Abstract
Purpose
Overweight in adolescence is a significant problem which is associated with body dissatisfaction and eating disorder (ED) behaviors. Cost-effective methods for early intervention of obesity and prevention of ED are important due to the refractory nature of both. This multisite RCT evaluated an Internet-delivered program targeting weight loss and ED attitudes/behaviors in adolescents.
Methods
Eighty overweight 12-17-year olds completed Student Bodies 2 (SB2), a 16-week cognitive-behavioral program, or usual care (UC).
Results
BMI z-scores were reduced in the SB2 group compared to the UC group from baseline (BL) to post-intervention (p=.027; ηp2=.08). The SB2 group maintained this reduction in BMI-z at 4-month follow-up, but significant differences were not observed due to improvement in the UC group. The SB2 group evidenced greater increases in dietary restraint at post (p=.016) and less improvement on shape concerns at follow-up (p=.044), however, these differences were not clinically significant. No other statistically significant differences were noted between groups on ED attitudes/behaviors. SB2 participants reported using healthy eating- and physical activity-related skills more frequently than UC participants at post (p=.001) and follow-up (p=.012).
Conclusions
Findings suggest that an Internet-delivered intervention yielded a modest reduction in weight status that continued four months following treatment and that ED attitudes/behaviors were not significantly improved. Group differences on weight loss were not sustained at 4-month follow-up due to parallel improvements in the groups. Future studies are needed to improve program adherence and to further explore the efficacy of Internet-delivery of weight control programs for adolescents.
Keywords: Overweight, treatment, Internet, eating disorders
More than one out of three adolescents is currently overweight or at-risk-for-overweight (OW) [1]. Many of these adolescents experience compromised mental and physical health [2] and are much more likely to face serious and chronic illnesses as adults [3]. Although a recently published review of the obesity literature points to well-established weight loss treatments for children between the ages of 8 and 12 years [4], few randomized controlled trials targeting weight loss in adolescents have been conducted. As described in this review, behavior modification counseling (e.g., self-monitoring of diet and physical activity) holds the most promise for adolescents [4] and addressing cognitive barriers (e.g., body dissatisfaction) may be a helpful adjunct [5-7].
A challenging aspect of treating OW in adolescents is the presence of higher rates of weight/shape concerns and disordered eating behaviors, indicating elevated risk for the development of eating disorders (ED) [6, 8] and related barriers to effective weight control. OW adolescents use unhealthy and harmful weight loss techniques at a higher rate than normal weight adolescents who are equally dissatisfied with their bodies, possibly in an attempt to find a quick solution to their weight problem [9]. Simultaneously, OW adolescents are also less likely to engage in healthy eating habits and physical activity [10-11], both of which are essential for healthy weight control, making weight management more difficult. Likewise, OW may be perpetuated through dieting, by way of disinhibition of eating (e.g., binge eating) following bouts of dietary restraint [12]; however, ED symptoms have rarely been addressed in weight loss programs and the importance of treating both has been noted [6].
Due to the magnitude of obesity's impact on public health and the challenge of treating the OW population solely through face-to-face programs (e.g., due to transportation and financial limitations [13]), innovative and cost-effective methods of intervention are needed [14]. The Internet is a promising mode of service delivery due to its accessibility and convenience [14]. Internet-delivered weight loss interventions have been tested in adults with moderate success [15-17], and one study in African American adolescent girls and their parents reported short-term results in favor of the Internet intervention [18], which then dissipated at 18-month follow-up [19]. In addition, Internet interventions have been successful in reducing ED risk factors, as well ED onset in some high-risk subgroups [20-21]. To date, however, an Internet program targeting a diverse group of adolescents for weight loss and ED prevention has not been evaluated to our knowledge.
This study presents an evaluation of an Internet-delivered program concurrently targeting weight loss and ED attitudes and behaviors in adolescents. It was hypothesized that participants in the experimental group would show improvements in weight status and ED attitudes and behaviors compared with a control group receiving usual care. Secondary hypotheses include improvements in the intervention group on dietary behaviors and physical activity-related behaviors compared with the control group.
Methods
Participants
Participants were recruited in San Diego and St. Louis through newspaper and on-line advertisements, and flyers posted at schools, medical facilities, and weight loss organizations targeting adolescents interested in losing weight and their parents. In addition, referrals were obtained through pediatricians and school nurses.
Participants were eligible if they were between the ages of 12-18, overweight or at risk for overweight (≥85th percentile [22]), and had Internet access either at home or at a location where regular use was possible (e.g., school, library). Exclusion criteria included: the presence of medical conditions (e.g., endocrinologic diseases) or use of prescription medication resulting in significant weight changes; complications of OW that contraindicated moderate physical activity (e.g., orthopedic disorders); and past or present diagnosis of a clinical ED (i.e., anorexia nervosa, bulimia nervosa, binge eating disorder).
