Abstract
Fas ligand (FasL/CD95L) is a member of the tumour necrosis factor superfamily that triggers apoptosis following crosslinking of the Fas receptor. Despite studies strongly implicating tumour-expressed FasL as a major inhibitor of the anti-tumour immune response, little is known about the mechanisms that regulate FasL expression in tumours. In this study, we show that the cyclooxygenase (COX) signalling pathway, and in particular prostaglandin E2 (PGE2), plays a role in the upregulation of FasL expression in colon cancer. Suppression of either COX-2 or COX-1 by RNA interference in HCA-7 and HT29 colon tumour cells reduced FasL expression at both the mRNA and protein level. Conversely, stimulation with PGE2 increased FasL expression and these cells showed increased cytotoxicity against Fas-sensitive Jurkat T cells. Prostaglandin E2-induced FasL expression was mediated by signalling via the EP1 receptor. Moreover, immunohistochemical analysis using serial sections of human colon adenocarcinomas revealed a strong positive correlation between COX-2 and FasL (r=0.722; P<0.0001) expression, and between EP1 receptor and FasL (r=0.740; P<0.0001) expression, in the tumour cells. Thus, these findings indicate that PGE2 positively regulates FasL expression in colon tumour cells, adding another pro-neoplastic activity to PGE2.
Keywords: Fas ligand, prostaglandin E2, regulation, tumour immune evasion
Colorectal cancer is a formidable health-care problem, being one of the leading causes of cancer death worldwide. Despite evidence that the host immune system can initiate an immune response against colon tumours, a large number of tumours continue to grow and evade immune-mediated elimination owing to the development of multiple immune escape mechanisms (Waldner et al, 2006). Upregulation of Fas ligand (FasL/CD95L) expression by tumour cells may represent one such mechanism (O’Connell et al, 1996). FasL is a member of the tumour necrosis factor (TNF) superfamily that can trigger apoptotic cell death following ligation to its receptor Fas (CD95/APO-1) on sensitive cells (Nagata and Golstein, 1995). Many human cancers, including colon cancer, express FasL, with growing evidence supporting a role for FasL in colon carcinogenesis (Houston and O’Connell, 2004; Whiteside, 2007). Upregulation of FasL expression is an early event in colon carcinogenesis (Bennett et al, 2001; Belluco et al, 2002), with tumour-expressed FasL being associated with apoptosis and loss of tumour-infiltrating lymphocytes (TIL) in vivo, and triggering the death of Fas-bearing sensitive cells in vitro (O’Connell et al, 1996; Okada et al, 2000). Engagement of Fas by FasL can also trigger proliferation of tumour cells (Lambert et al, 2003; Li et al, 2008) and increase tumour cell motility and invasiveness (Barnhart et al, 2004). Moreover, downregulation of FasL expression in colon tumour cells was recently shown to result in reduced tumour development and growth in immune-competent mice in vivo (Ryan et al, 2005). However, despite this, little is known about the molecular mechanisms underlying FasL expression in tumours.
Numerous studies have shown that cyclooxygenase-2 (COX-2) plays an important role in colon carcinogenesis (Cao and Prescott, 2002). Cyclooxygenase is a rate-limiting enzyme in the conversion of arachidonic acid to prostaglandins. Two isoforms of COX have been characterised, COX-1 and COX-2 (Williams and DuBois, 1996). Cyclooxygenase-1 is constitutively expressed, generating prostaglandins for normal physiological processes. In contrast, COX-2 is usually undetectable in most normal tissues, but can be induced rapidly by a variety of agents, including LPS, cytokines, growth factors and tumour promoters. Overproduction of COX-2 and its major metabolite prostaglandin E2 (PGE2) has been found in many human cancers, including colorectal tumours (Rigas et al, 1993; Eberhart et al, 1994; Sano et al, 1995), with COX-2 levels increased in about 90% of colon cancers and ∼50% of pre-malignant colorectal adenomas (Eberhart et al, 1994).
As increased expression of COX-2 and FasL in colon tumours has been widely observed, we tested the hypothesis that the COX signalling pathway may play a role in FasL expression in colon tumours. Here we provide evidence that the COX signalling pathway, and in particular PGE2, increases FasL expression in colon tumour cells. We also show that PGE2-induced FasL expression is mediated by the EP1 receptor. Consistent with these findings, we observed a strong positive correlation between COX-2 expression and FasL, and between EP1 receptor expression and FasL in human colon tumour cells in vivo. Collectively, these results support a role for PGE2 as a critical mediator of FasL expression in colon tumours.
Materials and Methods
Reagents
Prostaglandin E2, SC19220 and arachidonic acid were obtained from Cayman Chemical Company (Ann Arbor, MI, USA). SC-560 and SC-791 were purchased from Calbiochem (San Diego, CA, USA). rhFas:Fc was obtained from Alexis Corp. (Lausen, Switzerland).
Cell lines and culture conditions
HT29 human colon adenocarcinoma cells and Jurkat T cells were obtained from the ATCC (Rockville, MD, USA). HCA-7 cells were a generous gift from Susan Kirkland (University of London). WIDR, SW480 and Caco-2 cells were obtained from Ken Nally (University College Cork). HT29, WIDR, SW480, Caco-2 and HCA-7 cells were maintained in DMEM containing 10% fetal calf serum (FCS) and penicillin–streptomycin, whereas Jurkat T cells were cultured in RPMI-1640 supplemented with 10% FCS and penicillin–streptomycin.
RNA interference
The targeted sequences that effectively mediate the silencing of COX-1 (siGENOME SMARTpool, M-004556-00), COX-2 (siGENOME SMARTpool, M-004557-01), EP1 (ON-TARGETplus SMARTpool, L-005711-00), EP2 (ON-TARGETplus SMARTpool, L-005712-00) and EP4 (ON-TARGETplus SMARTpool, L-005714-00) expression were obtained from Dharmacon Research (Lafayette, CO, USA). HCA-7 and HT29 cells were seeded 24 h before transfection at a concentration achieving 70% confluence at the time of transfection. The transfection was carried out in serum-free medium using Dharmafect 4 transfection reagent (Dharmacon Research). Cells were transfected with 100 nM of COX-1 small interfering RNA (siRNA), COX-2 siRNA, EP1 siRNA, EP2 siRNA, EP4 siRNA or irrelevant control siRNA according to the manufacturer's protocol. At 48 h after transfection, cells were treated with PGE2 for 24 h. Depletion of protein was confirmed by real-time RT-PCR and immunoblotting. Culture medium was collected and stored at −20°C for subsequent measurement of PGE2 levels by ELISA. Levels of FasL in cell lysates were determined by real-time RT-PCR and immunoblotting.
