Abstract
Hypoxia inducible factor 1 (HIF-1) represses the transcription of pro-apoptotic bid in colorectal cancer cells in vitro. To assess the clinical relevance of this observation, HIF-1α and Bid were assessed in serial sections of 39 human colorectal adenocarcinomas by immunohistochemistry. In high HIF-1α nuclear-positive cell subpopulations, there was a significant reduction in Bid expression (ANOVA, P=0.04). Given the role of Bid in drug-induced apoptosis, these data add impetus to strategies targeting HIF-1 for therapeutic gain.
Keywords: colorectal cancer, tumour hypoxia, Bid, HIF-1α
Approximately 30–50% of patients diagnosed with colorectal cancer (CRC) (35 000 new cases per year in the United Kingdom) will either present with or develop distant metastases. For these patients, management with combination chemotherapy offers survival prolongation (Saunders and Iveson, 2006), but the disease course is frequently characterised by acquired drug resistance manifesting as tumour progression and the need to alter treatment.
Tumour hypoxia and suppression of apoptosis are important drivers of drug (Makin and Dive, 2003; Shannon et al, 2003) and radiotherapy (Saunders et al, 2002) resistance in solid tumours. The transcription factor, hypoxia inducible factor-1 (HIF-1), consists of α and β subunits: the former is ubiquitinated and degraded in normoxia but stabilised in hypoxia; the latter is constitutively expressed independent of oxygen (Semenza, 2003). Under hypoxic conditions, HIF-1α is translocated to the cell nucleus where it dimerises with HIF-1β to bind hypoxia-responsive elements (HRE) in target gene promoters. Hypoxia inducible factor-1 targets encode multiple components of adaptive pathways, including increased glucose uptake, pH stabilisation (via carbonic anhydrase (CA-IX) (Wykoff et al, 2000), and regulation of apoptosis (Greijer and van der Wall, 2004).
Of the Bcl-2 family of apoptosis regulatory proteins, pro-apoptotic Bid is of particular interest as it links the mitochondrial (intrinsic)- and death receptor (extrinsic)-driven apoptotic pathways (Andersen et al, 2005; Letai, 2008). In exploring links between tumour hypoxia and apoptosis, we previously demonstrated that HIF-1 repressed transcription of bid in CRC cell lines in vitro (Erler et al, 2004). Moreover, a reciprocal relationship was demonstrated between hypoxic regions and Bid expression in CRC xenografted tumours (Erler et al, 2004). This study sought to determine the clinical significance of these observations and examined the relationship between the number of cells with stabilised nuclear HIF-1α and Bid expression in ex vivo CRC tissue. To assess HIF-1 functionality, nuclear HIF-1α expression was examined in parallel with CA-IX.
Materials and methods
Patients
Tissues from 39 patients with colorectal adenocarcinoma were used from the joint Christie Hospital and Hope Hospital CRC tissue banks (Manchester, UK) under ethical approvals (LREC-02/051; 03/SM/449). Clinical details have been published previously (Renehan et al, 2000; Bibi et al, 2006). All samples were from luminal tumour edges and processed, formalin-fixed, and paraffin-embedded using standard operational procedures.
Immunohistochemical staining and analysis
Antibodies used were mouse monoclonal anti-human HIF-1α (610958, diluted 1 : 100, BD Biosciences, Oxford, UK); goat polyclonal anti-human Bid (1 : 50, Santa Cruz Biotechnology, CA, USA); and mouse anti-human CA-IX (anti-MN 75, 1 : 20, kindly provided by Bayer Diagnostics). Sections of 4 μm were stained as previously described (Wilson et al, 2000). Before HIF-1α, and Bid immunostaining, antigen retrieval was by microwaving in 10 mM citrate buffer (pH 6: 2 × 10 min), and the Tyramide Signal Amplication System (NEN Life Sciences, Boston, MA, USA) was used to optimise HIF-1α staining. All staining was completed using diaminobenzidene (EnVision HRP kit, Dako, Cambridge, USA) for 2–3 min before counterstaining with haematoxylin. A variety of approaches were used to control the experiment (see legend, Figure 1). Batch-to-batch variation was assessed using two regions with clear high or low nuclear HIF-1α expression, comparing sections from these with each batch.
