Abstract
Objective
Innovative approaches can strengthen patient-caregiver-clinician information exchange and more effectively address the physical and psychosocial challenges of advanced disease. This study reports initial findings from implementation of the Clinician Report (CR)—a patient and caregiver status report tool accessible by the oncology clinic team.
Design
The CR tracks and communicates essential information from cancer patients and caregivers to the oncology team. The CR conveys patient symptoms, emotional strain, and key concerns.
Measurements
Authors used a model developed to explain acceptance, implementation, and sustainability of Interactive Health Communication Systems (IHCS) to evaluate implementation of the new CR system. The study carried out qualitative analyses of interviews with clinicians regarding their experience utilizing the Clinician Report.
Results
Primary CR benefits included enhancement of patients' clinic visit experiences, greater caregiver involvement, and facilitation of earlier interventions. Challenges included CR functional issues, users' desire for greater depth of information, user privacy concerns, and limited patient use. These findings are discussed using parameters of the implementation model. Limitations of this study include its small clinician sample size, which represented only a portion of existing organizational settings in which CR systems might be implemented.
Conclusion
Though in its early implementation stages, the CR demonstrates the potential to positively impact care delivery in the cancer clinic setting, particularly by facilitating earlier interventions and improving patient-caregiver-clinician communication both during and between clinic visits.
Introduction
As part of a larger study evaluating a web-based interactive health communication system (IHCS), this study reports initial findings regarding the implementation of the Clinician Report (CR)—a patient status reporting tool used by the patient and/or caregiver and accessible by the oncology clinic team. Authors present benefits and challenges of this reporting system through the parameters of the IHCS implementation model.
Background
The diagnosis of advanced cancer often invokes fear, despair and hopelessness in patients and their families. Coping well with advanced cancer requires effective and ongoing communication among patients, caregivers and clinicians. In order to intervene more appropriately, clinicians can benefit from timely updates on patients' clinical and psychosocial statuses between scheduled clinical encounters. Conversely, patients and their caregivers need clinical information, advice, and emotional support to respond to the rapidly changing physical, spiritual, and emotional burdens of advanced cancer. Timely information and available support can enhance crucial end of life communication between patients, their families and the clinical team. Ineffectiveness in any of these lines of communication will compromise patient-caregiver-clinician information exchange, and will often result in less-than-ideal care.
Cancer Communication Barriers
Unfortunately, the information exchange among patients, caregivers and clinicians is frequently hindered by healthcare system-related factors and by the circumstances of the individuals in the patient-caregiver-clinician triad. Often, patients and caregivers do not share physical and emotional concerns with the clinical team, 1–9 or when they do, they exclude psychosocial issues that are very important in cancer care. 10–11 Many clinicians feel pressure to spend less time with their patients due to current productivity objectives; others may believe they do a good job of information sharing when they do not, and some clinicians believe it is not their job to talk to patients about emotional and spiritual aspects of cancer and dying. 12–14
Benefits of Effective Communication
By understanding changes in the patient's clinical and psychosocial status, as well as monitoring the caregiver's ability to support the patient as needed, clinicians could more efficiently and effectively improve patients' and caregivers' quality of life. Timely communication between clinicians and caregivers in late-stage cancer can accomplish the following: facilitate information exchange, leading to adjustments in symptom treatment; facilitate individuals' participation in care and decision-making; and allow discussion about existential issues involved in death and dying. 15–24 Conversely, breakdowns in information exchange increase health care costs 20 and lead to unnecessary suffering. 25–27 Substantial evidence indicates that damaging effects accrue to caregivers when needed information and support are lacking. 28–30
Communication Innovations
While new approaches could improve information sharing and support, 31 past interventions have had mixed success. Some studies found that when patients or caregivers are assertive, physicians are more attentive. 32–33 In contrast, the SUPPORT study, 34 involving 4800 patients, found that physician behavior did not change despite an intensive intervention to improve patient-physician communication. Specially trained nurses repeatedly communicated patient or family preferences and concerns. The nurses encouraged physicians to address pain control, advance care planning and to communicate with the patient and family. 34
Newer, technology-based communication methods have the potential to bring patients, caregivers and clinicians together as a united team. Several studies have shown that electronic symptom monitoring is feasible and effective in chronic illness settings such as asthma and diabetes. 35–39 While few studies have examined such applications in cancer populations, preliminary evidence suggests that patients and caregivers will complete computerized assessments and that those assessments can influence clinician behavior. 40–43 For instance, interactive health computer systems have collected patient/caregiver information in a number of settings and shared it with clinicians. 40,42 Armed with such additional knowledge prior to the clinic visit, clinicians can streamline their assessment accordingly. This provides more time to address deeper concerns (e.g., giving difficult news in a sensitive way), increased opportunities to listen to patients and to encourage their questions, and improved ability to sense when patients are ready to talk about death. 17,19,44–45
The NIH-funded, multi-center collaborative Patient-Reported Outcomes Measurement Information System (PROMIS) project examines opportunities to develop and administer clinical research questions about quality of life to patients undergoing treatments for chronic diseases. Collecting information from patients about quality of life is important in regular clinic practice. A recent study indicated the benefits of patient self-reporting while undergoing cancer chemotherapy. 42
The CR comprises one of many possible approaches to administering key questions that patients (or caregivers) can answer in ‘real time.' In addition, the CR provides a mechanism for clinicians to receive the most current information regarding a patient's status. Nevertheless, with the promotion of new technologies to improve clinician-patient communication comes problems that pose challenges to implementing technological advances. These obstacles to interactive health communication systems involve the clinicians, patients and caregivers, along with information system staff and the targeted healthcare organization (in this case the cancer clinics). 46 Successful technology implementation depends upon characteristics of the innovation itself, the organization, and the manner in which the implementation process unfolds.