The number of participants targeted for enrollment was chosen based on results of an adolescent weight control intervention by Saelens and colleagues [23]. Estimating an effect size of f=0.40 with power of 0.80 to detect an effect on weight outcomes using ANOVA, the necessary number of participants was calculated to be 52. Accounting for 20% attrition, at least 62 participants were deemed necessary at baseline.
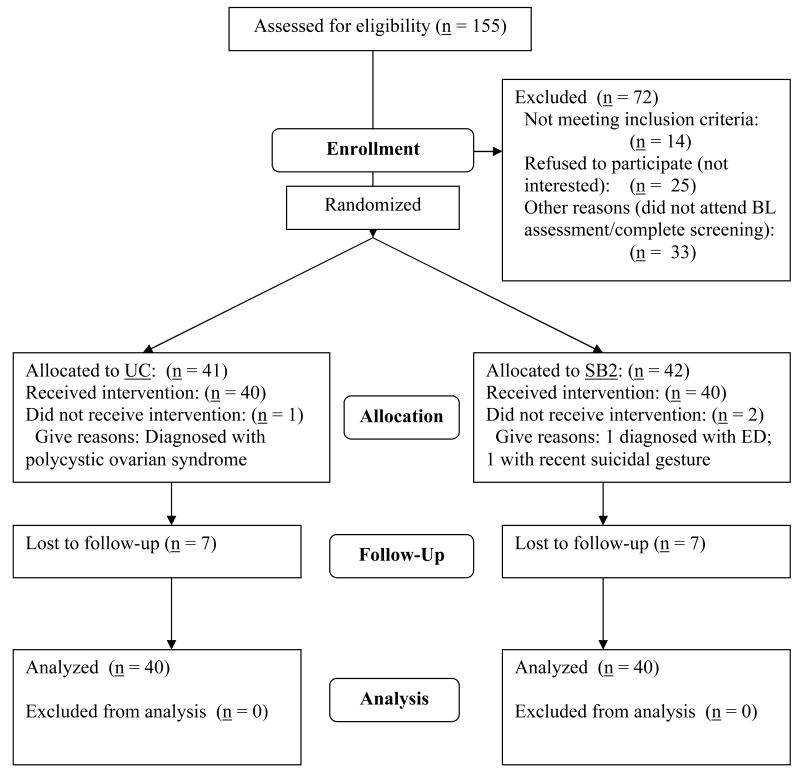
One hundred fifty-five adolescents or their parents contacted the study with interest in participation (see Figure 1) between November 2003 and May 2005. Subsequently, 83 adolescents were deemed eligible and randomized to either the intervention group (n = 42) or control group (n = 41). Three participants were excluded after randomization had taken place because of medical or psychiatric problems. This resulted in sample sizes of 40 adolescents for both the intervention and control groups. Participants were enrolled in the study in four separate cohorts; two cohorts were run in San Diego, CA and two cohorts were run in St. Louis, MO. Participant demographics can be found in Table 1.
Figure 1.
Participant Flowchart.
Table 1. Demographic characteristics of sample.
|
Student Bodies 2 (n = 40) |
Usual Care (n = 40) |
Total (n = 80) |
|||
|---|---|---|---|---|---|
| Age, M (SD) | 14.9 (1.7) | 14.1 (1.6) | 14.5 (1.7) | t(78) = -2.06, p = .04 | |
| BMI, M (SD) | 34.8 (7.6) | 33.6 (6.3) | 34.2 (7.0) | ||
| BMI percentile, M (SD) | 97.6 (2.8) | 97.8 (2.4) | 97.7 (2.6) | ||
| Sex | Girls | 26 (65.0%) | 24 (60.0%) | 50 (62.5%) | |
| Boys | 14 (35.0%) | 16 (40.0%) | 30 (37.5%) | ||
| Race | White | 21 (52.5%) | 19 (47.5%) | 40 (50%) | |
| Black | 11 (27.5%) | 10 (25.0%) | 21 (26.3%) | ||
| Hispanic | 3 (7.5%) | 7 (17.5%) | 10 (12.5%) | ||
| Other | 5 (12.5%) | 4 (10.0%) | 9 (11.3%) | ||
| Internet Access at Home | |||||
| Yes | 37 (92.5%) | 40 (100%) | 77 (96.3%) | ||
| No | 3 (7.5%)* | 0 (0%) | 3 (3.8%) | ||
| Parent Highest Education Achieved | |||||
| < High school | 2 (5.1%) | 1 (2.5%) | 3 (3.8%) | ||
| High school graduate | 3 (7.7%) | 3 (7.5%) | 6 (7.6%) | ||
| Some college or technical school | 17 (43.6%) | 19 (47.5%) | 36 (45.6%) | ||
| College graduate | 7 (17.9%) | 9 (22.5%) | 16 (20.3%) | ||
| Some graduate school | 3 (7.7%) | 4 (10.0%) | 7 (8.9%) | ||
| Graduate/Professional degree | 7 (17.9%) | 4 (10.0%) | 11 (13.9%) | ||
| Marital status | |||||
| Married/Remarried | 25 (62.5%) | 25 (62.5%) | 50 (62.5%) | ||
| Single, Divorced, or Separated | 15 (37.5%) | 15 (37.5%) | 30 (37.5%) | ||
Participants had access to the Internet at school, a relative's house, or a local library.
