Abstract
Context: Although panic disorder is linked to hypertension and smoking, the relationship between panic disorder and coronary artery disease (CAD) is unclear.
Objective: To extend our understanding about the strength of the association between panic disorder and coronary artery disease and known cardiovascular risk factors.
Data sources: Potential studies were identified via a computerized search of MEDLINE and PsycINFO databases and review of bibliographies. MeSH headings used included panic disorder with chest pain, panic disorder with coronary disease or cardiovascular disorders or heart disorders, and panic disorder with cholesterol or essential hypertension or tobacco smoking.
Study selection: The diagnosis of panic disorder in eligible studies was based on DSM-IV criteria, and studies must have used objective criteria for CAD and risk factors. Only case-control and cohort studies were included.
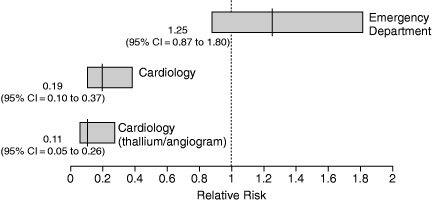
Data Synthesis: Concerning the relationship between panic disorder and CAD, studies conducted in emergency departments found a relative risk [RR] of 1.25 (95% CI = 0.87 to 1.80), while those conducted in cardiology settings found an inverse relationship (RR = 0.19, 95% CI = 0.10 to 0.37). However, there is an inverse relationship between the prevalence of CAD in the study and the RR (r = –.554, p = .097), suggesting that, in primary care settings in which the prevalence of CAD is low, there may be a significant association between panic disorder and CAD.
Conclusion: The association between panic disorder and CAD has several implications for primary care physicians managing patients with chest pain. When comorbid, the panic attacks may cause the patient with coronary disease to seek care but could also provoke a cardiac event. If one condition is recognized, a search for the other may be warranted because of the potential consequences if left undetected. The treatment approach to the panic disorder should be adjusted in the presence of comorbid CAD.
There are several reasons to consider that a relationship between panic disorder and coronary artery disease (CAD) might exist. First, panic disorder has been linked to other forms of cardiac disease. Second, the most likely source of the chest pain during panic attacks is ischemia. Finally, there is evidence that panic disorder may be associated with cardiovascular risk factors, such as hypertension, hyperlipidemia, and smoking.
Panic disorder is associated with several cardiac abnormalities. In addition to patients with panic disorder having elevated standing heart rates,1 10% have an arrhythmia.2 Panic disorder is associated with increased left ventricular mass and diameter,3 and patients with panic disorder have poorer cardiovascular fitness as demonstrated by lower maximum oxygen consumption and decreased exercise tolerance.4 Patients presenting to the emergency department with panic attacks were found to have increased levels of B-type natriuretic peptide.5 Conflicting studies concerning an association with idiopathic cardiomyopathy have been reported.6–8 Case reports have linked panic disorder to a descending aortic aneurysm9 and pulmonary hypertension secondary to an atrial septal defect with pulmonic valve disease.10 However, the strongest association is between panic disorder and mitral valve prolapse (MVP). The panic-MVP relationship has been well documented,11 but MVP is not likely to be the source of chest pain.12 In addition, the significance of the panic-MVP relationship is unclear. Not only does the presence of MVP not alter psychiatric comorbidity13,14 or treatment response,15 but the source of the linkage is also unclear. There is no supporting evidence for a MVP-to-panic sequence as proposed.16 Indirect linkages via autonomic vulnerability or dysfunction have also been proposed.17 However, the most likely explanation is that the decreased left ventricular volume due to the tachycardia seen in panic disorder produces the MVP.18 The observation that the MVP disappears with remission of the panic disorder supports this sequence.19 Thus, panic disorder has been linked to several forms of cardiac disease. In fact, this association is seen in studies from the United States20 and around the world.21 Although a relationship with MVP is probably the most common, an association with CAD would be the most significant.
Whether because of decreased heart rate variability, microvascular angina, or coronary artery disease, ischemia is believed to be the cause of chest pain during panic attacks. Smoller et al.22 found an association between panic attacks and both ischemic and nonischemic chest pain among women undergoing Holter monitoring. In fact, in a large managed care database, an association between diagnoses of panic disorder and coronary heart disease was found even after controlling for covariates (odds ratio = 1.87, 95% CI = 1.80 to 1.91).23 Similarly, women enrolled in the Women's Health Initiative Observational Study demonstrated an association between panic attacks and coronary heart disease (hazard ratio = 4.20, 95% CI = 1.76 to 9.99).24 If this association is true, myocardial ischemia could cause panic attacks via increased catecholamines or cerebral carbon dioxide levels secondary to lactate.25
Finally, a relationship between panic disorder and CAD could exist through a relationship between panic disorder and cardiac risk factors. While Dammen et al.26 reported no association with hypertension, diabetes, obesity, or hyperlipidemia, Bajwa27 reported no association with BMI and Roy-Byrne et al.28 reported no association with hypercholesterolemia. However, most studies have linked panic disorder with cardiac risk factors. In fact, people with panic disorder frequently have a family history of CAD and have a higher number of risk factors than controls.26
Not only would a panic-CAD association lead to serious consequences, but because the respective characteristics of the chest pain do not accurately distinguish between them, panic symptoms could overshadow those typically linked to CAD, obscuring its presence. Although prior reviews have looked at the panic disorder-CAD relationship, none have focused on their association among primary care patients presenting with chest pain. The purpose of this review was to estimate the strength of the association between panic disorder and CAD in primary care settings, attempt to understand possible reasons for an association to exist, and translate that understanding into recommendations for management.
LITERATURE REVIEW
This review extends the results from a systematic review previously reported.29 Briefly, potential studies were identified via a computerized search of MEDLINE and PsycINFO databases, and review of bibliographies. MeSH headings used included panic disorder with chest pain, panic disorder with coronary disease or cardiovascular disorders or heart disorders, and panic disorder with cholesterol or essential hypertension or tobacco smoking. The diagnosis of panic disorder in eligible studies was based on DSM-IV criteria, and studies must have used objective criteria for CAD and risk factors. Only case-control and cohort studies were included. Using the same search and selection strategies, new studies were sought. Although the results of the original systematic review did not change, the synthesis has been extended to include an assessment of the limitations of the literature on which it is based, an estimation of whether there is a panic-CAD association in primary care settings, and suggestions of how these translate into management strategies.
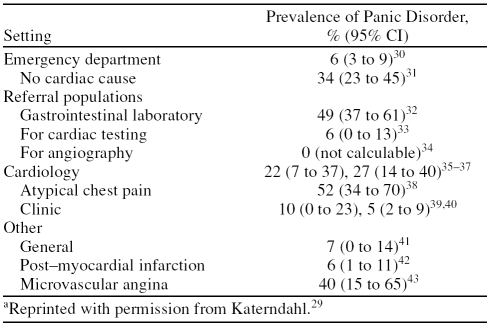
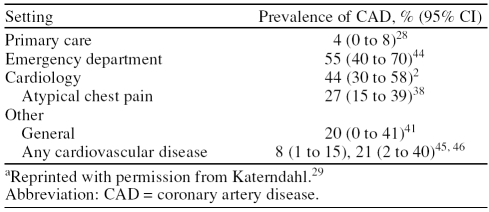
Tables 1 and 2, respectively, show that panic disorder occurs in 0% to 53% of patients with CAD and that CAD occurs in 4% to 55% of patients with panic disorder. Although panic disorder is usually more common in people without CAD than with CAD,33–35,38,41 it is still seen in a significant portion of those with CAD. In fact, Kane et al.32 found more panic disorder in patients with CAD than without it among cardiac patients referred for esophageal motility studies.