Western blot analysis
Cells were seeded at 5 × 105 cells per well in six-well plates and serum-deprived for 48 h before treatment for 24 h with either serum-free medium containing vehicle or PGE2, unless otherwise stated. For inhibitor studies, cells were pretreated for 1 h with the inhibitor, before the addition of PGE2. Cells were washed in PBS and lysed on ice in 50 mM Tris-HCl, pH 8, containing 150 mM NaCl and 1% Triton X-100, supplemented with the complete-TM mixture of protease inhibitors (Roche Molecular Biochemicals, Indianapolis, IN, USA). Protein concentrations were measured using the BCA Protein assay (Pierce, Rockford, IL, USA). Proteins (40 μg protein per lane) were separated on a 10% SDS–polyacrylamide gel, transferred to a nitrocellulose membrane and then probed with one of the following primary antibodies: anti-FasL (N-20/1 : 200 dilution), anti-Fas (C-20/1 : 1000), anti-COX-1 (C-20/1 : 250) (Santa Cruz Biotechnology, Santa Cruz, CA, USA), anti-FasL (Ab-1/1 : 100 dilution) (Calbiochem), anti-TNF-related apoptosis-inducing ligand (anti-TRAIL; 1 : 500 dilution), anti-COX-2 (1 : 1000), anti-EP1 (1 : 300), anti-EP2 (1 : 500), anti-EP4 (1 : 500) (Cayman Chemical Company). As an internal control, all membranes were subsequently stripped of the first antibody and reprobed with anti-β-actin-specific antibody (AC-74; 1 : 10 000 dilution; Sigma, St Louis, MO, USA). The antigen–antibody complex was detected by incubating the membranes for 1 h at room temperature with the appropriate horseradish peroxidase (HRP)-conjugated secondary antibody (Dako Corp., Carpinteria, CA, USA). Peroxidase activity was detected with the enhanced chemiluminescence system (Pierce) and analysed using Scion Image analysis software (Scion Inc., Frederick, MD, USA). Changes in protein expression were determined after normalising the band intensity of each lane to that of β-actin.
Quantification of mRNA
Total RNA was isolated from cultured cells using the Agilent Total RNA isolation kit (Agilent Technologies, Santa Clara, CA, USA) according to the manufacturer's instructions and cDNA synthesised using AMV reverse transcriptase, random hexanucleotide primers, RNasin (40 U) and dNTPs (500 μM) (Promega, Madison, WI, USA). Quantitative PCR was then performed in triplicate using an ABI PRISM 7500 Sequence Detection System and commercially available TaqMan probes (Applied Biosystems, Foster City, CA, USA). Briefly, cDNA in 22.5 μl of water was mixed with 2.5 μl of 20 × TaqMan Gene Expression assay primer and probe mix (FasL=Hs00181225, TRAIL=Hs00366272, EP1=Hs00168752, EP2=Hs00168754, EP3=Hs00168755, EP4=Hs00168761, glyceraldehyde-3-phosphate dehydrogenase (GAPDH)=4326317E) and 25 μl of 2 × TaqMan Gene Expression master mix in a 96-well optical reaction plate. The following PCR conditions were used: 50°C for 2 min, then 95°C for 10 min, followed by 50 cycles at 95°C for 15 s and 60°C for 1 min. The expression level of the target genes was normalised to internal GAPDH. Data were analysed using Microsoft Excel and calculated using the relative standard curve method (ABI, User Bulletin 2).
Prostaglandin E2 assay
Prostaglandin E2 production was measured by ELISA, according to the manufacturer's instructions (R&D Systems, Minneapolis, MN, USA).
Co-culture experiment
HCA-7 and HT29 cells were plated in triplicate in 96-well plates and allowed to reach ∼70% confluency. Cells were serum-starved for 48 h, followed by treatment with serum-free medium containing vehicle (0.1% DMSO), 0.5 or 1.0 μM PGE2 for 24 h. Cells were then fixed with 1.5% paraformaldehyde and washed with PBS. Jurkat cells were added at a concentration of 5 × 104 cells per well. To block FasL-mediated cytotoxicity, Jurkat cells were co-cultured with paraformaldehyde-fixed 1.0 μM PGE2-treated cells in the presence of recombinant Fas:Fc (10 μg ml−1). After 24 h, Jurkat cell viability was assessed by measuring the increase in fluorescence intensity associated with the cellular reduction of resazurin to resorufin, according to the manufacturer's instructions (R&D Systems). Briefly, the cells were pulsed with 44 μM resazurin solution and 1 h later fluorescence was measured at 535/590 nm using a standard spectrophotometer in bottom reading mode. This fluorescence was expressed as a percentage of that shown by control Jurkat T cells in RPMI-1640 only, after subtraction of background fluorescence.
Immunofluorescent detection of FasL
Cells were seeded at 2 × 105 cells per well in six-well plates containing sterile coverslips. After serum-starving for 48 h, cells were treated with serum-free medium containing 0.5, 1.0 or 2 μM PGE2 for 24 h. Cells were fixed with 1.5% paraformaldehyde, permeabilised with 0.2% Triton X-100 in PBS and nonspecific binding of antibody was blocked with 10% normal goat serum for 30 min at room temperature. Cells were incubated overnight at 4°C with anti-FasL-specific antibody (G247-4; Pharmingen, San Diego, CA, USA) diluted 1 : 50. Antibody binding was localised using an FITC-labelled secondary antibody (Dako Corp.). Coverslips were mounted on slides with anti-fading mounting media (Dako Corp.) and visualised using a fluorescent microscope when dry.
Human colon adenocarcinoma tissues and immunohistochemistry
Formalin-fixed, paraffin-embedded human colonic adenocarcinomas (n=27) were obtained from the archives of the Mercy Hospital, Cork, following a protocol approved by the Cork Teaching Hospitals Clinical Research Ethics Committee. None of the cases used in this study had patient identifiers and strict confidentiality was maintained. None of the patients had received chemotherapy, radiotherapy or immunotherapy before tissue collection.
Tissue sections were de-paraffinised in xylene and rehydrated before analysis. Antigen retrieval was performed by microwave irradiation in 0.01 M citrate buffer, pH 6.0. Slides were washed and endogenous peroxidase was quenched with 3.0% hydrogen peroxide in methanol for 5 min. Nonspecific binding was blocked with 5% normal serum in wash buffer for 1 h. Serial sections were incubated overnight at 4°C with monoclonal FasL (G247-4) antibody (Pharmingen) at 5 μg ml−1, rabbit polyclonal COX-2 antibody (Santa Cruz Biotechnology) at 0.5 μg ml−1, rabbit polyclonal EP1 antibody (Cayman Chemical Company) at 0.27 μg ml−1 or goat polyclonal COX-1 antibody (Santa Cruz Biotechnology) at 0.133 μg ml−1. Antibody binding was localised using a biotinylated secondary antibody, avidin-conjugated HRP and DAB substrate, contained within the Vectastain ABC detection kit (Vector Laboratories, Burlingame, CA, USA). Slides were counterstained with haematoxylin and mounted. Parallel negative controls were performed for each antibody, using rabbit (COX-2, EP1) IgG, mouse (FasL) IgG or normal goat serum (COX-1) instead of primary antibody.