Procedures
Adolescents or parents who responded to study advertisements were assessed for initial eligibility via a telephone screen after verbal consent was obtained. If initial eligibility criteria were met, an in-person baseline (BL) assessment was scheduled. At that time, informed consent (parents/guardians) and assent (adolescents) were obtained in compliance with the IRBs of San Diego State University, University of California at San Diego, and Washington University.
Following completion of BL measures, adolescents were randomly assigned to the intervention or control group. Randomization occurred by selection among opaque envelopes prepared by research assistants, with each envelope containing information on the intervention or control group. If the adolescent was assigned to the intervention group, the adolescent and parent received a brief orientation to the Internet program, a pedometer, and a calorie/fat guide for common foods and beverages.
Adolescents assigned to Usual Care (UC) and their parents received color handouts containing basic information on nutrition and physical activity, but were not given specific instructions on behavior modification. They were told to continue visit their physicians as needed. The UC group was offered access to the Internet program at the conclusion of the 4-month follow-up.
Intervention
Student Bodies 2 (SB2) is a 16-week, Internet-delivered program using a cognitive-behavioral approach to help OW adolescents lose weight and increase positive body image. SB2 weekly content includes basic education (e.g., portion sizes, recommended daily activity), guided behavior modification for weight control (e.g., self-monitoring with feedback), and cognitive exercises for improving body image (see Table 2). The first 8 weeks of the program were primarily oriented towards behavioral weight loss while the focus shifted towards body image improvement during the second half of the program. SB2 uses gender-specific Internet interfaces for visual appeal (e.g., more feminine/masculine color schemes) and boys and girls are automatically guided to gender-specific content (e.g., media portrayals of attractiveness). Each week, adolescents were asked to record their food intake, the amount of physical activity attained, and their weekly weight using a private, on-line journaling feature. Participants were expected to spend 1-2 hours/week and no more than 30 minutes/day using the program.
Table 2. Program components of Student Bodies 2.
| Program Components | Description |
|---|---|
| Psychoeducational readings | Reading modules included Nutrition; Fitness (including Physical Activity/Sedentary Behaviors); Body Image (including eating disorder prevention, binge eating module); and Behavior Change skills |
| Discussion group | On-line, asynchronous, discussion group, moderated by a psychology doctoral student with close supervision, used for communication with other adolescents for social support and problem solving. |
| Food, activity, and weight monitoring | Private on-line journals used for self-monitoring. Behavioral modification was aimed at establishing healthy eating and physical activity patterns. |
| Body image journal | Private on-line journal to record triggers to negative body image and practice challenging negative thoughts. Increase awareness of thoughts and feelings related to body. |
| Weekly newsletter (emailed) | Moderator provided feedback on participant progress and encouraged compliance. |
| Personal profiles | On-line profiles of participants to facilitate communication & cohesion in discussion group. |
| Participant-only site/password protected | Protection of privacy. |
| Automatic, timed log-off | Protection of privacy. |
| Parent newsletter | Mailed materials sent once/month. Included psychoeducation, descriptions of what their adolescent was learning & tips for parents. |
A clinical psychology doctoral student moderated the program with close supervision by a licensed clinical psychologist. The moderator emailed each SB2 participant a weekly newsletter containing individualized feedback regarding food, physical activity, and weight journals, as well as any other program activities for the week (e.g., setting goals for reducing sedentary activity). Additionally, participants were invited to use an on-line body image journal to record triggers to body dissatisfaction as they learned how to challenge negative thoughts. The website also served as the forum for a moderated discussion group for the adolescents. The moderator guided the asynchronous discussion group for the adolescents, which ranged in size from 8-13 participants across the four cohorts. The discussion group was developed to be an enjoyable place for the adolescents to seek support, build relationships, and problem-solve as a group.
Adherence was monitored by reviewing participants' log-on data and use of on-line journals. Also, the moderator was able to access participants' journals to assess adherence with journal entries, with the participants' consent. Participants' adherence with the intervention was encouraged through a lottery system based on completion of program tasks in which participants were could win $20 gift cards; weekly, brief telephone calls to check in on difficulties with the program; and reminders provided through the weekly newsletters.