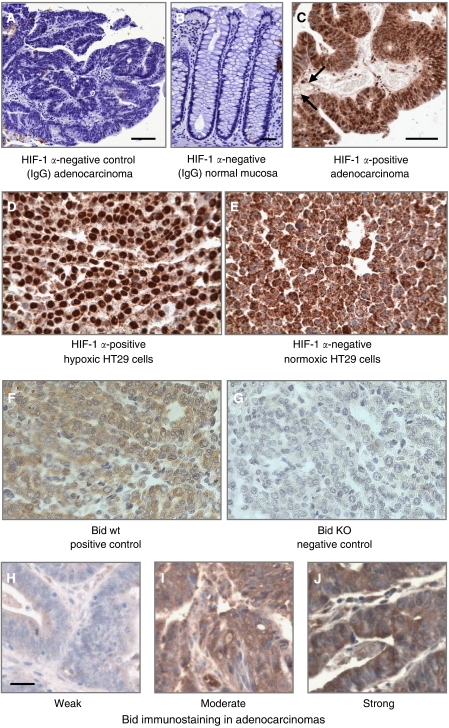
Figure 1.
Experimental controls for immunohistochemistry. (A) Substitution of the primary antibody with mouse IgG1 at the same dilution was used as a negative control in all experiments. (B) Normal large bowel mucosa was an additional IgG1-negative control. (C) Representative immunostaining for HIF-1α demonstrating immunopositivity in close proximity to blood vessels (arrows). Both nuclear and cytoplasmic staining is seen. (D and E) Formalin-fixed and paraffin-embedded pellets of HT-29 human colorectal cancer cells previously cultured for 16 h in normoxic or hypoxic conditions (1% O2) and stained for HIF-1α. Only nuclear staining, as seen in hypoxic cells, was considered positive; we considered the diffuse cytoplasmic staining in normoxic cells as nonspecific, reasoning that HIF-1 is not transcriptionally active in cytosol. (F and G) Formalin-fixed and paraffin-embedded pellets of Bid knockout and wild-type mouse embryonic fibroblasts (kindly provided by SJ Korsmeyer, Harvard Medical School, Boston, MA, USA) were used as positive and negative controls for Bid. Pellets were processed identical to that for human tumour specimens. (H–J) Bid immunostaining in human adenocarcinomas with representative sections of weak (score 1), moderate (score 2), and strong (score 3) staining. The magnification bar for all sections is 50 μm.
Hypoxia inducible factor-1α expression was heterogeneous both within and between tumours. To quantify this, a scoring system was developed with nuclear HIF-1α expression as a continuous variable, and the number of immunopositive cells expressed per area (see below). Immunopositivity was defined by strong nuclear staining; cytoplasmic staining alone was considered negative. The mean HIF-1α score was based on the average of three counts. A pilot study identified that all tumours were HIF-1α immunopositive, but that high- and low-positive subpopulations existed using a cutoff of 20 positive cells per 40 000 μm2 (200 × 200).
Expression scores for Bid and CAIX were semiquantitative based on stain intensity (Rhodes et al, 2000). Bid was assigned as weak, moderate, or strong (scored as 1, 2, or 3, respectively). For CA-IX, some tumours exhibited no staining and, therefore, the scores included zero. From these scores, a consensus of three observers was taken.
To quantify specifically the relationship between nuclear HIF-1α and Bid expression, a technique of paired same area serial analysis was developed. Each specimen was sectioned to produce serial slides 4 μm apart. Slides were viewed and imaged using a Nikon E600 microscope (× 100 magnification). A 200 × 200 μm2 boxed area of high HIF-1α staining was selected and an identical box placed on the corresponding area on the Bid slide. This procedure was repeated for low HIF-1α areas resulting in 78 paired analyses. A series of experiments were repeated for paired HIF-1α and CA-IX.
Assessment of internal validity
Interobserver variations were assessed to confirm the validity of our analytic approaches. The number of nuclear HIF-1α-immunopositive cells within each boxed area was counted independently by three observers (MMS, MPS, and CD). For Bid and CA-IX, tumour images were randomised before the same observer assessed staining within the assigned boxes.
