Abstract
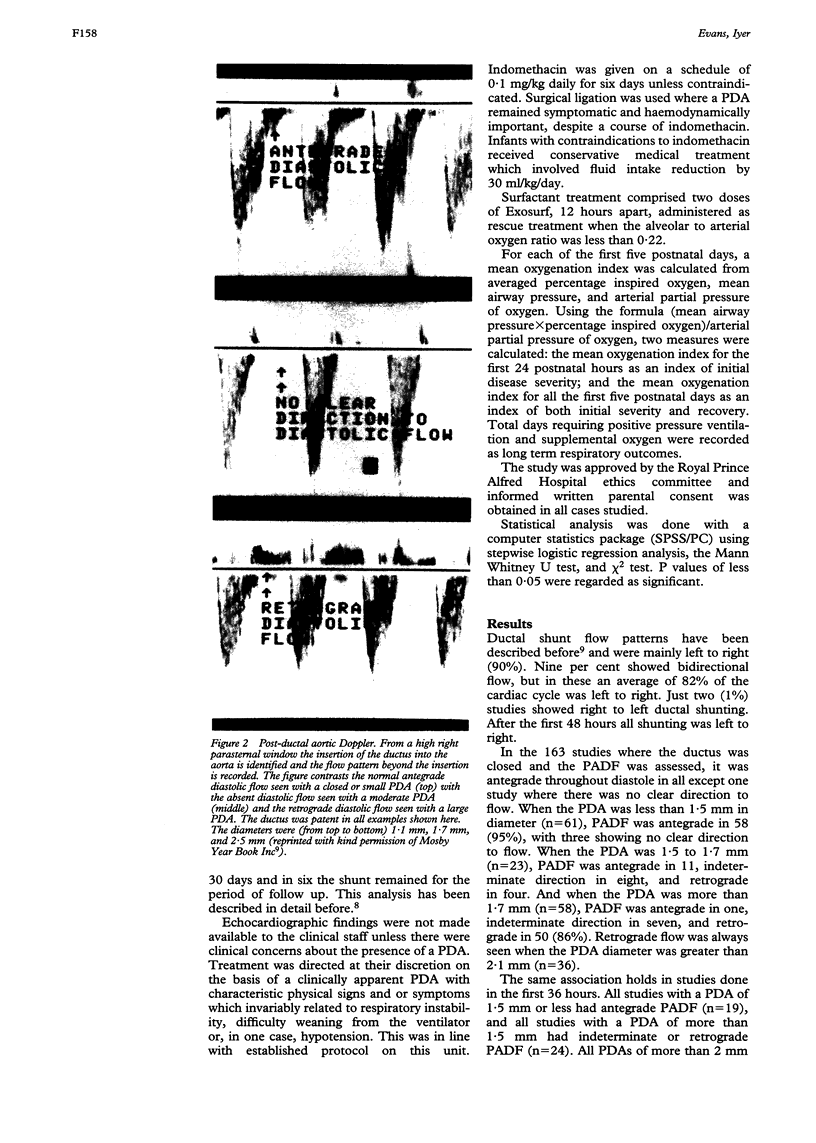
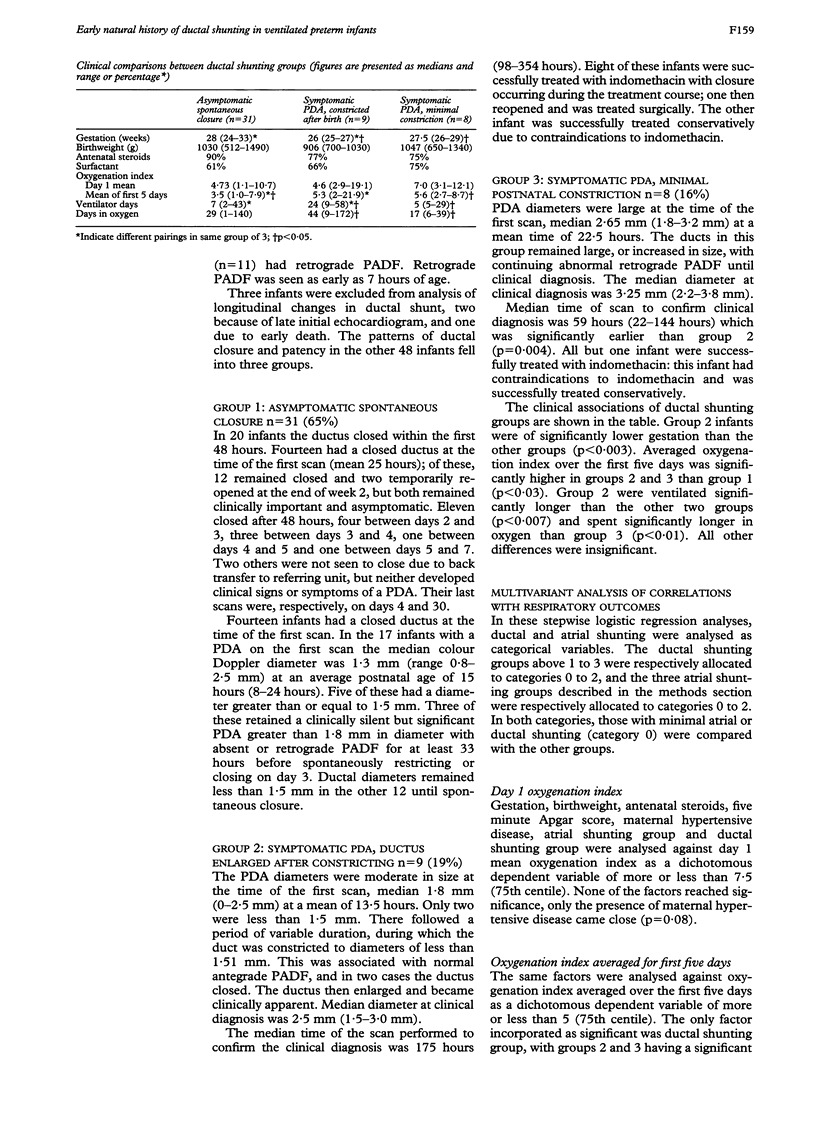
This study aimed to examine the early natural history of ductal shunting in ventilated preterm infants (< 1500 g) and to document the association between this shunting and respiratory outcomes. The size of the ductal shunt was assessed in 48 infants using serial echocardiographic measurement of colour Doppler internal ductal diameter and pulsed Doppler postductal aortic diastolic flow (PADF). At all postnatal ages, normal antegrade PADF was invariably seen when the ductal diameter was 1.5 mm or less, and was usually abnormal (absent or retrograde) when more than 1.5 mm. Longitudinal progress of ductal diameter fell into three groups: (i) asymptomatic spontaneous closure (n = 31)--in 20 of these infants closure occurred within 48 hours; (ii) symptomatic PDA which enlarged after a postnatal constriction (n = 9); and (iii) symptomatic PDA that showed minimal postnatal constriction (n = 8). Infants in group 2 were significantly less mature and had PDAs which became symptomatic significantly later than those in group 3. Logistic regression showed that ductal shunting had a significant correlation with mean oxygenation index over the first five days but not with ventilator or oxygen days. Gestation had the most significant association with the latter two variables, with atrial shunting also being related to days in oxygen. The preterm duct displays a wide spectrum of postnatal constrictive activity. Symptomatic PDAs usually showed slower early postnatal constriction. Ductal shunting independently related to short term but not long term respiratory outcomes.