A monthly newsletter was mailed to parents to encourage creating a positive and constructive home environment in which their adolescent could achieve his/her health goals. In addition, the moderator was available to the parents via telephone during the program to answer questions and to give additional guidance on these topics as needed.
Assessment
Assessments occurred at three time points: BL, post-treatment, and 4-month follow-up (FU). Assessors were blinded to group assignment. The follow-up period ended in January 2006.
Primary outcomes
Participants were weighed and measured in plain clothes (i.e., after removing shoes, coats, and heavy clothing items) using a calibrated balance-beam or digital scale and a wall-mounted stadiometer. The same scale and stadiometer were used at each assessment timepoint within each site. BMI z-scores, calculated using CDC 2000 data, were chosen as the primary outcome variable in order to control for differences in sex and age [24].
The Eating Disorder Examination-Questionnaire (EDE-Q) [25] is a validated, self-report version of the Eating Disorder Examination interview (EDE) [26], which is a rigorous assessment of ED psychopathology over the past 28 days. The EDE-Q yields Weight Concern, Shape Concern, Eating Concern, and Dietary Restraint subscales, as well as a global score of overall eating pathology. The frequency of diagnostic behaviors, such as binge eating and self-induced vomiting, are also assessed. The EDE-Q has good internal consistency (alpha coefficients: .78-.93) and test-retest reliability (Pearson r: .81-.94; [27]). For the St. Louis participants (n = 35), a youth version of the EDE-Q which uses simplified language was administered [28] in an effort to pilot test this new instrument.
Secondary outcomes
The frequency of adolescent behavioral and cognitive skills use (e.g., self-monitoring, problem solving, seeking out social support, setting goals) related to eating and physical activity over the past four months were assessed using a questionnaire adapted for this study from measures used by Saelens and colleagues [23]. Psychometrics are not yet available for this qualitative questionnaire, which includes items such as, “How often did you set goals for your eating for the week?” In addition, the intervention group was administered a qualitative questionnaire to measure satisfaction with the Internet program (e.g., “Overall, how satisfied were you with the discussion group?”) and an on-line social support scale using Likert responses indicating level of agreement (e.g., “I could talk about my concerns with members of the on-line discussion group.”) [29] at post-treatment.
Data Analytic Plan
Data were screened for normality. BL differences between groups and sites were assessed using chi-square and t-tests. Analyses were run excluding participants who were not measured in person (SB2: n = 33/40; UC: n = 33/40) as well as intent-to-treat, with missing data replaced with BL values. Adherence was measured as the percentage of screens accessed on-line.
The primary hypothesis was tested using analyses of covariance (ANCOVAs) for BL to post and BL to FU. Multiple analyses of covariance (MANCOVA) were conducted for the EDE-Q subscales. Group was included as a fixed factor. For all of the aforementioned analyses, BL values of the dependent variable(s) were included as covariates, along with site and demographic variables for which there were BL differences between groups. In addition, effect sizes (partial eta squared, ηp2) were calculated. Only participants who completed assessments were included in effect size calculations.
Results
Preliminary Analyses
All variables were approximately normally distributed. At BL, SB2 participants were slightly older than the control group (see Table 1). Sites differed by ethnicity (χ2(3) = 10.83, p = .01), with a greater proportion of Black participants at the St. Louis site (40% vs. 15.6%) and a greater proportion of Hispanics at the San Diego site (20% vs. 2.9%), reflecting area demographics. Thus, ethnicity, site, and age were entered as covariates in the analyses.
