevance for transit operators, as alcohol consumption has also been found to be related positively to both job dissatisfaction and employment tenure.13 Job stress was also found to be positively related to alcohol consumption. Heavy drinking has been reported to increase as the length of employment increases. When other forms of coping are not available, alcohol consumption has been suggested as a “coping” strategy used by bus drivers. Self-reported strain reactions were also found to be positively related to alcohol consumption lending some credence to the notion that alcohol use as a form of coping helps to mitigate the effects of strain. Job monotony for bus drivers has been found to be correlated with volume of drinking and alcohol and dependency.14 Cunradi et al. found that alcohol dependency among bus drivers is related to job burnout.15
Similarly, increased smoking among urban transit operators has also been linked to on-the-job strain.14,16 Relative to workers in white-collar and professional occupations, rates of smoking among transit and motor vehicle operators have been found to be elevated. For example, respondents who were classified as motor vehicle operators in the third National Health and Nutrition Examination Survey (NHANES III), conducted from 1988 to 1994, had an estimated smoking prevalence of 41.5%.17 In contrast, those classified as machine operators had an estimated smoking prevalence of 34.2%; freight, stock, and material movers had an estimated smoking prevalence of 25.2%; and the smoking prevalence of teachers was estimated at 12.2%. Although it is well-established that smoking is the main cause of lung cancer incidence and mortality, few studies have conducted longitudinal follow-up to assess all-cause mortality among blue-collar occupational cohorts in which the role of smoking and alcohol use are accounted for. This study assessed the contribution of smoking to all-cause mortality among a cohort of predominately minority male and female urban transit operators. Results from several general population studies suggest that there may be important gender and racial/ethnic differences in mortality associated with smoking and level of alcohol consumption.18–21
For example, Greenfield et al. reported that specific drinking patterns for men (e.g., more than six drinks per day; former drinker with heavy drinking occasions) showed an increased risk for mortality; the impact of smoking was marginally significant.19 For women, the impact of alcohol was not significant, but smoking showed an increased risk for mortality. Rehm et al. found that alcohol intake and smoking increased mortality in a longitudinal study based on a community sample in rural Bavaria.20 In an analysis of NHANES I data with follow-up to 1992, Sempos et al. found no protective effect of moderate drinking on all-cause mortality adjusting for smoking status among African-American males and females.21
Although a great deal of research has been done among male drivers, there is little prospective research and, of these studies, there are few which also includes female drivers. Moreover, the minority population, the blue-collar urban transit setting and the length of follow-up are unique in the literature and may help to understand the role of smoking in a stressful occupational setting.
Methods
Sample and Data Collection
The sample for this study is based on a cohort of transit operators employed by the San Francisco Municipal Railway (MUNI). The details of the data collection process and the algorithm for inclusion in the study sample are described elsewhere and are summarized below.22 The current study’s human subjects’ protocol was approved by the Institutional Review Board of the Pacific Institute for Research and Evaluation.
The first step in the data collection was part of a state-mandated commercial driver’s license renewal examination at the Center for Municipal Occupational Safety and Health (CMOSH) clinic. All operators who underwent their mandatory biennial exam between December 1983 and September 1985 were eligible to participate. A total of 1,871 operators completed a self-reported health questionnaire, which was reviewed with a medical examiner, and each driver then received a complete physical examination. The second part of the data collection was conducted after the operator underwent a relicensing medical examination. At the request of the research staff, 1,450 operators agreed to complete a confidential, self-administered occupational and psychosocial questionnaire (77.5% response rate). These data were then matched against state and national death records obtained from the National Death Index through the year 2000. Complete data were available for 1,785 workers.
Baseline variables included age, gender, self-reported race/ethnicity (African American; white; Hispanic; Asian, Pacific Islander, or Filipino; and other), current smoking status (current smoker; former smoker; never smoker), total years smoked, and mean drinks per week. The mean drinks per week was calculated based on the self-reported number of drinks of wine, beer, and liquor consumed in an average week. Heavy drinking among MUNI transit operators has been defined as drinking 15 or more drinks per week.13,22 This is in contrast to the NIAAA definition of moderate drinking, which is no more than one drink per day for women and two drinks per day for men.