Formulation Process
In an effort to facilitate patient-caregiver-clinician communication, the CR was conceived as a new feature to enhance the pre-existing CHESS (Comprehensive Health Enhancement Support System) website. 47–49 Two ongoing clinical trials were in place, testing the effectiveness of the CHESS system for caregivers of advanced cancer patients (more details in Validation Through Example section). A multidisciplinary research team—including experts in clinical systems industrial engineering, oncology, clinical psychology, communications, graphic design and programming—designed the CR system to work within the CHESS website. The CR content and interactive features derived from initial testing with paper-based prototypes. 50,51 This method optimized CR development by allowing project members to test specific features without delays imposed by programming time, and in turn facilitated rapid cycling of modifications for further prototyping and testing. Three oncologists representing different subspecialties (prostate cancer, breast cancer, and palliative care) provided primary feedback regarding numerous iterations of paper prototypes for the patient status report page. Their feedback covered CR content, functionality and design issues.
Based on literature review of current oncology practices, and clinician feedback, the project decided to measure patients' symptom levels and functional status using familiar measures commonly used in clinical practice—the Edmonton Symptom Assessment Scale (ESAS) 52 and Karnofsky Performance Scale. 53 The project modified these measures somewhat to include additional symptoms that project clinicians had found useful in their practices (e.g., tracking diarrhea). The final list of CR symptoms included pain, fatigue, shortness of breath, diarrhea, constipation, poor appetite, sleep disturbance, depression, anxiety, and distress. Additional questions assessed caregiver burden and confidence. After determining the basic content and design elements through paper prototyping, the project team developed an online prototype for which the oncologists provided additional feedback through hands-on testing.
Model Description
The Clinician Report (CR) is one of many features available through CHESS (Comprehensive Health Enhancement Support System), a non-commercial interactive health communication system (IHCS) developed at the University of Wisconsin-Madison. 47–49 In an easy-to-use, Internet-based format, CHESS provides to users (patients and their caregivers) information, strategies that promote behavior change, tools for decision-making, and access to support services. A critically important aspect of CHESS is that it provides a closed, guided universe of tailored information and support options through an integrated package. Within CHESS, every item points efficiently to other salient materials; the system does not make users employ complicated search and discovery methods. Built upon a model of coping self-efficacy, CHESS helps users to appraise the controllability of cancer-related stressors and to improve their coping skills. 47–48,54
The CHESS website is secure: users must have a codename and password to access CHESS. Information entered by CHESS users is encrypted before being sent to a secure server housed at the central research site. In implementing the Clinician Report, CHESS operated as an independent system. It was not integrated into the participating clinic's existing computerized systems. The programming and web design were developed by staff at the CHESS research center. The CHESS is proprietary software and meets accessibility standards as set by the Federal Rehabilitation Act Section 508. The CHESS software is owned by the Wisconsin Alumni Research Foundation (WARF); the authors do not have any financial relationship with WARF.
