Abstract
Objective
To examine prospectively the natural course of bulimia nervosa and eating disorder not otherwise specified (EDNOS) and to test for the effects of personality disorder psychopathology on remission and relapse.
Method
Subjects were 92 female patients with current bulimia nervosa (N = 23) or EDNOS (N = 69) at baseline enrollment in the Collaborative Longitudinal Personality Disorders Study. Axis I psychiatric disorders (including eating disorders) were assessed with the Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Version, and personality disorders were assessed with the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV). The course of eating disorders was assessed with the Longitudinal Interval Follow-Up Evaluation and the course of personality disorders with the Follow-Along version of the DIPD-IV at 6 and 12 months and then yearly through 60 months. The study was conducted from July 1996 through June 2005.
Results
Probability of remission by 60 months was 74% for bulimia nervosa and 83% for EDNOS, and probability of relapse among those with a remission was 47% for bulimia nervosa and 42% for EDNOS. Patients with and without personality disorders did not differ in probability of remission. Cox proportional hazards regression analyses revealed that bulimia nervosa and EDNOS did not differ significantly in time to remission and that personality disorder comorbidity did not significantly predict time to remission. Analyses using proportional hazards regression with time-varying covariates revealed that dimensional changes in personality disorders were minimally related to either remission or relapse in these eating disorders.
Conclusions
The 5-year natural course of bulimia nervosa and EDNOS differed little with both eating disorder categories showing similar patterns of remissions and relapses. These findings suggest the clinical significance of EDNOS and the need for further research on this most common but least studied eating disorder. The natural course of bulimia nervosa and EDNOS does not appear to be influenced significantly by the presence, severity, or time-varying changes of co-occurring personality disorder psychopathology.
Although several studies have investigated the course of eating disorders,1–5 these are mostly treatment-outcome studies. Notable exceptions include the long-term ongoing study of bulimia nervosa and anorexia nervosa by Herzog and colleagues,6 the 5-year naturalistic community-based follow-up study of bulimia nervosa and binge eating disorder—a specific example of eating disorder not otherwise specified (EDNOS)—by Fairburn and colleagues,7 and the follow-up study of a mixed clinical/community sample of anorexia nervosa, bulimia nervosa, and EDNOS by Milos and colleagues.8 Herzog et al.,6 in their study of the natural course and outcome at 7.5 years of women with bulimia nervosa and anorexia nervosa, reported that anorexia nervosa had a significantly lower recovery rate than bulimia nervosa. In terms of prognostic factors, anorexia nervosa diagnosis, including duration of anorexia nervosa episode and lower percentage adult body weight, predicted poorer outcome, whereas no predictors were identified for bulimia nervosa recovery or relapse.6
Take-Home Points.
The natural course of bulimia nervosa and eating disorder not otherwise specified (EDNOS) differs little over a 5-year period.
Patients with bulimia nervosa and EDNOS have remission rates of roughly 74% and 83% and relapse rates of roughly 47% and 42%, respectively over 5-year follow-up.
The natural course of bulimia nervosa and EDNOS does not appear to be influenced by personality disorder psychopathology.
While it is well established that anorexia nervosa has a worse course9 than other eating disorders such as bulimia nervosa,1–3 questions remain regarding the natural course of bulimia nervosa and EDNOS. Unlike most other psychiatric disorders in the DSM-IV, the NOS category (EDNOS) is by far the most prevalent category of eating disorders in most outpatient settings10,11 but is also the least studied despite its clinical significance.12–14 Indeed, except for the specific example of binge eating disorder,15 EDNOS as a general category has received strikingly little research attention. It is important to emphasize, however, that EDNOS, unlike many other NOS categories, does not appear to simply reflect a “threshold” issue.16 Indeed, Fairburn and Bohn,12 in their recent review of the available data, emphasized that most cases of EDNOS reflect “mixed” eating disorder symptoms rather than just falling short (“subthreshold”) on a particular criterion (e.g., binge frequency or weight.). Thus, empirical studies of EDNOS, a mixed eating disorder construct supposedly capturing clinical significance, represent a research priority, especially in light of the future DSM-V.
Several recent longitudinal studies of bulimia nervosa and EDNOS are noteworthy. Fairburn et al.7 reported that the 5-year natural course of bulimia nervosa was significantly worse than that for binge eating disorder (an example of EDNOS) in a young female community-based sample, while Ben-Tovim and colleagues1 reported that the 5-year course of bulimia nervosa and EDNOS was nearly identical (remission rates of 74% and 78%, respectively). The assessment methods used in these studies of bulimia nervosa and EDNOS,1,7 while clinically sound, utilized cross-sectional (“dipstick”) methods. Thus, unlike the Herzog et al.6 study of bulimia nervosa and anorexia nervosa, no information is available on periods between the assessments. In our initial analysis of the natural course of eating disorders,17 using data from the first 24 months of prospective follow-up performed as part of the Collaborative Longitudinal Personality Disorders Study,18,19 we reported that over the short-term, bulimia nervosa had a worse course than EDNOS. Specifically, we found that the probability of remission was 40% for bulimia nervosa and 59% for EDNOS. This mixed literature clearly indicates the need for additional investigation of the longer-term course of bulimia nervosa and EDNOS that would also allow for examination of relapses in addition to remissions.
Another related pressing research need is the identification of prognostic factors. While some predictors have emerged for anorexia nervosa,5,6 reliable predictors for the course or outcome of bulimia nervosa have not been identified6 although there have been hints that general psychosocial and self-esteem deficits may predict poorer outcomes.1,20 In the case of EDNOS, Ben-Tovim and colleagues1 were unable to identify any predictors of 5-year outcomes. Since personality disorders and eating disorders frequently co-occur21 and research has found that personality disorders have a negative impact on the course of some psychiatric disorders,22,23 this line of investigation seemed indicated to correct many substantial methodological limitations inherent in the existing literature.24 In our initial 24-month study,17 we found that the 24-month natural course of bulimia nervosa and EDNOS was not influenced significantly by the presence of or time-varying changes in personality disorders.
