Abstract
Introduction
This study explores the extent to which consumers seek wellness care when choosing chiropractors whose practice methods are known to include periodic evaluative and interventional methods to maintain wellness and prevent illness.
Methods
Using an international convenience sample of Sacro-Occipital Technique (SOT) practitioners, 1316 consecutive patients attending 27 different chiropractic clinics in the USA, Europe and Australia completed a one-page survey on intake to assess reason for seeking care. A forced choice response was obtained characterizing the patient’s reason for seeking chiropractic care.
Results
More than 40% of chiropractic patient visits were initiated for the purposes of health enhancement and/or disease prevention.
Conclusion
Although prudence dictates great caution when generalizing from this study, if confirmed by subsequent research among other similar cohorts, the present results may lend support to continued arguments of consumer demand for a more comprehensive paradigm of chiropractic care, beyond routine musculoskeletal complaints, that conceptualizes the systemic, nonspecific effects of the chiropractic encounter in much broader terms.
Keywords: chiropractic, wellness, care
Abstract
Introduction
cette étude explore la mesure dans laquelle les consommateurs recherchent le bien-être lorsqu’ils choisissent un chiropraticien qui adopte des méthodes périodiques d’intervention et d’évaluation afin de maintenir le bien-être des patients et de prévenir les maladies.
Méthodes
à l’aide d’un échantillon international à l’aveuglette de chiropraticiens utilisant la technique sacro-occipitale, 1 316 patients consécutifs répartis dans 27 cliniques chiropratiques différentes aux États-Unis, en Europe et en Australie ont répondu à un sondage d’une page visant à déterminer la raison pour laquelle les patients visitent les chiropraticiens. Le patient devait indiquer le motif de sa visite à partir d’un choix de réponses.
Résultats
plus de 40 % des patients ont répondu que leur visite chez le chiropraticien avait pour objet d’améliorer leur santé ou de prévenir les maladies.
Conclusion
bien que la prudence s’impose lors de la généralisation pour cette étude, des recherches plus approfondies auprès de cohortes semblables pourraient confirmer ces résultats, donnant ainsi de bons arguments aux consommateurs qui exigent un paradigme plus détaillé des soins chiropratiques, au-delà des plaintes musculosquelettiques habituelles qui conceptualisent les conséquences systémiques et non spécifiques du rendez-vous chiropratique en termes beaucoup plus approfondis.
Introduction
In the emerging health care arena, the topic of wellness care has generated considerable interest. Consumers are seeking, alongside of conventional medical options, improved ways to prevent the onset of chronic diseases and even the common effects of aging by increasing their use of complementary and alternative (CAM) approaches to promoting health and preventing illness.1,2
With regard to non-allopathic services, chiropractic is among the most commonly used modality.3–5 Although prevalence estimates vary, it has been suggested that each year in the U.S. there may be more total visits to CAM providers (including homeopaths, acupuncturists, and chiropractors) than to more traditional primary care physicians.2 Moreover, CAM use is predicted to rise with increasing third party reimbursement and managed care coverage.5,6 Research focused on patient motivations for seeking CAM suggest that this trend is not primarily rooted in patient dissatisfaction with conventional care but, instead, rests on more complex considerations including a “philosophical congruence” with alternative practitioners emphasizing a holistic approach to wellness.5–7 Indeed, the growing popularity of wellness care has been described as a fundamental change in the “healthcare paradigm”8 that may reflect a “tipping point”9 in the evolution from a purely biomedical to a more holistic, biopsychosocial perspective10 that is reverberating throughout the healthcare system, affecting both allopathic as well as complementary and alternative (CAM) providers.3
Recently, chiropractic has expanded its longstanding spinal wellness emphasis by disseminating a widely adopted Model Course for Public Health Education in Chiropractic Colleges12 as well as specifying health promotion and wellness as key chiropractic competencies.13 In support of these developments, Hawk and colleagues3,4 have advocated promoting “wellness concepts” in chiropractic student training, emphasizing national health targets (such as those found in Healthy People 201014) and evidence-based-practices for health promotion and disease prevention.3,4
The recent formal inclusion of public health preventive measures within the scope of chiropractic practice has raised concerns about chiropractic’s evolving public identity and the potential public acceptance of chiropractors as wellness providers. For instance, the World Federation of Chiropractic’s Identity Consultation Task Force, in its 2005 final report,15 emphasized the urgent need for a clear public identity in chiropractic. Indeed, in terms of public perception, chiropractic has long been synonymous with spinal manipulation and is characterized as “manual healing” (not “alternative systems”) in NC-CAM’s taxonomy.3 Without a better understanding of the public’s willingness to seek out wellness care from chiropractic providers, the preparation of chiropractors as wellness providers may be a case of the cart leading the horse.