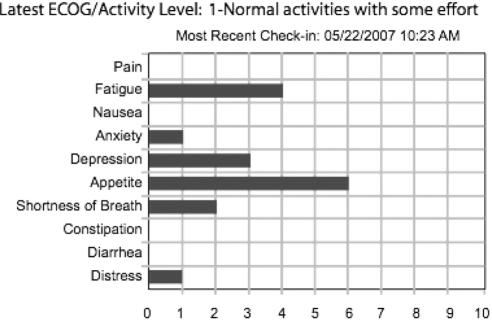
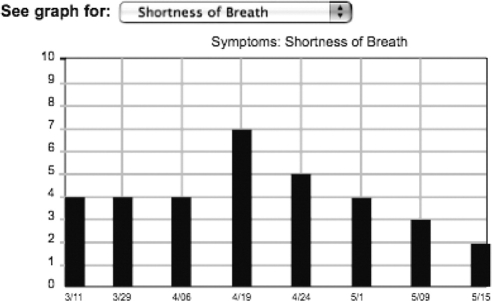
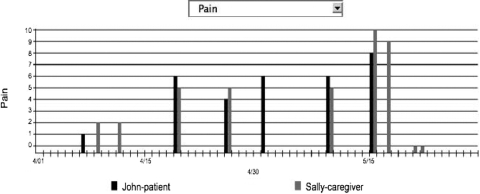
Via the Check-In Service, CHESS tracked changes in key patient and caregiver status information. Each week, patients and/or caregivers completed a short Check-In questionnaire, which asked them to revise previous answers to questions about patient symptom status and, for caregivers, their caregiving-related burden. The Check-In process also asked users to list questions they had for the next scheduled clinic visit. After logging in with a codename and password, the clinical team could review a summary page that listed all their patients who used the CR. Clinicians could readily access the most recent check-in report for each individual. The CR provided a graphical summary of the patient's symptom scores for each of the ten modified ESAS symptom items (▶). One type of graphical display depicted the most recent score for each item, and another type of display allowed clinicians to examine scores for any one of the ten symptoms longitudinally over time for up to eight previous entries (▶). An additional display category showed members of the clinical team a side-by-side comparison chart of patient and caregiver ratings of selected symptoms (▶). The CR also summarized information needs conveyed by patients and their caregivers, providing clinical staff with an understanding of topics that were important concerns. Finally, the CR indicated to providers the questions and comments that patients and caregivers wanted to address at their next clinic visit. The CHESS system saved data as they were entered and could create and display the above-noted reports after each Check-In was completed.
Figure 1.
Most recent ratings on symptom items.
Figure 2.
Longitudinal view of selected symptom item.
Figure 3.
Comparison of patient and caregiver ratings for selected symptom item.
The clinical team received CR reports about patients and their caregivers in three ways. First, a clinician could log onto CHESS with an approved name and password, and then access a summary report of their patients. Second, for qualifying patients, the CHESS system generated an e-mail message that was immediately sent to clinician-designated staff whenever the patient's CR exceeded a threshold score (at least 7 on a 0–10 scale) for at least one ESAS symptom item. Finally, clinicians also received a CR email two days before a scheduled clinic visit.
The CR was designed to accommodate a variety of organizational structures. Clinicians could select which members of their clinical teams were to receive email alerts. Furthermore, while the CR design easily provided detailed information through interactive web links, clinicians could alternatively print out reports—e.g., for personal quick reference or for inclusion in patients' charts.
Validation through Example
Study Context
Providing a detailed description of the larger longitudinal CHESS study falls beyond the scope of the current article. Nevertheless, a brief summary of this study follows to clarify the context in which authors implemented the Clinician Report (CR). The larger study participants included advanced-stage breast cancer, prostate cancer, and lung cancer patients and their identified community-based caregivers. The study recruited subjects from five major cancer centers in the Northeastern, Midwestern and Southwestern United States. Eligibility criteria varied by patients' types of cancer. Eligible prostate cancer patients included men with hormone refractory or metastatic disease. For a woman with breast cancer to be eligible for the study, she had to have one of the following: 1) a diagnosis of metastatic breast cancer, 2) recurrent or metastatic inflammatory breast cancer, or 3) a chest wall recurrence following mastectomy. Eligible lung cancer patients included those with non-small cell lung cancer at stage IIIA, IIIB, or IV. Participating caregivers completed pretests and bi-monthly follow-up surveys for either one year (breast and prostate cancer) or two years (lung cancer). The longitudinal surveys examined the impact of CHESS on patients and caregivers.
The above-described study enrolling patients with breast cancer or prostate cancer had two arms. Both arms gave participants a computer, Internet access, and access to the CHESS website. In addition, only one research arm provided the CR feature via CHESS. The lung cancer study had two arms, with the “usual care” control group receiving only a computer and Internet access, and the intervention group added access to the CHESS website including the CR. In both studies, after completion of the pretest survey, patient-caregiver dyads were randomized within respective study treatment arms and provided with computers, Internet, and CHESS access as appropriate. The study provided training on how to use the computer and Internet (and CHESS website) to those who wanted such instruction. Participants completed follow-up surveys every two months for the duration of the study. The University of Wisconsin Health Sciences Institutional Review Board approved both studies.
The study also obtained consent from clinicians to participate in each study, because they had to be willing to accept and potentially utilize the Clinician Report email alerts as part of their clinic practice for patients who were randomized to that condition. The study did not prescribe how clinicians were to use the Clinician Report or how they should respond to the information reported, as the objective was to learn how clinicians would naturally adapt this information into their individual clinic flow. Furthermore, the project team was concerned that prescribing specific changes in clinician behavior might cause clinicians to perceive the study as burdensome, which would deter their interest in participating due to high baseline workloads. The study trained participating clinicians on how to use the Clinician Report.