The present study examined prospectively the 5-year natural course of bulimia nervosa and EDNOS and tested for the effects of personality disorder psychopathology on remission and relapse. The present study extends our initial 24-month analysis of remission17 to 60 months and considers the following additional questions: (1) What is the pattern of relapses, as well as remissions, in patients with bulimia nervosa and EDNOS? and (2) In addition to the presence of personality disorder, what are the effects of time-varying changes in personality disorder psychopathology on the pattern and timing of remissions and relapses? Thus, rather than focusing on personality disorder categories (as in our earlier 2-year study17), we focused on number of personality disorder criteria since this dimensional approach may be both more conceptually relevant and empirically valid25–27 and it provides greater statistical power.
Method
Participants
Participants for this study were enrolled in the Collaborative Longitudinal Personality Disorders Study, an on-going National Institute of Mental Health–funded, multisite, prospective naturalistic study. The overall study aims, design, assessment methodology, and the demographic and clinical characteristics of the participants have been previously reported.18,19 Briefly, the Collaborative Longitudinal Personality Disorders Study enrolled a total of 668 participants aged 18 to 45 years with at least 1 of 4 study personality disorders (schizotypal personality disorder, borderline personality disorder, avoidant personality disorder, or obsessive-compulsive personality disorder) or with (current) major depressive disorder without any personality disorder. Exclusion criteria included schizophrenia and schizoaffective disorders; active psychosis; confusional states due to organic disorders, post–electroconvulsive therapy status, or substance intoxication or acute withdrawal; IQ estimated below 85; or inability to read English. Of the 668 participants, 64% were women and 36% were men. In terms of ethnicity, 76% were white, 11% were African American, 9% were Hispanic American, and 4% were “other ethnicity.” Mean age was 32.8 (SD = 8.1) years. Participants were generally well distributed across the social classes except for the relatively small representation from the lowest socio-economic class. Forty-five percent were outpatients in a variety of mental health settings, 11% were psychiatric inpatients, 5% were from medical settings, and 39% were self-referred (from postings and advertisements) and were either in psychiatric treatment or seeking such. This study, conducted from July 1996 through June 2005, received complete institutional review board review and approval at all participating sites. All participants signed written informed consent after procedures had been fully explained.
The current report is based on all 92 female participants who met criteria for either current bulimia nervosa or EDNOS at baseline entry into the Collaborative Longitudinal Personality Disorders Study and had follow-up data. We focused on women in this report since the majority of eating disorder cases are female plus the limited number of men with current eating disorder diagnoses and follow-up data (N = 11) precluded meaningful analysis. A previous report28 details lifetime co-occurrence rates of Axis I psychiatric and Axis II personality disorders for all patients with eating disorders enrolled in Collaborative Longitudinal Personality Disorders Study, and the report by Grilo et al.17 details 2-year outcomes for remission from eating disorders. Of the 92 female patients, 23 met criteria for bulimia nervosa and 69 met criteria for EDNOS. The bulimia nervosa and EDNOS groups did not differ significantly in lifetime rates of anorexia nervosa. Specifically, of the 23 patients with bulimia nervosa, 3 (13%) had a lifetime diagnosis of anorexia nervosa versus 8 (12%) of the 69 patients with EDNOS; in addition, 7 (10%) of the 69 EDNOS patients had a lifetime diagnosis of bulimia nervosa. The bulimia nervosa and EDNOS patients did not differ significantly in age (mean = 30.6 [SD = 6.6] years versus mean = 31.6 [SD = 8.8] years, respectively).
Procedures
Baseline diagnostic evaluation
All participants were interviewed in person by experienced interviewers with master's or doctoral degrees in a mental health discipline. Research interviewers underwent extensive standardized training to achieve reliability in the administration of the major diagnostic measures for both Axis I and II disorders.29 The research interviewers were monitored and received regular on-going supervision by the investigators at each site, as well as supervision across sites to prevent drift over time.
Interviewers administered the Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Version (SCID-I/P30) to assess Axis I psychiatric disorders (including eating disorders) and the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV31) to assess all Axis II personality disorder diagnoses and criteria.
Follow-Up evaluations
Participants were reinterviewed at 6 and 12 months and then yearly thereafter following the baseline assessment. The course of eating disorders (bulimia nervosa and EDNOS) was assessed using the Longitudinal Interval Follow-Up Evaluation (LIFE32). The course of personality disorders was assessed using a modified version of the DIPD-IV—the Follow-Along version (DIPD-FA).31
Assessment Instruments
Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Version (SCID-I/P)
The SCID-I/P30 is a widely used diagnostic interview to assess current and lifetime Axis I psychiatric disorders. When assessing the eating disorder diagnoses, the SCID-I/P and DSM-IV criteria and principles were strictly adhered to. The SCID-I/P specifically assesses bulimia nervosa, and the diagnosis of EDNOS was assigned, following the DSM-IV principles, if eating disorder features were present and resulted in clinically meaningful levels of impairment (despite the failure to fulfill full diagnostic criteria for the “formal” eating disorder diagnoses of bulimia nervosa or anorexia nervosa). This approach, following the DSM-IV, is the same as used in other recent studies of eating disorders that have considered EDNOS.8,33 In the current study, median κ coefficients for interrater reliability for Axis I psychiatric disorders ranged from 0.57 to 1.0; median κ for eating disorders was 0.77.29
Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV)
The DIPD-IV31 is a semistructured diagnostic interview for the assessment of all DSM-IV Axis II personality disorders and criteria. Each of the criteria for all diagnoses is assessed with 1 or more questions, which are then rated on a 3-point scale (0 = not present; 1 = present but of uncertain clinical significance; 2 = present and clinically significant). The DIPD-IV requires that the criteria be present and pervasive for at least 2 years, and that they be characteristic of the person for most of his or her adult life in order to be counted toward a diagnosis. In the present study, the interrater reliability κ's (based on 84 pairs of raters) for 12 personality disorders (10 formal and 2 research categories) ranged from 0.58 to l.0.29 Kappa coefficients for interrater reliability for the 4 personality disorders of primary interest ranged from 0.68 for borderline personality disorder to 0.73 for avoidant personality disorder and 100% agreement for schizotypal personality disorder, and test-retest reliability κ's (based on 52 cases) ranged from 0.69 for borderline personality disorder to 0.74 for obsessive-compulsive personality disorder.
