Abstract
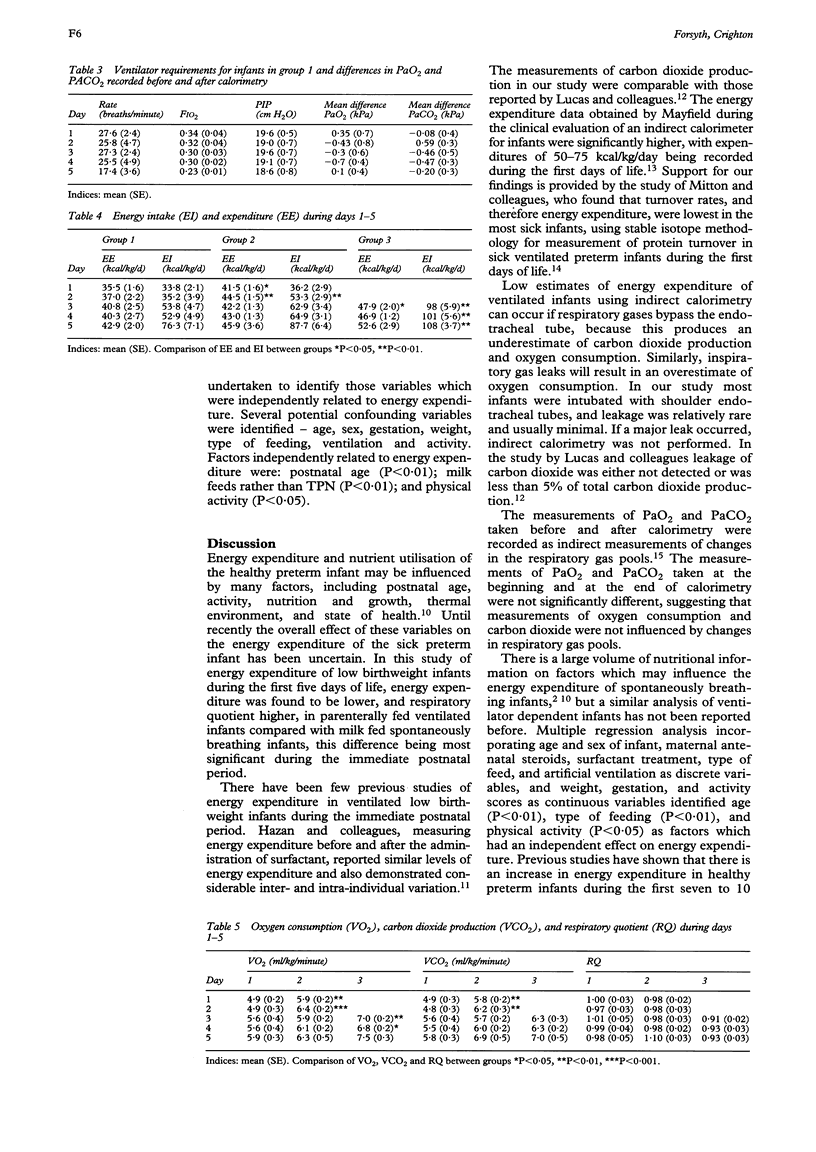
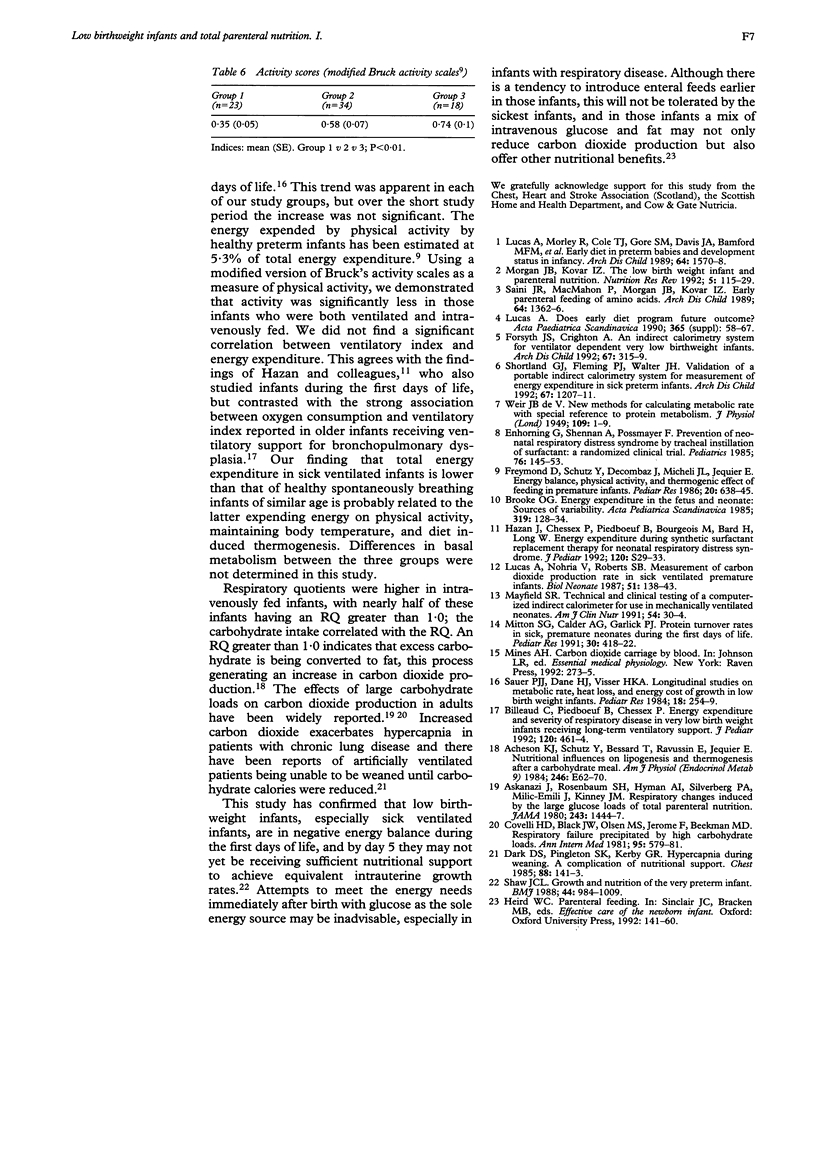
The aim of this study was to determine the energy expenditure and respiratory quotient (RQ) of ventilated and non-ventilated low birthweight infants during the first five days of life, in order to determine optimal feeding regimens. Eighty six infants, of birthweight less than 1750 g, were grouped according to whether they were artificially ventilated or breathing air spontaneously, and whether they were parenterally or enterally fed at the time of study. Energy expenditure and respiratory quotient were measured during days 1-5 and the relation of energy expenditure to several explanatory variables was investigated using multiple regression analysis. The energy expenditure of ventilated infants was less than that of spontaneously breathing infants; the differences were significant on days 1-3. The respiratory quotient (mean (SE)) was greater in intravenously fed infants compared with milk-fed--0.99 (0.03) v 0.92 (0.01) (P < 0.05), with 42% of studies of infants receiving total parenteral nutrition (TPN) producing an RQ of > 1.0 compared with 16.6% of milk-fed infants (P < 0.01). There was a significant correlation between glucose intake and RQ (r = 0.39, P < 0.001). The activity scores were measured during 75 studies and scores were significantly higher in spontaneously breathing milk-fed infants compared with ventilated parenterally fed infants. Factors independently related to energy expenditure were: postnatal age (P < 0.01); milk feeds (P < 0.01); and physical activity (P < 0.05). A mix of carbohydrate and fat from day 1 may not only meet energy needs but may also reduce respiratory quotient.