Primary Analyses
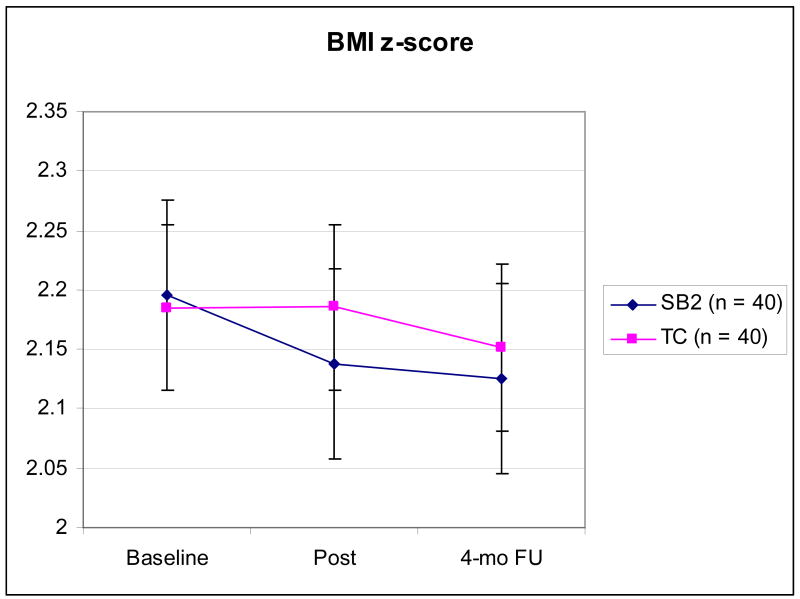
ANCOVAs of BMI z-scores yielded a significant difference between groups from BL to post (F(5,60) = 5.11, p = .027), but not from BL to FU (F(5,60) = 1.14, p = .289; see Figure 2). Intent-to-treat analyses were non-significant from BL to post (F(5,74) = 3.78, p = .056) and BL to FU (F(5,74) = 0.64, p = .426). Translated into absolute weight and height changes, the SB2 participants lost 0.14 lbs (SD = 9.09) from BL to post and then gained 4.20 lbs (SD = 10.93) from post to FU. The UC participants gained 4.71 lbs (SD = 12.17) from BL to post and gained an additional 3.71 lbs (SD = 10.54) from post to FU. Due to increases in height (M = 1 inch, SDs = 0.80 [SB2], 0.92 [UC]) and age, these changes translated into a reduction of OW for both groups. Means and effect sizes are presented in Table 3.
Figure 2.
BMI z-scores by group with error bars.
Table 3. Means, standard deviations, and effect sizes (partial eta squared) for participants with complete data at each time point.
| Intervention (n = 33) | Control (n = 33) | |||||||
|---|---|---|---|---|---|---|---|---|
| BL M (SD) | Post M (SD) | 4-mo FU M (SD) | BL M (SD) | Post M (SD) | 4-mo FU M (SD) | BL-Post ηp2 | BL-4-month FU ηp2 | |
| BMI z | 2.19 (.50) | 2.11 (.51) | 2.10 (.51) | 2.19 (.44) | 2.20 (.43) | 2.15 (.48) | .08* | .02 |
| BMI | 34.64 (7.79) | 33.99 (7.60) | 34.37 (7.64) | 33.86 (6.87) | 34.07 (6.57) | 34.34 (6.90) | .06 | .03 |
| Weight (lbs) | 214.50 (65.32) | 214.36 (64.23) | 218.56 (64.43) | 206.06 (50.19) | 210.77 (47.21) | 214.49 (47.51) | .03 | .01 |
| EDE-Q | ||||||||
| Weight Concern | 2.24 (1.35) | 1.63 (1.17) | 1.95 (1.32) | 2.56 (1.12) | 1.99 (1.34) | 1.94 (1.55) | .00 | .04 |
| Shape Concern | 2.54 (1.61) | 2.00 (1.36) | 2.17 (1.54) | 2.95 (1.62) | 2.25 (1.60) | 1.96 (1.63) | .00 | .08* |
| Eating Concern | 1.03 (.93) | .72 (.64) | .89 (.91) | 1.18 (1.01) | .86 (.77) | .78 (.93) | .00 | .05 |
| Restraint | 1.05 (.93) | 1.56 (1.36) | 1.28 (1.06) | 1.40 (1.20) | 1.02 (.97) | .99 (1.15) | .12* | .06 |
Abbreviations: BL = Baseline; FU = Follow-up; EDE-Q = Eating Disorder Examination-Questionnaire.
= p<.05
MANCOVA demonstrated an increase in dietary restraint for the SB2 group (F(8, 71) = 6.1, p = .016) from BL to post. Both groups reported a decrease in Shape Concern between BL and FU, with a greater decrease in the UC group (F(8, 71) = 4.2, p = .044). All other subscale comparisons were non-significant.
Secondary Analyses
SB2 participants reported greater use of eating-related skills use than UC participants at post (F(5, 74) = 12.66, p = .001) and 4-mo FU (F(5, 74) = 6.58, p = .012). Similarly, SB2 participants reported greater use of PA-related skills use than UC participants at post (F(5, 74) = 12.91, p = .001) and 4-mo FU (F(5, 74) = 6.58, p = .012).
On average, SB2 participants read 29.9% (SD = 27.3) of the Internet material (range: 0– 90.7%) and 35% of the participants (n = 14) viewed <10% of the screens. Seventy-nine percent of SB2 participants were satisfied with the program, 15.8% were neither satisfied nor dissatisfied and 5.3% were dissatisfied. While 63.2% of participants were satisfied with the discussion group, 22.5% of the participants felt that there was not enough interaction within the group, and two participants suggested a real-time chat room rather than a discussion board. Participants reported moderate levels of social support obtained via the discussion group (M = 4.85, SD = 1.21; possible range: 1-7), which was comparable to past participants in Internet-delivered body image improvement programs (e.g., M = 4.79, SD = 1.1) and face-to-face group interventions for body image (M = 4.77, SD = 1.6) [30].