Full text
PDF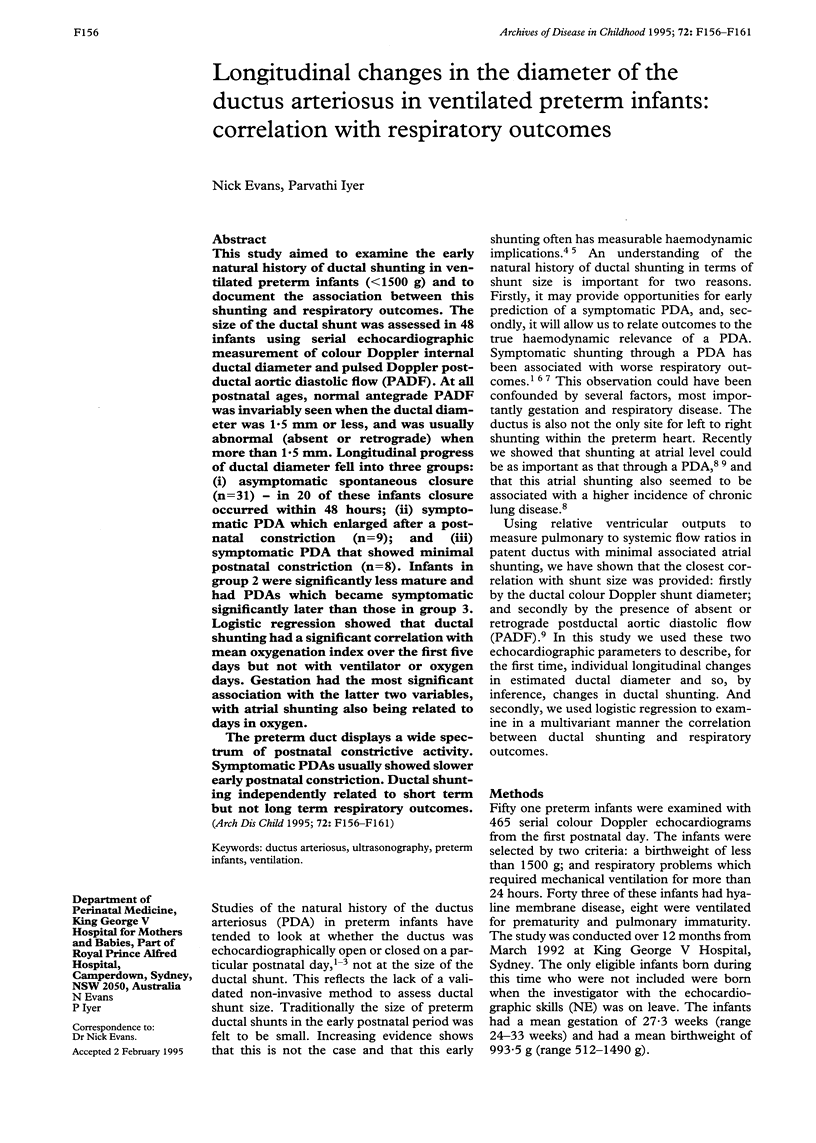
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bandstra E. S., Montalvo B. M., Goldberg R. N., Pacheco I., Ferrer P. L., Flynn J., Gregorios J. B., Bancalari E. Prophylactic indomethacin for prevention of intraventricular hemorrhage in premature infants. Pediatrics. 1988 Oct;82(4):533–542. [PubMed] [Google Scholar]
- Brown E. R. Increased risk of bronchopulmonary dysplasia in infants with patent ductus arteriosus. J Pediatr. 1979 Nov;95(5 Pt 2):865–866. doi: 10.1016/s0022-3476(79)80454-0. [DOI] [PubMed] [Google Scholar]
- Clyman R. I., Ballard P. L., Sniderman S., Ballard R. A., Roth R., Heymann M. A., Granberg J. P. Prenatal administration of betamethasone for prevention of patient ductus arteriosus. J Pediatr. 1981 Jan;98(1):123–126. doi: 10.1016/s0022-3476(81)80557-4. [DOI] [PubMed] [Google Scholar]
- Dudell G. G., Gersony W. M. Patent ductus arteriosus in neonates with severe respiratory disease. J Pediatr. 1984 Jun;104(6):915–920. doi: 10.1016/s0022-3476(84)80499-0. [DOI] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Doppler assessment of pulmonary artery pressure and extrapulmonary shunting in the acute phase of hyaline membrane disease. Arch Dis Child. 1991 Jan;66(1 Spec No):6–11. doi: 10.1136/adc.66.1_spec_no.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Postnatal circulatory adaptation in healthy term and preterm neonates. Arch Dis Child. 1990 Jan;65(1 Spec No):24–26. doi: 10.1136/adc.65.1_spec_no.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N., Iyer P. Assessment of ductus arteriosus shunt in preterm infants supported by mechanical ventilation: effect of interatrial shunting. J Pediatr. 1994 Nov;125(5 Pt 1):778–785. doi: 10.1016/s0022-3476(94)70078-8. [DOI] [PubMed] [Google Scholar]
- Evans N., Iyer P. Incompetence of the foramen ovale in preterm infants supported by mechanical ventilation. J Pediatr. 1994 Nov;125(5 Pt 1):786–792. doi: 10.1016/s0022-3476(94)70079-6. [DOI] [PubMed] [Google Scholar]
- Evans N., Moorcraft J. Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child. 1992 Oct;67(10 Spec No):1169–1173. doi: 10.1136/adc.67.10_spec_no.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt T., Bancalari E. Lung compliance in newborns with patent ductus arteriosus before and after surgical ligation. Biol Neonate. 1980;38(1-2):96–105. doi: 10.1159/000241348. [DOI] [PubMed] [Google Scholar]
- Hammerman C., Strates E., Valaitis S. The silent ductus: its precursors and its aftermath. Pediatr Cardiol. 1986;7(3):121–127. doi: 10.1007/BF02424985. [DOI] [PubMed] [Google Scholar]
- Hornberger L. K., Sahn D. J., Krabill K. A., Sherman F. S., Swensson R. E., Pesonen E., Hagen-Ansert S., Chung K. J. Elucidation of the natural history of ventricular septal defects by serial Doppler color flow mapping studies. J Am Coll Cardiol. 1989 Apr;13(5):1111–1118. doi: 10.1016/0735-1097(89)90270-2. [DOI] [PubMed] [Google Scholar]