Longitudinal Interval Follow-Up Evaluation
The LIFE32 is a semistructured interview rating system with demonstrated reliability and validity34 for assessing the longitudinal course of mental disorders. The LIFE has served as the primary measure of major longitudinal studies of anorexia nervosa and bulimia nervosa5,6 and other Axis I disorders, including depressive disorders22,35 and anxiety disorders.34 In the present study, the LIFE was administered to measure the presence and severity of psychopathology on a weekly basis. In the LIFE, the severity of psychopathology is quantified on weekly Psychiatric Status Ratings (PSRs), which are made for each Axis I disorder present. For eating disorder, PSRs are based on the following 3-point scale: PSR = 1 signifies no symptoms; PSR = 2 corresponds to subthreshold symptoms with up to moderate impairment in functioning; PSR = 3 corresponds to symptoms meeting full criteria for diagnosis. In this study, the official LIFE trainers at Brown University provided training and continuous consultation in its use.
Definition of Remission
Remission from eating disorders (bulimia nervosa and EDNOS) was defined as 8 consecutive weeks with PSR ratings on the LIFE of less than 2 (for any type of eating disorder diagnosis). This definition of remission (PSR < 2) for eating disorders parallels that used in studies of other Axis I psychiatric disorders22,34,35 and was used in our initial 2-year study of remission of eating disorders.17
Data Analyses
Statistical analyses were conducted using Statistical Analysis Systems (SAS) software version 8.0,36 using PROC FREQ, PROC ANOVA, PROC LIFETEST, and PROC PHREG. Depending on the type of variables (continuous or discrete), analysis of variance or χ2 analyses were performed to evaluate demographic and clinical differences between groups.
Time to remission from eating disorder and relapse to eating disorder
Life table survival methods37 were used to analyze time to remission during the 60-month follow-up period. The same methods were then used to analyze time to relapse among those eating disorder cases that had achieved a remission. The Kaplan-Meier38 method, which is well suited for analyzing longitudinal data for psychiatric illnesses,39 was used to estimate cumulative remission rates and cumulative relapse rates. Cox proportional hazards regression tests for significance40 were used for the omnibus predictor analysis of time to eating disorder remission that jointly considered the presence or absence of a personality disorder diagnosis along with 3 predictor variables selected to reflect severity (number of Axis I psychiatric disorders, earliest age at onset of eating disorder, and duration of eating disorder).
Dynamic time-varying dimensional personality disorder effects on eating disorder remission and relapse
We examined how the course of personality disorders affects the course of eating disorders (i.e., both remission and relapse). We focused on the 4 personality disorders targeted by the Collaborative Longitudinal Personality Disorders Study (borderline personality disorder, avoidant personality disorder, obsessive-compulsive personality disorder, and schizotypal personality disorder) in relation to remission from eating disorders and subsequently to relapse to eating disorders. Here we specifically focused on the number of personality disorder criteria since this dimensional approach may be both more conceptually relevant and empirically valid.25–27 Analyses were performed on follow-up data obtained using the LIFE for eating disorders and the DIPD-FA for the personality disorders. For the eating disorder analysis, we collapsed together the 2 eating disorders (bulimia nervosa and EDNOS) given the sample size and the lack of any overall differences in time to remission and in time to relapse between the 2 eating disorders.
Proportional hazards regression analyses with time-varying covariates were used to test dimensional changes in personality disorder psychopathology as predictors of changes in eating disorders over time—i.e., remissions and relapses. All proportional hazards regression analyses were performed with 3 covariates that reflected severity (number of Axis I psychiatric disorders, earliest age at onset of eating disorder, and duration of eating disorder).
Results
Remission and Relapse Rates for Bulimia Nervosa and EDNOS Over 60 Months
Figure 1 represents the survival curves showing time to remission for bulimia nervosa and EDNOS. Of the 23 subjects with bulimia nervosa, 17 had a remission during the 60-month follow-up period for an overall remission rate of 74%. Of the 69 subjects with EDNOS, 57 had a remission, for an overall remission rate of 83%. A comparison of the likelihood of remission between the 2 eating disorders revealed a nonsignificant trend toward a higher likelihood of remission for EDNOS (Wilcoxon χ2 = 3.17, p = .08).
Figure 1.
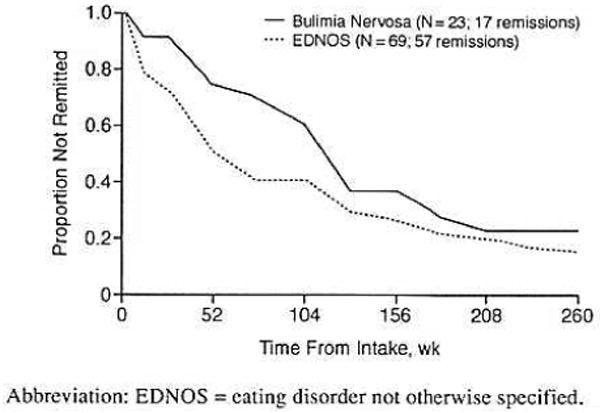
Time to Eating Disorder Remission by EDNOS Versus Bulimia Nervosa Status
Figure 2 represents the survival curves showing time to relapse for those patients who had achieved a remission. For bulimia nervosa, 8 of the 17 remitted patients subsequently relapsed for an overall relapse rate of 47%. For EDNOS, 24 of the 57 remitted patients subsequently relapsed for an overall relapse rate of 42%. There was no significant difference in likelihood to relapse between the 2 eating disorders (Wilcoxon χ2 = 0.02, p = .88).