The World Federation of Chiropractic’s “Consultation on Identity” found that only 6% of patients seek wellness care from chiropractic providers.16 However, the fact that a minority of patients currently seek wellness care from chiropractic providers may have more to do with consumers’ current understanding of actual chiropractors’ scope of practice than with the acceptability of chiropractors as wellness practitioners. Indeed, practicing chiropractors currently differ substantially on whether they provide one therapeutic modality or a “complete system of healing.”3
Accordingly, as a first step effort, the present study explored the extent to which consumers seek wellness care when the provider is known to offer complementary approaches beyond standard manipulation to alleviate patient symptoms and enhance patient feelings of wellness.18 Based on studies indicating that patients seek chiropractic care primarily for musculoskeletal complaints such as neck and low back pain,17 the present study examined wellness preferences of patients visiting an international convenience sample of Sacro-Occipital Technique (SOT) practitioners utilizing a broad palate of holistic methods.
Methods
This study was granted approval by the Institutional Review Board of Cleveland Chiropractic College. A convenience sample of 27 SOT doctors, practicing in Europe, Australia and the United States, were recruited to participate in a survey of their patients (See Appendix). The questionnaires were handed out to consecutive patients, which included both new and returning patients. No patients filled out the form more then once. The surveys were written in English and patients who participated were English speaking. The data were collected over a 9-month period beginning in October, 2004.
After arriving for the scheduled visit but before being seen by the chiropractor, patients were given the opportunity to voluntarily participate in a chiropractic research study by completing a brief 3-item questionnaire asking their age, gender and motivation for seeking chiropractic care. The survey form did not request or contain any information that could later identify individual patients. Regarding motivation for seeking care, patients were asked to circle one of a possible five options that best reflected their reason for coming to the chiropractic office on that day. The five options, in simple multiple choice, were based on the model developed by Greene & Kreuter.18 While this model appears to have good face and content validity, it has not been translated into a testing instrument and therefore has not be subjected to reliability and validity studies. Using Greene and Krueter’s definitions, each response choice reflects a different health care motivation including wellness (defined as optimizing health among the self-identified healthy), preventive health (defined as preventing illness among the self-identified healthy), at risk (defined as preventing illness among the currently healthy who are at heightened risk to develop a specific condition), sick role (defined as getting well among those self-perceived as ill with an emphasis on therapist-directed treatment), and self care (defined as getting well among those self-perceived as ill favoring the use of self vs. therapist directed strategies). The Greene and Kreuter model was preliminarily developed to elevate awareness of various patient preferences and facilitate improved health promotion messaging and practices through practitioner identification of various states of wellness behavior that may be encountered in the clinical setting.
Completed questionnaires from volunteer patients were collected and numbered sequentially by office staff (starting with 001 for the first patient at each site) and these de-identified forms were returned to the first author. The de-identified data were entered into the Statistical Package for the Social Sciences for Windows, version 12.0 (SPSS Inc, Chicago, Ill), with a 10% check to ensure data entry accuracy.
Data Analyses and Results
Descriptive statistics were used to summarize the demographic characteristics and geographic distribution of the sample and patient responses to the questionnaire. SOT practitioners from three geographic locations (14 from the United States contributing data from 565 patients, 9 from Australia contributing data from 469 patients, and 4 from Europe contributing data from 282 patients) participated in providing data for this study (Table 1). A total of 1316 patients responded to the questionnaire. Although no quantitative data on the number who refused to participate in the anonymous questionnaire were collected, qualitatively, none of the participating chiropractors or their office staffs reported any significant issues related to patients refusing to complete the questionnaire. Patient respondents were predominantly female (n = 837, 64%) with the majority of patients ranging in age from between 30 and 65.
Table 1.