Analytic Strategy
Kaplan–Meier survival analysis was conducted to assess the probability of survival based on smoking status (current, former, never). Next, a multivariate proportional hazard model (Cox regression) was used to estimate the relative risk of death for each variable, taking into account all other covariates. Covariates included in the analysis were demographic factors (gender, age, race/ethnicity), years of smoking, and alcohol use (average number of drinks per week).
Results
Sample characteristics are shown in Table 1. Approximately 61% of the study sample was African American, and 9% were female. At baseline, approximately 45% of the workers were current smokers, 30% were former smokers, and 25% had never smoked.
Table 1.
Baseline sample characteristics (N = 1,785)
| Characteristics | Number (%) |
|---|---|
| Mean age (SD) | 41.86 (7.76) |
| African American | 1,093 (61.2) |
| White | 299 (16.8) |
| Hispanic | 157 (8.8) |
| Asian/Pacific Islander/Filipino | 212 (11.9) |
| Other | 24 (1.3) |
| Male | 1,624 (91.0) |
| Female | 161 (9.0) |
| Former smoker | 532 (29.8) |
| Current smoker | 800 (44.8) |
| Never smoker | 453 (25.4) |
| Means drinks per week (SD) | 2.59 (3.89) |
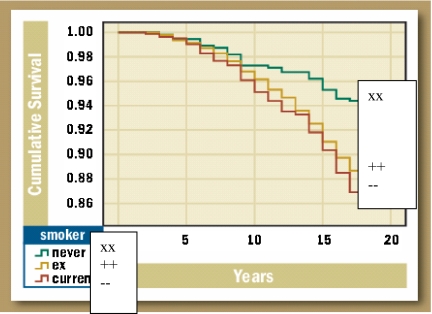
There were 198 deaths during the follow-up period. Kaplan–Meier survival analysis (Figure 1) indicated that the probability of survival did not differ between former and current smokers, but was significantly lower compared to never smokers (p < 0.001). Data were further analyzed using Cox regression with age, gender, race/ethnicity, years of smoking, and average weekly alcohol use as predictors of mortality. The results (Table 2) showed that years of smoking significantly contributed to mortality (hazard ratio [HR] = 1.023; p < 0.001). Compared to Asian-American transit operators, elevated mortality risk was observed for African-American operators (HR = 2.78, p < 0.01) and white operators (HR = 2.93, p < 0.01). Gender and average weekly number of drinks were not significantly associated with mortality. Additional analyses (data not shown) indicated that there was no interaction between smoking and drinking.
FIGURE 1.
Kaplan–Meier survival analysis.
Table 2.
Cox regression results, San Francisco transit operators
| Category | B | SE | Wald | df | p value | HR | 95% confidence interval | |
|---|---|---|---|---|---|---|---|---|
| Year smoked | 0.022 | 0.006 | 13.109 | 1 | 0.000 | 1.023 | 1.010, 1.035 | |
| Drinks per week | 0.023 | 0.014 | 2.823 | 1 | 0.093 | 1.024 | 0.996, 1.052 | |
| Age | 0.053 | 0.010 | 29.352 | 1 | 0.000 | 1.055 | 1.035, 1.075 | |
| Male gender | 0.381 | 0.330 | 1.336 | 1 | 0.248 | 1.464 | 0.767, 2.795 | |
| Race/ethnicity | Black | 1.023 | 0.346 | 8.717 | 1 | 0.003 | 2.780 | 1.410, 5.482 |
| White | 1.074 | 0.368 | 8.518 | 1 | 0.004 | 2.928 | 1.423, 6.025 | |
| Hispanic | 0.423 | 0.472 | 0.804 | 1 | 0.370 | 1.527 | 0.605, 3.851 | |
| Other | 1.385 | 0.603 | 5.273 | 1 | 0.022 | 3.992 | 1.225, 13.026 | |
Discussion
We found that ex-smokers and current smokers had similar and significantly lower survival than those who never smoked. The lack of a difference in survival between ex-smokers and current smokers could be a function of several issues such as a “healthy smoker effect” whereby ex-smokers could have quit not just for the obvious reasons of good health derived from not smoking, but because they were in relatively poorer health as a result of smoking-related problems. The increased risk found for Caucasians and African-Americans compared to other ethnic groups when controlling for a range of covariates suggests that racial/ethnic/cultural issues may be involved in stress and coping differentially or that there is a specific selection effect that is occurring across these categories. The lack of significant results for alcohol use could be a function of the ambiguous positive and negative effects alcohol has on mortality and cardiovascular health. The possible protective effects of drinking to cope, a precarious claim, can, even if actually present, be attenuated or reversed by the negative effects of alcohol abuse or heavy drinking. Age was found to be positively related to mortality and this is also an interesting finding. On one level, it is clear that older people are more subject to risk of death than younger people; nevertheless, there is a healthy worker effect that might also be at play in which those who remain on the job are healthier than those who stopped working. Such an effect is often seen in the literature and if present here may be attenuating the significant positive effect observed.