Neoplasms displaying immunoreactivity in more than 5% of the tumour cells were regarded as positive. Semiquantitative analysis of the immunohistochemical score for COX-2, COX-1, EP1 and FasL staining was performed by light microscopy for each tumour using a scoring system that included the extent (0=negative; 0.25=1–25% of cells stained; 0.5=26–50% of cells stained; 0.75=51–75%; 1=>75% of cells stained) and intensity (0, negative; 1, weak; 2, moderate; 3, strong; 4, intense) of staining. The scores from the two scales were multiplied by each other to give a single immunohistochemical score. For each tumour, 10 random high-power fields were scored.
Statistics
All experiments were performed in triplicate unless otherwise indicated, and mean values were presented as mean±s.e.m. Paired Student's t-test was performed to compare the data between indicated groups. Spearman's rank correlation test was used for correlation between the expression of FasL and COX-1, COX-2 and EP1 in colon tumour tissue. A value of P<0.05 was considered statistically significant.
Results
Prostaglandin E2 induces FasL mRNA and protein expression in colon cancer cells
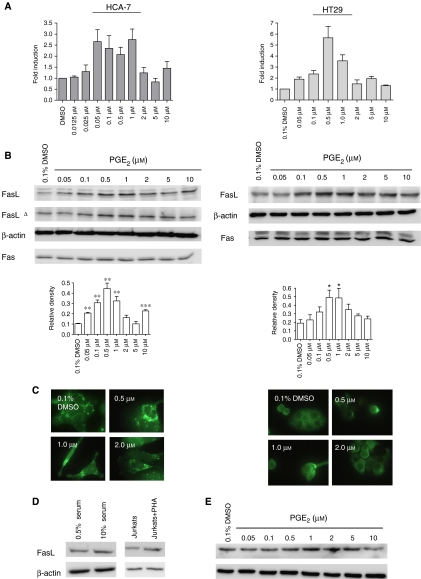
Numerous studies have shown that PGE2 produced via the COX-2 signalling pathway plays a crucial role in the development of colon cancer (Kamei et al, 2003). To determine if PGE2 induces FasL expression in colon cancer cells, we analysed the effect of PGE2 on FasL expression in HCA-7 human colon cancer cells. HCA-7 cells have high endogenous levels of COX-2, PGE2 and FasL. As COX-2 is an inducible gene that is regulated by, among other factors, serum (Dubois et al, 1998), HCA-7 cells were serum-starved before treatment with increasing concentrations of PGE2, ranging from low (0.025 μM) to high (10 μM), and FasL expression was analysed by real-time RT-PCR, Western blotting and immunofluorescence. As shown in Figure 1, PGE2 increased FasL expression at both the mRNA and protein level, with maximum induction of FasL mRNA occurring at 1.0 μM PGE2 (>2.7-fold induction) (Figure 1A). Analysis of protein production by Western blotting and immunofluorescence showed that FasL protein also peaked at relatively low levels of PGE2 (0.5–1.0 μM) (Figure 1B and C), whereas the levels of the Fas receptor were unaffected. This increase in FasL protein was confirmed using two different anti-FasL-specific antibodies. Prostaglandin E2 engagement also increased FasL expression in HT29 colon cancer cells. Relative to HCA-7 cells, HT29 cells have low levels of COX-2 and PGE2. However, there was an ∼5.7- and 3.6-fold induction in FasL mRNA following incubation with 0.5 and 1.0 μM PGE2, respectively (Figure 1A), with FasL protein also peaking at 0.5–1.0 μM PGE2 (Figure 1B and C). Based on these findings, a concentration of 1.0 μM PGE2 was used in all subsequent experiments.
Figure 1.
Prostaglandin E2 induces FasL expression in colon cancer cells. (A) HCA-7 cells and HT29 cells were cultured in serum-free medium for 48 h before treatment with PGE2. After 24 h, total RNA was extracted and was reverse transcribed to cDNA. FasL mRNA levels were measured by quantitative real-time RT-PCR. Columns indicate fold induction relative to control (DMSO). Mean±s.e.m. values are plotted. (B) Following the isolation of total cellular protein from cells treated as in (A), equal amounts of protein were separated by SDS–PAGE and visualised with anti-FasL (N-20), anti-FasLΔ (Ab-1), anti-Fas or anti-β-actin. Semiquantitative analysis of FasL expression was determined by calculating the ratio between FasL protein and β-actin protein from three independent experiments. Mean±s.e.m. values are plotted (*P<0.05, **P<0.01; compared with DMSO control; Student's t-test). (C) Cells were treated as in (A) and FasL protein was detected by immunofluorescence. (D) HCA-7 cells were serum-starved for 48 h and thereafter the medium was replaced with complete medium (10% serum) for 24 h. As a control for FasL detection, Jurkat T cells were treated with 2.5 μg ml−1 PHA for 24 h, which has been shown to increase FasL expression in these cells. Cellular lysates were analysed by Western blotting using antibodies against FasL and β-actin. (E) HCA-7 cells were cultured in complete medium followed by treatment with PGE2 for 24 h. Cellular isolates were treated as in (D).
Since serum deprivation induces cell cycle arrest, and FasL expression in T cells has been reported to be cell cycle sensitive, we also determined if PGE2 induced FasL expression in cells grown in complete medium (10% serum). The addition of serum to serum-starved cells increased FasL expression in these cells by ∼40% as assessed by Western blotting (Figure 1D). However, the addition of serum also induced an increase in PGE2 secretion by these cells (data not shown). Thus, we investigated if PGE2 induces FasL expression in cells grown in complete medium. The addition of PGE2 increased FasL expression in HCA-7 cells and this increase was ∼2.5 times (1 μM PGE2) greater than that induced by serum alone (Figure 1E), suggesting that PGE2 induces FasL expression independently of entry into the cell cycle. Interestingly, this induction of FasL by PGE2 also exhibited a ‘bell-shaped’ dose–response relationship, similar to that obtained following PGE2 treatment of serum-starved cells. This ‘bell-shaped’ dose–response relationship has been previously demonstrated in SW1116 cells on measuring proliferation in response to PGE2 and was suggested to be due to differential activation of the EP receptors at different concentrations of PGE2 (Qiao et al, 1995). Prostaglandin E2 binds to and activates four different receptor subtypes, EP1, EP2, EP3 and EP4 (Bos et al, 2004), suggesting that one (or more) EP receptor is involved in inducing FasL expression in colon cancer cells.