Frequency Distribution of Subject Characteristics and Motivation for Seeking Chiropractic Care
| Frequency (%) n = 1316 | |
|---|---|
| Location | |
| Europe | 282 (21.4) |
| Australia | 469 (35.6) |
| United States | 565 (42.9) |
| Sex | |
| Male | 479 (36.4) |
| Female | 837 (63.6) |
| Age | |
| 30–41 | 318 (24.2) |
| 42–53 | 360 (27.4) |
| 54–65 | 331 (25.2) |
| 66–77 | 110 (8.4) |
| 78 plus | 29 (2.2) |
| Missing | 168 (12.8) |
| Patient Healthcare Motivations for Seeking Chiropractic Care | |
| Wellness | 184 (14.0) |
| Prevention | 163 (12.4) |
| At Risk | 207 (15.7) |
| Sick Role | 227 (17.2) |
| Self Care | 535 (40.7) |
Descriptive statistics demonstrated that 42.1% percent of patients (554 in the “Wellness,” “Prevention” and “At Risk” categories combined out of a total of 1316) in this convenience sample reported seeking chiropractic care without a specific focused complaint. These patients presented either for wellness, prevention, or to reduce their risk of illness or injury, compared to 41% presenting for self-care, and only 17% seeking illness care (sick role) (Table 1).
Differences in the motivation for seeking chiropractic care were assessed by age, gender and region in which the care was received using Chi-Square (a non-parametric test of statistical significance for categorical data). Chi-Square analysis of the comparison of health care motivations by region (Table 2) revealed that, overall, Europeans were more likely than Australians and Americans to report that their chiropractic visits were based upon a desire for care due to illness or “sick role” motivation (27.3%, 14.5%, and 14.5%, respectively, p < .001). Moreover, compared to Americans, Europeans and Australians were more likely to be motivated by “at risk” considerations (11.5%, 20.9%, and 17.7 respectively, Pearson Chi-Square Test = 49.7, p < .001).
Table 2.
Patient Motivations for Seeking Chiropractic Care by Subject Characteristics
| Wellness n (%) | Prevent n (%) | At Risk n (%) | Sick Role n (%) | Self Care n (%) | Pearson Chi-Square | |
|---|---|---|---|---|---|---|
|
Site Europe Australia United States |
23 (8.2)
71 (15.1) 90 (15.9) |
28 (9.9)
59 (12.6) 76 (13.5) |
59 (20.9)
83 (17.7) 65 (11.5) |
77 (27.3)
68 (14.5) 82 (14.5) |
95 (33.7)
188 (40.1) 252 (44.6) |
49.7** |
|
Gender Male Female |
65 (13.6)
119 (14.2) |
58 (12.1)
105 (12.5) |
86 (18.0)
121 (14.5) |
97 (20.3)
130 (15.5) |
173 (36.1)
362 (43.2) |
10.3* |
|
Age At or below 65 years of age Older than 65 years of age |
128 (12.7)
31 (22.3) |
130 (12.9)
16 (11.5) |
153 (15.2)
20 (14.4) |
163 (16.2)
28 (20.1) |
433 (43.0)
44 (31.7) |
13.3* |
*p < 0.05;
**p < 0.001.
Chi-Square analysis of responses by gender (Table 2) revealed a statistically significant difference between male and female health-seeking behaviors (Pearson Chi-Square Test = 10.3, p < 0.5), with males exhibiting a greater tendency to seek “at risk” and “sick role” care than females (18.0% and 20.3% versus 14.5% and 15.5%, respectively), who were more prone to seek ”self-care” than their male counterparts (43.2% versus 36.1%, respectively).
Examination of the relationship between self-reported age and the reason for seeking chiropractic care (Table 2) revealed that younger patients (i.e., 65 or below) reported being more likely to report that they were presenting for “self care” compared to the older patients (ages 66 and older) whose motivations tended to be more equally distributed between “wellness,” “prevention,” “at risk,” “sick role” and “self-care” (Pearson Chi-Square Test = 13.3, P < 0.05).