Table 1.
Prevalence of Panic Disorder in Patients With Coronary Artery Diseasea
Table 2.
Prevalence of Coronary Artery Disease in Patients With Panic Disordera
LIMITATIONS OF THIS LITERATURE
How reliable and valid is the literature on which this discussion is based? Reliability assessments have shown that the diagnoses of both spontaneous and situational panic attacks have good-to-excellent reliability.47 The validity of the diagnosis of panic disorder in these studies is supported by several sources. First, subjects with panic disorder and noncardiac chest pain have decreased partial pressure of carbon dioxide levels suggestive of the hyperventilation commonly seen in panic disorder.48 In addition, in studies of patients in whom the results of coronary angiograms are normal, the validity of the diagnosis of panic disorder is supported by the clinical description, family studies, lactate and CO2 challenge tests, treatment response, and diagnostic stability in longitudinal studies.49
The concerns expressed by family physicians relate to the research settings and sample characteristics of studies in the literature. Few studies have been conducted in primary care settings. Most of the research has been conducted in emergency medicine, cardiology, and psychiatry settings. Although comparisons between patients with panic disorder in primary care settings versus those in emergency medicine settings have not been done, patients referred to cardiology settings for chest pain often have personality disorders that, in turn, are associated with increased rates of avoidance and suicidality.50 Similarly, comparing patients with chest pain in primary care versus cardiology settings, the prevalence of CAD is considerably higher in cardiology settings even when controlling for the number of cardiac risk factors.51 The use of psychiatric settings is even more problematic. Not only did 22% of primary care patients with panic disorder referred to psychiatrists initially present with chest pain,52 but previous work found that patients who see mental health professionals for panic attacks have more severe disease as measured by symptom severity and health care utilization.53 Finally, although patients with chest pain in emergency medicine versus psychiatry settings do not differ in prevalence of generalized anxiety disorder, major depression, or suicidal ideation, those seeing psychiatrists have higher rates of agoraphobia, social and specific phobias, and posttraumatic stress disorder.54 Thus, the literature may reflect the differences of patients seen in different settings and results may not apply to primary care settings.
ASSOCIATION BETWEEN PANIC DISORDER AND CAD
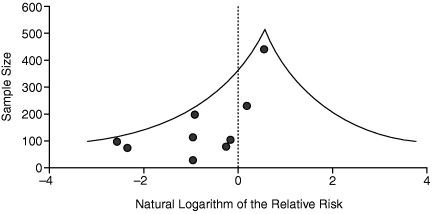
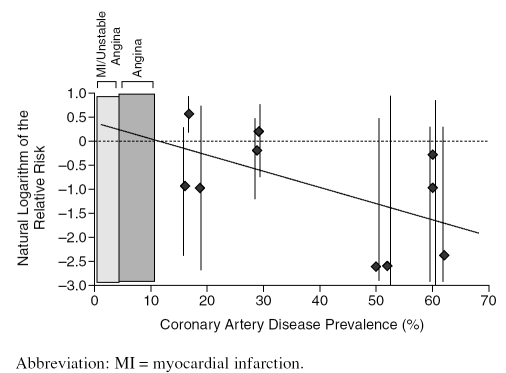
This systematic review failed to document an overall association between panic disorder and CAD (RR = 0.77, 95% CI = 0.56 to 1.05). However, to assess whether publication bias exists, the sample size for each study was plotted against the natural logarithm of the relative risk (LnRR) in a funnel plot (Figure 1).55 In an unbiased literature, studies should be uniformly distributed under the “funnel.” The lack of a right-hand “tail” suggests that the published literature is incomplete, lacking several small studies that would document a positive association between CAD and panic disorder.
Figure 1.
Funnel Plot of Studies on the Panic–Coronary Artery Disease Association
This finding may be due to a relationship between study setting and RR (Figure 2). Although there were insufficient population-based or primary care studies to summarize, studies conducted in emergency departments found an RR of 1.25 (95% CI = 0.87 to 1.80). Because the CI includes 1.0, no significant association between panic disorder and CAD in emergency departments was found. Cardiology-based studies that excluded patients with prior evidence of CAD found an RR of 0.19 (95% CI = 0.10 to 0.37), while limiting studies to those in which the diagnosis of CAD was based on either thallium treadmill tests or angiography produced an RR of 0.11 (95% CI = 0.05 to 0.26). These results suggest an inverse relationship between the presence of panic disorder and CAD, strengthened by the fact that the RR decreases with increasing precision of CAD assessment. However, the selective nature of the samples prevents a strong conclusion about the association between CAD and panic disorder from being made.
Figure 2.
Association Between Coronary Artery Disease and Panic Disorder in Chest Pain
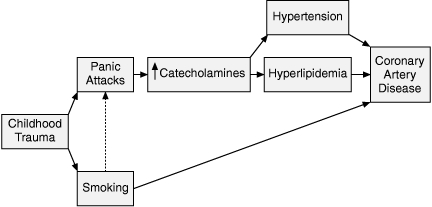
Using all 10 studies conducted in patients with chest pain, there is an inverse relationship between the prevalence of CAD in the study and the RR found in the study (r = –.554, p = .097); thus, the more selective the sample, the lower the detected association (expressed as the LnRR) between panic disorder and CAD (Figure 3). The resulting regression equation is
Figure 3.
Strength of Association Versus Coronary Artery Disease Prevalence
Thus, based on the CAD prevalence in the study with the largest sample size as the best estimate of overall association in that setting,31 the RR in emergency departments should be 1.75. Although previous primary care studies have not looked for a panic-CAD association, the prevalence for CAD in chest pain in primary care settings should be around 2% based on the 1.5% prevalence of unstable coronary artery disease56 and the 2.9% prevalence of myocardial infarction (MI)57 in 2 practice-based network studies. Using a CAD prevalence of 2% for primary care settings and the regression equation above, the expected panic-CAD RR should be 1.26 for primary care. Even the prevalence of angina in primary care populations with chest pain is about 10%,56,58 the crossover point in the graph. These findings suggest that a significant positive association may exist between panic disorder and CAD in both primary care and emergency department settings. This association is consistent with the observation that chest pain patients are diagnosed with psychopathology as a cause more often in primary care than emergency department settings.59
PANIC DISORDER AND CARDIOVASCULAR RISK FACTORS
If there is an association between panic disorder and CAD, could they be linked through a relationship with cardiovascular risk factors? Systematic review found that there were insufficient numbers of homogeneous studies to quantitatively summarize the relationship, but several known cardiac risk factors have been reported present in people with panic disorder.