Figure 2.
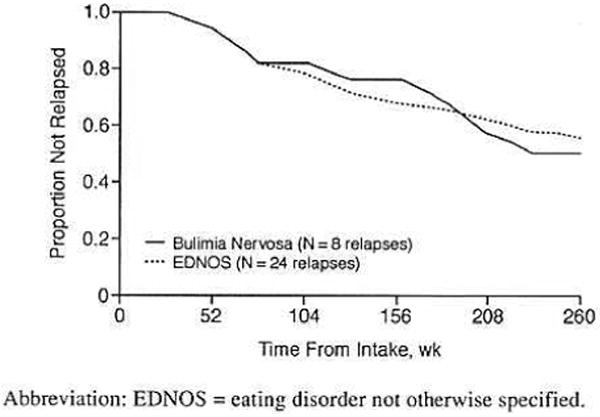
Time to Eating Disorder Relapse by EDNOS Versus Bulimia Nervosa Status
Time to Eating Disorder Remission by Personality Disorder Comorbidity
Time to remission from eating disorders was examined as a function of personality disorder comorbidity. Overall, the mean number of personality disorder diagnoses met by the participants was 1.8 (SD = 1.1); patients with bulimia nervosa and EDNOS did not differ significantly in the mean number of co-occurring personality disorders (mean = 1.8 [SD = 1.0] versus 1.8 [SD = 1.2]; F = 0.17, df = 90, p = .86). The bulimia nervosa and EDNOS groups also did not differ significantly in number of co-occurring current Axis I psychiatric disorders (mean = 3.3 [SD = 1.6] versus mean = 3.1 [SD = 1.5]; F = 0.43, df = 90, p = .67). These findings, along with the similar survival curves over 60 months (Figure 1) and the small number of bulimia nervosa cases, led us to group both bulimia nervosa and EDNOS in these analyses. Overall in the eating disorder patients, 15 had no personality disorder and 77 met criteria for at least 1 personality disorder. Patients with bulimia nervosa and EDNOS did not differ significantly in the distribution of grouping by personality disorder. Survival curves (time to remission) for eating disorders as a function of personality disorder co-occurrence (i.e., no personality disorder versus at least 1 personality disorder) are shown in Figure 3. Personality disorder comorbidity (along with Axis I psychiatric comorbidity, age at onset, and duration of eating disorder) was unrelated to time to remission from eating disorders (Wilcoxon χ2 = 0.13, p = .72).
Figure 3.
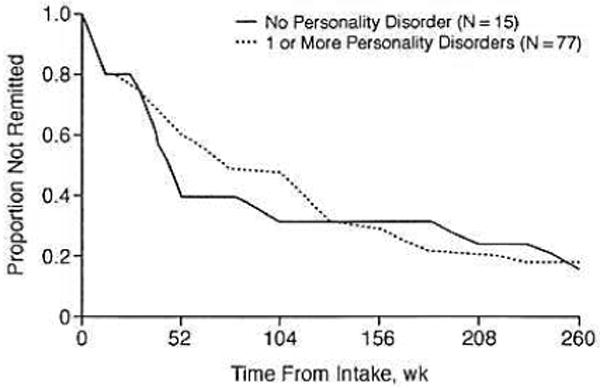
Time to Eating Disorder Remission by No Personality Disorder Versus 1 or More Personality Disorders Status
Personality Disorder Criteria as Time-Varying Predictors of Eating Disorder Remission and Relapse
Table 1 summarizes analyses for dimensional variations in personality disorder criteria (on the DIPD-FA) as predictors of remission in eating disorders (on the LIFE). Table 2 summarizes the analyses for dimensional variations in personality disorder criteria as predictors of relapse in eating disorder patients that had previously achieved a remission from eating disorder. Proportional hazards regression analyses with time-varying covariates were used. Table 1 (for remission) and Table 2 (for relapse) both include the risk ratio and the p value for a 2-tailed test in which the risk ratio is different from 1.0. The risk ratio is a good index of effect size (risk ratio of 1.0 indicates no association between the variables).
Table 1.
Change in Number of Personality Disorder Criteria as Time-Varying Predictors of Remission From Eating Disorders
| Eating Disorder Remissiona | ||
|---|---|---|
| Personality Disorder | Risk Ratio | p Valueb |
| Borderline | 0.96 | .35 |
| Avoidant | 0.90 | .02 |
| Obsessive-compulsive | 0.97 | .57 |
| Schizotypal | 0.92 | .21 |
Eating disorder denotes all eating disorders (combined bulimia nervosa and eating disorder not otherwise specified). Of the 92 patients with eating disorders, 74 achieved a remission during the 5-year period of prospective follow-up.
p Value denotes significance level for 2-tailed test.
Table 2.
Change in Number of Personality Disorder Criteria as Time-Varying Predictors of Relapse to Eating Disorder
| Relapse to Eating Disordera | ||
|---|---|---|
| Personality Disorder | Risk Ratio | p Valueb |
| Borderline | 1.13 | .09 |
| Avoidant | 1.03 | .76 |
| Obsessive-compulsive | 1.07 | .59 |
| Schizotypal | 1.08 | .55 |
Eating Disorder denotes all eating disorders (combined bulimia nervosa and eating disorder not otherwise specified). Of the 74 patients with eating disorders who had a remission, 32 relapsed back to eating disorder status during the 5-year period of prospective follow-up.
p Value denotes significance level for 2-tailed test.