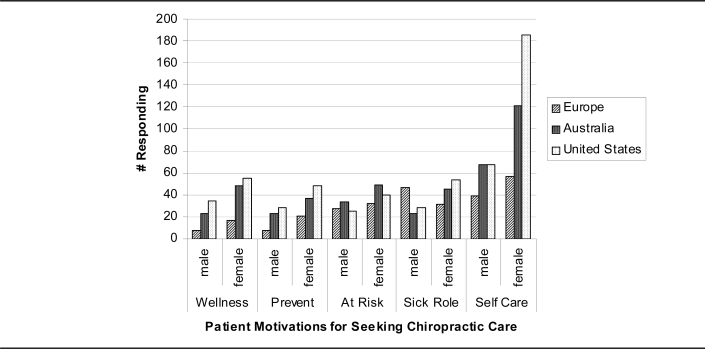
To examine health motivations by geographic care location, gender, and age together, a series of stratified Chi Square analyses was performed. As shown in Figure 1, the first analysis of health motivations stratified by gender and geographic region yielded a significant difference only for Europe (Pearson Chi-Square = 13.9, p = 0.008), with European women reporting greater interest in “preventive” care than Australian or U.S. women (75% vs. 61% and 63.2%, respectively) and European men being more likely to favor “sick role” care (59.7%) than Australian or U.S. men (33.8% and 34.1%, respectively).
Figure 1.
Patient Motivations for Seeking Chiropractic Care as a Function of Gender and Care Location
In the next analysis, the responses to the chiropractic care motivation items were assessed by stratifying on both age and gender. Consistent with results of the other gender analyses, differences emerged between males and females, especially for patients between the ages of 30 and 41 years (Pearson chi-square = 13.7, p = 0.008). Again females demonstrated a somewhat greater interest in “wellness,” “preventive,” and “self” care than males.
Discussion
Using an international convenience sample, this study attempted to identify patients’ specific wellness preferences when seeking chiropractic care from a cohort of chiropractors where wellness care is affirmatively promoted. Findings indicate, overall, more than 40% of patients seeking care reported doing so for the purpose of “optimizing health” or “preventing illness” (including the prevention and/or early intervention of potential risk factors). These findings differ from a previous World Federation of Chiropractic survey, which indicated less than 5–10% of patients seeking care for non-musculoskeletal conditions. Indeed, the rates of patient-initiated wellness visits in this convenience sample of wellness promoting chiropractors is notable when compared to previous estimates indicating lower consumer demand for chiropractic wellness care.16,17 One obvious explanation for the outcomes may be related to these patients’ awareness that their chiropractors actually offer care other than solely for pain reduction for musculoskeletal conditions such as low back pain. Sacro-Occipital Technique practitioners are trained to utilize a system of complex diagnostic and treatment procedures focused upon systemic as well as neuromusculosketal complaints. SOT practitioners educate patients on the value of periodic (1–2 times per year) examination/wellness check-ups to assess patient’s overall/systemic health status by evaluating the spine and nervous system through various mechanical and reflex techniques. Treatment recommendations are then individualized based upon the findings and typically involve short-term, outcome-based interventions supported by modification in patient lifestyles, diet, exercise, nutrition, and other modifying behavioral and psychosocial factors. Furthermore, the SOT model of care does not advocate the unethical use of long-term, pre-paid maintenance treatment programs developed outside of the normative parameters of clinical indicators. While the authors clearly believe that the frequency of maintenance/supportive care should ethically be left strictly to individual patient preferences, this tendentious aspect of chiropractic preventive care is clearly beyond the focus of this paper.
Based on the public’s (and their chiropractors’) current perceptions of chiropractic as primarily an NMS specialty,19,16 the typical consumer responding to prior surveys may not have been aware of the possibility that preventive/wellness care is a chiropractic option and therefore would have been less likely to express a desire for this type of care. By contrast, patients in this cohort of SOT practitioners, where preventive/wellness approaches to health are emphasized in their practices (and presumably transmitted through patient social and informal referral networks), appeared to report higher rates of wellness seeking preferences. This phenomenon might have important implications for those chiropractic educators and policy-makers who also continue to advocate a primary healthcare role for chiropractors, particularly emphasizing wellness/preventive care. A profession that does not regularly offer their patients primary care services nor educate their patients as to their capabilities to serve as a primary care provider will certainly find it challenging to alter patient attitudes and behaviors in this regard.