Clinician Report Evaluation
All clinicians in the current study were involved in the larger clinical trials being conducted with advanced stage cancer patients and their caregivers. The three study interviewers were researchers who had developed the CR system. At least two interviewers were present at each interview, and took notes. All participating interviewers present at each session generated summaries of key points for the session, and reviewed the summaries to assure an accurate record of the interview. The interviewers met with participating clinic staff to understand: (a) how the staff used the CR in the clinic setting; (b) perceived overall CR functionality; and, (c) user-suggested ways to improve the CR. At the time of the interviews, a total of 107 patients (46 breast, 34 prostate, and 27 lung) had access to the CR system. The subset of study clinicians who were interviewed had between 6 and 33 patients within their caseloads who were in the CR study arm. Some clinicians were not interviewed as they had fewer than two patients in the CR study arm, and therefore not enough exposure to the CR system to provide feedback. Clinicians who could not successfully schedule even telephone interviews were excluded from the study. The project team interviewed seven clinicians (three doctors specializing in lung, prostate, or breast cancer, and four cancer center nurses) individually or in small groups over a two-month period approximately 18 months after the first patient-provider pair was randomized to the CR arm. The study interviewed clinic nurses six months later (at approximately 24 months into the CR study) to obtain feedback on the effectiveness of changes made to the CR based on initial interview feedback.
A project graduate research assistant used content analysis to independently organize the interviewees' comments regarding the CR into the overarching categories of: Utilization, Benefits, and Challenges. Benefits were further divided into four categories: Enhanced Clinic Visit Experience, Enhanced Caregiver Involvement, Enabled Earlier Intervention, and Appropriate Measures. Challenges were divided into five categories: Functionality, Limited Use, User Privacy, Measurement Design, and Limits of Technology. Two project researchers who had conducted the interviews reviewed the graduate research assistant's categorizations independently. Disagreements were resolved through discussion.
Utilization of the Clinician Report
The adaptive design of the CR to work within disparate clinic organizational structures led to a variety of methods of its use. Three clinics that relied on paper charting reported using a key staff member to receive CR email alerts and print copies of CR reports for placement in patients' charts. One exception was an individual physician comfortable with using e-mail and other electronic tools. In contrast, two clinics using electronic medical record (EMR) systems accessed CR information directly online. Given that there was no direct interface within the EMR to CR, clinicians reported that CR utilization would be more efficient if CR was incorporated into the EMR they were already using. Nevertheless, clinicians used the CR information in a variety of contexts: to provide references at the clinic visit, to alert nursing staff to issues arising between visits (at times precipitating a telephone follow-up, as appropriate), and to serve as references in discussions at regularly scheduled clinical case meetings.
Benefits of the Clinician Report
The current study identified four categories of positive CR attributes. Overall, the nursing staff rated the CR more helpful than did physicians.
1) Enhanced Clinic Visit Experience. The CR helped clinicians prepare for clinic visits and enhanced communication and interactions among clinicians, patients and caregivers. One nurse stated the CR “gave them a heads up about a problem before the visit” so that they were better prepared to discuss patients' and caregivers' concerns.
2) Enhanced Caregiver Involvement. Clinicians recognized that the CR enhanced involvement of caregivers during the clinical encounter. That CR provided caregivers capabilities to directly describe the patient's condition and to report their own concerns to the clinical staff helped caregivers to feel “a part of the team.” The CR also helped clinicians recognize areas where patients and caregivers rated the patient's symptoms differently. This provided a basis for nurses to “spark communication between the patient and caregiver, as well as themselves.”
3) Enabled Earlier Intervention. The CR automatically generated alerts to clinical teams when a reported symptom exceeded a predefined threshold level. Clinicians appreciated that such potentially urgent issues might otherwise have gone unreported and unattended. As one nurse stated, “Threshold reports help us get earlier information. Earlier intervention was achieved.”
4) Applied Appropriate Measures. Clinicians generally agreed that the threshold level for reporting of “7” on the 0–10 scale was appropriate for filtering e-mail alerts. While clinicians did not report receiving too many email alerts, they stated the numeric rating limited the usefulness of the information reported (see Challenges below). Generally, clinicians agreed that the variety of symptoms measured on the CR were appropriate for their practice needs and concerns.
Challenges for the Clinician Report
The study identified five areas for improvement in the CR system and implementation.
1) Functionality. Clinicians initially reported having difficulty in printing the CR from their computers. Clinician-users wanted all reported symptoms to appear on one page rather than printing one symptom per page. This issue was resolved by redesigning the presentation format of the CR. Clinicians also suggested that an enhanced version of CR might offer patients and caregivers feedback in response to their symptom ratings—for example, steering them to enter or view additional appropriate information (e.g., “You reported high pain. Check out the information related to pain management …”)—or providing them with instructions for taking appropriate actions (e.g., “Please call your clinician”).
