Abstract
Effects of lifetime histories of grandparental (G1) and parental (G2) major depressive disorder (MDD) on children's (G3) internalizing problems were investigated among 267 G3 children (ages 2–18 years) who received Child Behavior Checklist (CBCL) ratings and had diagnostic data available on 267 biological G2 parents and 527 biological G1 grandparents. Results indicated that G1 MDD conferred risk for G2 MDD, but not for G3 CBCL scores. G2 MDD predicted higher G3 Internalizing and Anxious/Depressed scores. Also, there was an interaction between G1 MDD and G2 MDD in predicting higher G3 Anxious/Depressed scores such that scores were highest among children with both depressed parents and grandparents. These effects were robust to statistical adjustments for status variables and parental relationship measures but not to adjustment for concurrent parental depressive symptoms.
Familial transmission of major depressive disorder (MDD) is a topic of long-standing interest (e.g., Rutter et al., 1990; Warner, Weissman, Mufson, & Wickramaratne, 1999). Numerous studies have documented that parental MDD confers risk of psychopathology and behavior problems in offspring (Beardslee, Versage, & Gladstone, 1998; Downey & Coyne, 1990; Goodman & Gotlib, 2002). Such research has enhanced understanding of parent–offspring patterns of depression and informed investigations of specific genetic, biological, and psychosocial mechanisms by which depression may be transmitted from one generation to the next. As longitudinal studies have progressed, there also has been an upsurge in interest in the presence of psychopathology across three successive generations (e.g., special issue of Journal of Abnormal Child Psychology, April 2003; NIMH Meeting on Intergenerational Research, October 2003). Identification of familial patterns across multiple generations represents a promising step toward understanding risk and protective factors that sustain—or disrupt—familial cycles of MDD and related problems (Bailey, Hill, Oesterle, & Hawkins, 2006).
Two recent studies addressed this issue by exploring MDD transmission across three generations (Hammen, Shih, & Brennan, 2004; Weissman et al., 2005). In a prospective study of families at high and low risk for depression, Weissman et al. (2005) reported that grandparental (Generation 1; G1) MDD predicted grandchild (Generation 3; G3) psychopathology. Children with depressed parents (Generation 2; G2) and depressed grandparents had the highest rate of anxiety disorders and general Axis I psychopathology. However, G3 children of depressed G2 parents were only at risk for psychopathology if G1 grandparents also had a history of MDD. The authors concluded that nonfamilial parental depression (i.e., G2 MDD in the absence of G1 MDD) was not a risk factor for psychopathology. However, a cross-sectional study with a community sample reported divergent findings (Hammen et al., 2004). Both grandmother (G1) MDD and maternal (G2) MDD predicted G3 MDD, and the effect of G1 MDD on G3 MDD was accounted for by G2 maternal MDD. Of note, G2 chronic interpersonal stress mediated the paths from G1 MDD-G2 MDD and from G2 MDD-G3 MDD, suggesting a possible mechanism by which MDD may be transmitted across generations.
Initial studies on the transmission of MDD across three generations are therefore consistent in suggesting that both G1 and G2 MDD influence G3 internalizing problems in late childhood and adolescence but provide different accounts of the roles of G1 and G2 MDD. In addition to these discrepant findings, limitations of prior investigations leave several unanswered questions about the transmission of MDD and internalizing problems across three generations. For example, existing studies have examined G3 in late childhood and adolescence but have not yet examined the impact of parental and grandparental MDD on internalizing problems in younger children. This is important because familial MDD negatively impacts emotional adjustment and general functioning not only in adolescence but also in early childhood (Goodman & Gotlib, 1999; Luby et al., 2002). Once present, internalizing problems are likely to interfere with young children's ability to competently resolve developmental challenges (Cicchetti & Toth, 1998), thereby increasing the risk for future depressive and other psychopathological outcomes (Birmaher et al., 2004; Kovacs et al., 1984; Weissman et al., 1999). Furthermore, to our knowledge, Weissman et al. (2005) provided the only three-generation study of MDD that obtained prospective data across generations. Advantages of a prospective design with repeated assessments is minimization of recall bias—and consequent underestimation of lifetime MDD rates (Wells & Horwood, 2004)—and potentially more accurate assessment of young children's internalizing symptoms.
To address these issues, the study presented here examined four primary areas relevant to the intergenerational transmission of internalizing problems using data collected in the Oregon Adolescent Depression Project (OADP). The OADP contains extensive lifetime diagnostic data for probands (G2) and their parents (G1), as well as Child Behavior Checklist (CBCL; Achenbach, 1991, 1992) ratings on probands' children (G3). First, based on past research and theory, we hypothesized that the presence of both G1 and G2 MDD would be associated with higher scores on CBCL Internalizing and Anxious/Depressed scales. Although we predicted main effects of G1 MDD and G2 MDD, we expected the size of these effects to be relatively small in our sample because of the young age of G3 children (M age = 4.69 years). Genetic effects, as are presumably at work in familial transmission of depression, tend to become stronger as children progress into adolescence (e.g., Scourfield et al., 2003). Likewise, depressogenic psychosocial impairments and cognitions that may be transmitted in families via social learning processes may not exert their influences until later childhood or adolescence (Kaslow, Adamson, & Collins, 2000). Nonetheless, examination of predictors of internalizing problems in young children remains important given the chronic, recurrent, and impairing course of childhood depression (Kovacs & Devlin, 1998; Luby et al., 2002) and the potential value for informing early intervention and prevention strategies (Luby, Belden, & Spitznagel, 2006).
Second, we tested several models of moderation (cf. Weissman et al., 2005) and mediation (cf. Hammen et al., 2004). Plausible theoretical arguments can be made for both models. Heritable risk and biological markers (e.g., temperamental variables, elevated Cortisol levels) of emotional disorder that are identifiable in early childhood may be passed across consecutive generations (e.g., Ashman, Dawson, Panagiotides, Yamada, & Wilkinson, 2002; Goldsmith, Buss, & Lemery, 1997). In a like manner, psychosocial characteristics that increase the risk of emotional disturbances may be passed from parent to child via processes such as modeling and direct communications. For example, parental MDD is associated with increased marital conflict and interferes with parents' responsiveness to and support for young children, which are likely to lead to insecure attachment styles that increase both proximal and distal risks of emotional distress (e.g., Besser & Priel, 2005; Cummings, Keller, & Davies, 2005). Similarly, as children develop, parents provide feedback to assist them in understanding and interpreting the meaning of life events. The provision of negative parental feedback about the causes or consequences of events in children's lives, as is likely to happen among depressed parents, is associated with more negative cognitive styles and enhanced risk of emotional distress in children (Mezulis, Hyde, & Abramson, 2006; Murray, Woolgar, Cooper, & Hipwell, 2001). To the extent that these genetic, biological, and psychosocial characteristics— and their attendant risk of MDD—are transmitted from one generation to the next, an intergenerational mediation model (i.e., G1 → G2 → G3) may best characterize the development of emotional disorders.