Consistent with the broader literature on gender differences in health attitudes and practices,20–25 women in the present sample were more likely to express interest in wellness, prevention, and self-care compared to men, who were somewhat more prone to favor illness care, which was most evident in the responses from the European sample. Although explanations for these well-documented gender differences are complex and remain a focus of active research efforts, there are some empirical hints in the broader literature that women’s socialization experiences may sensitize them to identify incipient somatic symptoms, and facilitate help-seeking sooner than their male counterparts. By contrast, traditional male socialization tends to reward risk-taking and a projected image of strength, which often involves problem denial (especially at sub threshold levels of severity such as those associated with emerging health problems) and a reluctance to seek help.20–25 These socialization patterns have direct implications for women’s greater propensity to seek out health information and to utilize primary prevention and early detection efforts.26,27 However, our findings also resonate with extant research suggesting that, despite well-documented gender differences, within group variability also exists in men and women’s health beliefs and practices,28 highlighting the need to continue efforts at unpacking the construct of gender with an eye toward better tailoring of public health promotion messages.22 This need for more relevant public health communications is especially pressing given that the health behaviors of most adults still fall far short of public health recommendations29 and that these modifiable risk factors significantly impact national health care costs.30
Interestingly, the geographic differences noted herein are also consistent with the burgeoning literature highlighting the importance of sociocultural and ethnic factors in shaping symptom perceptions and motivations for seeking health care. Although very little research has focused specifically on chiropractic, numerous longitudinal and cross-sectional studies have documented regional variability in lifestyle, symptom perception, illness behavior, general health care utilization, and health outcomes as a function of complex combinations of sociocultural, ethnic, and other local influences.31–33 Hence, in addition to being compatible with results from the broader health care literature, our findings on regional variability provide a preliminary foundation on which to build subsequent research on consumer motivations for seeking chiropractic care specifically.
Although international in scope, our convenience sample of SOT practitioners certainly introduced selection bias, thereby reducing the generalizability of the results. The point was to demonstrate whether the previously reported low rates of demand for wellness care were a function of lack of interest on the part of patients or, perhaps, a lack of understanding on the part of previous chiropractic patients and their doctors that wellness/preventive care was an option. The absence of information on patient ethnicity, socioeconomic status, and other potentially relevant background characteristics (which was not collected in the present study) may have also constrained our ability to examine some potentially important influences on patient care preferences. Moreover, the self-reported nature of responses may have been influenced by a variety of potential response biases (including social desirability and other demand characteristics). In addition, the cross sectional nature of the data certainly precludes any inferences about causality.
Further study should include more controlled research that systematically examines chiropractic preferences, perhaps utilizing an expanded survey administered in a variety of chiropractic settings (beyond SOT) where wellness/preventive care is normatively, ethically practiced, including questions targeting patient interest in receiving wellness/preventive care from their chiropractors.
Conclusion
This study was an attempt to determine patients’ specific wellness preferences when seeking chiropractic care. Based on an international convenience sample of Sacro-Occipital technique (SOT) practitioners utilizing a broad palate of holistic methods, more than 40% of patients agreeing to participate in this study self-reported a preference for care targeted at health enhancement and/or disease prevention. Although generalizations from these preliminary data cannot be made, the findings from this study suggest there may be a sector of chiropractic patients who seek out a more comprehensive paradigm of chiropractic care that conceptualizes health broadly, beyond the simple absence of disease or disability.34 Indeed, the Final Report of the Identity Consultation Task Force of the World Federation of Chiropractic includes the following foundational statement: “A patient-centered and biopsychosocial approach, emphasizing the mind/body relationship in health, the self-healing powers of the individual, individual responsibility for health, and encouraging patient independence” (page ii).15 In order for chiropractors to optimally serve their patients, there appears to be a need for greater clarity and more well-developed understanding of actual consumers’ health care preferences. While the research literature indicates that there is a substantial demand for complementary and alternative care in the United States,1,2,35 further research is warranted to evaluate how chiropractors may ethically and productively serve various subpopulations who exhibit a preference for including access to some chiropractic wellness approaches to health promotion and disease prevention.