First, panic disorder is linked to elevations in both systolic and diastolic blood pressures.60,61 Consistent across primary care and cardiology settings, hypertension is associated with both panic disorder2,27,46,52,62,63 and panic attacks.62,64,65 This association may explain why 9% to 32% of patients with chest pain and normal results of coronary angiograms have hypertension.66
Second, panic disorder is associated with lipid abnormalities. Specifically, total cholesterol levels are increased in those with panic disorder.26,67 This association is supported by studies documenting elevated cholesterol levels in 8% to 55% of patients with chest pain and normal coronary angiograms.66 In addition, the presence of panic attacks in patients with chronic obsessive-compulsive disorder was associated with elevated triglyceride and decreased high-density lipoprotein (HDL) levels.68 Conflicting gender differences in lipid patterns have been found. In one study, women with panic disorder frequently have elevated low-density lipoprotein (LDL) levels with decreased HDL levels, while men with panic disorder frequently have elevated triglyceride levels.67 However, Perez-Parada et al.69 found elevated LDL levels in men in response to pentagastrin-induced panic attacks but not in women. But associations between panic disorder and lipid abnormalities are not always found70 and, if found, are primarily seen in psychiatric settings and in studies with small sample sizes, as opposed to large studies conducted in primary care or cardiology settings, which have failed to document an association.
Finally, consistent across community, cardiology, and psychiatry settings, smoking is linked to panic disorder25,71,72 uniquely among anxiety disorders73 and this association is supported by the observation that 32% to 64% of patients with chest pain and coronary angiograms with normal results are smokers.66 The nature of the panic-smoking relationship, however, is unclear.74 Although 19% of patients with panic disorder report that they increased their smoking due to their panic,72 panic attacks are not believed to induce smoking.71 On the other hand, 72% of patients with panic disorder report smoking at the onset of their attacks, while 55% and 26% report having decreased or stopped their smoking, respectively, in response to their panic.72 Daily or continuous smoking is linked to the onset of panic, and the frequency of panic attacks correlates with the amount of smoking.71 On the other hand, panic attacks have also started after acute smoking abstinence.75 Although panic disorder has been linked to chronic obstructive coronary disease,76 and it has been suggested that the smoking-panic association could be secondary to associated lung disease,71 the weakness of this association refutes a causal relationship. Perceptions of health may moderate the smoking-panic association.77
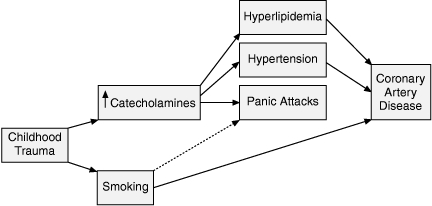
To understand how these risk factors could be related to panic disorder, we must understand how catecholamines are involved. It is unclear whether the elevated levels of catecholamines seen in panic disorder6 are a cause or effect of panic disorder. Elevations in cholesterol may be because of increased catecholamines27 and may explain a correlation between total cholesterol and fear of dying in patients with panic disorder.78 In addition, panic disorder may cause the increased catecholamines, which lead to hypertension and hyperlipidemia via activation of lipoprotein lipase.67 Although childhood trauma is linked to panic disorder79 as well as to smoking and increased catecholamines,80–83 it is only observed in 23% of people with panic disorder. Ultimately, these associations could yield at least 2 possible pathways linking panic disorder and CAD through cardiac risk factors.
Figure 4 presents one of several possible pathways linking panic disorder with CAD through the cardiac risk factors. The key to this pathway is the initial childhood trauma and/or smoking behavior. In this pathway, childhood trauma and possibly smoking trigger the onset of panic attacks that, in turn, increase catecholamines. These high levels of catecholamines produce hypertension and hyperlipidemia. However, this sequence does not account for the observation that the diagnosis of hypertension is usually made prior to the onset of panic attacks.62
Figure 4.
Possible Mechanism Linking Panic Disorder and Coronary Artery Disease (model 1)
An alternative model is presented in Figure 5. In this model, childhood trauma is linked to both smoking and increased catecholamines.81–83 While the increased catecholamines produce hyperlipidemia and hypertension, they and/or the smoking trigger panic attacks as well. In this model, the association between panic disorder and CAD is not causal but rather because of the increased catecholamines that they have in common. Because this pathway requires childhood trauma as the initial step, it could only apply to a portion of those with panic disorder.
Figure 5.
Possible Mechanism Linking Panic Disorder and Coronary Artery Disease (model 2)
IMPLICATIONS
If a panic-CAD association exists in primary care, what would be the implications for health outcomes, evaluation, and management? The comorbidity between CAD and panic disorder could have serious consequences. Not only can diagnosing panic disorder result in failure to recognize CAD, but panic disorder itself is often unrecognized,44,84 leading to increased social disability, medical costs, and disease progression.84 Men with panic disorder have an increased rate of cardiovascular mortality.85 The tachycardia observed during a panic attack could potentially lead to an acute MI in someone with underlying CAD. This may reflect the increased sudden death and fatal cardiovascular disease observed in patients with anxiety in general. In fact, phobic anxiety is a stronger predictor of fatal cardiovascular events than are cardiovascular risk factors such as smoking, systolic blood pressure, and hypercholesterolemia.86
EFFECT ON EVALUATION
Which primary care patients with chest pain and panic disorder should be further evaluated for CAD? The most defensible strategy is to consider working up panic disorder patients who have any cardiac risk factors, particularly males and postmenopausal women. Because patients with both CAD and panic disorder tend to exhibit distress due to the panic attacks,31 the panic attacks may serve a valuable role in convincing the patient with CAD to seek care, alerting the physician to the possibility of CAD. Because MVP can produce an exercise treadmill test (ETT) with false positive results, either perform a thallium ETT on all patients with panic disorder or use the Bruse ETT as a screening test to be followed by a thallium ETT if the results of the Bruce ETT are abnormal. Cardiac workups should not be performed to convince patients that they do not have cardiac disease, because chest pain patients continue to have symptoms and disability after reassurance87 or a coronary angiogram with normal results.88 The disease conviction of patients with panic disorder may explain why only 56% of emergency department patients with chest pain begun on paroxetine therapy for panic are still taking it 1 month later.89
EFFECT ON MANAGEMENT OF CAD AND PANIC DISORDER
Treatment of CAD
CAD and cardiac risk factors must be treated aggressively. Some cardiac treatments may potentially affect panic anxiety and its management. Smoking cessation and exercise can improve both CAD and panic disorder. Although cholesterol reduction is important, statin therapy has rarely been associated with increased anxiety. Similarly, because there is evidence that verapamil90 and clonidine91,92 have some antipanic activity, these drugs may play a specific role in the treatment of hypertension in patients with panic disorder. Although propranolol is recommended post-MI and may reduce panic symptoms93 it has also been linked to exacerbation of panic disorder.94 Finally, the combination of tricyclic antidepressants (TCAs) with nitrates and vasodilators can result in significant orthostatic hypotension95
Treatment of Panic Disorder
Traditionally, panic disorder is treated with either cognitive behavioral therapy (CBT), pharmacotherapy (antidepressants, high-potency benzodiazepines), or both. A recent survey of family physicians found that, of their patients with panic disorder who were not referred to mental health providers, 73% received selective serotonin reup-take inhibitors (SSRIs), 23% received high-potency benzodiazepines, and 18% received CBT.96 Comparison of CBT in primary versus secondary care settings found a more rapid response in primary care settings.97 In fact, previous studies have shown that, after 20 minutes of instruction in the emergency department, exposure therapy decreases depression, avoidance, panic attack frequency, and emergency department visits.98 Thus, CBT may be useful in the management of panic disorder in the presence of CAD.