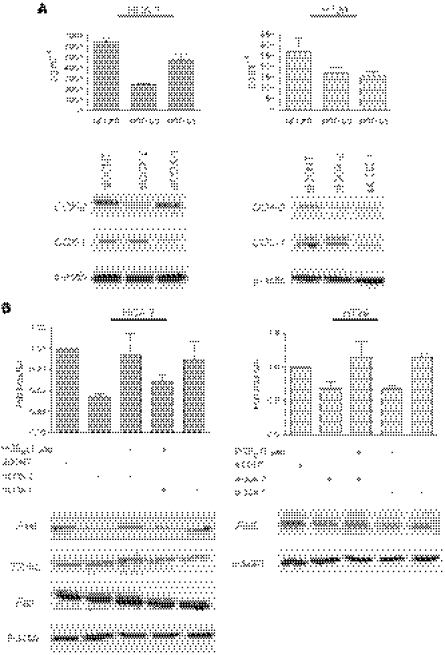
Furthermore, depletion of COX-1 and COX-2 by RNA interference (RNAi) reduced FasL expression in both HCA-7 and HT29 cells. Although COX-2 is the isoform that is overexpressed in colon cancer, evidence from mouse experiments has also implicated COX-1 as a causal agent in COX-induced colorectal carcinogenesis (Chulada et al, 2000), with production of PGE2 being the common denominator. Thus, the expression of both COX-1 and COX-2 was reduced by RNAi, and the efficiency of depletion was verified by PGE2 ELISA and Western blotting (Figure 2A). Suppression of COX-2 and COX-1 by RNAi reduced FasL expression in both HCA-7 and HT29 cells, as evidenced by a reduction in FasL mRNA and protein production (Figure 2B). Cyclooxygenase-2 depletion resulted in a >55% reduction in FasL mRNA in HCA-7 cells and a >30% reduction in FasL mRNA in HT29 cells, as assessed by real-time RT-PCR, whereas FasL mRNA was reduced by >38 and >32% in HCA-7 and HT29 cells, respectively, by COX-1 RNAi. Western blot analysis confirmed these findings at the protein level, with siCOX-2 and siCOX-1 significantly reducing FasL protein in HCA-7 (P<0.01 and P<0.01, respectively) and HT29 (P<0.01 and P<0.05, respectively) cells, as assessed by semiquantitative densitometric analysis. This effect was specific for FasL and did not affect TRAIL, another death-inducing member of the TNF superfamily, or Fas receptor, as assessed by real-time RT-PCR (data not shown) and Western blotting (Figure 2B). Importantly, PGE2 restored FasL production in both cell lines in the presence of COX-2 and COX-1 RNAi, demonstrating that COX-derived PGE2 is an important mediator of FasL expression in colon cancer cells. These findings were also confirmed using COX-1- and COX-2-specific inhibitors. As shown in Figure 3, treatment with SC-560 (COX-1-specific inhibitor) or SC-791 (COX-2-specific inhibitor) reduced PGE2 secretion into the culture medium in both systems, with a concomitant reduction in FasL protein. Interestingly, inhibition of both COX-1 and COX-2 did not completely abrogate FasL expression (Figure 3C), suggesting that in colon tumour cells PGE2 is only one of the factors responsible for regulating FasL expression.
Figure 2.
Suppression of either COX-1 or COX-2 by RNAi reduces FasL expression in HT29 and HCA-7 colon cancer cells. (A) HCA-7 and HT29 cells were transfected with control nonspecific RNAi (siCONT), COX-2-specific RNAi (siCOX-2) or COX-1-specific RNAi (siCOX-1). After 48 h, cell culture medium and cellular lysates were collected. Levels of PGE2 in the cell culture medium were determined by ELISA. Mean±s.e.m. values are plotted. Changes in COX-1 and COX-2 protein levels were detected by Western blotting. (B) RNA was extracted from cells treated as in (A) and reverse transcribed to cDNA. FasL mRNA levels were measured by quantitative real-time RT-PCR. Columns indicate fold induction relative to siCONT-treated cells. Mean±s.e.m. values are plotted. Cellular lysates were analysed by Western blotting using antibodies raised against FasL, TRAIL, Fas or β-actin.
Figure 3.
Inhibition of COX-1 using SC-560 or that of COX-2 using SC-791 reduces FasL expression in colon cancer cells. (A) HCA-7 and HT29 cells were serum-deprived for 48 h before treatment with SC-560 or SC-791. After 1 h, cell culture medium was collected and the levels of PGE2 were determined by ELISA. Mean±s.e.m. values are plotted. (B) HCA-7 and HT29 cells were serum-deprived for 48 h, treated with SC-560 or SC-791 and 24 h later cell lysates were collected. Lysates were analysed by Western blotting using antibodies raised against FasL and β-actin. Data shown are representative of three independent experiments. (C) HCA-7 cells were serum-deprived for 48 h, treated with 10 μM SC-560 and/or 10 μM SC-791 and 24 h later cell lysates were collected and treated as in (B).
To corroborate the role of PGE2 in inducing FasL expression at a functional level, HCA-7 and HT29 cells were treated with PGE2 for 24 h, washed with PBS, fixed and then co-cultured with Jurkat T cells. The Jurkat T-cell line is a Fas-sensitive cell line of T-cell origin that is widely used experimentally as a model for activated T cells. There was a 14.5 and 29.1% reduction in Jurkat T-cell viability following co-culture with control HT29 and HCA-7 cells, respectively. However, upregulation of FasL expression by PGE2 on HCA-7 and HT29 cells substantially increased their effector function against the Jurkat T cells (Figure 4). Following co-culture with 1.0 μM PGE2-treated HT29 and HCA-7 colon cancer cells, Jurkat T-cell viability decreased by 55.9 and 54.8%, respectively, relative to cells cultured in medium only. This reduction in cell viability following co-culture with 1.0 μM PGE2-treated cells was confirmed to be Fas-mediated, as it could be blocked by the addition of neutralising anti-FasL antibody.
Figure 4.
Reduction in Jurkat T-cell viability following co-culture with colon cancer cells treated with PGE2. HT29 and HCA-7 cells were serum-deprived for 48 h, followed by treatment for 24 h with 0.1% DMSO, 0.5 or 1.0 μM PGE2. Cells were fixed and then co-cultured with Jurkat T cells for 24 h. Jurkat T-cell viability was determined by resazurin reduction. To block FasL-mediated apoptosis, Jurkat T cells were also co-cultured with 1.0 μM PGE2-treated colon cancer cells in the presence of 10 μg ml−1 recombinant Fas:Fc blocking protein. Data denote mean±s.e.m. and are representative of two independent experiments. Viability is expressed as an index (% of control Jurkat T cells maintained in medium only).