Appendix: Patient Health Preference Categories*
| Behavior | Definition |
| Wellness | Activity undertaken by a person, who believes himself to be healthy, for the purpose of attaining a greater level of health. |
| Preventive Health | Activity, undertaken by a person, who perceives himself to be healthy, for the purpose of preventing illness or detecting it in an asymptomatic state. |
| At-risk | Activity undertaken by a person, who believes himself to be healthy, but at greater risk of developing a specific health condition, for the purpose of preventing that condition or detecting it in an asymptomatic state. |
| Illness | Activity undertaken by a person, who perceives himself to be ill, to define the state of his health and discover a suitable remedy. |
| Sick role | Activity undertaken by a person, who considers himself to be ill, for the purposes of getting well. It includes receiving treatments, involves few dependent behaviors, and leads to some degree of neglect of ones’ usual duties. |
| Self care | Activity undertaken by a person, who considers himself to be ill, for the purpose of getting well. It includes minimal reliance on therapists, involves a few dependent behaviors, and leads to little neglect of one’s duties. |
Handbook of Clinical Chiropractic Care, 2005: Jones and Barlett Publishers, Sudbury, MA. www.jbpub.com, Reprinted with permission.
Form Sent to Participating SOT Clinicians
Health Behaviors [1][2]
Wellness behavior – Are you here today because although you feel healthy you want to even have a greater level of health?
Preventive health behavior – Are you here today because although you feel healthy you want to help prevent an illness or possible injury?
At-risk behavior – Are you here today because although you feel healthy you have a tendency to be at risk for injuring yourself and want to prevent that from happening?
Sick role Behavior – Are you here today because you are injured or ill and want help so that you will feel better, without having to do any home therapies or modifying activities out of this office?
Self role Behavior – Are you here today because you are injured or ill and want help so that you will feel better, and want to have home therapies and activities that I can do to help myself outside this office? [2]
It is questionable whether one can “motivate someone sufficiently to affect their lifestyle behaviors which play a large role in many of today’s disease states.” [2] If effective health promotion is based upon the person’s willingness to change for something better and wellness is a behavior, then understanding various health behaviors will help gain insight into the types of patients and what they are seeking in a chiropractor’s office. [2]
As chiropractors “acknowledge that patients may present with various health behaviors the clinical encounter will become more exacting as well as educational. The knowledge of such behaviors will aid in identifying patients to help meet their unique individual needs.” [2]
Few if any studies have been performed in the chiropractic profession evaluating patients’ health behaviors relating to their reason for seeking chiropractic care. While it might not seem all that important to a typical practitioner it is essential for those in the research and epidemiological community to understand the thought processes of a typical chiropractic patient. This pilot study will help gain insight and greater understanding into the nature of the presenting health behavior of patients in a sacro occipital technique (SOT) chiropractic office.
- 1.Green LW, Kreuter MW. Health Promotion Planning. Mayfield Publishing Company; Mountain View, CA: 1999. [Google Scholar]
- Mirtz TA. Health Promotions in Clinical Practice. 2nd edition. Jones and Bartlett Publishers; Sudbury, MA: 2005. pp. 8–9. Handbook of Clinical Chiropractic Care (Wyatt LH) [Google Scholar]
Appendix: DOCTOR’S INFORMATION REGARDING SURVEY FORM
Thank you so much for being a part of this project. The information will be extremely important for chiropractic and helpful that SOT practitioners are pioneering this effort and are associated with chiropractic research.
For purposes of patient confidentiality we would appreciate not having any forms that have patient’s names on them sent in any communication. The easiest way to compile this information would be as follows:
Before the doctor sees the patient the first thing is that at the front desk or wherever the initial intake is made that the patient reads the form and fills it out. Ideally this would only be filled out by one patient once, unless there is a change in their presentation to the office.
The doctor or front desk personal can assess a identification number for the patient by the number of responses filled out starting from 001, 002, 003 etc. (The first person to fill out the form would be 001, the second one would be 002, and so on.)
Age and gender are helpful in determining various statistical analysis of the responses and if the patient neglects to fill in or forgets to fill in, staff can assist in this data gathering.
It would be preferred if the doctor in the study would keep the raw data in a safe place but send only a filled out table which can be photocopied along with the initial health behavior questionnaire.
- The sample table would look like this:Sample Participating Doctor’s Survey Form
Patient Gender Age Number Selection 001 M 34 4 002 F 45 1 003 F 21 2 Once the sample survey forms are filled out then they can be send by mail to Charles L. Blum, DC, 1752 Ocean Park Boulevard, Santa Monica, CA 90405 or via fax at (310) 478–1918.