2) Limited Use. Clinicians expressed concern that caregivers appeared to use the CR more often than the patients. Clinicians were uncertain how to handle information that was provided by the caregiver but not substantiated by the patient. Accordingly, they would like to receive more reports from patients “whose information was crucial to trigger the interventions.” A lung cancer clinic nurse hypothesized that their patients' usage might be low because lung cancer patients are not as “information hungry” as other types of cancer patients, possibly due to the grim prognostic information available.
3) User Privacy. Clinicians raised two key concerns regarding user privacy. First, in the initial system, patients and caregivers entered their questions prior to a clinic visit into a shared text box. Both oncologists and nurses were concerned that sharing this space may “deter caregivers from asking questions, such as ”what ifs” that they would not want the patient to see and vice versa. Furthermore, unsolicited comments from caregivers and patients revealed that this was an important issue for them as well. Sometimes either the patient or caregiver had a sensitive question to ask the doctor and preferred to keep it confidential. In response to this early feedback, the project staff altered the CR to contain private text boxes for patient and caregivers to separately list their questions and concerns. In addition, to address the concern that clinicians might mistakenly divulge such private questions, CR adds an alert to the clinicians warning them that such questions may need to be addressed privately. Clinicians raised a second, related issue: whether data provided by the caregiver alone should be included as part of the patient's medical record.
4) Measurement Design. Currently, the CR uses 0–10 likert-type scales to quantitate patients' symptoms. Clinicians requested additional descriptions that “contain more detailed, objective information of symptoms, such as sleeping more than 15 hrs or less than 4 hours.” Clinicians also indicated that some CR-documented symptoms were already frequently monitored at regularly scheduled clinic visits, so that CR did not provide additional useful information. In response, an interim change to the CR added a text box requesting greater detail when a symptom is reported at threshold level. Some clinicians reported that this additional feature has been beneficial. Clinicians also suggested adding a measure of dehydration, a critical issue that patients face during treatment. Furthermore, clinicians felt greater input from the patient could be solicited by altering the wording of the “questions for next visit” box by asking patients, “What do you feel needs to be addressed at your next visit?” However, future improvements must address additional concerns discussed below.
5) Limits of Technology. Clinicians also identified limitations due to the very nature of the CR's technical properties. Symptoms rating scales, brief problem descriptions, and/or time-delayed written communication cannot convey many categories of critical patient data and needs. At that point, telephone conversations provide greater “bandwidth” and efficiency, and become necessary. As reflected by one nurse, “the information provided in the CR may not be the most clear and phone conversation would be preferred.”
Discussion
The development and implementation of the Clinician Report service for patients with advanced cancer was a dynamic process that involved iterative clinician feedback and system redesign. The current pilot, informal evaluation study provides insight into beneficial features that such systems can provide, identifies desiderata that challenge current system capabilities, and indicates areas for future development and research.
Application of the Readiness for IHCS Implementation Model
The Readiness for IHCS Implementation Model 46 identifies seven factors to address in the implementation of such systems: organizational environment; organizational motivation; technology usefulness; promotion; implementation process; department-technology fit; and key personnel awareness and support. The project team summarizes below the study findings regarding CR acceptability and utility in the context of these factors.
For the CR, the organizational environment included the nature of the clinics in which the system was implemented. The CR had to address security, privacy, and confidentiality issues. The CHESS system (including CR) collected and provided clinical data through a secure, password-protected website. To protect each individual's confidentiality, the patient and caregiver logged in separately to the system to respond to the check-in questions. Nevertheless, clinicians who received both patient and caregiver comments saw merit in doing so, but they expressed concerns about how to address caregiver reports that were not substantiated by the patient. Some contentious issues remained, including whether the CR should become part of the patient record, and whether to initiate patient contact based on information provided by the caregiver.
Healthcare, and cancer care in particular, benefits from the ability to intervene early in patients' problems, at a time when preventive actions might avert critical situations escalating into a crisis. As the CR enabled earlier interventions on key symptom-related problems, it fulfilled the organizational motivation to improve communication with patients and families to intervene in their problems earlier.
The CR demonstrated a degree of technological usefulness. The threshold levels for symptoms to generate alerts resulted in an appropriate volume of alerts, which the team believed was appropriate for notification about patient concerns. In contrast, clinicians raised concerns regarding the usefulness of numerically scaled symptom reports. The interim addition of a text box for describing symptoms in greater detail provided some benefit. Nevertheless, planned additional improvements must add more detailed operational assessment capabilities (e.g., “Have not had a bowel movement in the last three days despite taking medicine to help with bowel movements.”). Overall, the CR study provided the clinics an affordable and easy way to test a new communication tool with patients and caregivers. Challenges identified included a desire for greater depth of patients' problem details, such as those that could only be obtained via interactive telephone conversations or direct person-to-person dialogues.