Although rates of smoking have declined over the past two decades among blue-collar workers, the elevated prevalence of former smoking will likely continue to contribute to excess mortality among some blue-collar populations, such as urban transit operators.
Limitations and Strengths
Although the cohort included female transit operators, there were relatively few women involved; thus, there might not be enough statistical power to detect actual differences if they do exist. Furthermore, although the alcohol measures are relatively common in the literature, they might not be specific or in-depth enough to discern differences. In addition, the long interval between assessment times may not properly assess changes in alcohol behavior within this time frame.
Another limitation of the study is that more detailed smoking information, such as cigarette brand or type (e.g., mentholated vs. nonmentholated), were not available. In addition, the course of smoking throughout the follow-up period is unknown. Heavier smokers may get sick at a younger age than those who smoke less. Such smokers may be exposed or experience job stress more strongly than other types of smokers and nonsmokers. Alternately, heavy smokers could be attracted to such a high stress job disproportionately compared to other types of smokers. Because such smokers may not stay in the cohort as long as others, there may be an attenuation of effect; thus, we might expect to see even larger differences between smokers and nonsmokers than found. The fact that differences were still found given the relatively crude measure of smoking gives some credence to the notion that a significant effect exists.
Occupational exposures may have changed over time of employment. At the time of the original data collection, the overwhelming majority of transit operators operated diesel buses or buses and trolley coaches powered by overhead electric lines.22 A smaller number operated light rail vehicles and cable cars. Job assignments are largely a function of seniority and these positions will change over time. It is plausible that the effect of these occupational exposures on mortality could vary. Indeed, those who are in the system longer will most likely choose relatively less stressful jobs as they become available. The assumption is that this process is generalized throughout the course of employment across all employees. That is, everyone or almost everyone will go from a relatively higher stress to a relatively lower stress position. Those who stay at relatively higher stress positions may do so because they may not feel the stress the same way, but again, the assumption is that most people will tend toward less stressful jobs.
The alcohol measure used, drinks per week, is admittedly crude. More detailed alcohol data was not available in this data set, and ideally, we would have obtained information on quantity and frequency of drinking, distribution of drinking pattern over the week, and alcohol content. This relatively general measure could have allowed for more variation than with a more specific alcohol measure/group of measures making it more difficult to determine statistical significance. A more detailed alcohol consumption measure should be included in future research.
Notwithstanding such issues, this study is one of the first to attempt to relate behavioral factors such as smoking and alcohol use to overall mortality in a blue-collar occupational cohort setting. The distinct differences in survival curves found between smokers and nonsmokers may point to stress and coping issues that can be addressed in future research.
Acknowledgement
Funding Funding for this study was received from the California Tobacco-related Disease Research Program, University of California Office of the President, Grant 14-RT-0116, Dr. Carol Cunradi, Principal Investigator.