Alternatively, intergenerational patterns of psychopathology may operate via additive or interactive effects of risk factors. The presence of MDD in both grandparents and parents, as opposed to only one generation, may reflect higher genetic loadings for emotional disorders (cf. Weissman et al., 2005), more stressful familial contexts, and greater exposure to depressed models and depressogenic feedback from adults. If that is the case, then the sequential paths of transmission across consecutive generations (i.e., mediation) may be less relevant to early childhood adjustment than the cumulative effects of risk factors in multiple relatives (i.e., moderation).
Third, we examined the specificity of transmission across gender. The majority of intergenerational work in depression has emphasized the role of mothers (e.g., Goodman & Tully, 2006; Hammen et al., 2004), but recent work suggests that depression in fathers also enhances risk in offspring and leads to similar impairments in parent–child relationships (Kane & Garber, 2004). Therefore, we predicted that patterns of intergenerational transmission would apply to both men and women. However, prior evidence suggests that maternal MDD may be more closely related to young children's internalizing problems than paternal MDD (Connell & Goodman, 2002) and that this may be the case particularly for girls. Mothers' role as primary caretaker for young children may lead to stronger effects on children's adjustment, and social-cognitive effects such as modeling of depressogenic behaviors may be stronger among daughters, given the greater salience of the same gender parent (Goodman & Tully, 2006). Based on past research and theory, therefore, we hypothesized that (a) G2 maternal MDD would be a stronger predictor than G2 paternal MDD of G3 Internalizing scores, and (b) the impact of G2 maternal MDD on G3 Internalizing scores would be stronger for girls than boys.
Fourth, we examined whether the effects of parental and grandparental MDD on children's internalizing problems are robust to controls for potential confounds or explanatory variables. Prior research suggests that parental marital conflict and stress may mediate the link between parental MDD and offspring adjustment (Cummings et al., 2005; Hammen et al., 2004). Furthermore, parents' current mood state may bias ratings of their children's adjustment (the depression–distortion effect; Richters & Pellegrini, 1989). Given the possibility of these explanatory and confounding effects, we tested our hypotheses before and after controlling for parental stress, marital conflict, and concurrent depressive symptoms. If the predictive strength of G1 or G2 MDD weakens after controls, it would suggest that MDD in parents or grandparents impacts young children at least partially via parents' impaired psychosocial functioning.
Methods
Participants
G2 parents
A diagram of the assessment points, sample size, and attrition rates is displayed in Figure 1. Original OADP probands (G2) were randomly selected from nine high schools in western Oregon. A total of 1,709 adolescents (ages 14–18; M age = 16.6; 52.2% female; 91.1% Caucasian) completed an initial (T1) assessment between 1987 and 1989. The T1 participation rate was 61%. Approximately 1 year later, 1,507 (M age = 17.6; 53.7% female; 91.8% Caucasian) returned for a second evaluation (T2). Differences between the sample and the larger population from which it was selected, and between participants and those who declined or dropped out before T2, were small (Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993). At age 24, all probands with a history of MDD or non–mood disorders and a random sample of probands with no history of psychopathology (NMI) by T2 (n = 457) were invited to a third (T3) evaluation. The remaining 406 T2 NMI probands were deliberately excluded because of the extensive costs of reassessing all probands. Of the 1101 probands selected for a T3 interview, 941 (57.3% female; 90.4% Caucasian) completed the evaluation. T2 diagnostic groups did not differ on the rate of participation at T3. At age 30, all T3 probands were invited to a T4 evaluation. Of the 941 T3 probands, 816 (59.3% female; 89.2% Caucasian) completed the T4 diagnostic interview. Among those invited to T3 and T4 assessments, women were more likely than men to complete evaluations (χ2 > 5.99, ps < .05) participation did not differ as a function of other status variables or previous diagnoses.
Figure 1.
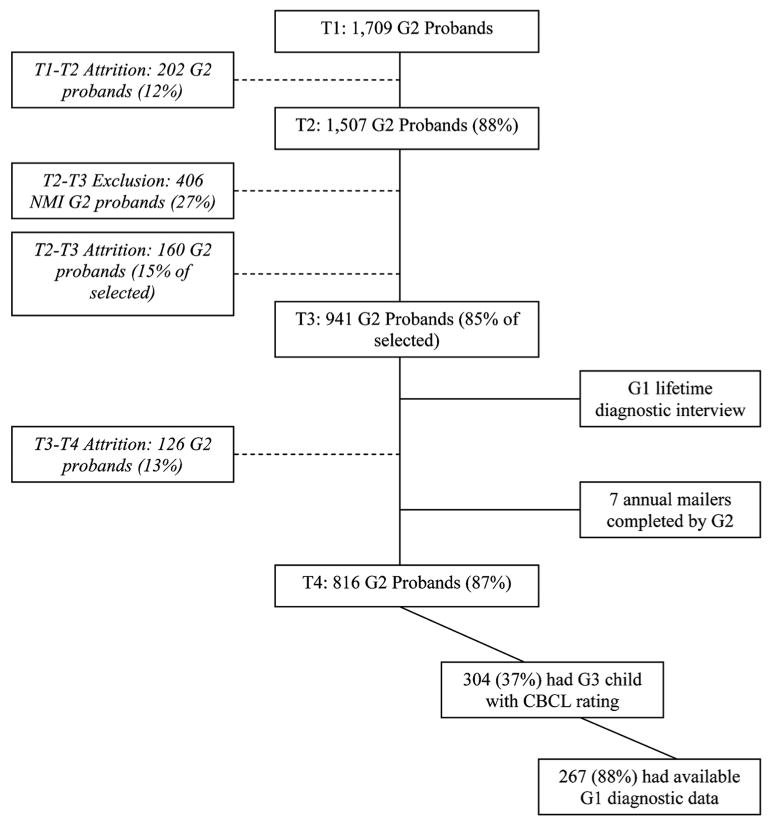
Sample selection and participation at each assessment point. Note: G1 = Generation 1; G2 = Generation 2; G3 = Generation 3; NMI = never mentally ill; CBCL = Child Behavior Checklist.