As summarized in Tables 1 and 2, the findings suggest that most time-varying dimensional changes in personality disorder criteria were unrelated to eating disorder remission or to eating disorder relapse. Of the 4 sets of Cox proportional hazards regression analyses of dimensional changes in personality disorder predicting eating disorder remission (which included covariates of Axis I comorbidity, age at onset, and duration of eating disorder), only the one for avoidant personality disorder was statistically significant. For each avoidant personality disorder criterion increase during the month prior to the timing of the remission from eating disorder, the risk or chance of remission is decreased by 10%. Of the 4 analyses of dimensional changes in personality disorder predicting eating disorder relapse, none was statistically significant. From a clinical perspective, 3 of the risk ratios were essentially 1.0, which indicates no association, and the risk ratio for borderline personality disorder changes was only 1.1, which reflects only a 10% change in risk.
Discussion
The present report represents a novel contribution to the literature on the association between personality disorders and eating disorders and addresses 2 important issues.13,24 First, the 5-year natural course of bulimia nervosa and EDNOS differed little with both eating disorder categories showing similar patterns of remissions and relapses. These findings suggest the clinical significance of EDNOS and the need for further research on this most common but least studied eating disorder.12 Second, the natural course (i.e., patterns and timing of remissions and relapses) of bulimia nervosa and EDNOS over 5-year prospective follow-up does not appear to be influenced significantly by the presence, severity, or time-varying dimensional changes of co-occurring personality disorder psychopathology.
Over the 5-year period of prospective follow-up in this study of natural course and outcome, the probability of remission was 74% for bulimia nervosa and 83% for EDNOS. These remission rates based on the LIFE-FA32 are nearly identical to those also reported for bulimia nervosa (74%) and EDNOS (78%) in a 5-year study of treatment outcomes performed in Australia based on different methods (clinical interviews and self-report measures).1 Among those patients who achieved a remission, relapse was not uncommon and was observed in 47% of bulimia nervosa cases and 42% of EDNOS cases within the 5-year follow-up study. These findings are generally consistent with those of a recent follow-up study conducted in Zurich,8 which documented an overall low remission rate over a 30-month follow-up. In that study, the course of eating disorder seemed best characterized by a fluctuating course over time with instances of remissions and relapses both within and between diagnoses, leading the authors to suggest that the different eating disorders may have common causal and maintaining factors.8 Collectively, these findings suggest that EDNOS is a clinically meaningful category insofar as it appears to have the same natural course as bulimia nervosa over a 5-year period. Thus, the current DSM-IV EDNOS construct, although flawed, does appear to capture a clinically meaningful group of persons with eating disorder–related problems. The challenge for DSM-V is to define more useful categories for clinicians and researchers. Our findings here support the importance of this “mixed” clinical category, and additional empirical research is needed to inform the efforts toward DSM-V and improving eating disorder nosology.12
Our findings indicate that the patterns and timing of remissions and relapses of bulimia nervosa and EDNOS do not appear to be influenced significantly by the presence, severity, or time-varying dimensional changes of co-occurring personality disorder psychopathology. We note that Ben-Tovim and colleagues1—who found that nature of treatment was unrelated to outcome—were unable to identify predictors for EDNOS outcome although some evidence was found in bulimia nervosa for the prognostic utility of psychosocial deficits. Although the lack of association between personality disorder psychology and course of eating disorders may be clinically counter-intuitive, especially since it is at odds with findings for other psychiatric disorders such as major depression,22 we note that Grilo,24 in a previous critical review, concluded that personality disorder represents only a weak prognostic predictor of eating disorder outcome. We previously noted that although eating disorders and personality disorders frequently co-occur, they do not differentially co-occur across diagnoses, and thus speculated that this co-occurrence is inconsistent with meaningful comorbidity.28 Our findings presented here for personality disorder psychopathology are clearly inconsistent with spectrum models (i.e., that eating disorder and personality disorder are manifestations of shared underlying pathology). It is important to note that the absence of longitudinal associations between the eating disorders and personality disorders does not rule out the possibility of other causal relationships.41
Thus, our findings suggest that bulimia nervosa and EDNOS arc characterized by considerable independence or uniqueness from categorical and dimensional aspects of personality disorder psychopathology as reflected in the DSM-IV. Of course, it is quite possible that other personality variables or traits42,43 not considered in this study might have different patterns of associations with eating disorders.24,44 Also, it is possible that such forms of personality disorder psychopathology (e.g., obsessionality) might be related to anorexia nervosa,45 which was not included in our study. Grilo24 speculated, however, that personality disorder psychopathology may represent a more meaningful predictor of longer-term psychiatric and psychosocial impairment in patients with bulimia nervosa.46,47 For example, early factor analytic work with bulimia nervosa patients characterized eating-related psychopathology and general psychological disturbances as separate “semiautonomous” components.48 A recent study predicting 6-year outcomes of eating disorders using structural equation modeling is most relevant here. Fichter and colleagues20 found that bulimia nervosa and binge eating disorder were quite similar to each other but different from anorexia nervosa, and structural equation modeling revealed almost completely different predictions for eating disorder psychopathology outcomes versus non–eating disorder (i.e., general) psychopathology.