Prostaglandin E2-induced FasL expression is EP1 receptor-dependent
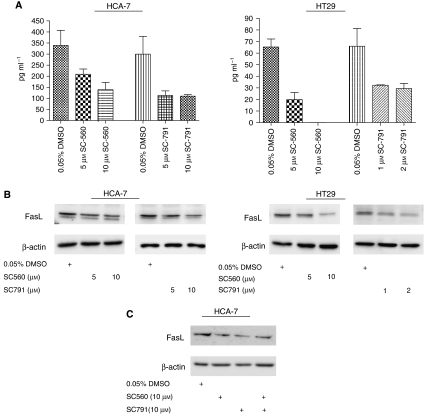
Prostaglandin E2 exerts its biological activity through four different receptor subtypes, EP1, EP2, EP3 and EP4 (Bos et al, 2004), with HCA-7 cells expressing all four receptors, as determined by real-time RT–PCR. In contrast, HT29 cells expressed only EP1 and EP4. As EP1, EP2 and EP4 have previously been reported to play a role in colon carcinogenesis, we investigated whether these receptors are involved in PGE2-induced FasL expression. In the first experiment, we utilised siRNA to downregulate EP1, EP2 and EP4 in HCA-7 cells. Transfection with EP1-, EP2- and EP4-specific siRNA resulted in efficient impairment of EP1, EP2 and EP4 transcription (64, 84 and 59% reduction in mRNA, respectively) and protein translation (Figure 5A). Cells were then treated with PGE2 and FasL production was analysed by real-time RT-PCR and immunoblotting. As shown in Figure 5B and C, suppression of EP1 prevented PGE2-induced FasL expression in HCA-7 cells at both the mRNA and protein levels. In contrast, EP2- and EP4-specific siRNA had little or no effect. Similar results were obtained with HT29 cells, where transfection with EP1-specific siRNA resulted in a decreased induction of FasL following treatment with PGE2 (Figure 5B and C).
Figure 5.
Suppression of EP1 blocks PGE2-induced FasL upregulation in HCA-7 and HT29 cells. (A) HCA-7 cells were transfected with control nonspecific RNAi (siCONT), EP1-specific RNAi (siEP1), EP2-specific RNAi (siEP2) or EP4-specific RNAi (siEP4). After 48 h, cells were lysed and successful depletion of EP1, EP2 and EP4 receptors in cells transfected with the corresponding siRNA was confirmed by Western blotting. (B) At 48 h after transfection with siCONT, siEP1, siEP2 or siEP4, HCA-7 and HT29 cells were treated with 1.0 μM PGE2 for 24 h and RNA was extracted and reverse transcribed to cDNA. FasL mRNA levels were measured by quantitative real-time RT-PCR. Columns denote fold induction relative to siCONT-treated cells. Mean±s.e.m. values are plotted. (C) Total protein was isolated from cells treated as in (B) and lysates were analysed by Western blotting using antibodies raised against FasL and β-actin. (D) Cells were serum-starved for 48 h, pretreated with SC19220 for 1 h, followed by treatment with 1.0 μM PGE2 for 24 h. Cells were lysed and analysed by Western blotting using antibodies raised against FasL and β-actin.
As an alternative approach to inhibiting EP1 receptor activity, in a second experiment cells were pretreated for 1 h with SC19220 (25–100 μM), which is an EP1 receptor antagonist, before the addition of PGE2 and FasL expression was analysed by immunoblotting. As shown in Figure 5D, SC19220 prevented the PGE2-induced increase in FasL expression in a dose-dependent manner, consistent with a role for EP1 receptor in mediating this effect.
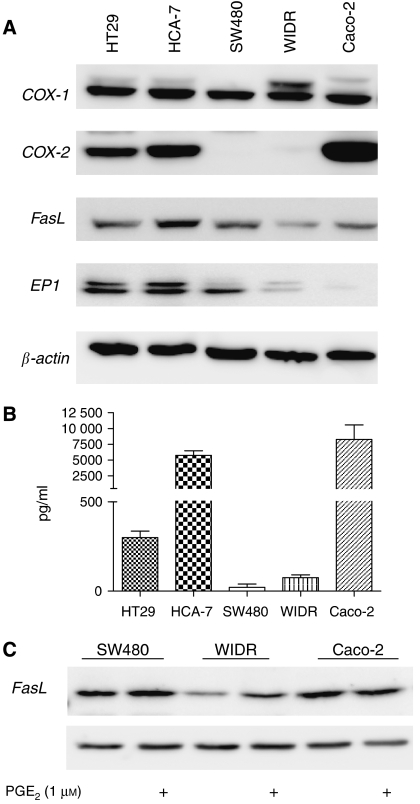
To determine if there was any correlation between the basal expression level of FasL and the EP1 receptor, five different colon cancer cell lines were grown in complete media and the expression of COX-1, COX-2, FasL and EP1 was assessed by Western blotting (Figure 6A), whereas PGE2 secretion was determined by ELISA (Figure 6B). Four of the cell lines (HT29, HCA-7, WIDR and Caco-2) expressed all five proteins, although at very different levels. (COX-2 was detectable in WIDR cells on increased exposure). In contrast, SW480 cells were negative for COX-2, whereas Caco-2 cells expressed very low levels of EP1 receptor. Interestingly, although both HCA-7 and Caco-2 cells strongly expressed COX-2 and PGE2, HCA-7 cells exhibited much stronger expression of FasL than Caco-2 cells, which is likely due to the much higher expression level of EP1 receptor found in these cells. HT29 cells also strongly expressed FasL, despite producing much lower levels of PGE2. However, HT29 cells also strongly expressed the EP1 receptor. SW480 and WIDR in turn secreted very low amounts of PGE2. However, SW480 cells expressed more EP1 receptor than WIDR cells, together with stronger basal production of FasL. Finally, 1.0 μM PGE2 induced FasL expression in both SW480 and WIDR cells, but not in Caco-2 cells, which is likely due to the very low/negligible levels of EP1 receptor expressed by Caco-2 cells.
Figure 6.
FasL expression is correlated with EP1 receptor expression in colon cancer cells in vitro. (A) Cells were seeded at 1 × 105 cells per ml and after 24 h the medium was replaced with fresh growth medium. After 24 h, cell culture medium and cellular lysates were collected. Cellular lysates were analysed by Western blotting using antibodies raised against COX-1, COX-2, FasL, EP1 receptor or β-actin. (B) Levels of PGE2 in the cell culture medium were determined by ELISA. Mean±s.e.m. values are plotted. (C) SW480, WIDR and Caco-2 cells were serum-starved for 48 h before treatment with 1.0 μM PGE2 for 24 h. Cellular isolates were separated by SDS–PAGE and visualised with anti-FasL or anti-β-actin.