Pharmacotherapy for panic disorder in CAD patients is more complicated. Although TCAs are effective in panic disorder, their cardiotoxicity precludes them as first-line agents in the presence of CAD. In fact, tricyclic use has been linked to the development of MI.99 In addition, imipramine therapy for panic disorder increases cardiovascular mortality risk secondary to increased blood pressure and heart rate.95
SSRIs and nonselective serotonin reuptake inhibitors (NSRIs) may be appropriate for patients with both panic disorder and CAD, but they may affect cardiac risk factors. Although angina and hypertension are rare side effects of SSRI therapy, studies have shown that SSRIs are safe in patients with ischemic heart disease,100 post-MI patients, and patients with unstable angina.101,102 In patients without cardiac risk factors, SSRI use does not increase the risk of a first MI.103 In fact, SSRI use in patients with known CAD is associated with a reduction in cardiovascular morbidity and mortality.104 In addition, paroxetine use is associated with a reduction in the normal stress-induced rise in blood pressure among CAD patients.105 However, as a group, SSRIs may increase cholesterol levels in patients with panic disorder.106 More specifically, SSRIs may increase total, LDL, and HDL levels from baseline.107 Although sertraline and possibly paroxetine may increase LDL cholesterol,108,109 this effect may be offset by SSRI-linked attenuation of platelet activity and increase in endothelial nitrous oxide, which further inhibits platelet aggregation and produces vasodilatation.110,111 In addition, beta blockers, typically used to treat CAD, have been shown to potentiate SSRI activity.112 Paroxetine can interact with digitalis to increase the risk of toxicity.113 In addition, citalopram may be associated with atrioventricular blocks.114
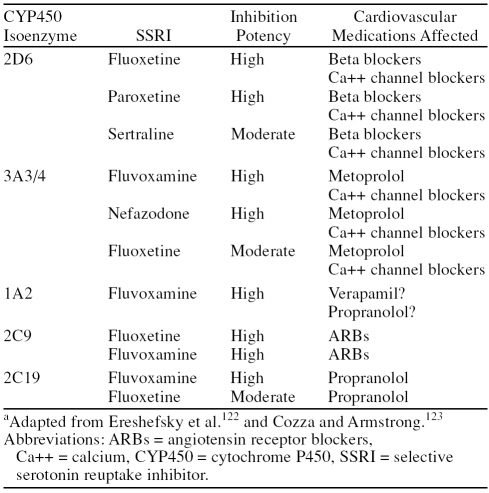
Similarly, NSRIs (venlafaxine, nefazodone, and mirtazapine) can be effective in the treatment of panic disorder. However, high-dose venlafaxine (> 300 mg/day) has been associated with hypertension in 5% of cases;115 doses up to 225 mg can reduce heart rate variability more than paroxetine116 which, in turn, may increase oxygen demand and ischemia,37 and a case of acute ischemia occurring within 1 week of venlafaxine onset has been reported.117 Although generic nefazodone has antipanic activity, and electrocardiogram changes are rare,118 its potential hepatic toxicity limits its use. In addition, nefazodone may increase the risk of rhabdomyolysis in patients on simvastatin therapy.119 Finally, mirtazapine may also be considered. Although there is some evidence that mirtazapine is effective in panic disorder, there are case reports suggesting that, when combined with clonidine,120 mirtazapine can induce hypertension. While no effect of mirtazapine on HDL or LDL has been documented, it may increase total cholesterol secondary to weight gain.121 Finally, the role of antidepressants in the management of panic disorder in patients with CAD may depend on their potential interactions with medications for CAD (beta blockers, angiotensin receptor blockers, and calcium channel blockers) via their cytochrome P450 (CYP450) effects (Table 3). Generally, based on their CYP450 profiles, sertraline, venlafaxine (and presumably duloxetine), citalopram, escitalopram, and mirtazapine are felt to have a good margin of safety.123
Table 3.
Potential Cytochrome P450 Effects Between SSRIs and Cardiovascular Medicationsa
Finally, high-potency benzodiazepines should also be considered. Alprazolam treatment of panic disorder actually decreases total cholesterol124 and catecholamine response to exercise.125 In addition, although alprazolam does not decrease the frequency or severity of anginal attacks in CAD patients taking propranolol, it does decrease symptom severity and reduce nitroglycerin use.126 Other potential cardiovascular benefits of low-dose benzodiazepines include decreased myocardial contractility and increased blood flow.127 In fact, benzodiazepines were found to delay onset of ETT-induced ischemia128 and to reduce MI rate129 in patients with CAD. However, benzodiazepines should generally not be used in elderly patients or those with a history of substance abuse or personality disorders.
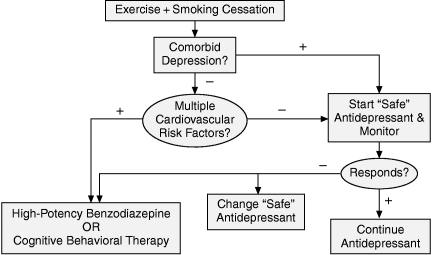
Thus, in the presence of CAD, panic disorder should be treated with an SSRI, a high-potency benzodiazepine, or CBT. Figure 6 presents the treatment algorithm recommended for patients with panic disorder and comorbid CAD. Exercise and smoking cessation are recommended for all patients. If not contraindicated, patients with comorbid depression should be started on an antidepressant therapy with few CYP450 effects (sertraline, venlafaxine, citalopram, escitalopram, mirtazapine). Patients without depression should be treated based on their number of cardiovascular risk factors. Patients with few or no risk factors should be started on citalopram or escitalopram therapy. Patients with multiple cardiac risk factors or an SSRI-exacerbated risk factor are probably best treated initially with a high-potency benzodiazepine or CBT.
Figure 6.
Treatment Algorithm for Panic Disorder in the Presence of Coronary Artery Disease
CONCLUSION
Although both are independent causes of chest pain, panic disorder and coronary artery disease may coexist, particularly in primary care settings. When comorbid, the panic attacks may cause the patient with coronary disease to seek care but could also provoke a cardiac event. Distinguishing between the 2 disorders can be difficult when based on clinical criteria alone. If one condition is recognized, a search for the other is warranted in particular patient subgroups. All patients with comorbid panic disorder and CAD should be treated with exercise and smoking cessation. Treatment with a “safe” antidepressant, high-potency benzodiazepine, or CBT depends on the presence of comorbid depression and cardiovascular risk factors.
Drug names: alprazolam (Xanax, Niravam, and others), citalopram (Celexa and others), duloxetine (Cymbalta), escitalopram (Lexapro and others), fluoxetine (Prozac and others), fluvoxamine (Luvox and others), imipramine (Tofranil and others), metoprolol (Toprol, Lopressor, and others), mirtazapine (Remeron and others), paroxetine (Paxil, Pexeva, and others), propranolol (Innopran, Inderal, and others), sertraline (Zoloft and others), venlafaxine (Effexor and others), verapamil (Verelan, Covera, and others).
Footnotes
Dr. Katerndahl has served on the speakers/advisory boards for AstraZeneca and GlaxoSmithKline.