Statistical analysis
Distributions of mean nuclear HIF-1α were skewed, and were therefore log-transformed. Comparisons of means used univariate and multivariate analysis of variance (ANOVA). Other immunostaining scores were treated as ordinal. Interobserver variation of continuous data (mean nuclear HIF-1α) was assessed using intraclass correlations: for ordinal data (Bid and CA-IX), κ-correlations were performed. All analyses were performed using STATA (version 9.0, College Station, TX, USA).
Results
Immunopositivity for nuclear HIF-1α was present in all adenocarcinomas but was heterogeneous within tumours. Hypoxia inducible factor-1α staining was noted adjacent to areas of necrosis but also adjacent to blood vessels (Figure 1C). Bid immunostaining was diffuse non-nuclear and positive in all sections but its intensity varied between tumours (Figure 1E).
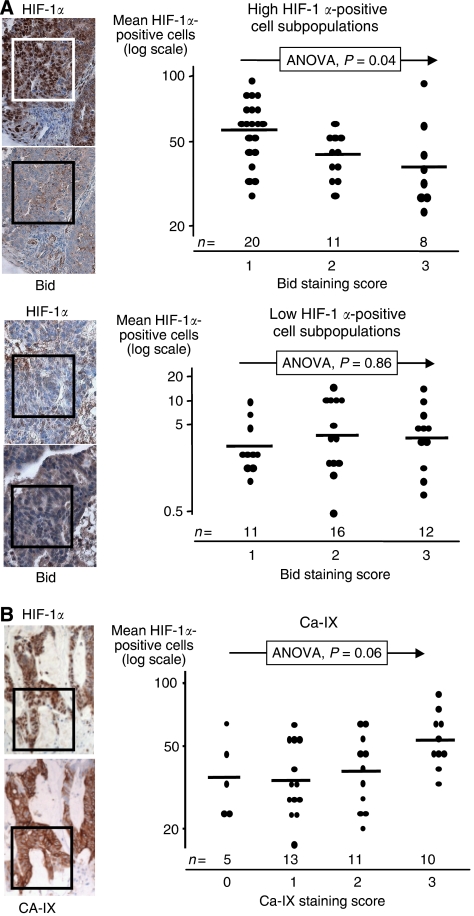
Areas of high HIF-1α immunopositivity were often associated with low Bid expression, whereas areas of low HIF-1α immunopositivity were associated with variable Bid expression. This was quantified as follows: for high-HIF-1α areas, there was a stepwise reduction in Bid expression with increasing mean HIF-1α positivity (ANOVA, P=0.04) (Figure 2A). This relationship was absent for low HIF-1α areas.
Figure 2.
(A) Hypoxia inducible factor-1α-positive nuclei scores vs Bid category scores in the paired same area serial analysis. Upper panel represents high mean HIF-1α scores (greater than 20 positive nuclei per area). Lower panel represents low mean HIF-1α scores. Boxes represent 200 × 200 μm2. Geometric means (horizontal lines) are compared across the categories using an ANOVA model. Y axis is log-transformed. n indicates number of tumours per Bid category score. (B) Similar graphic representation of HIF-1α-positive nuclei scores vs CA-IX expression.
Mean HIF-1α immunopositivity correlated with the total number of epithelial cells per square (r=0.86, P<0.001), that is, cell density. To assess this further, a multivariate ANOVA model was generated, and demonstrated the attenuation of the extent of inverse association between mean HIF-1α and Bid expression in the high HIF-1α subpopulations (P=0.07).
In the assessment of HIF-1 functionality, there was coincident staining of mean HIF-1α immunopositivity with CA-IX immunopositivity (ANOVA, P=0.06) (Figure 2B).
Internal validity
The intraclass correlation for HIF-1α immunopositivity counts (among high HIF-1α areas) was 0.77 (95 confidence interval: 0.67–0.88), with an estimated reliability of 91%. The κ-correlations for observer 1 vs 2, 1 vs 3, and 2 vs 3 were as follows: Bid: 0.72, 0.72, and 0.83; CA-IX: 0.55, 0.75, and 0.56; respectively.