In addition to the four major assessments (T1–T4), probands were asked to complete a mailer questionnaire near the time of the T3 interview. For probands with children, the questionnaire included the CBCL. Annually for up to 7 years, and then again at T4, probands were requested to complete the mailer questionnaire. At least one CBCL rating was completed for biological children of 304 probands. No Axis I diagnostic status differed as a function of proband parental status.
G1 grandparents
We assessed lifetime psychopathology in the biological parents (G1) of probands near the time of the T3 evaluation. Of the 304 probands with available child data, 267 (87.8%) also had available data on G1 diagnostic status. Cases with missing G1 data (n = 37, 12.2%) did not significantly differ from other cases on any measured variable.
Reference sample for our investigation
These 267 G3 children (51.3% female), their 267 G2 parents (68.5% female), and 527 G1 grandparents (50.7% female) represent the reference sample for this study. At T4, the majority (76.0%) of the G2 parents were married, 10.8% had never married, and 13.1% were separated or divorced. Most (71.1%) had graduated from or completed some college, 27.0% were high school or trade school graduates, and 75.7% were employed. Annual household income was as follows: <$10,000 (5.5%); $10–19,999 (10.1%); $20–29,999 (13.6%); $30–39,999 (19.6%); $40–49,999 (11.2%); > $50,000 (34.8%); data on household income were not available for 12 (4.5%) families.
G3 children at the time of the CBCL rating ranged in age from 2 to 18 years (Mn = 4.69; SD = 2.51) with 97% under age 10. Most (68.9%) CBCL ratings were completed by mothers; 31.1% were completed by fathers. Almost all (98.9%) children lived with the parent who completed the CBCL rating. One-way analyses of variance indicated that mothers' mean CBCL scores were significantly higher than fathers' for Internalizing, F(1, 266) = 4.26, p = .04, but not Anxious/Depressed. Because of this difference in mean CBCL scores across raters, G2 rater status was controlled in multivariate analyses in which G3 CBCL scores are placed as dependent variables (DVs).
After a description of the study, written informed consent was obtained from G1 and G2. G1 and G2 participants were remunerated for their participation as follows: $50 at T1 and T2; $70 at T3; $40 for each annual mailer questionnaire; and $120 at T4. This research was approved by the Institutional Review Board at the Oregon Research Institute.
Measures
G1 grandparents
Grandparents were directly interviewed using a version of the nonpatient edition of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (3rd ed. rev. [DSM–III–R]; American Psychiatric Association, 1987) that had been modified for DSM–IV (4th ed.; American Psychiatric Association, 1994) criteria (Spitzer, Williams, Gibbon, & First, 1992). Interviewers were unaware of probands' diagnoses. Of the 267 grandmothers and 260 grandfathers included in our study, 203 (76.0%) grandmothers and 121 (46.5%) grandfathers were directly interviewed. Family history data were collected using the Family Informant Schedule and Criteria (Mannuzza & Fyer, 1990), supplemented with items to derive DSM–IV diagnoses. At least one informant interview was available for all grandfathers and for 263 (98.5%) grandmothers. Each grandmother without an informant interview completed a direct interview. (Statistical controls for direct vs. informant interview status had no meaningful impact on any analysis.) Independent review of randomly selected audiotapes revealed excellent interrater reliability for MDD diagnoses in both direct and informant interviews (κ > 0.90).
G2 parents
At T1, probands were interviewed with a version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (Orvaschel, Puig-Antich, Chambers, Tabrizi, & Johnson, 1982), which included additional items to derive DSM–III–R diagnoses. At following assessment waves, probands were interviewed using the Longitudinal Interval Follow-up Evaluation (Keller, Lavori, Friedman, & Nielsen, 1987), which elicited detailed information about the onset and course of psychiatric disorders since the previous evaluation. Independent review of randomly selected audiotapes revealed excellent interrater reliability for MDD diagnoses (κs ≥ 0.85 at each assessment wave).
Numerous G2 psychosocial measures, including the CBCL, were collected at each mailer questionnaire. We selected measures of depressive symptoms, stress, marital adjustment, and parent conflict because of their theoretical relevance or potential confounding effects. Measures completed at the same time as the highest CBCL Internalizing rating were used for analyses. Psychometric properties of some of these measures in the OADP have been reported elsewhere (Andrews, Lewinsohn, Hops, & Roberts, 1993) and are not described at length here.
The Center for Epidemiologic Studies Depression Scale (CES–D; Radloff, 1977) is a self-report measure of the frequency of 20 depressive symptoms during the past week. Symptoms are rated on a 0 to 3 scale; total scores range from 0 to 60. Its reliability and validity (i.e., correlations with the Hamilton Depression Rating Scale and Beck Depression Inventory) in the OADP sample has been supported (Andrews et al., 1993; Roberts, Lewinsohn, & Seeley, 1991; α = .89 in our sample).
Participants reported whether any of 33 major events happened to them in the past 12 months (see Andrews et al., 1993). Events were selected from the Schedule of Recent Experiences (Holmes & Rahe, 1967) and the Life Events Schedule (Sandler & Block, 1979). In addition, the Unpleasant Events Schedule (Lewinsohn, Mermelstein, Alexander, & MacPhillamy, 1985) was used to assess daily hassles that have occurred over the past 4 weeks. Our study used a 20-item version of the scale (e.g., Lewinsohn et al., 1994). The measure has demonstrated acceptable reliability (α = .88) and validity (i.e., correlations with the CES–D and the Hamilton Depression Rating Scale) in the OADP sample has been supported (Andrews et al., 1993).