Your help is greatly appreciated and will help further understanding of health behavior models and their relationship to chiropractic and SOT practices.
Appendix: Form Filled Out by Patients
Patient Identification Number: __________
Gender M F Age ______
CHIROPRACTIC RESEARCH STUDY
Thank you for taking a few moments to circle the number next to the question that relates to the reason why you have come to this chiropractic office today. We know there can be various reasons for your office visit today and more than one answer might apply, but please pick only ONE that most relates to you currently.
Are you here today because although you feel healthy you want to even have a greater level of health?
Are you here today because although you feel healthy you want to help prevent an illness or possible injury?
Are you here today because although you feel healthy you have a tendency to be at risk for injuring yourself and want to prevent that from happening?
Are you here today because you are injured or ill and want help so that you will feel better, without having to do any home therapies or modifying activities out of this office?
Are you here today because you are injured or ill and want help so that you will feel better, and want to have home therapies and activities that you can do to help yourself outside this office?
Thank you very much for participating in this chiropractic research study. The information you provided will be used to improve the quality of chiropractic care in the future.
Footnotes
Preliminary portions of this research were presented at the 13th Annual Conference of the Association of Chiropractic Colleges, the abstracts of which were published in The Journal of Chiropractic Education [Blum et al. (2006). Patient preference for wellness care: Is it on the menu? The Journal of Chiropractic Education, 20(1), 53].
References
- 1.Eisenberg D, Davis R, Ettner S, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the U.S.: prevalence, costs and patterns of use. NEJM. 1993;280:1569–75. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 3.Hawk C. Should chiropractic be a “wellness” profession? Top Clin Chiropr. 2000;7:23–26. [Google Scholar]
- 4.Hawk C, Rupert RL, Hyland JK, Odhwani A. Implementation of a course on wellness concepts into a chiropractic college curriculum. J Manipulative Physiol Ther. 2005;28:423–428. doi: 10.1016/j.jmpt.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Kessler R, Davis R, Foster D, et al. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 6.Wolsko P, Eisenberg D, Davis R, et al. Insurance coverage, medical conditions, and visits to alternative medicine providers. Arch Intern Med. 2002;162:281–287. doi: 10.1001/archinte.162.3.281. [DOI] [PubMed] [Google Scholar]
- 7.Astin JA. Why patients use alternative medicine. JAMA. 1998;279:1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 8.Thurkettle M, Noji A. Shifting the healthcare paradigm. Lippincott’s Case Management. 2003;8:160–165. doi: 10.1097/00129234-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Gladwell M. The tipping point. Little, Brown & Co.; 2000. [Google Scholar]
- 10.Bausell R, Berman B. Commentary: alternative medicine: is it a reflection of the continued emergence of the biopsychosocial paradigm? American Journal of Medical Quality. 2002;17:28–32. doi: 10.1177/106286060201700106. [DOI] [PubMed] [Google Scholar]
- 11.Nelson C. Chiropractic and wellness care. Journal of Chiropractic Humanities. 1994;4:3–19. [Google Scholar]
- 12.Health Resources and Services Administration. Association of Schools of Public Health; 2002. A model course for public health education in chiropractic colleges. ASPH Project #H092-04/04. [Google Scholar]
- 13.The Council on Chiropractic Education. Standards for Doctor of Chiropractic Programs and Requirements for Institutional Status. Scottsdale, AZ: The Council on Chiropractic Education; 2006. pp. 45–47. [Google Scholar]
- 14.US Department of Health and Human Services. Healthy People 2010: understanding and improving health. 2nd ed. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 15.World Federation of Chiropractic. Final Report of the Identity Consultation Taskforce April 30, 2005. Carey P, Clum G, Dixon P. Task Force Co-Chairs. Available at http://www.wfc.org/Website/WFC/Library.nsf/CatalogByTitleLive/Aa-TF%20Final%20Rept-Am%2004-29-05/$FILE/Aa-TF%20Final%20Rept-Am%2004-29-05.pdf (accessed 10–22–07)
- 16.World Federation of Chiropractic. World Federation of Chiropractic; Dec 7, 2004. Consultation on Identity: Quantitative Research Findings. Available at: http://www.wfc.org/Website/WFC/Library.nsf/CatalogByTitleLive/WFC%20Report_January%2052005/$FILE/WFC%20Report_January%2052005.ppt (last accessed 4–22–07) [Google Scholar]
- 17.National Board of Chiropractic Examiners. Job Analysis of Chiropractic. 2005 Available at: http://www.nbce.org/publications/pub_analysis.html.
