Abstract
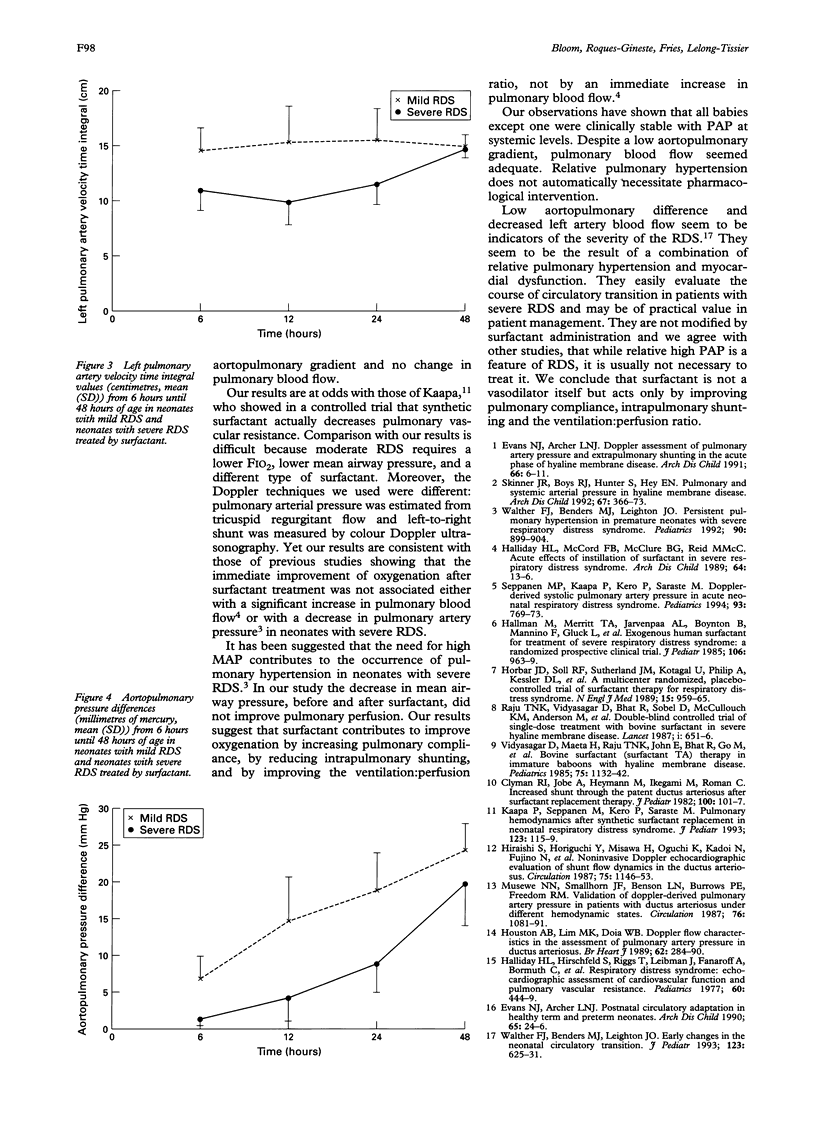
Aortopulmonary pressure difference and pulmonary blood flow velocity were studied during the first 48 hours of life in 12 premature neonates with severe respiratory distress syndrome (RDS), treated by natural surfactant, and in 25 premature neonates with mild RDS. A non-invasive Doppler ultrasound method was used to estimate aortopulmonary pressure difference and pulmonary blood flow velocity from the left pulmonary artery. Aortopulmonary pressure difference was significantly lower at 6 hours of age in the infants with severe RDS and was not increased one hour after surfactant therapy. Aortopulmonary gradient started to rise at 24 hours of age and was equal to that of neonates with mild RDS at 48 hours. Pulmonary blood flow velocity was significantly lower, initially in the severe RDS group, and was not increased one hour after surfactant therapy. Left pulmonary artery flow velocity began to rise after 24 hours and reached the values of the mild RDS group at 48 hours. These data indicate that aortopulmonary pressure difference and pulmonary blood flow are low in the acute phase of RDS and that surfactant treatment does not seem to affect these values.