Discussion
A 16-week, Internet-delivered program produced a reduction in BMI z-score in adolescent boys and girls, which was not sustained in the four months following the intervention. Upon examining the data, the intervention group maintained their weight during the intervention, which is encouraging considering that adolescents can “outgrow” their overweight if they maintain weight and continue to increase in height [31], as they did in the current sample. In comparison, adolescents who received usual care, consisting of educational handouts on nutrition and physical activity, also reduced their BMI z-scores, but to a lesser degree. ED attitudes and behaviors were generally reduced in both groups, with slight, but not clinically significant, increases in dietary restraint (at post) and shape concerns (at follow-up) in the intervention group. These findings suggest that a minimally intensive and easily disseminable program is modestly effective for weight control in the short term and that ED risk factors were not significantly impacted either positively or negatively. These findings may have implications for the early intervention of OW without negative impact on ED risk.
The weight loss reported in this study is much less than that reported in adult studies [15, 17, 32]. However, the weight change from baseline to post was comparable to or better than that found in an evaluation of an Internet weight control program for African American adolescent females (e.g., +5.29 lbs control group; +1.21 lbs intervention) [33]. Adolescents may possess lower levels of self-efficacy or motivation to lose weight compared with adults. Parental involvement was limited in this study and it may be helpful to increase the support and motivation provided by parents in assisting adolescents with weight control. For instance, it may be beneficial to develop a parallel Internet program instructing parents on changing the home environment and providing instrumental support for their adolescents' behavioral changes (e.g., helping obtain a gym membership), as has been found in previous programs [19]. Specifically targeting parents for weight control, as well, may be an important way to increase family-wide behavioral changes for weight control [34].
Overall, the hypothesis that the intervention would reduce ED behaviors and attitudes compared to the control group was not supported. In fact, participants appeared to decrease ED symptoms in both groups, with the exception of dietary restraint. Dietary restraint can be defined as cognitive and/or behavioral efforts to limit food intake for shape or weight reasons. An example of this would be avoiding certain foods that one likes in an effort to change one's weight/shape or going for long periods of time without eating (e.g., 8 hours or more) in order to influence one's weight/shape. The intervention group reported increased dietary restraint from BL to post, which is likely due to adherence to program recommendations, rather than a reflection of increased ED attitudes or behaviors; indeed, the SB2 group's mean scores on the Restraint subscale were commensurate with healthy young adolescent girls [35] and OW adults [36]. Shape concerns were reduced in both groups, but to a greater degree in the control group. It is possible that the increased focus on weight control in the intervention group moderated the downward shift on this measure compared with the control group. In addition, to explore the possibility that different versions of the EDE-Q may have impacted these findings, the primary analyses were run separately for the EDE-Q and the youth version of the EDE-Q. The differences between the intervention and control groups on ED variables were no longer found, thus, differences between groups on shape concerns and dietary restraint may have been a product of using different versions of the EDE-Q.
Alternatively, it is possible that the lack of improvement in the SB2 group on ED variables was due to the limited exposure to the relevant materials in the intervention. Adherence with the intervention was surprisingly low, with one-third of participants accessing <10% of the program. Yet, low adherence with Internet-delivered programs for weight loss in youth has been seen in other studies [37]. This highlights the importance of identifying ways to increase adherence when using Internet-delivered programs with youth. Further, the ED related materials were presented during weeks 8-16 and this relatively late introduction may have come at a time when adherence was decreasing. In contrast, satisfaction was quite high, suggesting that Internet interventions are appealing to adolescents and that additional reminders through innovative means (e.g., cell phone text messaging) or incentives to use the program could improve adherence and outcome. An analysis of the effective components of the program could aid in reducing the overall number of program expectations, thus improving adherence as well.
The SB2 group reported greater use of eating- and PA-related weight-loss skills at post and 4-month FU, such as self-monitoring calorie intake and the use of problem-solving skills to be more physically active, than the control group. This finding reflects skills taught in the intervention and suggests that the SB2 group adopted and maintained important, healthy lifestyle changes. Although the reduction in OW was modest, these behavior changes could translate into future weight control.
Limitations of the current study include a small sample size and lack of longer-term follow-up. Also, these findings may not apply to adolescent populations with less comfort with and/or access to the Internet. The strengths of the current study include a randomized design incorporating a usual care group to represent what most OW adolescents might routinely receive in the community. The study's sample was ethnically diverse, with half of the sample identifying themselves as Black, Hispanic, or “other”, representing an important contribution given that most studies of pediatric obesity treatments have been conducted with a largely White population [38]. The current findings provide preliminary support for the feasibility of Internet-delivered weight control in reducing overweight status in adolescents.