Despite staff, patient, and caregiver training regarding use of the CR, the ongoing promotion of the system presented many challenges. Clinicians perceived the system as primarily used by caregivers rather than patients, and thus less useful. Lack of direct use by patients with advanced stage cancers may occur because patients are physically less able to use information systems like CHESS (due to severe symptoms that inhibit sitting at the computer), or they may be less motivated because they are too sick or feel helpless in the face of a poor prognosis. Future innovative approaches may overcome such hurdles and enhance cancer care.
While the customizability of the CR system (i.e., clinicians choose who received reports, as well as online and/or print capabilities) facilitated the implementation process, challenges arose due to the inability of CR to adapt to existing practices in the clinic. For example, the CR required clinicians to log into a separate website rather than to link out to CR during review of a patient's information in the familiar EMR or paper chart. Thus, using CR required additional steps for the clinical team during an already busy day. Furthermore, due to eligibility criteria of the clinical trial, each clinician had only a small portion of their patient population utilizing the CR system. The clinicians might have adapted to CR more easily if it had been implemented uniformly across their practice.
The CR demonstrated good department-technology fit by positively impacting care providers' activities. Consistent with previous IHCS research 39,43–45 clinicians found that the Clinician Report better prepared them to address patient concerns during clinic visits. The CR also enhanced communication among clinicians, patients and caregivers. Although the CR could not provide real-time patient-clinician dialog regarding patients' symptoms, it at least alerted the clinical team earlier to issues that might require further attention. While such alerts might cause clinical staff to initiate telephone contacts with patients, inconsequential alerts could inflate clinicians' workloads in an already busy clinical setting.
The successful implementation of IHCS like the CR requires the awareness and support of key personnel. The CR implementation required clinician, patient and caregiver involvement. Within the clinic, nursing staff were primary users of the CR, but physician support for the CHESS research study and use of the CR was a critical factor for the CR implementation.
Limitations and Future Directions
The current study provides initial impressions from early implementation of a clinician reporting system for patients with advanced cancer. It occurred in the context of a large scale clinical trial examining the impact of an internet-based information and support system for cancer patients and their informal caregivers. Because the current study design was not a formal implementation evaluation, limitations occurred in the analysis of the CR. The small number of clinicians, representing a small sample of organizational roles, who provided feedback decreased study generalizability. Each organization has its own unique environment, motivation, and other factors that will affect implementation of a system like a CR. Despite these limitations, the current study attempted to identify essential factors to consider when implementing CR-like systems in other healthcare organizations.
Future CR-like system implementations should consider the clinician feedback reported here as potentially relevant. One such finding was that CR systems should be integrated within existing medical record system frameworks in an organization, not as a standalone system—clinicians should be able to access the CR seamlessly from the EMR. In addition, presentation design, such as graphics, should be consistent with existing frameworks with which clinicians are familiar. Additional desiderata include the ability to tailor how patients' symptoms are measured and reported, based on the needs of an individual clinic or patient population. Accordingly, criteria for when clinicians receive reports or alerts should follow from the symptoms they indicate are useful in their specific practices. Future CR systems should provide more specific, objective threshold criteria that allow clinicians to customize cutoffs for each patient. The ongoing CHESS clinical trials are collecting patient, caregiver and clinician login data that will better characterize the exact nature of CR system use (i.e., who used it, how often, and in correlation with what specific events) to further inform CR system development.
Conclusion
While still early in its implementation, the CHESS Clinician Report system has demonstrated the potential to make a positive impact in the cancer clinic setting through facilitating patient-caregiver-clinician communication before and during patient encounters, and in promoting earlier interventions, prior to symptom-related crises. However, limitations remain that should be addressed through future design elements, and by better integrating CR within existing organizational processes and systems. Future successful implementations of the CR may depend on a good fit between the needs of particular clinicians (i.e., nursing staff vs. oncologists), and larger organizational structure. The unique culture of various cancer clinics will be a key factor in insuring future CR implementation success. 46
Footnotes
This research was made possible through grant funding from the National Cancer Institute (1 P50 CA095817-01A1) and National Institute of Nursing Research (RO1 NR008260-01). This research was presented at the Critical Issues in eHealth Research Conference, Bethesda, MD, September 11, 2006, as a poster titled “Evaluation of the Utility of an Online Reporting System that Connects Cancer Patients and Their Informal Caregivers to Their Clinical Team.”
References
- 1.Dar R, Beach CM, Barden PL, Cleeland CS. Cancer pain in the marital system: a study of patients and their spouses J Pain Symptom Manage 1992;7(2):87-93. [DOI] [PubMed] [Google Scholar]
- 2.Roter D, Hall JA. Doctors talking with patients/patients talking with doctors: improving communication in medical visitsWestport (CN): Auburn House; 1992.