REFERENCES
- Taylor CB, King R, and Ehlers A. et al. Treadmill exercise test and ambulatory measures in panic attacks. Am J Cardiol. 1987 60:48J–52J. [DOI] [PubMed] [Google Scholar]
- Goldberg R, Morris P, and Christian F. et al. Panic disorder in cardiac out-patients. Psychosomatics. 1990 31:168–173. [DOI] [PubMed] [Google Scholar]
- Kahn JP, Gorman JM, and King DL. et al. Cardiac left ventricular hypertrophy and chamber dilatation in panic disorder patients: implications for idiopathic dilated cardiomyopathy. Psychiatry Res. April1990 32(1):55–61. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, and Santiago H. et al. Effects of heart-rate feedback on estimated cardiovascular fitness in patients with panic disorder. Depress Anxiety. 2000 12:59–66. [DOI] [PubMed] [Google Scholar]
- Vural M, Akbas B, and Acer M. et al. Blood B-type natriuretic peptide level increases in patients who complain shortness of breath and chest pain in the course of panic attack. Int J Cardiol. April2007 117(2):e82–e83. [DOI] [PubMed] [Google Scholar]
- Kahn JP, Drusin RE, Klein DF.. Idiopathic cardiomyopathy and panic disorder. Am J Psychiatry. 1987;144:1327–1330. doi: 10.1176/ajp.144.10.1327. [DOI] [PubMed] [Google Scholar]
- Magni G, Borgherini G, Canton G.. Idiopathic cardiomyopathy and panic disorder in cardiac transplant candidates [letter] Am J Psychiatry. 1988;145:902–903. doi: 10.1176/ajp.145.7.aj1457902. [DOI] [PubMed] [Google Scholar]
- Griez EJL, Mammar N, and Loirat JC. et al. Panic disorder and idiopathic cardiomyopathy. J Psychosom Res. 2000 48:585–587. [DOI] [PubMed] [Google Scholar]
- Benjamin AB, Adityanjee MBBS, Wright J.. Aortic aneurysm in the differential for panic attacks. Psychosomatics. 2000;41:282–283. doi: 10.1176/appi.psy.41.3.282. [DOI] [PubMed] [Google Scholar]
- Sietsema KE, Simon JI, Wasserman K.. Pulmonary hypertension presenting as a panic disorder. Chest. 1987;91:910–912. doi: 10.1378/chest.91.6.910. [DOI] [PubMed] [Google Scholar]
- Katerndahl D.. Panic and prolapse. J Nerv Ment Dis. 1993;1781:539–544. doi: 10.1097/00005053-199309000-00002. [DOI] [PubMed] [Google Scholar]
- Savage DD, Devereuz RB, and Garrison RJ. et al. Mitral valve prolapse in the general population. Am Heart J. 1983 106:577–581. [DOI] [PubMed] [Google Scholar]
- Mavissakalian M, Salerni R, and Thompson ME. et al. Mitral valve prolapse and agoraphobia. Am J Psychiatry. 1983 140:1612–1614. [DOI] [PubMed] [Google Scholar]
- Dager SR, Cowley DS, Dunner DL.. Biological markers in panic states. Biol Psychiatry. 1987;22:339–359. doi: 10.1016/0006-3223(87)90152-1. [DOI] [PubMed] [Google Scholar]
- Grunhaus L, Gloger S, Birmacher B.. Clomipramine treatment for panic attacks in patients with mitral valve prolapse. J Clin Psychiatry. 1984 Jan;45(1):25–27. [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute: Clinical and epidemiological issues in mitral valve prolapse. Proceedings of a National Heart, Lung, and Blood Institute Symposium. Am Heart J. 1987;113:1265–1332. [Google Scholar]
- Klein DF, Gorman JM.. Panic disorders and mitral valve prolapse. J Clin Psychiatry [monograph] 1984;2:14–17. [Google Scholar]
- Ballenger JC, Gibson R, and Peterson GA. et al. “Functional” MVP in agoraphobia/panic disorder. Presented at the 139th annual meeting of the American Psychiatric Association; May 10–16, 1986; Washington, DC. [Google Scholar]
- Gorman JM. Panic disorder; focus on cardiovascular status. Presented at the 139th annual meeting of American Psychiatric Association; May 10–16, 1986; Washington, DC. [Google Scholar]
- Korczak DJ, Goldstein BI, Levitt AJ.. Panic disorder, cardiac diagnosis and emergency department utilization in an epidemiologic community sample. Gen Hosp Psychiatry. 2007;29:335–339. doi: 10.1016/j.genhosppsych.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Ormel J, Von Korff M, and Burger H. et al. Mental disorders among people with heart disease—results from World Mental Health surveys. Gen Hosp Psychiatry. 2007 29:325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoller JW, Pollack MH, and Wassertheil-Smoller S. et al. Panic attacks, daily life ischemia, and chest pain in postmenopausal women. Psychosom Med. 2006 68:824–832. [DOI] [PubMed] [Google Scholar]
- Gomez-Caminero A, Blumenthal WA, and Russo LJ. et al. Does panic disorder increase the risk of coronary heart disease? Psychosom Med. 2005 67:688–691. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Pollack MH, and Wassertheil-Smoller S. et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women's Health Initiative Observational Study. Arch Gen Psychiatry. 2007 64:1153–1160. [DOI] [PubMed] [Google Scholar]
- Gallerani M, Manfredini R, and Mele D. et al. Can panic disorder be considered as an angina equivalent? [letter]. Eur Heart J. 1995 16(12):2013–2014. [DOI] [PubMed] [Google Scholar]
- Dammen T, Arnesen H, and Ekeberg O. et al. Panic disorder in chest pain patients referred for cardiological outpatient investigation. J Intern Med. 1999 245:497–507. [DOI] [PubMed] [Google Scholar]
- Bajwa WK, Asuis GM, and Sanderson WC. et al. High cholesterol levels in patients with panic disorder. Am J Psychiatry. 1992 149:376–378. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Stein MB, and Russo J. et al. Panic disorder in the primary care setting: comorbidity, disability, service utilization, and treatment. J Clin Psychiatry. July1999 60(7):492–499. [DOI] [PubMed] [Google Scholar]
- Katerndahl D.. Panic and plaques: panic disorder & coronary artery disease in patients with chest pain. J Am Board Fam Pract. 2004;17:114–126. doi: 10.3122/jabfm.17.2.114. [DOI] [PubMed] [Google Scholar]
- Yingling KW, Wulsin LR, and Arnold LM. et al. Estimated prevalences of panic disorder and depression among consecutive patients seen in an emergency department with acute chest pain. J Gen Intern Med. 1993 8:231–235. [DOI] [PubMed] [Google Scholar]
- Fleet RP, Dupuis G, and Marchand A. et al. Panic disorder in coronary artery disease patients with noncardiac chest pain. J Psychosom Res. 1998 44:81–90. [DOI] [PubMed] [Google Scholar]
- Kane FJ Jr, Strohlein J, Harper RG.. Noncardiac chest pain in patients with heart disease. South Med J. 1991;84:847–852. doi: 10.1097/00007611-199107000-00007. [DOI] [PubMed] [Google Scholar]