Acknowledgments
This research was supported in part by a Student Research Award by the American Psychological Association's Division 38 (Health Psychology) to Angela Celio Doyle, Ph.D., grant 1K24MH070446-02 from the National Institute of Mental Health, National Institutes of Health, awarded to Denise E. Wilfley, Ph.D., and an RGA/Washington University Longer Life Foundation Research Award to Dr. Wilfley. Appreciation is expressed to Brian Saelens, Ph.D., for contributing program content from Health Habits to the intervention as well as Christina Huang and Janet Malacane for their invaluable help with recruitment and data collection.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Angela Celio Doyle, Department of Psychiatry, The University of Chicago
Andrea Goldschmidt, Department of Psychology, Washington University, St. Louis
Christina Huang, Department of Nutrition, Food Studies & Public Health, New York University
Andrew J. Winzelberg, Department of Psychiatry & Behavioral Science, Stanford University
C. Barr Taylor, Department of Psychiatry & Behavioral Science, Stanford University
Denise E. Wilfley, Department of Psychiatry, Washington University, St. Louis
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006 Apr 5;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Goldschmidt AB, Passi VA, Sinton MM, Tanofsky-Kraff M, Wilfley DE. Abnormal eating patterns in overweight children and adolescents Recent Progress in Obesity Research. Proceedings of the International Congress on Obesity Conference; 2007. [Google Scholar]
- 3.Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007 Dec 6;357(23):2371–9. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- 4.American Dietetic Association (ADA) Position of the American Dietetic Association: individual-, family-, school-, and community-based interventions for pediatric overweight. J Am Diet Assoc. 2006 Jun;106(6):925–45. doi: 10.1016/j.jada.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Zabinski MF, Saelens BE, Stein RI, Hayden-Wade HA, Wilfley DE. Overweight children's barriers to and support for physical activity. Obes Res. 2003 Feb;11(2):238–46. doi: 10.1038/oby.2003.37. [DOI] [PubMed] [Google Scholar]
- 6.Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res. 2006 Dec;21(6):770–82. doi: 10.1093/her/cyl094. [DOI] [PubMed] [Google Scholar]
- 7.Darby A, Hay P, Mond J, Rodgers B, Owen C. Disordered eating behaviours and cognitions in young women with obesity: relationship with psychological status. 2007 May;31(5):876–82. doi: 10.1038/sj.ijo.0803501. [DOI] [PubMed] [Google Scholar]
- 8.Burrows A, Cooper M. Possible risk factors in the development of eating disorders in overweight pre-adolescent girls. Int J Obes Relat Metab Disord. 2002 Sep;26(9):1268–73. doi: 10.1038/sj.ijo.0802033. [DOI] [PubMed] [Google Scholar]
- 9.Neumark-Sztainer D, Wall M, Eisenberg ME, Story M, Hannan PJ. Overweight status and weight control behaviors in adolescents: longitudinal and secular trends from 1999 to 2004. Prev Med. 2006 Jul;43(1):52–9. doi: 10.1016/j.ypmed.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 10.Boutelle K, Neumark-Sztainer D, Story M, Resnick M. Weight control behaviors among obese, overweight, and nonoverweight adolescents. J Pediatr Psychol. 2002 Sep;27(6):531–40. doi: 10.1093/jpepsy/27.6.531. [DOI] [PubMed] [Google Scholar]
- 11.Patrick K, Norman GJ, Calfas KJ, Sallis JF, Zabinski MF, Rupp J, Cella J. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch Pediatr Adolesc Med. 2004;158(4):385–390. doi: 10.1001/archpedi.158.4.385. [DOI] [PubMed] [Google Scholar]
- 12.Stice E, Shaw H, Nemeroff C. Dual pathway model of bulimia nervosa: Longitudinal support for dietary restraint and affect-regulation mechanisms. J Soc Clinical Psychol. 1998;17:129–149. [Google Scholar]
- 13.Neumark-Sztainer D, Martin SL, Story M. School-based programs for obesity prevention: What do adolescents recommend? American Journal of Health Promotion. 2000;14(4):232–235. doi: 10.4278/0890-1171-14.4.232. [DOI] [PubMed] [Google Scholar]
- 14.Zabinski MF, Celio A, Wilfley DE, Taylor CB. Prevention of eating disorders and obesity via the Internet. Cogn Behav Ther. 2003;32:137–150. doi: 10.1080/16506070310000939. [DOI] [PubMed] [Google Scholar]
- 15.Tate DF, Wing RR, Winett RA. Using Internet-based technology to deliver a behavioral weight loss program. JAMA. 2001 Mar 7;285(9):1172–7. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 16.Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: A pilot study comparing a structured behavioral intervention to a commercial program. Obesity. 2007 Jan;15(1):155–64. doi: 10.1038/oby.2007.520. [DOI] [PubMed] [Google Scholar]