We briefly note several methodological issues as a context for considering our findings. First, our findings pertain to female treatment-seeking patients who were recruited for a longitudinal study with a primary focus on personality disorder and major depressive disorder. The generalizability of the findings regarding course and outcome to males is uncertain as is the generalizability to eating disorder patients who present to eating disorder or specialty clinics. Given our recruitment focus, the rates of personality disorder in our eating disorder patients are higher than reported for some clinic samples (see Grilo24 for discussion of the extent and variability in co-occurrences among eating disorders and personality disorders across recruitment methods.) Thus, our findings may not generalize to community samples or to eating disorder cases that seek treatment at specialty clinics for eating disorders, which might be prone to different forms of clinic biases.49,50 Although we considered Axis I comorbidity in our multivariate analyses, we did not exhaustively explore other potential confounding factors, such as specific psychiatric disorders including major depressive disorder. We note, however, that Ben-Tovim and colleagues1 previously documented that depression was unrelated to the 5-year course of either bulimia nervosa or EDNOS. In addition, our sample size precluded us from performing analyses on personality disorder diagnoses predicting relapse and the time-varying dimensional analyses of personality disorder criteria separately for bulimia nervosa and EDNOS. Although it is possible that our sample size may have prevented us from detecting significant effects of a small magnitude, we note that the hazard ratios for dimensional changes in personality disorder predicting changes (remissions and relapses) in eating disorders are very close to 1.0, which is indicative of no association.
A methodological limitation concerns the nature and preciseness of our assessments for eating disorders. We relied on the LIFE, which was used in previous studies with eating disorders5,6 and represents the primary instrument in major longitudinal studies of several other Axis I disorders.22,35 Unfortunately, this assessment instrument did not allow us to identify specific examples of EDNOS, such as binge eating disorder, which is included as a research category in the DSM-IV. In addition, while it could be argued that other assessment instruments can produce more detailed and specific data regarding the features of eating disorders for specific points in time,7 these approaches do not lend themselves well to survival analyses and their considerable strengths.39 Regardless, our results that “large” differences in eating disorder (i.e., diagnostic remission and relapse) were unrelated to dimensional changes in personality disorders would not be expected to change if we had looked for “small” differences that other eating disorder assessment methods could provide.51,52 In addition, although the LIFE does not provide as detailed information about the attitudinal features of eating disorders as some other instruments,51 it does generate information specific enough to test the formal DSM-IV–based eating disorder diagnostic constructs.
Another limitation of naturalistic longitudinal studies of clinically ascertained subjects is the potential for confounding by treatment. In our initial analysis of treatment utilization, Bender and colleagues53 reported that major depressive disorder patients without personality disorder utilized significantly less treatment than patients with personality disorder and that the more severe forms of personality disorders (including patients with more assigned personality disorder) reported receiving the most treatment. Thus, consistent with most naturalistic studies,54 such findings suggest that the amount of treatment received is driven by the severity of the disorder. Indeed, in our earlier analysis of change and outcome of personality disorders,25 we found that higher treatment utilization was associated with less change in personality disorders. We note that the current study was designed to address the question of course of eating disorder in patients in real-world clinical settings and receiving treatments as applied in current practice, not with experimentally manipulated treatments (controlled treatment or efficacy trials). For example, in contrast to naturalistically delivered treatments in the community, which were found to be unrelated to EDNOS and bulimia nervosa,1 delivery of empirically supported treatments for these problems at specialty clinics tends to produce clinically robust outcomes.55,56
In summary, the 5-year natural course of bulimia nervosa and EDNOS differed little. Both of these eating disorder categories showed similar rates and patterns of remissions and relapses over a 5-year period of prospective follow-up. These findings suggest the clinical significance of EDNOS and the need for further research on this broad category, which is by far the most common eating disorder diagnosis in clinical settings but remains the least studied. The patterns of remissions and relapses of these eating disorder categories did not appear to be influenced significantly by the presence or time-varying dimensional changes of co-occurring personality disorder psychopathology
Acknowledgments
This research was supported by the following grants from the National Institutes of Health: MH 50837, 50838, 50839, 50840, and 50850. Preparation of this article was also supported, in part, by the following National Institutes of Health grants: K24 DK070052 (Dr. Grilo), K01 AA 015137 (Dr. Pagano). K23 MH 073708 (Dr. Sanislow), and K05 MH 01645 (Dr. McGlashan).
Footnotes
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME article were asked to complete a statement regarding all relevant financial relationships between themselves or their spouse/partner and any commercial interest (i.e., any proprietary entity producing health care goods or services consumed by, or used on, patients) occurring within at least 12 months prior to joining this activity. The CME Institute has resolved any conflicts of interest that were identified. The disclosures are as follows: Drs. Grilo, Pagano, Skodol, Sanislow, McGlashan, Gunderson, and Stout have no personal affiliations or financial relationships with any proprietary entity producing health care goods or services consumed by, or used on, patients to disclose relative to the article.
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside U.S. Food and Drug Administration–approved labeling has been presented in this article.
Contributor Information
Carlos M. Grilo, Department of Psychiatry, Yale University School of Medicine, New Haven, Conn.
Maria E. Pagano, Department of Psychiatry, Case Western Reserve University, Cleveland, Ohio
Andrew E. Skodol, Department of Psychiatry, Columbia University, New York State Psychiatric Institute, New York
Charles A. Sanislow, Department of Psychiatry, Yale University School of Medicine, New Haven, Conn.
Thomas H. McGlashan, Department of Psychiatry, Yale University School of Medicine, New Haven, Conn.
John G. Gunderson, McLean Hospital, Belmont, and Harvard Medical School, Boston, Mass.
Robert L. Stout, Department of Psychiatry and Human Behavior, Brown University, and Decision Sciences Institute, Pacific Institute for Research and Evaluation, Providence, R.I.