- Cormier LE, Katon W, and Russo J. et al. Chest pain with negative cardiac diagnostic studies. J Nerv Ment Dis. 1988 176:351–358. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE, and Ludbrook PA. et al. Major depression, panic disorder, and mitral valve prolapse in patients who complain of chest pain. Am J Med. 1990 89:757–760. [DOI] [PubMed] [Google Scholar]
- Dammen T, Ekeberg O, and Arnesen H. et al. Detection of panic disorder in chest pain patients. Gen Hosp Psychiatry. 1999 21:323–332. [DOI] [PubMed] [Google Scholar]
- Basha I, Mukerji V, and Langerin P. et al. Atypical angina in patients with coronary artery disease suggest panic disorder. Int J Psychiatry Med. 1989 19:341–346. [DOI] [PubMed] [Google Scholar]
- Fleet R, Lavoie K, Beitman BD.. Is panic disorder associated with coronary artery disease? J Psychosom Res. 2000;48:347–356. doi: 10.1016/s0022-3999(99)00101-4. [DOI] [PubMed] [Google Scholar]
- Beitman BD, Basha I, and Flaker G. et al. Atypical or nonarginal chest pain. Arch Intern Med. 1987 147:1548–1552. [PubMed] [Google Scholar]
- Bass C, Chambers JB, and Kiff P. et al. Panic anxiety and hyperventilation in patients with chest pain. Quart J Med. 1988 69:949–959. [PubMed] [Google Scholar]
- Todaro JF, Shen BJ, and Raffa SD. et al. Prevalence of anxiety disorders in men and women with established coronary heart disease. J Cardiopulm Rehabil Prev. Mar–Apr 2007 27(2):86–91. [DOI] [PubMed] [Google Scholar]
- Katon W, Hall ML, and Russo J. et al. Chest pain: relationship of psychiatric illness to coronary arteriographic results. Am J Med. 1988 84:1–9. [DOI] [PubMed] [Google Scholar]
- Smith MG, Hecker JE.. Prevalence of panic disorder in post-myocardial infarction patients. Int J Rehabil Health. 1997;3(3):197–204. [Google Scholar]
- Roy-Byrne PP, Schmidt P, and Cannon RO. et al. Microvascular angina and panic disorder. Int J Psychiatry Med. 1989 19:315–325. [DOI] [PubMed] [Google Scholar]
- Fleet RP, Dupuis G, and Marchand A. et al. Detecting panic disorder in emergency department chest pain patients. Ann Behav Med. 1997 19:124–131. [DOI] [PubMed] [Google Scholar]
- Carter CS, Maddock RJ, and Amsterdam E. et al. Panic disorder and chest pain in the coronary care unit. Psychosomatics. 1992 33:302–309. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JS, and Ouellette R. et al. Panic disorder and cardiovascular/cerebrovascular problems. Am J Psychiatry. 1990 147:1504–1508. [DOI] [PubMed] [Google Scholar]
- Fyer AJ, Mannuzza S, and Martin LY. et al. Reliability of anxiety assessment. Arch Gen Psychiatry. 1989 46:1102–1110. [DOI] [PubMed] [Google Scholar]
- Maddock RJ, Carter CS, and Tavano-Hall. et al. Hypocapnia associated with cardiac stress scintigraphy in chest pain patients with panic disorder. Psychosom Med. 1998 60:52–55. [DOI] [PubMed] [Google Scholar]
- Beitman BD, Mukerji V, and Kushner M. et al. Validating studies for panic disorder in patients with angiographically normal coronary arteries. Med Clin North Am. September1991 75(5):1143–1155. [DOI] [PubMed] [Google Scholar]
- Dammen T, Ekeberg O, and Arnesen H. et al. Personality profiles in patients referred for chest pain. Psychosomatics. 2000 41:269–276. [DOI] [PubMed] [Google Scholar]
- Sox HC Jr, Hickam DH, and Marton KI. et al. Using the patient's history to estimate the probability of coronary artery disease. Am J Med. 1990 89:7–14. [DOI] [PubMed] [Google Scholar]
- Katon W.. Panic disorder and somatization. Am J Med. 1984;77:101–106. doi: 10.1016/0002-9343(84)90443-1. [DOI] [PubMed] [Google Scholar]
- Katerndahl DA, Realini JP.. Patients with panic attacks seeking care from family physicians compared with those seeking care from psychiatrists [letter] J Nerv Ment Dis. 1998;186:249–250. doi: 10.1097/00005053-199804000-00009. [DOI] [PubMed] [Google Scholar]
- Fleet RP, Marchard A, and Dupuis G. et al. Comparing emergency department and psychiatric setting patients with panic disorder. Psychosomatics. 1998 39:512–518. [DOI] [PubMed] [Google Scholar]
- Ferrer RL.. Graphical methods for detecting bias in meta-analysis. Fam Med. 1998;30(8):579–583. [PubMed] [Google Scholar]
- Klinkman MS, Stevens D, Gorenflo DW.. Episodes of care for chest pain. J Fam Pract. 1994;38:345–352. [PubMed] [Google Scholar]
- Ambulatory Sentinel Practice Network. Exploratory report of chest pain in primary care. J Am Board Fam Pract. 1990;3:143–150. [PubMed] [Google Scholar]
- Kroenke K, Mangelsdorff AD.. Common symptoms in ambulatory care. Am J Med. 1989;86:262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- Buntinx F, Knockaert D, and Bruyninckx R. et al. Chest pain in general practice or in the hospital emergency department. Fam Pract. 2001 18(6):586–589. [DOI] [PubMed] [Google Scholar]
- Bystritsky A, Maidenberg E, and Craske MG. et al. Laboratory psychophysiological assessment and imagery exposure in panic disorder patients. Depress Anxiety. 2000 12:102–108. [DOI] [PubMed] [Google Scholar]
- Katon WJ.. Chest pain, cardiac disease, and panic disorder. J Clin Psychiatry. 1990 May;51(5, suppl):27–30. [PubMed] [Google Scholar]
- Davies SJC, Ghahramani P, and Jackson PR. et al. Association of panic disorder and panic attacks with hypertension. Am J Med. 1999 107:310–316. [DOI] [PubMed] [Google Scholar]
- Noyes R Jr, Claney J, and Hoenk PR. et al. Prognosis of anxiety neurosis. Arch Gen Psychiatry. 1980 37:173–178. [DOI] [PubMed] [Google Scholar]
- Katerndahl D, Trammell C.. Prevalence and recognition of panic states in STARNET patients presenting with chest pain. J Fam Pract. 1997;45:54–63. [PubMed] [Google Scholar]
- Goodwin RD, Hamilton SP.. Panic attack as a marker of core psychopathological processes. Psychopathology. 2001;34:278–288. doi: 10.1159/000049326. [DOI] [PubMed] [Google Scholar]
- Chambers J, Bass C.. Chest pain with normal coronary anatomy. Prog Cardiovasc Dis. 1990;33:161–184. doi: 10.1016/0033-0620(90)90007-o. [DOI] [PubMed] [Google Scholar]
- Hayward C, Taylor CB, and Roth WT. et al. Plasma lipid levels in patients with panic disorder or agoraphobia. Am J Psychiatry. 1989 146:917–919. [DOI] [PubMed] [Google Scholar]