Marital adjustment was assessed using the 32-item Dyadic Adjustment Scale (DAS; Spanier, 1976). It is designed for use with either married or unmarried cohabiting couples. Its psychometric properties and validity have received ample support, with internal reliability estimates consistently greater than .90 and strong correlations with other measures of marital adjustment (e.g., P. M. Cohen, 1985). Our study included total DAS scores to capture Global levels of couples' adjustment. In our sample, internal reliability was excellent (α = .93). The 10-item O'Leary-Porter Scale (OPS; Porter & O'Leary, 1980) was used to measure overt parent conflict. The OPS has been shown to discriminate distressed from nondistressed parents (Porter & O'Leary, 1980). Internal reliability was acceptable in our sample (α = .84). Of the 267 G2 probands selected for this report, complete data on the DAS and OPS were available for 218 (81.6%). Compared to those who completed these G2 parent measures, noncompleters (n = 49) were significantly less likely to be married, χ2(1, N = 267) = 78.18, p < .001; this was expected given that the DAS and OPS are not applicable to parents who are not living with a spouse or partner (n of parents living together = 223). Noncompleters also had significantly lower household incomes, F(1, 262) = 31.44, p < .001, and were significantly more likely to have a positive lifetime history of MDD, χ2(1, N = 267) = 6.83, p < .01.
G3 children
The CBCL was completed by parents at up to eight assessment points. Only G3 children born at least 2 years prior to the first mailer were eligible for all eight ratings; the majority of G3 children were born during the course of the mailer questionnaires. On average, 1.86 CBCL ratings were completed for each child. For G3 children with multiple CBCL ratings, the rating with the highest Internalizing score on the analyzed scale was selected, consistent with our lifetime diagnostic approach used with G2 and G3.1 Among families with ratings on two or more G3 children, we included ratings only for firstborn children to reduce potential biases associated with birth order and to increase the mean age of G3.
The CBCL 2–3 consists of 99 items and the CBCL 4–18 consists of 113 items. Items are rated on a 3-point scale, corresponding to whether the behavior is not true, somewhat/sometimes true, or very true/often true of the target child. The CBCL factor structure consists of eight narrow-band problem scales and two broadband scales, Internalizing Problems and Externalizing Problems. For our study, we examined dimensional T scores on the Internalizing and the Anxious/Depressed scales. We selected these scales based on evidence that they best predict the presence of internalizing disorders (Aschenbrand, Angelosante, & Kendall, 2005).
Results
Prevalence of Psychopathology
G1 grandparents
Lifetime diagnostic information on the 527 grandparents is presented in the upper half of Table 1. The majority (58.4%) met criteria for at least one Axis I disorder. G1 women displayed higher rates of MDD and anxiety disorder (ANX); G1 men displayed higher rates of substance use disorder (SUD). In a sizeable minority of cases, both grandparents met diagnostic criteria for psychopathology: any Axis I disorder (39.2%), nonaffective disorders (21.5%), SUD (15.4%), MDD (13.1%), and ANX (3.8%).
Table 1.
Prevalence of Selected Axis I Lifetime Diagnoses Among G1 and G2 Participants
| Diagnosis | Mena (%) | Womenb (%) | Totalc (%) |
|---|---|---|---|
| G1 | |||
| MDD | 61 (23.5) | 104 (39.0)* | 165 (31.3) |
| SUD | 127 (48.8) | 58 (21.7)* | 185 (35.1) |
| ANX | 25 (9.6) | 49 (18.4)* | 74 (14.0) |
| Nonaffective | 134 (51.5) | 91 (34.1)* | 225 (42.7) |
| Any Axis I | 161 (62.9) | 147 (55.1)* | 308 (58.4) |
| G2 | |||
| MDD | 32 (38.1) | 136 (74.3)* | 168 (65.4) |
| SUD | 46 (54.8) | 68 (37.2)* | 114 (42.7) |
| ANX | 10 (11.9) | 66 (36.1)* | 76 (27.5) |
| Nonaffective | 51 (60.7) | 101 (55.2) | 152 (56.9) |
| Any Axis I | 60 (71.4) | 156 (85.2)* | 216 (80.9) |
Note: G1 = generation 1; G2 = generation 2; MDD = major depressive disorder; ANX = any anxiety disorder; SUD = any substance use disorder.
G1 n = 260; G2 n = 84.
G1 n = 267; G2 n = 183.
G1 N = 527; G2 N = 267.
χ2 significant gender difference at p < .001.
G2 parents
Lifetime diagnostic information on G2 is provided in the lower half of Table 1. The high prevalence rates are because of our oversampling of probands with psychopathology at T3. Consistent with prior research, women displayed significantly higher rates of MDD, ANX, and any Axis I disorder, whereas men displayed significantly higher rates of SUD.
G3 grandchildren
Mean t scores on CBCL scales were highly similar to those of the normative sample (Achenbach, 1991, 1992). Scores on the two scales strongly intercorrelated (r = .82). Age was significantly and positively associated with scores on both scales (rs = .29, .26). Scores did not differ by sex. Relatively few children scored in the borderline or clinically elevated range: Internalizing (14.2%); Anxious/Depressed (6.4%).
Does Parental MDD Predict Offspring Internalizing Problems?
G1 MDD predicting G2 MDD
Prior findings with overlapping samples (Klein, Lewinsohn, Rohde, Seeley, & Olino, 2005; Rohde, Lewinsohn, Klein, & Seeley, 2005) document that G2 probands with at least one depressed parent are at significantly higher risk of MDD. Logistic regression procedures in our sample replicated those findings and suggested that they are robust to controls for G2 status variables. The effect held when restricting analyses to G1 fathers and dropped to a trend level for G1 mothers. G1 maternal and paternal MDD did not interact to predict G2 MDD. Likewise, G1 MDD did not interact with G2 gender to predict G2 MDD (all ps > .10).
G2 MDD predicting G3 CBCL scores
Linear regression procedures were used to examine associations between lifetime histories of G2 MDD and G3 CBCL scales (see unadjusted ts in Table 2). G2 MDD was significantly associated with higher scores on both scales. To account for potential explanatory or confounding variables, analyses were repeated controlling for three blocks of covariates (see adjusted ts and semipartial rs [sr] in Table 2). In the first block, covariates included CBCL rater status, sex, and age. In the second block, marital status, educational attainment, and household income were added. In the third block, dyadic adjustment, parent conflict, major events, and daily hassles were added. (Each covariate had significant univariate associations with both CBCL scales, with the exceptions of nonsignificant associations between G3 Anxious/Depressed and G2 sex and G2 dyadic adjustment, respectively; results available upon request to the first author.) As displayed in Table 2, the effect of G2 MDD on G3 scores was robust to statistical adjustments for Internalizing but dropped to a trend level (p = .06) for Anxious/Depressed when the third block was entered.
Table 2.