References
- 1.Ben-Tovim DI, Walker K, Gilchrist P, et al. Outcome in patients with eating disorders: a 5-year study. Lancet. 2001;357:1254–1257. doi: 10.1016/S0140-6736(00)04406-8. [DOI] [PubMed] [Google Scholar]
- 2.Fichter MM, Quadflieg N. Twelve-year course and outcome of bulimia nervosa. Psychol Med. 2004;34:1395–1406. doi: 10.1017/s0033291704002673. [DOI] [PubMed] [Google Scholar]
- 3.Fichter MM, Quadflieg N, Hedlund S. Twelve-year course and outcome predictors of anorexia nervosa. Int J Eat Disord. 2006;39:87–100. doi: 10.1002/eat.20215. [DOI] [PubMed] [Google Scholar]
- 4.Keel PK, Mitchell JE, Miller KB, et al. Long-term outcome of bulimia nervosa. Arch Gen Psychiatry. 1999;56:63–69. doi: 10.1001/archpsyc.56.1.63. [DOI] [PubMed] [Google Scholar]
- 5.Strober M, Freeman R, Morrell W. The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int J Eat Disord. 1997;22:339–360. doi: 10.1002/(sici)1098-108x(199712)22:4<339::aid-eat1>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 6.Herzog DB, Dorer DJ, Keel PK, et al. Recovery and relapse in anorexia and bulimia nervosa: a 7.5-year follow-up study. J Am Acad Child Adolesc Psychiatry. 1999;38:829–837. doi: 10.1097/00004583-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Fairburn CG, Cooper Z, Doll HA, et al. The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry. 2000;57:659–665. doi: 10.1001/archpsyc.57.7.659. [DOI] [PubMed] [Google Scholar]
- 8.Milos G, Spindler A, Schnyder U, et al. Instability of eating disorder diagnoses: prospective study. Br J Psychiatry. 2005;187:573–578. doi: 10.1192/bjp.187.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinhausen HC. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry. 2002;159:1284–1293. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- 10.Ricca V, Mannucci E, Mezzani B, et al. Psychopathological and clinical features of outpatients with an eating disorder not otherwise specified. Eat Weight Disord. 2001;6:157–165. doi: 10.1007/BF03339765. [DOI] [PubMed] [Google Scholar]
- 11.Turner H, Bryant-Waugh R. Eating disorder not otherwise specified (EDNOS): profiles of clients presenting at a community eating disorder service. Eur Eat Disord Rev. 2004;12:18–26. [Google Scholar]
- 12.Fairburn CG, Bohn K. Eating disorder NOS (EDNOS): an example of the troublesome “Not Otherwise Specified” (NOS) category in the DSM-IV. Behav Res Ther. 2005;43:691–701. doi: 10.1016/j.brat.2004.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grilo CM, Devlin MJ, Cachelin FM, et al. Report of the National Institutes of Health Workshop on the development of research priorities in eating disorders. Psychopharmacol Bull. 1997;33:321–333. [PubMed] [Google Scholar]
- 14.Andersen AE, Bowers WA, Watson T. A slimming program for eating disorders not otherwise specified: reconceptualizing a confusing, residual diagnostic category. Psychiatr Clin North Am. 2001;24:271–280. doi: 10.1016/s0193-953x(05)70223-9. [DOI] [PubMed] [Google Scholar]
- 15.Allison KC, Grilo CM, Masheb RM, et al. Binge eating disorder and night eating syndrome: a comparative study of disordered eating. J Consult Clin Psychol. 2005;73:1107–1115. doi: 10.1037/0022-006X.73.6.1107. [DOI] [PubMed] [Google Scholar]
- 16.Thaw JM, Williamson DA, Martin CK. Impact of altering DSM-IV criteria for anorexia and bulimia nervosa on the base rates of eating disorder diagnoses. Eat Weight Disord. 2001;6:121–129. doi: 10.1007/BF03339761. [DOI] [PubMed] [Google Scholar]
- 17.Grilo CM, Sanislow CA, Shea MT, et al. The natural course of bulimia nervosa and eating disorder not otherwise specified is not influenced by personality disorders. Int J Eat Disord. 2003;34:319–330. doi: 10.1002/eat.10196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gunderson JG, Shea MT, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: development, aims, designs and sample characteristics. J Personal Disord. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- 19.McGlashan TH, Grilo CM, Skodol AE, et al. The collaborative longitudinal personality disorders study: baseline Axis I/II and Axis II/II co-occurrence. Acta Psychiatr Scand. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- 20.Fichter MM, Quadflieg N, Rehm J. Predicting the outcome of eating disorders using structural equation modeling. Int J Eat Disord. 2003;34:292–313. doi: 10.1002/eat.10193. [DOI] [PubMed] [Google Scholar]
- 21.Grilo CM, Levy KN, Becker DF, et al. DSM-III-R Axis I and II disorders in inpatients with eating disorders. Psychiatr Serv. 1996;47:426–429. doi: 10.1176/ps.47.4.426. [DOI] [PubMed] [Google Scholar]
- 22.Grilo CM, Sanislow CA, Shea MT, et al. Two-year prospective naturalistic study of remission from major depressive disorder as a function of personality disorder comorbidity. J Consult Clin Psychol. 2005;73:78–85. doi: 10.1037/0022-006X.73.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grilo CM, McGlashan TH. Stability and course of personality disorders. Curr Opin Psychiatry. 1999;12:157–162. [Google Scholar]
- 24.Grilo CM. Recent research of relationships among eating disorders and personality disorders. Curr Psychiatry Rep. 2002;4:18–24. doi: 10.1007/s11920-002-0007-8. [DOI] [PubMed] [Google Scholar]
- 25.Grilo CM, Shea MT, Sanislow CA, et al. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72:767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGlashan TH, Grilo CM, Sanislow CA, et al. Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: toward a hybrid model of Axis II disorders. Am J Psychiatry. 2005;162:883–889. doi: 10.1176/appi.ajp.162.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Skodol AE, Oldham JM, Bender DS, et al. Dimensional representations of DSM-IV personality disorders: relationships to functional impairment. Am J Psychiatry. 2005;162:1919–1925. doi: 10.1176/appi.ajp.162.10.1919. [DOI] [PubMed] [Google Scholar]