- 17.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003 Apr 9;289(14):1833–6. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 18.Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe E, Alfonso A, Gordon S, Ryan D. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat Weight Disord. 2005 Sep;10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- 19.Williamson DA, Walden HM, White MA, York-Crowe E, Newton RL, Jr, Alfonso A, Gordon S, Ryan D. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006 Jul;14(7):1231–43. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 20.Taylor CB, Bryson S, Luce KH, Cunning D, Celio Doyle A, Abascal LB, Rockwell R, Dev P, Winzelberg AJ, Wilfley DE. Prevention of eating disorders in at-risk college-age women. Arch Gen Psychiatry. 2006 Aug;63(8):881–8. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heinicke BE, Paxton SJ, McLean SA, Wertheim EH. Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: A randomized controlled trial. J Abnorm Child Psychol. 2007 Jan 23; doi: 10.1007/s10802-006-9097-9. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. Health, United States, 2004 with chartbook on trends in the health of Americans. Hyattsville, Maryland: 2004. [PubMed] [Google Scholar]
- 23.Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obes Res. 2002 Jan;10(1):22–32. doi: 10.1038/oby.2002.4. [DOI] [PubMed] [Google Scholar]
- 24.Kuczmarksi RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. Adv Data. 314. 2000. Jun 8, CDC growth charts: United States; pp. 1–27. [PubMed] [Google Scholar]
- 25.Fairburn C, Beglin S. Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord. 1994 1994 Dec;16(4):363–70. [PubMed] [Google Scholar]
- 26.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12th. New York: The Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 27.Luce KH, Crowther JH. The reliability of the eating disorder examination – self-report questionnaire version (EDE-Q) Int J Eat Dis. 1999;25:349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 28.Goldschmidt AB, Celio Doyle A, Wilfley DE. Assessment of binge eating in overweight youth: Addressing the need for a questionnaire version of the Child Eating Disorder Examination. Int J Eat Dis. 2007;40(5):460–7. doi: 10.1002/eat.20387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Winzelberg AJ, Eppstein D, Eldredge KL, Wilfley DE, Dasmahapatra R, Dev P, Taylor CB. Effectiveness of an Internet-based program for reducing risk factors for eating disorders. J Consult Clin Psychol. 2000 Apr;68(2):346–50. doi: 10.1037//0022-006x.68.2.346. [DOI] [PubMed] [Google Scholar]
- 30.Celio AA, Winzelberg AJ, Wilfley DE, Eppstein D, Springer EA, Dev P, Taylor CB. Reducing risk factors for eating disorders: Comparison of an Internet- and a classroom-delivered psychoeducation program. J Consult Clin Psychol. 2000 Aug;68(4):650–7. [PubMed] [Google Scholar]
- 31.American Medical Association. [December 18, 2007]; Expert Committee Recommendations on the Assessment, Prevention, and Treatment of Child and Adolescent Overweight and Obesity [Online]. Available at: http://www.ama-assn.org/ama/pub/category/11759.html.
- 32.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006 Aug 14-28;166(15):1620–5. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- 33.White MA, Martin PD, Newton RL, Walden HM, York-Crowe EE, Gordon ST, Ryan DH, Williamson DA. Mediators of weight loss in a family-based intervention presented over the internet. Obes Res. 2004 Jul;12(7):1050–9. doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- 34.Epstein LH. Family-based behavioural intervention for obese children. Int J Obes Relat Metab Disord. 1996 Feb;20 1:S14–21. [PubMed] [Google Scholar]
- 35.Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behav Res Ther. 2001 May;39(5):625–32. doi: 10.1016/s0005-7967(00)00033-4. [DOI] [PubMed] [Google Scholar]
- 36.Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG. Using the eating disorder examination to identify the specific psychopathology of binge eating disorder. Int J Eat Disord. 2000 Apr;27(3):259–69. doi: 10.1002/(sici)1098-108x(200004)27:3<259::aid-eat2>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 37.Baranowski T, Baranowski JC, Cullen KW, Thompson DI, Nicklas T, Zakeri IE, Rochon J. The Fun, Food, and Fitness Project (FFFP): the Baylor GEMS pilot study. Ethn Dis. 2003 Winter;13(1 Suppl 1):S30–9. [PubMed] [Google Scholar]
- 38.Crawford PB, Story M, Wang MC, Ritchie LD, Sabry ZI. Ethnic issues in the epidemiology of childhood obesity. Pediatr Clin North Am. 2001 Aug;48(4):855–78. doi: 10.1016/s0031-3955(05)70345-x. [DOI] [PubMed] [Google Scholar]