Univariate and Multivariate Associations Between G2 MDD and G3 CBCL Scales
| Unadjusted | Model 2a | Model 3b | Model 4c | |
|---|---|---|---|---|
| Internalizing | 5.27** | 4.26** | 3.14** | 1.98* |
| sr | .24 | .17 | .12 | |
| Anxious/Depressed | 4.16** | 3.46** | 2.71** | 1.89† |
| sr | .20 | .16 | .12 |
Note: N = 267. All scores are t scores. G2 = generation 2; MDD = major depressive disorder; G3 = generation 3; CBCL = Child Behavior Checklist; sr = semipartial correlation.
Adjusted for G2 CBCL rater status and G2 and G3 age and sex (n = 267, df = 261).
Adjusted for G2 Marital Status, Education, and Income (n = 254, df = 245).
Adjusted for G2 Dyadic Adjustment, O'Leary Porter, Major Life Events and Daily Hassles (n = 206, df = 193).
p = .06.
p < .05.
p < .01.
To examine the extent to which concurrent G2 parental depressive symptoms may have influenced CBCL ratings, G2 CES–D scores at the time of the CBCL rating were included in the multivariate equations with G3 Internalizing and Anxious/Depressed scores as the respective DVs. The effects of G2 MDD on G3 Internalizing and Anxious/Depressed decreased to nonsignificance when G2 CES–D scores were controlled (ps > .30). Of note, G2 CES–D scores significantly correlated with G2 lifetime MDD (ρ = .37) and G3 CBCL scores (rs = .39, .44). To determine whether the impact of G2 MDD on G3 CBCL outcomes differed as a function of G2 gender, G3 gender, or the interaction between G2 and G3 gender, regression equations were repeated with three separate predictors representing their respective interactions (G2 Sex × G2 MDD; G3 Sex × G2 MDD; G2 Sex × G3 Sex × G2 MDD). None of the interaction terms significantly predicted G3 CBCL outcomes (all ps > .10).
Does Grandparental MDD Predict Grandchild Internalizing Problems?
Linear regression procedures were used to examine associations between G1 MDD and G3 CBCL scales. G1 MDD did not predict either G3 CBCL score (ps > .10). This remained the case when separately investigating grandmothers, grandfathers, the interaction of grandmother and grandfather MDD, and when restricting analyses to maternal versus paternal grandparents. G1 MDD did not interact with G3 gender to predict either CBCL score (all ps > .10).
Do Grandparental and Parental MDD Interact to Predict Grandchild Internalizing Problems?
Regression procedures revealed that the interaction of G1 MDD × G2 MDD significantly predicted G3 Internalizing, F(3, 263) =10.59, t = 1.99, sr = .12, p = .04, and Anxious/Depressed, F(3, 263) = 7.13, t = 2.00, sr = .12, p = .04. Analyses were repeated controlling for the three blocks of covariates. The significant effect of G1 MDD × G2 MDD on G3 Internalizing was robust to adjustments of the first two blocks of covariates, F(11, 243) = 8.63, t = 1.97, sr = .12, p = .04, but dropped to nonsignificance after adjusting for the third block of covariates, F(15, 191) = 6.61, t = 1.28, sr = .08, p = .20. The significant effect of G1 MDD × G2 MDD on G3 Anxious/Depressed scores was robust to all adjustments at a marginally significant level, F(15, 191) = 4.36, t = 1.97, sr = .12, p = .05.
A graphical depiction of the G1 MDD × G2 MDD interaction effect on G3 Anxious/Depressed scores is presented in Figure 2. The figure depicts the predicted levels of G3 Anxious/Depressed scores in the presence and absence of G1 MDD and G2 MDD, respectively, at the mean level of all covariates in the regression equation (J. Cohen, Cohen, West, & Aiken, 2003). As displayed in the figure, the mean difference in G3 Anxious/Depressed scores across G2 MDD status was just over 2 points (.31 SD increase) among those with no history of G1 MDD and was just under 5 points (.72 SD increase) among those with a positive history of G1 MDD. Finally, G2 CES–D was included as an independent variable in the multivariate equation predicting G3 Anxious/Depressed. After adjusting for G2 CES-D, the effect of G1 MDD × G2 MDD on G3 Anxious/Depressed decreased to a trend level, F(16, 190) = 5.85, t = 1.73, sr = .11, p = .08. When interaction analyses were restricted by G1 gender, no significant effects emerged on any G3 outcome. The impact of G1 MDD × G2 MDD on G3 CBCL did not differ as a function of G2 or G3 gender (all ps > .10).
Figure 2.
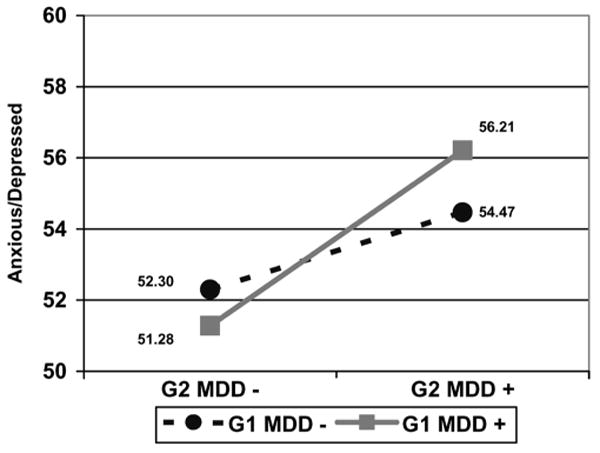
Interaction of G1 MDD and G2 MDD in predicting G3 CBCL Anxious/Depressed scores. Note: This figure presents the predicted Anxious/Depressed score in each of four conditions. G2 MDD- = no lifetime history of G2 MDD; G2 MDD + = positive lifetime history of G2 MDD; G1 MDD- = no lifetime history of G1 MDD; G1 MDD + = positive lifetime history of G1 MDD. MDD = major depressive disorder; CBCL = Child Behavior Checklist.
Discussion
Our study provides additional support for the transmission of MDD and internalizing problems across two generations. Consistent with previous research, including prior studies using data from the same OADP sample (Klein et al., 2005; Rohde et al., 2005), parental MDD predicted the presence of offspring MDD by adulthood (G1–G2). Parental MDD also predicted offspring internalizing problems in young childhood (G2–G3). When offspring MDD or CBCL Internalizing scores were the respective DVs, the effects were robust to adjustments of all potential confounders except concurrent parental depressive symptoms. In contrast, grandparental MDD exerted no main effect on grandchild behavior problems. Rather, grandparental MDD interacted with parental MDD to predict higher scores on Internalizing and Anxious/Depressed scales. The latter effect was robust to statistical adjustments, with the exception of adjustment for current parental depressive symptoms. Although the reduction in effects when controlling for parental depressive symptoms is consistent with the depression-distortion hypothesis, this also represents a highly stringent statistical test given the significant overlap between current depressive symptoms and lifetime MDD diagnostic status.