Full text
PDF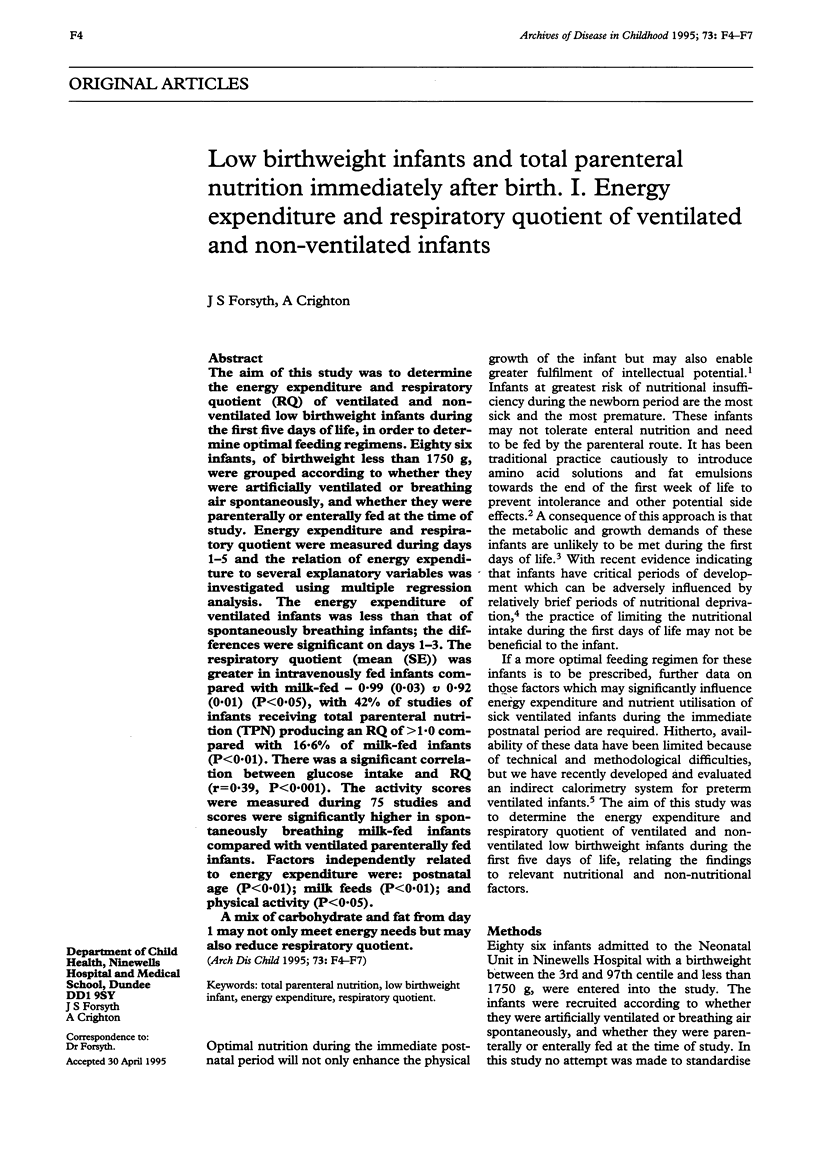

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Askanazi J., Rosenbaum S. H., Hyman A. I., Silverberg P. A., Milic-Emili J., Kinney J. M. Respiratory changes induced by the large glucose loads of total parenteral nutrition. JAMA. 1980 Apr 11;243(14):1444–1447. [PubMed] [Google Scholar]
- Billeaud C., Piedboeuf B., Chessex P. Energy expenditure and severity of respiratory disease in very low birth weight infants receiving long-term ventilatory support. J Pediatr. 1992 Mar;120(3):461–464. doi: 10.1016/s0022-3476(05)80921-7. [DOI] [PubMed] [Google Scholar]
- Brooke O. G. Energy expenditure in the fetus and neonate: sources of variability. Acta Paediatr Scand Suppl. 1985;319:128–134. doi: 10.1111/j.1651-2227.1985.tb10122.x. [DOI] [PubMed] [Google Scholar]
- Covelli H. D., Black J. W., Olsen M. S., Beekman J. F. Respiratory failure precipitated by high carbohydrate loads. Ann Intern Med. 1981 Nov;95(5):579–581. doi: 10.7326/0003-4819-95-5-579. [DOI] [PubMed] [Google Scholar]
- Dark D. S., Pingleton S. K., Kerby G. R. Hypercapnia during weaning. A complication of nutritional support. Chest. 1985 Jul;88(1):141–143. doi: 10.1378/chest.88.1.141. [DOI] [PubMed] [Google Scholar]
- Enhorning G., Shennan A., Possmayer F., Dunn M., Chen C. P., Milligan J. Prevention of neonatal respiratory distress syndrome by tracheal instillation of surfactant: a randomized clinical trial. Pediatrics. 1985 Aug;76(2):145–153. [PubMed] [Google Scholar]
- Forsyth J. S., Crighton A. An indirect calorimetry system for ventilator dependent very low birthweight infants. Arch Dis Child. 1992 Mar;67(3):315–319. doi: 10.1136/adc.67.3.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freymond D., Schutz Y., Decombaz J., Micheli J. L., Jéquier E. Energy balance, physical activity, and thermogenic effect of feeding in premature infants. Pediatr Res. 1986 Jul;20(7):638–645. doi: 10.1203/00006450-198607000-00012. [DOI] [PubMed] [Google Scholar]