Correlation between COX-1, COX-2, EP1 receptor and FasL expression in human colon cancer cells
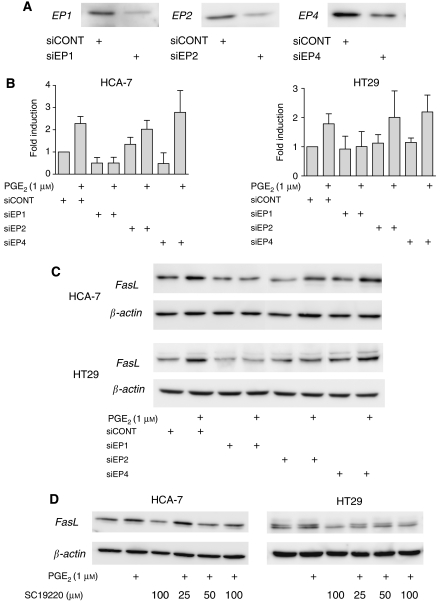
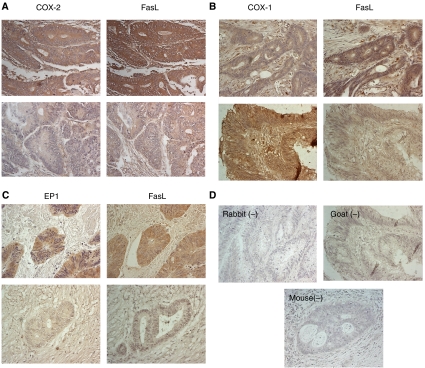
To determine if our in vitro data had in vivo relevance, COX-1, COX-2, EP1 receptor and FasL expression was analysed by immunohistochemistry on sequential sections from 27 human colon cancer tissues. Examination of stained tumour specimens revealed that 81% (22 out of 27) of the tumours expressed FasL and 96% (26 out of 27) expressed EP1, whereas COX-1 protein was detected in the neoplastic cells of 88% (22 out of 25) of tumours and COX-2 in 85% (23 out of 27) of tumours. Staining for all four proteins varied in intensity and extent both within individual tumours and between tumours, with some cells in the stromal compartments also exhibiting positive immunoreactivity. However, strong immunostaining for FasL was seen more frequently in cancer cells with strong immunostaining for COX-2 (Figure 7A) and EP1 receptor (Figure 7C). In contrast, strong immunostaining for COX-1 did not frequently coincide with strong FasL immunostaining (Figure 7B). No staining was seen when the primary antibody was substituted with isotype-matched controls (rabbit and mouse) or non-immune serum goat (Figure 7D).
Figure 7.
Immunohistochemical visualisation of COX-1, COX-2, EP1 receptor and FasL in human colon cancer. (A) Cyclooxygenase-2 and FasL, (B) COX-1 and FasL and (C) EP1 receptor and FasL immunostaining in cancer cells, with the upper and lower panels representing different colon cancer specimens. Specific protein stained brown. (D) Rabbit, goat and mouse controls demonstrated no staining. Representative micrographs are shown. Original magnification: × 300.
To determine if expression of the proteins correlated in vivo, consecutive sections were scored in a blinded fashion for both the number of COX-1-, COX-2-, EP1- and FasL-positive tumour cells and the intensity of staining, and the final scores were multiplied to give a total immunohistochemical score. There was no correlation between the immunostaining scores of COX-1 and FasL. However, a strong positive correlation was observed between COX-2 and FasL (r=0.722; P<0.0001), and between EP1 and FasL (r=0.740; P<0.0001) immunostaining, indicating a possible interrelationship in the expression of these proteins.
Discussion
Although there are conflicting reports on the role of FasL in tumorigenesis (Restifo, 2000;, O’Connell et al, 2001), considerable evidence now exists indicating that FasL expression by tumour cells may aid in tumour development. Studies performed in vitro, as well as evidence from numerous in situ examinations, indicate that tumour-expressed FasL is associated with apoptosis of TIL and may thus protect tumour cells from destruction by the immune system (O’Connell et al, 2001; Whiteside, 2007). Tumour-expressed FasL has also been shown to be associated with metastasis of tumour cells to the lymph nodes and liver (Mann et al, 1999; Younes et al, 2000), whereas ligation of Fas by FasL can stimulate cell proliferation (Lambert et al, 2003; Li et al, 2008), and increase tumour cell motility and invasiveness (Barnhart et al, 2004; Peter et al, 2007). Furthermore, recent studies suggest that tumour-expressed FasL may contribute to tumour growth in cancers associated with inflammation, in part through the induction of chemotactic factors (Matsumoto et al, 2007). Together, these findings suggest that the FasL signalling pathway plays a critical role in tumour development and immune evasion, and that suppression of FasL expression may aid in the treatment of certain cancers. In support of this, we have recently shown that specific inhibition of FasL expression in colon cancer cells significantly retards tumour formation in immune-competent syngeneic mice (Ryan et al, 2005). However, despite the role of FasL in tumorigenesis, little is known about the regulation of this molecule in tumour cells.
Increased PGE2 production has been shown to be strongly associated with colorectal neoplasia, increasing critical pro-survival and anti-apoptotic factors that favour cell growth (Wang and Dubois, 2006). However, the effector genes downstream of PGE2 have not been well characterised. In this study, we show using a variety of methods that PGE2 regulates FasL expression in colon cancer cells, suggesting that PGE2 may also play a role in FasL-mediated tumour immune evasion. Induction of FasL in vitro occurred at relatively low concentrations of PGE2 (∼0.5–1.0 μM), with both COX-2 and COX-1 appearing to play a role in this process. However, in human colon cancer cells in vivo, COX-2 appears to play a more important role in the induction of FasL than COX-1, with expression of COX-2 and not COX-1 correlating with FasL expression. One potential explanation may be that although both isoforms may play a role in the induction of FasL expression through production of PGE2, in vivo COX-2 is the isoform that is increased in colon cancer, with a concomitant increase in PGE2 (Rigas et al, 1993; Eberhart et al, 1994). In contrast, COX-1 expression has been reported to remain constant under most physiological and pathological conditions (Eberhart et al, 1994; Sano et al, 1995). Although recent studies have shown that COX-1 may also play a role in carcinogenesis in some cancers, such as ovarian (Gupta et al, 2003), head and neck (Erovic et al, 2008) and colon cancer (Chulada et al, 2000), the common denominator in all these studies is an increase in the overall level of PGE2. Following upregulation during colon carcinogenesis, COX-2 may be the primary source of PGE2 in the tumour microenvironment, and thus may play a more important role in inducing FasL expression in human colon tumour cells in vivo.