These findings are interesting in light of previous three-generation studies on the transmission of internalizing problems. Hammen et al. (2004) reported a main effect of grandparental MDD on grandchild MDD that was mediated by parental MDD and chronic interpersonal stress. Weissman et al. (2005) found that grandparental MDD moderated the association between parental MDD and grandchild anxiety disorders. Our findings suggest a relatively minimal effect of grandparental MDD on early childhood functioning. Only an interactive effect of G1 MDD on G3 outcomes was found, with G1 MDD moderating the association between G2 MDD and G3 Anxious/Depressed CBCL scores. Although this effect was relatively weak, it was robust to most statistical adjustments and accords with Weissman et al.'s findings. Together, these findings suggest that the presence of grandparental MDD in addition to parental MDD may reflect higher genetic loadings and higher rates of exposure to psychosocial risk processes such as models of depressive cognitions and familial conflict. Indeed, the decrease in the predictive effect of G1 × G2 MDD on G3 Internalizing problems when controlling for parental stress and marital adjustment is consistent with this notion.
In addition to theoretical explanations for discrepancies between three-generation studies, potential methodological explanations also deserve consideration. The extent to which between-study differences in sampling procedures (e.g., clinical vs. community) and assessment procedures (e.g., direct vs. informant interview; self-report vs. interview measure of stress) account for discrepant findings is unclear. Furthermore, the mostly null findings for G1 effects on G3 behavior problems in our study were not entirely unexpected given the young age of the sample. G3 children had not yet entered the peak onset period for most internalizing disorders, and proposed familial risk factors may not exert an effect until later developmental periods. Evidence suggests that genetic effects on internalizing psychopathology strengthen as children progress into adolescence (Rice, Harold, & Thapar, 2002; Scourfield et al., 2003; Silberg et al., 1999), although some studies report strong genetic contributions to internalizing problems even among young children (Bolton et al., 2006; Boomsa, van Beijsterveldt, & Hudziak, 2005). Likewise, cognitive and interpersonal risk factors for internalizing problems that may develop through social learning mechanisms (Cole, Jacquez, & Maschman, 2001; Mezulis et al., 2006) may become more salient in later childhood or adolescence. Developmentally speaking, our results may represent an earlier manifestation of Weissman et al.'s reported G1 × G2 interaction effect on G3 anxiety disorders. Warner et al. (1999) argued that anxiety symptoms are the earliest presentation of internalizing disorder and that early anxiety symptoms increase the risk for subsequent MDD. It is therefore possible that as children in our sample age, those with positive family histories of G1 MDD and G2 MDD will display clinically meaningful increases in anxiety and (later) depressive symptoms.2
As expected, patterns of intergenerational transmission appeared to be at work for both men and women. Findings did not suggest systematic differences in the impact of maternal versus paternal MDD, grandmother versus grandfather MDD, or when examining the interactive effects of parental and grandparental MDD. Based on prior research and theory (see Connell & Goodman's, 2002, review), we anticipated that child internalizing problems may be more strongly linked to maternal depression than paternal depression and that maternal MDD would be more strongly linked to girls' adjustment than boys'. Neither hypothesis was supported. On the surface, this appears to suggest that familial MDD negatively impacts young children regardless of gender. It may be that gender-specific effects, such as familial socialization processes or gender-specific modeling of depressive behaviors (Sheeber, Hops, & Davis, 2001), exert a stronger effect at later developmental stages. This notion is consistent with the absence in gender differences in the prevalance of internalizing disorders in young children but does not explain the absence of gender-specific effects from G1 to G2. An alternative explanation is that our relatively modest sample size, use of dichotomously coded diagnostic variables in G1 and G2, and single child outcome measure contributed to the absence of gender-specific effects.
Several limitations of this study are noted. First, the number of G3 children who displayed clinical elevations on CBCL scales was low. Second, we relied on only one report to assess G3 behavior problems (i.e., parent report). Unfortunately, we did not have clinical or observational measures of developmentally specific target behaviors. We also restricted analyses to the Internalizing and Anxious/Depressed scales. Although we selected these scales a priori because of their theoretical relevance and previously demonstrated associations with internalizing psychopathology, inclusion of the remaining CBCL scales may have revealed more detailed patterns of associations. Given the absence of a priori predictions for the additional clinical scales and our concerns about experiment-wide error, we opted not to include them in these analyses.
Limitations regarding G1 and G2 data should also be noted. First, not all G1 grandparents were directly interviewed, but rather they received diagnoses via informant reports. Second, little demographic data and no parenting or couples' adjustment measures were available for G1 (including the amount of time spent with G3), precluding investigation of mechanisms by which G1 MDD may impact G2 or G3. Third, a sizeable percentage (23.3%) of G2 did not provide data on couples' measures, and several indicators of G2 status differed among those with missing data. This introduced the possibility of biased results (although statistical controls were used) and reduced statistical power to detect effects when these variables were included in analyses. It is possible that decreases in effect sizes when the third block of covariates was entered resulted from a reduction in statistical power or the exclusion of more severely impaired families rather than the explanatory effects of the covariates. Fourth, a stratified sampling approach at T3 resulted in a high proportion of probands with MDD. Although oversampling does not distort effect sizes, it can reduce standard errors and therefore slightly bias significance tests. Caution should be used in generalizing the findings from this sample. Fifth, data were not collected from spouses/partners of G2 parents, which may have resulted in an underestimation of MDD in this generation. Sixth, we did not investigate whether features of G1 MDD and G2 MDD, such as comorbidity, severity, or chronicity, moderated effects on G3 outcomes. Future research is encouraged to examine such features, as well as to include multiple G3 assessment methods and multiple informants to develop a more complete picture of G3 outcomes. Finally, a large number of analyses were computed, which increased the potential for experiment-wide error. We did not statistically adjust for experiment-wide error, opting instead to control for several potential confounding factors. Our decision to not control for Type I error was made to balance this issue with avoiding a Type II error, given the statistical power for the analyses.