- 28.Grilo CM, Sanislow CA, Skodol AE, et al. Do eating disorders co-occur with personality disorders? Comparison groups matter. Int J Eat Disord. 2003;33:155–164. doi: 10.1002/eat.10123. [DOI] [PubMed] [Google Scholar]
- 29.Zanarini MC, Skodol AE, Bender D, et al. The Collaborative Longitudinal Personality Disorders Study: reliability of Axis I and II diagnoses. J Personal Disord. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) New York, NY: Biometrics Research, New York State Psychiatric Institute; 1996. [Google Scholar]
- 31.Zanarini MC, Frankenburg FR, Sickel AE, et al. The Diagnostic Interview for DSM-IV Personality Disorders. Belmont, Mass: McLean Hospital; 1996. [Google Scholar]
- 32.Keller MB, Lavori PW, Friedman B, et al. Longitudinal Interval Follow-Up Evaluation: comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 33.Rosenberger PH, Henderson KE, Grilo CM. Psychiatric disorder comorbidity and association with eating disorders in bariatric surgery patients: a cross-sectional study using structured interview-based diagnosis. J Clin Psychiatry. 2006;67:1080–1085. doi: 10.4088/jcp.v67n0710. [DOI] [PubMed] [Google Scholar]
- 34.Warshaw MG, Keller MB, Stout RL. Reliability and validity of the Longitudinal Interval Follow-Up Evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 35.Solomon DA, Keller MB, Leon AC, et al. Recovery from major depression: a 10-year prospective follow-up across multiple episodes. Arch Gen Psychiatry. 1997;54:1001–1006. doi: 10.1001/archpsyc.1997.01830230033005. [DOI] [PubMed] [Google Scholar]
- 36.SAS Institute Inc. SAS/STAT User's Guide. Version 8. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- 37.Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. New York, NY: John Wiley & Sons; 1980. [Google Scholar]
- 38.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 39.Fleiss JL, Dunner DL, Stallone F, et al. The life table: a method for analyzing longitudinal studies. Arch Gen Psychiatry. 1976;33:107–112. doi: 10.1001/archpsyc.1976.01770010067013. [DOI] [PubMed] [Google Scholar]
- 40.Cox DR. Regression models and life tables. J Royal Stat Soc. 1972;34:187–220. [Google Scholar]
- 41.Shea MT, Stout RL, Yen S, et al. Associations in the course of personality disorders and Axis I disorders over time. J Abnorm Psychol. 2004;113:499–508. doi: 10.1037/0021-843X.113.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Klump KL, Strober M, Bulik CM, et al. Personality characteristics of women before and after recovery from an eating disorder. Psychol Med. 2004;34:1407–1418. doi: 10.1017/s0033291704002442. [DOI] [PubMed] [Google Scholar]
- 43.Lilenfeld LR, Stein D, Bulik CM, et al. Personality traits among currently eating disordered, recovered and never ill first-degree female relatives of bulimic and control women. Psychol Med. 2000;30:1399–1410. doi: 10.1017/s0033291799002792. [DOI] [PubMed] [Google Scholar]
- 44.Lilenfeld LR, Wonderlich S, Riso LP, et al. Eating disorders and personality: a methodological and empirical review. Clin Psychol Rev. 2006;26:299–320. doi: 10.1016/j.cpr.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 45.Lilenfeld LR, Kaye WH, Greeno CG, et al. A controlled family study of anorexia nervosa and bulimia nervosa: psychiatric disorders in first-degree relatives and effects of proband comorbidity. Arch Gen Psychiatry. 1998;55:603–610. doi: 10.1001/archpsyc.55.7.603. [DOI] [PubMed] [Google Scholar]
- 46.Steiger H, Stotland S. Prospective study of outcome in bulimics as a function of Axis-II co-morbidity: long-term responses on eating and psychiatric symptoms. Int J Eat Disord. 1996;20:149–161. doi: 10.1002/(SICI)1098-108X(199609)20:2<149::AID-EAT5>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 47.Steiger H, Stotland S, Houle L. Prognostic implications of stable versus transient “borderline features” in bulimic patients. J Clin Psychiatry. 1994;55:206–214. [PubMed] [Google Scholar]
- 48.Gleaves DH, Williamson DA, Barker SE. Confirmatory factor analysis of a multidimensional model of bulimia nervosa. J Abnorm Psychol. 1993;102:173–176. doi: 10.1037//0021-843x.102.1.173. [DOI] [PubMed] [Google Scholar]
- 49.Fairburn CG, Welch SL, Norman P, et al. Bias and bulimia nervosa: how typical are clinic cases? Am J Psychiatry. 1996;153:386–391. doi: 10.1176/ajp.153.3.386. [DOI] [PubMed] [Google Scholar]
- 50.Grilo CM, Lozano C, Masheb RM. Ethnicity and sampling bias in binge eating disorder: black women who seek treatment have different characteristics than those who do not. Int J Eat Disord. 2005;38:257–262. doi: 10.1002/eat.20183. [DOI] [PubMed] [Google Scholar]
- 51.Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J Consult Clin Psychol. 2001;69:317–322. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- 52.Grilo CM, Masheb RM, Wilson GT. Different methods for assessing the features of eating disorders in patients with binge eating disorder: a replication. Obes Res. 2001;9:418–422. doi: 10.1038/oby.2001.55. [DOI] [PubMed] [Google Scholar]
- 53.Bender DS, Dolan RT, Skodol AE, et al. Treatment utilization by patients with personality disorders. Am J Psychiatry. 2001;158:295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- 54.Cochran W. Planning and analysis of observational studies. New York, NY: John Wiley & Sons; 1983. [Google Scholar]
- 55.Grilo CM, Masheb R, Wilson GT. Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of BED: randomized double-blind placebo-controlled trial. Biol Psychiatry. 2005;57:301–309. doi: 10.1016/j.biopsych.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 56.Wilson GT, Grilo CM, Vitousek K. Psychological treatments for eating disorders. Am Psychol. doi: 10.1037/0003-066X.62.3.199. In press. [DOI] [PubMed] [Google Scholar]