Prostaglandin E2 mediates its effects by binding to and activating four different G-protein-coupled receptors, EP1, EP2, EP3 and EP4, with genetic deletion and pharmacologic manipulation of the EP receptors identifying different roles for EP1, EP2 and EP4 in intestinal tumorigenesis (Wang and Dubois, 2006). In the current study, we show that the EP1 signalling pathway is the predominant pathway that mediates PGE2-induced FasL expression. Prostaglandin E2-induced FasL was blocked by both EP1-specific RNAi and pharmacologic inhibition of EP1, but not by EP2- or EP4-specific RNAi. Moreover, a strong correlation was observed between EP1 and FasL expression in colon cancer cells in vitro and in vivo, indicating a possible interrelationship in the expression of these two proteins and together suggesting that these findings may have physiological relevance. The EP1 receptor has previously been shown to play an important role in colon carcinogenesis. The development of both aberrant crypt foci and colon tumours was significantly reduced in EP1-knockout mice following treatment with the colon carcinogen azoxymethane (Watanabe et al, 1999; Kawamori et al, 2005). Also recent studies characterising EP receptor expression in a variety of tumour types showed that expression of EP1 is increased in tumour cells relative to normal tissue (Shoji et al, 2004; Miyata et al, 2006; Rask et al, 2006) and is associated with tumour progression and metastasis in prostate cancer (Miyata et al, 2006). Similarly, FasL expression has been shown to be upregulated in tumour cells relative to normal tissue and is associated with tumour progression and metastasis (Mann et al, 1999; Osaki et al, 2001; Belluco et al, 2002). As inhibition of FasL expression in colon cancer cells significantly retards tumour formation in mice (Ryan et al, 2005), these findings suggest that targeting the EP1 receptor may help to prevent or treat colon cancer, in part through preventing FasL upregulation in tumour cells.
However, PGE2 has also been shown to downregulate FasL expression in T cells, inhibiting activation-induced cell death (Porter and Malek, 1999). In contrast, FasL expression has recently been shown to be induced in normal colonocytes by PGE2 (Kim et al, 2007). Our results clearly demonstrate that PGE2 induces FasL expression in colon tumour cells. Together, these findings suggest that PGE2 can have multiple effects, perhaps depending on the cell type and oncogenic state of the target cell. Interestingly, in agreement with our findings, the EP1 receptor also played a critical role in PGE2-mediated induction of FasL in normal colonocytes. Although in this model upregulation of FasL expression resulted in colonocyte apoptosis, tumour cells have previously been shown to exhibit enhanced resistance to Fas-mediated apoptosis (Oikonomou et al, 2007). Thus, upregulation of FasL expression in response to PGE2 and subsequent activation of the EP1 receptor, coupled with resistance to Fas-mediated apoptosis, may aid in tumour development. Furthermore, activation of the transcription factor NF-κB was critical for FasL expression in toxin A-exposed colonocytes. Future studies will determine if EP1-mediated activation of NF-κB also plays an important role in inducing FasL expression in colon tumour cells.
In summary, our findings demonstrate that PGE2 upregulates FasL expression in colon cancer cells through the EP1 receptor. Interruption of the PGE2 pathway in vivo has been shown to delay and/or prevent tumour progression in many systems. These anti-tumour effects have been attributed to various mechanisms, such as reduced angiogenesis and increased apoptosis. Our finding that the pro-inflammatory cytokine PGE2 upregulates FasL expression in colon cancer cells adds another pro-neoplastic activity to this pathway, that is, tumour immune evasion, and suggests that targeting the PGE2–EP1–FasL signalling pathway may aid in the development of new therapeutic strategies to both prevent and treat this malignant disease.
Acknowledgments
We acknowledge financial support from the Irish Health Research Board of Ireland and Science Foundation Ireland (no. 5087115226).
References
- Barnhart BC, Legembre P, Pietras E, Bubici C, Franzoso G, Peter ME (2004) CD95 ligand induces motility and invasiveness of apoptosis-resistant tumor cells. EMBO J 22: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belluco C, Esposito G, Bertorelle R, Alaggio R, Giacomelli L, Bianchi LC, Nitti D, Lise M (2002) Fas ligand is up-regulated during the colorectal adenoma–carcinoma sequence. Eur J Surg Oncol 28: 120–125 [DOI] [PubMed] [Google Scholar]
- Bennett MW, O’Connell J, Houston A, Kelly J, O’Sullivan GC, Collins JK, Shanahan F (2001) Fas ligand upregulation is an early event in colonic carcinogenesis. J Clin Pathol 54: 598–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos CL, Richel DJ, Ritsema T, Peppelenbosch MP, Versteeg HH (2004) Prostanoids and prostanoid receptors in signal transduction. Int J Biochem Cell Biol 36: 1187–1205 [DOI] [PubMed] [Google Scholar]
- Cao Y, Prescott SM (2002) Many actions of cyclooxygenase-2 in cellular dynamics and in cancer. J Cell Physiol 190: 279–286 [DOI] [PubMed] [Google Scholar]
- Chulada PC, Thompson MB, Mahler JF, Doyle CM, Gaul BW, Lee C, Tiano HF, Morham SG, Smithies O, Langenbach R (2000) Genetic disruption of Ptgs-1, as well as Ptgs-2, reduces intestinal tumorigenesis in Min mice. Cancer Res 60: 4705–4708 [PubMed] [Google Scholar]
- Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, Van De Putte LB, Lipsky PE (1998) Cyclooxygenase in biology and disease. FASEB J 12: 1063–1073 [PubMed] [Google Scholar]
- Eberhart CE, Coffey RJ, Radhika A, Giardiello FM, Ferrenbach S, DuBois RN (1994) Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology 107: 1183–1188 [DOI] [PubMed] [Google Scholar]
- Erovic BM, Woegerbauer M, Pammer J, Selzer E, Grasl M, Thurnher D (2008) Strong evidence for up-regulation of cyclooxygenase-1 in head and neck cancer. Eur J Clin Invest 38: 61–66 [DOI] [PubMed] [Google Scholar]
- Gupta RA, Tejada LV, Tong BJ, Das SK, Morrow JD, Dey SK, DuBois RN (2003) Cyclooxygenase-1 is overexpressed and promotes angiogenic growth factor production in ovarian cancer. Cancer Res 63: 906–911 [PubMed] [Google Scholar]