Implications for Research, Policy, and Practice
When transmission patterns from G1 to G2 and G2 to G3 are considered jointly, it appears as though parental MDD enhances the risk for internalizing problems in young children, which may develop into full syndrome MDD as children progress into adulthood. Family status variables and parental relationship variables could account for some, but not all, of the risk conferred to young children. Future research is encouraged to examine the timing (developmentally) and mechanisms by which the presence of grandparental MDD may exert risk for child internalizing problems. Hammen et al. (2004) reported promising findings that maternal MDD and chronic interpersonal stress may represent mechanisms by which grandmother MDD increases risk for adolescent MDD. Although a measure of interpersonal stress per se was not available in our study, controlling for G2 major life events and daily hassles reduced the effect of G2 MDD on G3 Anxious/Depressed to a marginally significant level but did not reduce the significant interaction effect of G1 × G2 MDD on G3 Anxious/Depressed. Theory-driven examinations of additional social-cognitive factors and genetic factors (e.g., serotonin transporter gene) in late childhood and early adolescence will lead to a more complete understanding of the intergenerational transmission of internalizing problems. In conducting such research, be it basic research or prevention trials, our findings suggest that targeting youth with both parental and grandparental histories of MDD may yield the most homogeneous, highest risk samples.
Practice implications of our findings include the need to (a) assess for psychopathology in the parents of young children with behavior problems and (b) include parents in treatment approaches for young children with behavior problems. Reductions in the predictive strength of G2 MDD when controlling for parent variables also suggest that interventions aimed at reducing parental stress and improving marital adjustment may decrease the risk of behavior problems in children (Dadds, 1992). Whereas most previous studies and intervention efforts enlisted mothers, our findings demonstrate that paternal MDD also plays an important role in the presence of childhood internalizing problems and adulthood MDD. Targeting both depressed mothers and fathers (e.g., Beardslee, Gladstone, Wright, & Cooper, 2003), therefore, likely represents a promising avenue for breaking cycles of familial transmission of psychopathology.
Acknowledgments
This research was supported by NIMH awards MH40501, MH50522, and MH52858 to Peter M. Lewinsohn and MH75744 to Jeremy W. Pettit.
Footnotes
In 13 (4.32%) cases, the selected CBCL rating predated the onset of G2 MDD. Analyses were repeated while including a variable reflecting the temporal sequence of G2 MDD onset and G3 CBCL ratings (0 = G2 MDD onset prior to G3 CBCL rating; 1 = G2 MDD onset after G3 CBCL rating). In no instance was this variable significantly associated with any G3 outcome or meaningfully alter results (available upon request to the first author).
Regression analyses were conducted to test the possibility that G3 age moderated the effects of G1 MDD and G2 MDD on G3 outcomes in this sample. No moderation effects emerged, although the young age of our sample may have contributed to the null effects.
Publisher's Disclaimer: Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article maybe used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
Contributor Information
Jeremy W. Pettit, Department of Psychology, University of Houston
Thomas M. Olino, Department of Psychology, Stony Brook University
Robert E. Roberts, School of Public Health, University of Texas Health Science Center at Houston
John R. Seeley, Oregon Research Institute
Peter M. Lewinsohn, Oregon Research Institute
References
- Achenbach TM. Child Behavior Checklist: 4-18 Years (CBCL/4-18) Burlington: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/2-3 and 1992 profile. Burlington: University of Vermont Department of Psychiatry; 1992. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. rev. Washington, DC: Author; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Andrews JA, Lewinsohn PM, Hops H, Roberts RE. Psychometric properties of scales for the measurement of psychosocial variables associated with depression in adolescence. Psychological Reports. 1993;73:1019–1046. doi: 10.2466/pr0.1993.73.3.1019. [DOI] [PubMed] [Google Scholar]
- Aschenbrand SG, Angelosante AG, Kendall PC. Discriminant validity and clinical utility of the CBCL with anxiety-disordered youth. Journal of Clinical Child and Adolescent Psychology. 2005;34:735–746. doi: 10.1207/s15374424jccp3404_15. [DOI] [PubMed] [Google Scholar]
- Ashman SB, Dawson G, Panagiotides H, Yamada E, Wilkinson CW. Stress hormone levels of children of depressed mothers. Development and Psychopathology. 2002;14:333–349. doi: 10.1017/s0954579402002080. [DOI] [PubMed] [Google Scholar]
- Bailey JA, Hill KG, Oesterle S, Hawkins DJ. Linking substance use and problem behavior across threegenerations. Journal of Abnormal Child Psychology. 2006;34:273–292. doi: 10.1007/s10802-006-9033-z. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Gladstone TRG, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: Evidence of parental and child change. Pediatrics. 2003;112:119–131. doi: 10.1542/peds.112.2.e119. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TR. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Besser A, Priel B. The apple does not fall far from the tree: Attachment styles and personality vulnerabilities to depression in three generations of women. Personality and Social Psychology Bulletin. 2005;31:1052–1073. doi: 10.1177/0146167204274082. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Williamson DE, Dahl RE, Axelson DA, Kaufman J, Dorn LD, et al. Clinical presentation and course of depression in youth: Does onset in childhood differ from onset in adolescence? Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:63–70. doi: 10.1097/00004583-200401000-00015. [DOI] [PubMed] [Google Scholar]
- Bolton D, Eley TC, O'Connor TG, Perrin S, Rabe-Hesketh S, Rijsdijk F, et al. Prevalence and genetic and environmental influences on anxiety disorders in 6-year-old twins. Psychological Medicine. 2006;36:335–344. doi: 10.1017/S0033291705006537. [DOI] [PubMed] [Google Scholar]
- Boomsa DI, van Beijsterveldt CEM, Hudziak JJ. Genetic and environmental influences on anxious/depression during childhood: A study from the Netherlands twin register. Genes, Brain, & Behavior. 2005;4:466–481. doi: 10.1111/j.1601-183X.2005.00141.x. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. The development of depression in children and adolescents. American Psychologist. 1998;53:221–241. doi: 10.1037//0003-066x.53.2.221. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Cohen PM. Locke Marital Adjustment Scale and the Dyadi-cAdjustment Scale. American Journal of Family Therapy. 1985;13:66–71. [Google Scholar]