- Ikegami M., Jacobs H., Jobe A. Surfactant function in respiratory distress syndrome. J Pediatr. 1983 Mar;102(3):443–447. doi: 10.1016/s0022-3476(83)80673-8. [DOI] [PubMed] [Google Scholar]
- Jacob J., Gluck L., DiSessa T., Edwards D., Kulovich M., Kurlinski J., Merritt T. A., Friedman W. F. The contribution of PDA in the neonate with severe RDS. J Pediatr. 1980 Jan;96(1):79–87. doi: 10.1016/s0022-3476(80)80336-2. [DOI] [PubMed] [Google Scholar]
- Jefferies A. L., Coates G., O'Brodovich H. Pulmonary epithelial permeability in hyaline-membrane disease. N Engl J Med. 1984 Oct 25;311(17):1075–1080. doi: 10.1056/NEJM198410253111703. [DOI] [PubMed] [Google Scholar]
- Knight D. B. Patent ductus arteriosus: how important to which babies? Early Hum Dev. 1992 Jun-Jul;29(1-3):287–292. doi: 10.1016/0378-3782(92)90179-k. [DOI] [PubMed] [Google Scholar]
- Krueger E., Mellander M., Bratton D., Cotton R. Prevention of symptomatic patent ductus arteriosus with a single dose of indomethacin. J Pediatr. 1987 Nov;111(5):749–754. doi: 10.1016/s0022-3476(87)80262-7. [DOI] [PubMed] [Google Scholar]
- Mellander M., Larsson L. E., Ekström-Jodal B., Sabel K. G. Prediction of symptomatic patent ductus arteriosus in preterm infants using Doppler and M-mode echocardiography. Acta Paediatr Scand. 1987 Jul;76(4):553–559. doi: 10.1111/j.1651-2227.1987.tb10520.x. [DOI] [PubMed] [Google Scholar]
- Ment L. R., Oh W., Ehrenkranz R. A., Philip A. G., Vohr B., Allan W., Duncan C. C., Scott D. T., Taylor K. J., Katz K. H. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics. 1994 Apr;93(4):543–550. [PubMed] [Google Scholar]
- Reller M. D., Colasurdo M. A., Rice M. J., McDonald R. W. The timing of spontaneous closure of the ductus arteriosus in infants with respiratory distress syndrome. Am J Cardiol. 1990 Jul 1;66(1):75–78. doi: 10.1016/0002-9149(90)90739-n. [DOI] [PubMed] [Google Scholar]
- Reller M. D., Lorenz J. M., Kotagal U. R., Meyer R. A., Kaplan S. Hemodynamically significant PDA: an echocardiographic and clinical assessment of incidence, natural history, and outcome in very low birth weight infants maintained in negative fluid balance. Pediatr Cardiol. 1985;6(1):17–23. doi: 10.1007/BF02265403. [DOI] [PubMed] [Google Scholar]
- Reller M. D., Ziegler M. L., Rice M. J., Solin R. C., McDonald R. W. Duration of ductal shunting in healthy preterm infants: an echocardiographic color flow Doppler study. J Pediatr. 1988 Mar;112(3):441–446. doi: 10.1016/s0022-3476(88)80333-0. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Kim D. H., Ebrahimi M., Siassi B. Pulsed Doppler measurement of left ventricular output as early predictor of symptomatic patent ductus arteriosus in very preterm infants. Biol Neonate. 1989;56(3):121–128. doi: 10.1159/000243112. [DOI] [PubMed] [Google Scholar]