- Houston A, O’Connell J (2004) The Fas signalling pathway and its role in the pathogenesis of cancer. Curr Opin Pharmacol 4: 321–326 [DOI] [PubMed] [Google Scholar]
- Kamei D, Murakami M, Nakatani Y, Ishikawa Y, Ishii T, Kudo I (2003) Potential role of microsomal prostaglandin E synthase-1 in tumorigenesis. J Biol Chem 278: 19396–19405 [DOI] [PubMed] [Google Scholar]
- Kawamori T, Kitamura T, Watanabe K, Uchiya N, Maruyama T, Narumiya S, Sugimura T, Wakabayashi K (2005) Prostaglandin E receptor subtype EP(1) deficiency inhibits colon cancer development. Carcinogenesis 26: 353–357 [DOI] [PubMed] [Google Scholar]
- Kim H, Rhee SH, Pothoulakis C, Lamont JT (2007) Inflammation and apoptosis in Clostridium difficile enteritis is mediated by PGE2 up-regulation of Fas ligand. Gastroenterology 133: 875–886 [DOI] [PubMed] [Google Scholar]
- Lambert C, Landau AM, Desbarats J (2003) Fas—Beyond death: a regenerative role for Fas in the nervous system. Apoptosis 8: 551–562 [DOI] [PubMed] [Google Scholar]
- Li H, Cai X, Fan X, Moquin B, Stoicov C, Houghton J (2008) Fas Ag–FasL coupling leads to ERK1/2-mediated proliferation of gastric mucosal cells. Am J Physiol Gastrointest Liver Physiol 294: G263–G275 [DOI] [PubMed] [Google Scholar]
- Mann B, Gratchev A, Bohm C, Hanski ML, Foss HD, Demel G, Trojanek B, Schmidt-Wolf I, Stein H, Riecken EO, Buhr HJ, Hanski C (1999) FasL is more frequently expressed in liver metastases of colorectal cancer than in matched primary carcinomas. Br J Cancer 79: 1262–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto N, Imamura R, Suda T (2007) Caspase-8- and JNK-dependent AP-1 activation is required for Fas ligand-induced IL-8 production. FEBS J 274: 2376–2384 [DOI] [PubMed] [Google Scholar]
- Miyata Y, Kanda S, Maruta S, Matsuo T, Sakai H, Hayashi T, Kanetake H (2006) Relationship between prostaglandin E2 receptors and clinicopathologic features in human prostate cancer tissue. Urology 68: 1360–1365 [DOI] [PubMed] [Google Scholar]
- Nagata S, Golstein P (1995) The Fas death factor. Science 267: 1449–1456 [DOI] [PubMed] [Google Scholar]
- O’Connell J, Houston A, Bennett MW, O’Sullivan GC, Shanahan F (2001) Immune privilege or inflammation? Insights into the Fas ligand enigma. Nat Med 7: 271–274 [DOI] [PubMed] [Google Scholar]
- O’Connell J, O’Sullivan GC, Collins JK, Shanahan F (1996) The Fas counterattack: Fas-mediated T cell killing by colon cancer cells expressing Fas ligand. J Exp Med 184: 1075–1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oikonomou E, Kothonidis K, Zografos G, Nasioulas G, Andera L, Pintzas A (2007) Newly established tumourigenic primary human colon cancer cell lines are sensitive to TRAIL-induced apoptosis in vitro and in vivo. Br J Cancer 97: 73–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okada K, Komuta K, Hashimoto S, Matsuzaki S, Kanematsu T, Koji T (2000) Frequency of apoptosis of tumor-infiltrating lymphocytes induced by fas counterattack in human colorectal carcinoma and its correlation with prognosis. Clin Cancer Res 6: 3560–3564 [PubMed] [Google Scholar]
- Osaki M, Kase S, Kodani I, Watanabe M, Adachi H, Ito H (2001) Expression of Fas and Fas ligand in human gastric adenomas and intestinal-type carcinomas: correlation with proliferation and apoptosis. Gastric Cancer 4: 198–205 [DOI] [PubMed] [Google Scholar]
- Peter ME, Budd RC, Desbarats J, Hedrick SM, Hueber AO, Newell MK, Owen LB, Pope RM, Tschopp J, Wajant H, Wallach D, Wiltrout RH, Zornig M, Lynch DH (2007) The CD95 receptor: apoptosis revisited. Cell 129: 447–450 [DOI] [PubMed] [Google Scholar]
- Porter BO, Malek TR (1999) Prostaglandin E2 inhibits T cell activation-induced apoptosis and Fas-mediated cellular cytotoxicity by blockade of Fas-ligand induction. Eur J Immunol 29: 2360–2365 [DOI] [PubMed] [Google Scholar]
- Qiao L, Kozoni V, Tsioulias GJ, Koutsos MI, Hanif R, Shiff SJ, Rigas B (1995) Selected eicosanoids increase the proliferation rate of human colon carcinoma cell lines and mouse colonocytes in vivo. Biochim Biophys Acta 1258: 215–223 [DOI] [PubMed] [Google Scholar]
- Rask K, Zhu Y, Wang W, Hedin L, Sundfeldt K (2006) Ovarian epithelial cancer: a role for PGE2-synthesis and signalling in malignant transformation and progression. Mol Cancer 5: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restifo NP (2000) Not so Fas: re-evaluating the mechanisms of immune privilege and tumor escape. Nat Med 6: 493–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigas B, Goldman IS, Levine L (1993) Altered eicosanoid levels in human colon cancer. J Lab Clin Med 122: 518–523 [PubMed] [Google Scholar]
- Ryan AE, Shanahan F, O’Connell J, Houston AM (2005) Addressing the ‘Fas counterattack’ controversy: blocking fas ligand expression suppresses tumor immune evasion of colon cancer in vivo. Cancer Res 65: 9817–9823 [DOI] [PubMed] [Google Scholar]
- Sano H, Kawahito Y, Wilder RL, Hashiramoto A, Mukai S, Asai K, Kimura S, Kato H, Kondo M, Hla T (1995) Expression of cyclooxygenase-1 and -2 in human colorectal cancer. Cancer Res 55: 3785–3789 [PubMed] [Google Scholar]
- Shoji Y, Takahashi M, Kitamura T, Watanabe K, Kawamori T, Maruyama T, Sugimoto Y, Negishi M, Narumiya S, Sugimura T, Wakabayashi K (2004) Downregulation of prostaglandin E receptor subtype EP3 during colon cancer development. Gut 53: 1151–1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldner M, Schimanski CC, Neurath MF (2006) Colon cancer and the immune system: the role of tumor invading T cells. World J Gastroenterol 12: 7233–7238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Dubois RN (2006) Prostaglandins and cancer. Gut 55: 115–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe K, Kawamori T, Nakatsugi S, Ohta T, Ohuchida S, Yamamoto H, Maruyama T, Kondo K, Ushikubi F, Narumiya S, Sugimura T, Wakabayashi K (1999) Role of the prostaglandin E receptor subtype EP1 in colon carcinogenesis. Cancer Res 59: 5093–5096 [PubMed] [Google Scholar]
- Whiteside TL (2007) The role of death receptor ligands in shaping tumor microenvironment. Immunol Invest 36: 25–46 [DOI] [PubMed] [Google Scholar]
- Williams CS, DuBois RN (1996) Prostaglandin endoperoxide synthase: why two isoforms? Am J Physiol 270: G393–G400 [DOI] [PubMed] [Google Scholar]
- Younes M, Schwartz MR, Ertan A, Finnie D, Younes A (2000) Fas ligand expression in esophageal carcinomas and their lymph node metastases. Cancer 88: 524–528 [PubMed] [Google Scholar]