- Cole DA, Jacquez FM, Maschman TL. Social origins of depressive cognitions: A longitudinal study of self-perceived competence in children. Cognitive Therapy and Research. 2001;25:377–395. [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children's internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Dadds MR. Concurrent treatment of marital and child behaviour problems in behavioural family therapy. Behaviour Change. 1992;9:139–148. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH, Buss KA, Lemery KS. Toddler and childhood temperament: Expanded content, stronger genetic evidence, new evidence for the importance of environment. Developmental Psychology. 1997;33:891–905. doi: 10.1037//0012-1649.33.6.891. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Goodman SH, Tully E. Depression in women who are mothers: An integrative model of risk for the development of psychopathology in their sons and daughters. In: Keyes CLM, Goodman SH, editors. Women and depression: A handbook for the social, behavioral, and biomedical sciences. New York: Cambridge University Press; 2006. pp. 241–280. [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Holmes TH, Rahe RH. Schedule of Recent Experiences. Seattle: University of Washington, School of Medicine; 1967. [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children's psychopathology, and father–child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Adamson LB, Collins MH. A developmental psychopathology perspective on the cognitive components of child and adolescent depression. In: Sameroff J, Lewis M, Miller S, editors. Handbook of developmental psychopathology. New York: Kluwer; 2000. pp. 491–510. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Neilsen E. The Longitudinal Interval Follow-up Examination: A comprehensive method for assessing outcome in retrospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Olino TM. Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine. 2005;35:353–365. doi: 10.1017/s0033291704003587. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Devlin B. Internalizing disorders in childhood. Journal of Child Psychology and Psychiatry. 1998;39:47–63. [PubMed] [Google Scholar]
- Kovacs M, Feinberg T, Crouse-Novak M, Paulauskas SL, Pollock M, Finkelstein R. Depressive disorders in childhood: II. A longitudinal study of the risk for a subsequent major depression. Archives of General Psychiatry. 1984;41:643–649. doi: 10.1001/archpsyc.1984.01790180013001. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Mermelstein RM, Alexander C, MacPhillamy D. The Unpleasant Events Schedule: A scale for the measurement of aversive events. Journal of Clinical Psychology. 1985;41:483–498. doi: 10.1002/1097-4679(198507)41:4<483::aid-jclp2270410407>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- Luby JL, Belden AC, Spitznagel E. Risk factors for preschool depression: The mediating role of early stressful life events. Journal of Child Psychology and Psychiatry. 2006;47:1292–1298. doi: 10.1111/j.1469-7610.2006.01672.x. [DOI] [PubMed] [Google Scholar]
- Luby J, Heffelfinger A, Mrakotsky C, Hessler M, Brown K, Hildebrand T. Preschool major depressive disorder: Preliminary validation for developmentally modified DSM-IV criteria. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:928–937. doi: 10.1097/00004583-200208000-00011. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Fyer AJ. Family Informant Schedule and Criteria. New York: New York State Psychiatric Institute, Anxiety Disorders Clinic; 1990. July 1990 rev. [Google Scholar]
- Mezulis A, Hyde JS, Abramson LY. The developmental origins of cognitive vulnerability to depression: Temperament, parenting, and negative life events in childhood as contributors to negative cognitive style. Developmental Psychology. 2006;42:1012–1025. doi: 10.1037/0012-1649.42.6.1012. [DOI] [PubMed] [Google Scholar]
- Murray L, Woolgar M, Cooper P, Hipwell A. Cognitive vulnerability to depression in 5-year-old children of depressed mothers. Journal of Child Psychology and Psychiatry. 2001;42:891–899. doi: 10.1111/1469-7610.00785. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MR, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. Journal of the American Academy of Child and Adolescent Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Porter B, O'Leary KD. Marital discord and childhood behavior problems. Journal of Abnormal Child Psychology. 1980;8:287–295. doi: 10.1007/BF00916376. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rice F, Harold GT, Thapar A. Assessing the effects of age, sex and shared environment on the genetic aetiology of depression in childhood and adolescence. Journal of Child Psychology and Psychiatry. 2002;43:1039–1051. doi: 10.1111/1469-7610.00231. [DOI] [PubMed] [Google Scholar]
- Richters J, Pellegrini DS. Depressed mothers' judgments about their children: An examination of the depression-distortion hypothesis. Child Development. 1989;60:1068–1075. doi: 10.1111/j.1467-8624.1989.tb03537.x. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: A comparison of depression scales. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR. Association of parental depression with psychiatric course from adolescence to young adulthood among formerly depressed individuals. Journal of Abnormal Psychology. 2005;114:409–420. doi: 10.1037/0021-843X.114.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Macdonald H, Le Couteur A, Harrington R, Bolton P, Bailey A. Genetic factors in child psychiatric disorders: II. Empirical findings. Journal of Child Psychology and Psychiatry. 1990;31:39–83. doi: 10.1111/j.1469-7610.1990.tb02273.x. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Block M. Life stress and maladaption of children. American Journal of Community Psychology. 1979;7:425–439. doi: 10.1007/BF00894384. [DOI] [PubMed] [Google Scholar]
- Scourfield J, Rice F, Thapar A, Harold GT, Martin N, McGuffin P. Depressive symptoms in children and adolescents: Changing aetiological influences with development. Journal of Child Psychology & Psychiatry. 2003;44:968–976. doi: 10.1111/1469-7610.00181. [DOI] [PubMed] [Google Scholar]
- Sheeber LB, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Silberg J, Pickles A, Rutter M, Hewitt J, Simonoff E, Maes H, et al. The influence of genetic factors and life stress on depression among adolescent girls. Archives of General Psychiatry. 1999;56:225–232. doi: 10.1001/archpsyc.56.3.225. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID): I. History, rationale, and description. Archives of General Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Warner V, Weissman MM, Mufson L, Wickramaratne PJ. Grandparents, parents, and grandchildren at high risk for depression: A three-generational study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:289–296. doi: 10.1097/00004583-199903000-00016. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner D, Verdeli H, Pilowsky DJ, et al. Families at high and low risk for depression: A three generation study. Archives of General Psychiatry. 2005;62:29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wolk S, Wickramaratne P, Goldstein RB, Adams P, Greenwald S, et al. Children with prepubertal-onset major depressive disorder and anxiety grown up. Archives of General Psychiatry. 1999;56:794–801. doi: 10.1001/archpsyc.56.9.794. [DOI] [PubMed] [Google Scholar]
- Wells JE, Horwood LJ. How accurate is recall of key symptoms of depression? A comparison of recall and longitudinal reports. Psychological Medicine. 2004;34:1001–1011. doi: 10.1017/s0033291703001843. [DOI] [PubMed] [Google Scholar]