- Hazan J., Chessex P., Piedboeuf B., Bourgeois M., Bard H., Long W. Energy expenditure during synthetic surfactant replacement therapy for neonatal respiratory distress syndrome. J Pediatr. 1992 Feb;120(2 Pt 2):S29–S33. doi: 10.1016/s0022-3476(05)81230-2. [DOI] [PubMed] [Google Scholar]
- Lucas A. Does early diet program future outcome? Acta Paediatr Scand Suppl. 1990;365:58–67. doi: 10.1111/j.1651-2227.1990.tb11584.x. [DOI] [PubMed] [Google Scholar]
- Lucas A., Morley R., Cole T. J., Gore S. M., Davis J. A., Bamford M. F., Dossetor J. F. Early diet in preterm babies and developmental status in infancy. Arch Dis Child. 1989 Nov;64(11):1570–1578. doi: 10.1136/adc.64.11.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas A., Nohria V., Roberts S. B. Measurement of carbon dioxide production rate in sick ventilated premature infants. Biol Neonate. 1987;51(3):138–143. doi: 10.1159/000242644. [DOI] [PubMed] [Google Scholar]
- Saini J., MacMahon P., Morgan J. B., Kovar I. Z. Early parenteral feeding of amino acids. Arch Dis Child. 1989 Oct;64(10 Spec No):1362–1366. doi: 10.1136/adc.64.10_spec_no.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauer P. J., Dane H. J., Visser H. K. Longitudinal studies on metabolic rate, heat loss, and energy cost of growth in low birth weight infants. Pediatr Res. 1984 Mar;18(3):254–259. doi: 10.1203/00006450-198403000-00007. [DOI] [PubMed] [Google Scholar]
- Shaw J. C. Growth and nutrition of the very preterm infant. Br Med Bull. 1988 Oct;44(4):984–1009. doi: 10.1093/oxfordjournals.bmb.a072305. [DOI] [PubMed] [Google Scholar]
- Shortland G. J., Fleming P. J., Walter J. H. Validation of a portable indirect calorimetry system for measurement of energy expenditure in sick preterm infants. Arch Dis Child. 1992 Oct;67(10 Spec No):1207–1211. doi: 10.1136/adc.67.10_spec_no.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]