- 18.Green LW, Kreuter MW. Health Promotion Planning. Mayfield publishing Company; Mountain View, CA: 1999. [Google Scholar]
- 19.Nelson CF, Lawrence DJ, Triano JJ, Bronfort G, Perle SM, Metz RD, Hegetschweiler K, LaBrot T. Chiropractic as spine care: a model for the profession. Chiropr Osteopat. 2005 Jul 6;13:9. doi: 10.1186/1746-1340-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Courtenay W. Constructions of masculinity and their influence on men’s well being: A theory of gender and health. Soc Sci Med. 2000;50:1385–1401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 21.Courtenay W, McCreary D, Merighi J. Gender and ethnic differences in health beliefs and behaviors. J Health Psych. 2002;7:219–231. doi: 10.1177/1359105302007003216. [DOI] [PubMed] [Google Scholar]
- 22.Doyal L. Sex, gender, and health: The need for a new approach. BMJ. 2001;323:1061–1063. doi: 10.1136/bmj.323.7320.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.King K, Arthur H. Coronary heart disease prevention: views on women’s gender-based perceptions and meanings. J Cardiovasc Nurs. 2005;18:274–281. doi: 10.1097/00005082-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Spitzer D. Engendering health disparities. Canadian J Public Health. 2005;96(Suppl 2):S78–S96. doi: 10.1007/BF03403704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verbrugge L. Gender and health: An update on hypotheses and evidence. J Health Social Behavior. 1985;26:156–182. [PubMed] [Google Scholar]
- 26.Evans R, Brotherstone H, Miles A, Wardle J. Gender differences in early detection of cancer. J Men’s Health & Gender. 2005;2:209–217. [Google Scholar]
- 27.Stewart D, Abbey S, Shnek Z, et al. Gender differences in health information needs and decisional preferences in patients recovering from an acute ischemic coronary event. Psychosomatic Med. 2004;66:42–48. doi: 10.1097/01.psy.0000107006.83260.12. [DOI] [PubMed] [Google Scholar]
- 28.Schofield T, Connell R, Walker L, et al. Understanding men’s health and illness: a gender-relations approach to policy, research, and practice. J Amer College Health. 2000;48:247–256. doi: 10.1080/07448480009596266. [DOI] [PubMed] [Google Scholar]
- 29.Reeves M, Rafferty A. Healthy lifestyle characteristics among adults in the United States, 2000. Arch Intern Med. 2005;165:854–857. doi: 10.1001/archinte.165.8.854. [DOI] [PubMed] [Google Scholar]
- 30.Anderson D, Whitmer W, Goetzel R, et al. The relationship between modifiable health risks and group-level health care expenditures. Am J Health Promot. 2000;15:45–52. doi: 10.4278/0890-1171-15.1.45. [DOI] [PubMed] [Google Scholar]
- 31.deGroot L, Verheijden M, Henauw S, et al. Lifestyle, nutritional status, health, and mortality in elderly people across Europe: A review of the longitudinal results of the SENECA study. Journal of Gerontology: Medical Sciences. 2004;12:1277–1284. doi: 10.1093/gerona/59.12.1277. [DOI] [PubMed] [Google Scholar]
- 32.Shire N. Effects of race, ethnicity, gender, culture, literacy, and social marketing on public health. J Gender-Specific Med. 2002;5:48–54. [PubMed] [Google Scholar]
- 33.Schwartz S, Rubel T. Sex differences in value priorities: cross-cultural and multimethod studies. J Personality Social Psych. 2005;6:1010–1028. doi: 10.1037/0022-3514.89.6.1010. [DOI] [PubMed] [Google Scholar]
- 34.Insel P, Roth W, Price K. Core concepts in health. 9th ed. McGraw-Hill; New York, NY: 2004. [Google Scholar]
- 35.Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in Use of Complementary and Alternative Medicine by US Adults: 1997–2002. Alternative Therapies. 2005;11(1):42–9. [PubMed] [Google Scholar]