Discussion
We purposefully limited our clinical study design to test a single hypothesis that HIF-1 represses bid transcription leading to reduced Bid expression in ex vivo CRC having shown that hypoxia-driven downregulation of Bid occurred via a HIF-1-dependent pathway in CRC cell lines in vitro. We had demonstrated in vitro that this mechanism was operational during hypoxic resistance to etoposide and oxaliplatin, which was overcome to a degree by forced maintained expression of Bid. When CRC lines were xenografted into CD1 nude mice, a striking reciprocal relationship was observed between the hypoxia marker pimonidazole, which formed a penumbra adjacent to necrotic regions in tumours (a location typically associated with chronic hypoxia), and Bid expression, which stained more positively away from the necrotic regions (Erler et al, 2004). However, although the tumour–xenograft model is widely used for preclinical testing of anticancer agents, it has two key limitations – first, the degree of genetic heterogeneity observed in most human tumours does not exist in xenografts; and second, the native stromal microenvironment is lacking. Thus, it was necessary to test the HIF-1α and Bid relationship in human tissues.
The human data that emerged were consistent with HIF-1α-mediated repression of Bid occurring in human CRC. However, this relationship was modest, and attenuated after the adjustment for cell density. It is not surprising that HIF-1α expression varied after this adjustment, as its induction may be influenced by hypoxic and non-hypoxic mechanisms (Semenza, 2003). Hence, for example, in the human specimens, HIF-1α immunostaining was observed adjacent to oxygen-rich intratumoral blood vessels. One may expect the relationship between transcriptionally active HIF-1 and Bid to be independent of these mechanisms, but other regulators of Bid expression (e.g., p53 loss) (Sax et al, 2002) may also be operational in CRC tissue. We speculate that the absence of a relationship in low-score HIF-1α may indicate a threshold level for bid transcriptional repression to predominate.
As an additional dimension of complexity, it is increasingly clear that modulation of tumour apoptosis may occur through HIF-1-independent pathways, for example, Bad activation and cell survival through an adenosine–Akt pathway in glioblastoma cells (Merighi et al, 2007).
Strengths of our study were as follows: first, we used robust staining controls; second, we determined HIF-1α immunopositivity as a continuous variable allowing analyses that included adjustments for cell density; third, we developed and validated the use of the paired same area serial analysis; and fourth, we assessed HIF-1α functionality in the CRC tissues by demonstrating coincident expression with CA-IX, an established HIF-1 transcriptional target.
Tumour hypoxia offers a selective approach to the treatment of cancer, as, with only few exceptions, normal tissues do not usually experience low oxygen tension. Accordingly, HIF-1 is considered an attractive anticancer drug target (Semenza, 2003; Welsh and Powis, 2003; Melillo, 2007). Hypoxia inducible factor-1 inhibition could potentially ablate several adaptive responses that allow tumour cell survival under conditions of compromised oxidative phosphorylation. Negating HIF-1 functions improves response to therapy (Hussein et al, 2006) and small-molecule HIF-1 inhibitors are currently in early clinical trial (Semenza, 2003; Melillo, 2007). The data presented here give additional impetus to targeting HIF-1 for therapeutic gain, as it is predicted to increase Bid levels and, in turn, reduce the threshold for apoptosis.
Acknowledgments
We acknowledge the following funding: MMS was funded by Christie Hospital NHS Foundation Trust, Manchester; CC and the running costs for this project were supported by Cancer Research UK (C147 held by CD). DR was funded by a CR-UK project grant (C84/A43394) held by IJS, who is supported by an MRC programme grant (G6500366). AGR is an HEFCE-funded senior lecturer.
Footnotes
Conflict of interest
The authors state no conflict of interest.