- Agargun MY, Dulger H, and Inci R. et al. Serum lipid concentrations in obsessive-compulsive disorder patients with and without panic attacks. Can J Psychiatry. 2004 49(11):776–778. [DOI] [PubMed] [Google Scholar]
- Perez-Parada J, Jhangri GS, and Lara N. et al. Delayed increase in LDL cholesterol following pentagastrin-induced panic attacks. Psychopharmacology. 2007 193:333–340. [DOI] [PubMed] [Google Scholar]
- Kim EJ, Yu BH.. Increased cholesterol levels after paroxetine treatment in patients with panic disorder. J Clin Psychopharmacol. 2005 Dec;25(6):597–599. doi: 10.1097/01.jcp.0000186868.67418.f5. [DOI] [PubMed] [Google Scholar]
- Breslau N, Klein DF.. Smoking and panic attacks. Arch Gen Psychiatry. 1999;56:1141–1147. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- Amering M, Bankier B, and Berger P. et al. Panic disorder and cigarette snaking behavior. Compr Psychiatry. 1999 40:35–38. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Lewisohn PM, Seeley JR.. Cigarette smoking and panic attacks among young adults in the community. Biol Psychiatry. 2005;58:686–693. doi: 10.1016/j.biopsych.2005.04.042. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, and Schmidt NB. et al. Developmental course(s) of lifetime cigarette use and panic attack comorbidity: an equifinal phenomenon? Behav Modif. January2007 31(1):117–135. [DOI] [PubMed] [Google Scholar]
- Vessicchio JC, Termine A, George TP.. Smoking cessation and panic attacks: a report of 2 cases. J Clin Psychiatry. 2002 Jul;63(7):594–595. doi: 10.4088/jcp.v63n0710b. [DOI] [PubMed] [Google Scholar]
- Pollack MH, Kradin R, and Otto MW. et al. Prevalence of panic in patients referred for pulmonary function testing at a major medical center. Am J Psychiatry. 1996 153(1):110–113. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, and Bonn-Miller MO. et al. Perceived health moderates the association between smoking rate and panic vulnerability variables among daily smokers. Depress Anxiety. 2006 23:257–265. [DOI] [PubMed] [Google Scholar]
- Shioiri T, Fujii K, and Someya T. et al. Effects of pharmacotherapy on serum cholesterol levels in patients with panic disorder. Acta Psychiatr Scand. 1996 93:164–167. [DOI] [PubMed] [Google Scholar]
- Safren SA, Gershuny BS, and Marzol P. et al. History of childhood abuse in panic disorder, social phobia, and generalized anxiety disorder. J Nerv Ment Dis. 2002 190:453–456. [DOI] [PubMed] [Google Scholar]
- Anda RF, Croft JB, and Felitti VJ. et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999 282:1652–1658. [DOI] [PubMed] [Google Scholar]
- De Von Figueroa-Moseley C, Landrine H, Klonoff EA.. Sexual abuse and smoking among college student women. Addict Behav. 2004;29:245–251. doi: 10.1016/j.addbeh.2003.07.004. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Lefter L, and Trickett PK. et al. Urinary catecholamine excretion in sexually abused girls. J Am Acad Child Adolesc Psychiatry. Mar–Apr 1994 33(3):320–327. [DOI] [PubMed] [Google Scholar]
- Lemieuz AM, Coe CL.. Abuse-related posttraumatic stress disorder: evidence for chronic neuroendocrine activation in women. Psychosom Med. 1995;57(2):105–115. doi: 10.1097/00006842-199503000-00002. [DOI] [PubMed] [Google Scholar]
- Fleet RP, Dupuis G, and Marchand A. et al. Panic disorder, chest pain and coronary artery disease. Can J Cardiol. 1994 10:827–834. [PubMed] [Google Scholar]
- Coryell W, Noyes R, Clancy J.. Excess mortality in panic disorder: a comparison with primary unipolar depression. Arch Gen Psychiatry. 1982 Jun;39(6):701–703. doi: 10.1001/archpsyc.1982.04290060051010. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Sparrow D, and Vokonas PS. et al. Symptoms of anxiety and risk of coronary heart disease. Circulation. 1994 90:2225–2229. [DOI] [PubMed] [Google Scholar]
- Goodacre S, Mason S, and Arnold J. et al. Psychologic morbidity and health-related quality of life of patients assessed in a chest pain observation unit. Ann Emerg Med. 2001 38:369–376. [DOI] [PubMed] [Google Scholar]
- Kane FJ Jr, Harper RG, Wittels E.. Angina as a symptom of psychiatric illness. South Med J. 1988;81:1412–1416. doi: 10.1097/00007611-198811000-00018. [DOI] [PubMed] [Google Scholar]
- Wulsin L, Liu T, and Storrow A. et al. Randomized, controlled trial of panic disorder treatment initiation in an emergency department chest pain center. Ann Emerg Med. 2002 39:139–143. [DOI] [PubMed] [Google Scholar]
- Klein E, Uhde TW.. Controlled study of verapamil for treatment of panic disorder. Am J Psychiatry. 1988;145:431–434. doi: 10.1176/ajp.145.4.431. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR, Fyer AJ, and McGrath P. et al. Clonidine treatment of panic disorder. Psychopharmacol Bull. 1981 17(3):122–123.7232641 [Google Scholar]
- Uhde TW, Stein MB, and Vittone BJ. et al. Behavioral and physiologic effects of short-term and long-term administration of clonidine in panic disorder. Arch Gen Psychiatry. 1989 46:170–177. [DOI] [PubMed] [Google Scholar]
- Kathol R, Noyes R, and Slyman D. et al. Propranolol in chronic anxiety disorders. Arch Gen Psychiatry. 1980 37:1361–1365. [DOI] [PubMed] [Google Scholar]
- Levinson DF, Acquaviva J.. Exacerbation of panic disorder during propranolol therapy. J Clin Psychopharmacol. 1988;8(3):193–195. [PubMed] [Google Scholar]
- Taylor CB, Hayward C. Cardiovascular considerations in selection of antipanic pharmacotherapy. J Psychiatr Res. 1990 24suppl 2. 43–49. [DOI] [PubMed] [Google Scholar]
- Katerndahl D, Ferrer RL.. Knowledge about recommended treatment and management of major depressive disorder, panic disorder, and generalized anxiety disorder among family physicians. Prim Care Companion J Clin Psychiatry. 2004;6(4):147–151. doi: 10.4088/pcc.v06n0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortune L, Gracey D, Burke M.. Effect of service setting on treatment outcome: a comparison between cognitive behavioural approaches within primary and secondary care. J Ment Health. 2005;14(5):483–498. [Google Scholar]
- Swinson RP, Soulios C, and Cox BJ. et al. Brief treatment of emergency room patients with panic attacks. Am J Psychiatry. 1992 149:944–946. [DOI] [PubMed] [Google Scholar]
- Cohen HW, Gibson G, Alderman MH.. Excess risk of myocardial infarction in patients treated with antidepressant medications. Am J Med. 2000;108:2–8. doi: 10.1016/s0002-9343(99)00301-0. [DOI] [PubMed] [Google Scholar]