- 3.Von Roenn JH, Cleeland CS, Gonin R, Hatfield AK, Pandya KJ. Physician attitudes and practice in cancer pain management: A survey from the Eastern Cooperative Oncology Group Ann Intern Med 1993;119(2):121-126. [DOI] [PubMed] [Google Scholar]
- 4.Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview JAMA 1997;277(8):678-682. [PubMed] [Google Scholar]
- 5.Guadagnoli E, Ward P. Patient participation in decision-making Soc Sci Med 1998;47(3):329-339. [DOI] [PubMed] [Google Scholar]
- 6.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions Am J Prev Med 1999;17(4):285-294. [DOI] [PubMed] [Google Scholar]
- 7.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model Soc Sci Med 1999;49(5):651-661. [DOI] [PubMed] [Google Scholar]
- 8.Maguire P. Improving communication with cancer patients Eur J Cancer 1999;35(10):1415-1422. [DOI] [PubMed] [Google Scholar]
- 9.Street R. Active patients as powerful communicators: The linguistic foundation of participation in health careIn: Robinson WP, Giles H, editors. The new handbook of language and social psychology. 2nd ed.. Chichester (England): Wiley; 2001. pp. 541-560.
- 10.Cull A, Stewart M, Altman DG. Assessment of and intervention for psychosocial problems in routine oncology practice Br J Cancer 1995;72(1):229-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osoba D. Rationale for the timing of health-related quality-of-life (HQL) assessments in oncological palliative therapy Cancer Treat Rev 1996;22(Suppl A):69-73. [DOI] [PubMed] [Google Scholar]
- 12.Waitzkin H. Information Giving in Medical Care J. Health Soc. Behav 1985;26(2):81-101. [PubMed] [Google Scholar]
- 13.Ballard-Reisch DS. A model of participative decision making for physician-patient interaction Health Commun 1990;2(2):91-104. [Google Scholar]
- 14.Charles C, Gafni A, Whelan T. How to improve communication between doctors and patients: learning more about the decision making context is important BMJ 2000;320(7244):1220-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beisecker AE. Older persons' medical encounters and their outcomes Res Aging 1996;18(1):9. [Google Scholar]
- 16.Byock I. Dying well: the prospect for growth at the end of lifeNew York: Riverhead Books; 1997.
- 17.Dudley JR, Smith C, Millison MB. Unfinished business: assessing the spiritual needs of hospice clients Am J Hosp Palliat Care 1995;12(2):30-37Mar–Apr. [DOI] [PubMed] [Google Scholar]
- 18.Keller V, Carroll J. A new model for physician-patient communication Patient Educ Couns 1994;23:131-140. [DOI] [PubMed] [Google Scholar]
- 19.Lo B, Quill T, Tulsky J, ACP-ASIM End-of-Life Care Consensus Panel Discussing palliative care with patients Ann Intern Med 1999;130(9):744-749May 4. [PubMed] [Google Scholar]
- 20.Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature Soc Sci Med 1995;40(7):903-918. [DOI] [PubMed] [Google Scholar]
- 21.Tulsky JA, Fischer GS, Rose MR, Arnold RM. Opening the black box: how do physicians communicate about advance directives? Ann Intern Med 1998;129(6):441-449. [DOI] [PubMed] [Google Scholar]
- 22.Detmar SB, Muller MJ, Wever LD, Schornagel JH, Aaronson NK. The patient-physician relationship. Patient-physician communication during outpatient palliative treatment visits: an observational study. JAMA 2001;285(10):1351-1357. [DOI] [PubMed] [Google Scholar]
- 23.Arora NK. Interacting with cancer patients: the significance of physicians' communication behavior Soc Sci Med 2003;57(5):791-806. [DOI] [PubMed] [Google Scholar]
- 24.Stewart MA. Effective physician-patient communication and health outcomes: a review CMAJ 1995;152(9):1423-1433. [PMC free article] [PubMed] [Google Scholar]
- 25.Cegala DJ. A study of doctors' and patients' communication during a primary care consultation: implications for communication training J Health Commun 1997;2(3):169-194Jul–Sep. [DOI] [PubMed] [Google Scholar]
- 26.Northouse LL. Social support in patients' and husbands' adjustment to breast cancer Nurs Res 1988;37(2):91-95Mar–Apr. [PubMed] [Google Scholar]
- 27.Northouse PG, Northouse LL. Communication and cancer: issues confronting patients, health professionals, and family members J Psychosoc Oncol 1987;5(3):17-46. [Google Scholar]
- 28.Northouse LL, Peters-Golden H. Cancer and the family: strategies to assist spouses Semin Oncol Nurs 1993;9(2):74-82. [DOI] [PubMed] [Google Scholar]
- 29.Peters-Golden H. Breast cancer: varied perceptions of social support in the illness experience Soc Sci Med 1982;16(4):483-491. [DOI] [PubMed] [Google Scholar]
- 30.Vitaliano PP. Physiological and physical concomitants of caregiving: introduction Ann Behav Med 1997;19(2):75-77. [DOI] [PubMed] [Google Scholar]
- 31.Holland J. An algorithm for rapid assessment and referral of distressed patientsIn: Perry CM, editor. American Society of Clinical Oncology educational book. Alexandria (VA): ASCO; 2000. pp. 129-138.