References
- Andersen MH, Becker JC, Straten P (2005) Regulators of apoptosis: suitable targets for immune therapy of cancer. Nat Rev Drug Discov 4: 399–409 [DOI] [PubMed] [Google Scholar]
- Bibi R, Pranesh N, Saunders MP, Wilson MS, O'Dwyer ST, Stern PL, Renehan AG (2006) A specific cadherin phenotype may characterise the disseminating yet non-metastatic behaviour of pseudomyxoma peritonei. Br J Cancer 10: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erler JT, Cawthorne CJ, Williams KJ, Koritzinsky M, Wouters BG, Wilson C, Miller C, Demonacos C, Stratford IJ, Dive C (2004) Hypoxia-mediated down-regulation of Bid and Bax in tumors occurs via hypoxia-inducible factor 1-dependent and -independent mechanisms and contributes to drug resistance. Mol Cell Biol 24: 2875–2889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greijer AE, van der Wall E (2004) The role of hypoxia inducible factor 1 (HIF-1) in hypoxia induced apoptosis. J Clin Pathol 57: 1009–1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussein D, Estlin EJ, Dive C, Makin GW (2006) Chronic hypoxia promotes hypoxia-inducible factor-1alpha-dependent resistance to etoposide and vincristine in neuroblastoma cells. Mol Cancer Ther 5: 2241–2250 [DOI] [PubMed] [Google Scholar]
- Letai AG (2008) Diagnosing and exploiting cancer's addiction to blocks in apoptosis. Nat Rev Cancer 8: 121–132 [DOI] [PubMed] [Google Scholar]
- Makin G, Dive C (2003) Recent advances in understanding apoptosis: new therapeutic opportunities in cancer chemotherapy. Trends Mol Med 9: 251–255 [DOI] [PubMed] [Google Scholar]
- Melillo G (2007) Targeting hypoxia cell signaling for cancer therapy. Cancer Metastasis Rev 26: 341–352 [DOI] [PubMed] [Google Scholar]
- Merighi S, Benini A, Mirandola P, Gessi S, Varani K, Leung E, Maclennan S, Baraldi PG, Borea PA (2007) Hypoxia inhibits paclitaxel-induced apoptosis through adenosine-mediated phosphorylation of bad in glioblastoma cells. Mol Pharmacol 72: 162–172 [DOI] [PubMed] [Google Scholar]
- Renehan AG, Jones J, Potten CS, Shalet SM, O'Dwyer ST (2000) Elevated serum insulin-like growth factor (IGF)-II and IGF binding protein-2 in patients with colorectal cancer. Br J Cancer 83: 1344–1350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes A, Jasani B, Balaton AJ, Miller KD (2000) Immunohistochemical demonstration of oestrogen and progesterone receptors: correlation of standards achieved on in house tumours with that achieved on external quality assessment material in over 150 laboratories from 26 countries. J Clin Pathol 53: 292–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders M, Iveson T (2006) Management of advanced colorectal cancer: state of the art. Br J Cancer 95: 131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders MP, Patterson AV, Stratford IJ (2002) Programming of radiotherapy and sensitization. In Oxford Textbook of Oncology, Souhami RL, Tannock I, Hohenberger P, Horiot J-C (eds) 2nd edn, Vol. 1, pp 459–474. Oxford: Oxford University Press [Google Scholar]
- Sax JK, Fei P, Murphy ME, Bernhard E, Korsmeyer SJ, El-Deiry WS (2002) BID regulation by p53 contributes to chemosensitivity. Nat Cell Biol 4: 842–849 [DOI] [PubMed] [Google Scholar]
- Semenza GL (2003) Targeting HIF-1 for cancer therapy. Nat Rev Cancer 3: 721–732 [DOI] [PubMed] [Google Scholar]
- Shannon AM, Bouchier-Hayes DJ, Condron CM, Toomey D (2003) Tumour hypoxia, chemotherapeutic resistance and hypoxia-related therapies. Cancer Treat Rev 29: 297–307 [DOI] [PubMed] [Google Scholar]
- Welsh SJ, Powis G (2003) Hypoxia inducible factor as a cancer drug target. Curr Cancer Drug Targets 3: 391–405 [DOI] [PubMed] [Google Scholar]
- Wilson JW, Nostro MC, Balzi M, Faraoni P, Cianchi F, Becciolini A, Potten CS (2000) Bcl-w expression in colorectal adenocarcinoma. Br J Cancer 82: 178–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykoff CC, Beasley NJ, Watson PH, Turner KJ, Pastorek J, Sibtain A, Wilson GD, Turley H, Talks KL, Maxwell PH, Pugh CW, Ratcliffe PJ, Harris AL (2000) Hypoxia-inducible expression of tumor-associated carbonic anhydrases. Cancer Res 60: 7075–7083 [PubMed] [Google Scholar]