- Shader RI, Greenblatt DJ.. Selective serotonin reuptake inhibitor antidepressants: cardiovascular complications—sorting through findings. J Clin Psychopharmacol. 2001 Oct;21(5):467–468. doi: 10.1097/00004714-200110000-00001. [DOI] [PubMed] [Google Scholar]
- Strik JJ, Honig A, and Lousberg R. et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction. Psychosom Med. 2000 62:783–789. [DOI] [PubMed] [Google Scholar]
- Glassman AH, O'Connor CM, and Califf RM. et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002 288:701–709. [DOI] [PubMed] [Google Scholar]
- Meier CR, Schlienger RG, Jick H.. Use of selective serotonin reuptake inhibitors and risk of developing first-time acute myocardial infarction. Br J Clin Pharmacol. 2001;52:179–184. doi: 10.1046/j.0306-5251.2001.01426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CB, Youngblood ME, and Catallier D. et al. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005 62(7):792–798. [DOI] [PubMed] [Google Scholar]
- Golding M, Kotlyar M, and Carson SW. et al. Effects of paroxetine on cardiovascular response to mental stress in subjects with a history of coronary artery disease and no psychiatric diagnoses. Psychopharmacology. 2005 182(3):321–326. [DOI] [PubMed] [Google Scholar]
- Herran A, Ramirez ML, and Carrera M. et al. Panic disorder, treatment with selective serotonin reuptake inhibitors, and cholesterol levels. J Clin Psychopharmacol. 2006 26(5):538–540. [DOI] [PubMed] [Google Scholar]
- Ginsberg DL.. SSRI-induced hypercholesterolemia in panic disorder patients [Psychopharmacology Reviews] Prim Psychiatry. 2003;10(12):19. [Google Scholar]
- Bailey DL, LeMelledo JM.. Effects of selective serotonin reuptake inhibitors on cholesterol levels in patients with panic disorder [letter] J Clin Psychopharmacol. 2003;23(3):317–319. doi: 10.1097/00004714-200306000-00016. [DOI] [PubMed] [Google Scholar]
- Lara N, Baker GB, and Archer SL. et al. Increased cholesterol levels during paroxetine administration in healthy men. J Clin Psychiatry. December2003 64(12):1455–1459. [DOI] [PubMed] [Google Scholar]
- Le Melledo JM, Bailey D, Baker GB.. Selective serotonin reuptake inhibitors and myocardial infarction [letter] Circulation. 2004 Jan;109(3):E19. doi: 10.1161/01.CIR.0000113707.06004.3B. [DOI] [PubMed] [Google Scholar]
- Chrapko W, Jurasz P, and Radomski MW. et al. Alteration of decreased plasma NO metabolites and platelet NO synthase activity by paroxetine in depressed patients. Neuropsychopharmacology. 2006 31(6):1286–1293. [DOI] [PubMed] [Google Scholar]
- Hirschmann S, Dannon PN, and Ianco J. et al. Pindolol augmentation in patients with treatment-resistant panic disorder. J Clin Psychopharmacol. 2000 20:556–559. [DOI] [PubMed] [Google Scholar]
- Ginsberg DL.. Paroxetine coadministration results in digitalis intoxication [Psychopharmacology Reviews] Prim Psychiatry. 2006;13(8):29–30. [Google Scholar]
- Gambassi G, Incalzi RA, Gemma A.. Atrioventricular blocks associated with citalopram [letter] Am J Geriatr Psychiatry. 2005;13(10):918–919. doi: 10.1176/appi.ajgp.13.10.918. [DOI] [PubMed] [Google Scholar]
- Thase ME.. Effects of venlafaxine on blood pressure: a meta-analysis of original data from 3744 depressed patients. J Clin Psychiatry. 1998 Oct;59(10):502–508. doi: 10.4088/jcp.v59n1002. [DOI] [PubMed] [Google Scholar]
- Davidson J, Watkins L, and Owens M. et al. Effects of paroxetine and venlafaxine on heart rate variability in depression. J Clin Psychopharmacol. 2005 25:480–484. [DOI] [PubMed] [Google Scholar]
- Reznik I, Rosen Y, Rosen B.. Acute ischaemic event associated with the use of venlafaxine. J Psychopharmacol. 1999;13:193–195. doi: 10.1177/026988119901300212. [DOI] [PubMed] [Google Scholar]
- Stoudemire A.. New antidepressant drugs and the treatment of depression in the medically ill patient. Psychiatr Clin North Am. 1996 Sep;19(3):495–514. doi: 10.1016/s0193-953x(05)70303-8. [DOI] [PubMed] [Google Scholar]
- Karnik NS, Maldonado JR.. Antidepressant and statin interactions: a review and case report of simvastatin and nefazodone-induced rhabdomyolysis and transaminitis [letter] Psychosomatics. 2005 Nov–Dec;46(6):565–568. doi: 10.1176/appi.psy.46.6.565. [DOI] [PubMed] [Google Scholar]
- Abo-Zena RA, Bobek MB, Dweik RA.. Hypertensive urgency induced by an interaction of mirtazapine and clonidine. Pharmacotherapy. 2000;20:476–478. doi: 10.1592/phco.20.5.476.35061. [DOI] [PubMed] [Google Scholar]
- Nicholas LM, Ford AL, and Esposito SM. et al. The effects of mirtazapine on plasma lipid profiles in healthy subjects. J Clin Psychiatry. August2003 64(8):883–889. [DOI] [PubMed] [Google Scholar]
- Ereshefsky L, Riesenman C, and Lam YW. Serotonin selective reuptake inhibitor drug interactions and the cytochrome P450 system. J Clin Psychiatry. 1996 57suppl 8. 17–25. [PubMed] [Google Scholar]
- Cozza KL, Armstrong SC. Cytochrome P450 System. Washington, DC: American Psychiatric Publications. 2001 [Google Scholar]
- Shioiri T, Fujii K, and Someya T. et al. Serum cholesterol levels and panic symptoms in patients with panic disorder. J Affect Disord. 2000 58:167–170. [DOI] [PubMed] [Google Scholar]
- Stratton JR, Halter JB.. Effect of a benzodiazepine (alprazolam) on plasma epinephrine and norepinephrine levels during exercise stress. Am J Cardiol. 1985;56:136–139. doi: 10.1016/0002-9149(85)90582-x. [DOI] [PubMed] [Google Scholar]
- Mendels J, Chernoff RW, Blatt M.. Alprazolam as an adjunct to propranolol in anxious outpatients with stable angina pectoris. J Clin Psychiatry. 1986 Jan;47(1):8–11. [PubMed] [Google Scholar]
- Zeegers A, Van Wilgenburg H, Leeuwin RS.. Cardiac effects of benzodiazepine agonists and antagonists in the isolated rat heart. Life Sci. 1998;63:1439–1456. doi: 10.1016/s0024-3205(98)00411-1. [DOI] [PubMed] [Google Scholar]
- Rossetti E, Fragasso G, and Xuereb RG. et al. Anti-ischemic effects of intravenous diazepam in patients with coronary artery disease. J Cardiovasc Pharmacol. 1994 24:55–58. [DOI] [PubMed] [Google Scholar]
- Wheatley D.. The value of anti-anxiety drugs in the management of cardiac disease. Acta Med Scand Suppl. 1982;660:219–230. doi: 10.1111/j.0954-6820.1982.tb00377.x. [DOI] [PubMed] [Google Scholar]