References
- 1.Tse JLM, Flin R, Mearns K. Bus driver well-being review: 50 years of research. Transp Res Part F Traffic Psychol Behav. 2006;9:89–114. [DOI]
- 2.Rosengren A, Anderson K, Wilhelmsen L. Risk of coronary heart disease in middle-aged male bus and tram drivers compared to men in other occupations: a prospective study. Int J Epidemiol. 1991;20:82–87. [DOI] [PubMed]
- 3.Winkleby MA, Ragland DR, Syme SL. Excess risk of sickness and disease in bus drivers: a review and synthesis of epidemiological studies. Int J Epidemiol. 1988;17:255–261. [DOI] [PubMed]
- 4.Winkleby MA, Ragland DR, Syme SL. Self-reported stressors and hypertension: evidence of an inverse association. Am J Epidemiol. 1988;127:124–133. [DOI] [PubMed]
- 5.Netterstrom B, Laursen P. Incidence and prevalence of ischemic heart disease among urban bus drivers in Copenhagen. Scand J Soc Med. 1981;9:75–79. [DOI] [PubMed]
- 6.Hennessy DA, Wiesenthal DL. The relationship between traffic congestion, driver stress and direct versus indirect coping behaviors. Ergonomics. 1991;40:348–361.
- 7.Hennessy DA, Wiesenthal DL. Traffic congestion, driver stress, and driver aggression. Aggress Behav. 1999;25:409–423. [DOI]
- 8.Rimm EB, Klatsky A, Grobbee D, Stampfer MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits. BMJ. 1996;312(7033):731–736. [DOI] [PMC free article] [PubMed]
- 9.Gaziano JM, Buring JE, Breslow JL, et al. Moderate alcohol intake, increased levels of high-density lipoprotein and its subfractions, and decreased risk of myocardial infarction. N Engl J Med. 1993;329(25):1829–1834. [DOI] [PubMed]
- 10.Skog OJ. The J-curve, causality and public health. Addiction. 1995;90(4):490–492; discussion 493–498. [DOI] [PubMed]
- 11.Criqui MH. Do known cardiovascular risk factors mediate the effect of alcohol on cardiovascular disease. Novartis Found Symp. 1998;216:159–167; discussion 167–172. [DOI] [PubMed]
- 12.Maclure M. Demonstration of deductive meta-analyses: ethanol intake and risk of myocardial infarction. Epidemiol Rev. 1993;15(2):328–351. [DOI] [PubMed]
- 13.Ragland DR, Greiner BA, Krause N, Holman BL, Fisher JM. Occupational and non-occupational correlates of alcohol consumption in urban transit operators. Prev Med. 1995;24:634–645. [DOI] [PubMed]
- 14.Greiner BA, Krause N, Ragland DR, Fisher JM. Objective stress factors, accidents, and absenteeism in transit operators: a theoretical framework and empirical evidence. J Occup Health Psychol. 1998;3:130–146. [DOI] [PubMed]
- 15.Cunradi CB, Greiner BA, Ragland DR, Fisher JM. Burnout and alcohol problems among urban transit operators in San Francisco. Addict Behav. 2003;28:91–109. [DOI] [PubMed]
- 16.Maciulyte N. Bus driver’s health and conditions of work. Symposium conducted at the European Centre for Occupational Health, Safety and the Environment, Kaunas, Lithuania. 2000.
- 17.Bang KM, Kim JH. Prevalence of cigarette smoking by occupation and industry in the United States. Am J Ind Med. 2001;40:233–239. [DOI] [PubMed]
- 18.Stockwell T, Chikritzhs T, Bostrom A, et al. Alcohol-caused mortality in Australia and Canada: scenario analyses using different assumptions about cardiac benefit. J Stud Alcohol Drugs. 2007;68(3):345–352. [DOI] [PubMed]
- 19.Greenfield TK, Rehm J, Rogers JD. Effects of depression and social integration on the relationship between alcohol consumption and all-cause mortality. Addiction. 2002;97:29–38. [DOI] [PubMed]
- 20.Rehm J, Fichter MM, Elton M. Effects of mortality of alcohol consumption, smoking, physical activity, and close personal relationships. Addiction. 1993;88:101–112. [DOI] [PubMed]
- 21.Sempos CT, Rehm J, Wu T, Crespo CJ, Trevisan M. Average volume of alcohol consumption and all-cause mortality in African-Americans: the NHEFS cohort. Alcohol Clin Exp Res. 2003;27:88–92. [DOI] [PubMed]
- 22.Ragland DR, Greiner BA, Yen IH, Fisher JM. Occupational stress factors and alcohol-related behavior in urban transit operators. Alcohol Clin Exp Res. 2000;24:1011–1019. [DOI] [PubMed]