- 32.Street RL, Millay B. Analyzing patient participation in medical encounters Health Commun 2001;13(1):61-73. [DOI] [PubMed] [Google Scholar]
- 33.von Friederichs-Fitzwater MM, Gilgun J. Relational control in physician-patient encounters Health Commun 2001;13(1):75-87. [DOI] [PubMed] [Google Scholar]
- 34.Connors AF, Dawson NV, Desbiens NA, Fulkerson JWJ, Goldman L, Knaus WA. A controlled trial to improve care for seriously ill hospitalized patients: the study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA 1995;274(20):1591-1598. [PubMed] [Google Scholar]
- 35.Adams WG, Fuhlbrigge AL, Miller CW, et al. TLC-Asthma: an integrated information system for patient-centered monitoring, case management, and point-of-care decision support. Proceedings of the AMIA Annual Symposium 2003 Nov 8–12; Washington DC. [PMC free article] [PubMed]
- 36.Celler BG, Lovell NH, Basilakis J. Using information technology to improve the management of chronic disease MJA 2003;179:242-246. [DOI] [PubMed] [Google Scholar]
- 37.D'Alessandro D, Dosa N. Empowering children and families with information technology Arch Pediatr Adolesc Med 2001;155:1131-1136. [DOI] [PubMed] [Google Scholar]
- 38.Cherry JC, Moffatt TP, Rodriguez C, Dryden K. Diabetes disease management program for an indigent population empowered by telemedicine technology Diabetes Technol & Ther 2002;4(6):783-791. [DOI] [PubMed] [Google Scholar]
- 39.Selecky C. Integrating technology and interventions in the management of diabetes Dis Manag Health Out 2001;9(Suppl 1):39-52. [Google Scholar]
- 40.Bielli E, Carminati F, La Capra S, Lina M, Brunelli C, Tamburini M. A wireless health outcomes monitoring system (WHOMS): development and field testing with cancer patients using mobile phones BMC Med Inform Dec Making 2004;4(7)Jun 15, www.biomedcentral.com/1472-6947/4/7 . [DOI] [PMC free article] [PubMed]
- 41.Basch E, Artz D, Dulko D, et al. Patient online self-reporting of toxicity symptoms during chemotherapy J Clin Oncol 2005;23(15):3552-3561. [DOI] [PubMed] [Google Scholar]
- 42.Basch E, Iasonos A, Barz A, et al. Long-term toxicity monitoring via electronic patient-reported outcomes in patients receiving chemotherapy J Clin Oncol 2007;25(34):5345-5347Dec 1. [DOI] [PubMed] [Google Scholar]
- 43.DiMatteo M, Lepper H. Promoting adherence to courses of treatment: mutual collaboration in the physician–patient relationshipIn: Jackson LD, Duffy BK, editors. Health communication research: a guide to developments and directions. Westport (CT): Greenwood Press; 1998. pp. 75-86.
- 44.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man N Engl J Med 1976;295(24):1351-1355. [DOI] [PubMed] [Google Scholar]
- 45.Taenzer P, Bultz BD, Carlson LE, et al. Impact of computerized quality of life screening on physician behaviour and patient satisfaction in lung cancer outpatients Psychooncology 2000;9(3):203-213May–Jun. [DOI] [PubMed] [Google Scholar]
- 46.Gustafson DH, Brennan PF, Hawkins RP. Investing in e-Health: what it takes to sustain consumer health informaticsNew York: Springer; 2007.
- 47.Gustafson DH, McTavish FM, Stengle W, et al. Use and impact of eHealth system by low-income women with breast cancer J Health Commun 2005;10(Suppl 1):195-218. [DOI] [PubMed] [Google Scholar]
- 48.Gustafson DH, Hawkins RP, Boberg EW, et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved Int J Med Inf 2002;65(3):169-177. [DOI] [PubMed] [Google Scholar]
- 49.Gustafson DH, McTavish FM, Boberg E, Owens BH, Sherbeck C, Wise M, et al. Empowering patients using computer based health support systems Qual Health Care 1999;8:49-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Snyder C. Paper prototyping: The fast and easy way to refine user interfacesSan Francisco: Morgan Kaufmann; 2003.
- 51.Nielsen J. Usability engineeringCambridge (MA): Academic Press/AP Professional; 1993.
- 52.Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients J Palliat Care 1991;7(2):6-9. [PubMed] [Google Scholar]
- 53.Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status Cancer 1980;45(8):2220-2224. [DOI] [PubMed] [Google Scholar]
- 54.Shaw BR, Han JY, Baker T, et al. How women with breast cancer learn using interactive cancer communication systems Health Educ Res 2007;22(1):108-119. [DOI] [PubMed] [Google Scholar]