Full text
PDF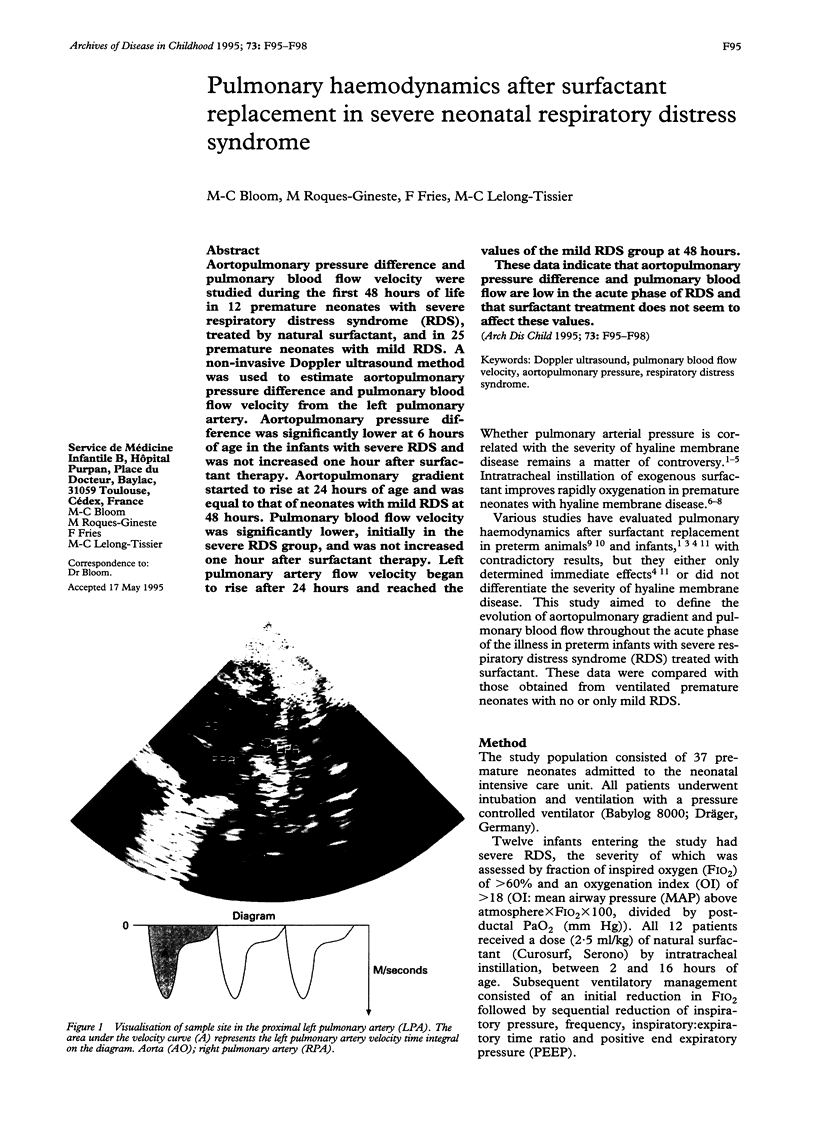


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Clyman R. I., Jobe A., Heymann M., Ikegami M., Roman C., Payne B., Mauray F. Increased shunt through the patent ductus arteriosus after surfactant replacement therapy. J Pediatr. 1982 Jan;100(1):101–107. doi: 10.1016/s0022-3476(82)80247-3. [DOI] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Doppler assessment of pulmonary artery pressure and extrapulmonary shunting in the acute phase of hyaline membrane disease. Arch Dis Child. 1991 Jan;66(1 Spec No):6–11. doi: 10.1136/adc.66.1_spec_no.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans N. J., Archer L. N. Postnatal circulatory adaptation in healthy term and preterm neonates. Arch Dis Child. 1990 Jan;65(1 Spec No):24–26. doi: 10.1136/adc.65.1_spec_no.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliday H., Hirschfeld S., Riggs T., Liebman J., Fanaroff A., Bormuth C. Respiratory distress syndrome: echocardiographic assessment of cardiovascular function and pulmonary vascular resistance. Pediatrics. 1977 Oct;60(4):444–449. [PubMed] [Google Scholar]
- Hallman M., Merritt T. A., Jarvenpaa A. L., Boynton B., Mannino F., Gluck L., Moore T., Edwards D. Exogenous human surfactant for treatment of severe respiratory distress syndrome: a randomized prospective clinical trial. J Pediatr. 1985 Jun;106(6):963–969. doi: 10.1016/s0022-3476(85)80253-5. [DOI] [PubMed] [Google Scholar]
- Hiraishi S., Horiguchi Y., Misawa H., Oguchi K., Kadoi N., Fujino N., Yashiro K. Noninvasive Doppler echocardiographic evaluation of shunt flow dynamics of the ductus arteriosus. Circulation. 1987 Jun;75(6):1146–1153. doi: 10.1161/01.cir.75.6.1146. [DOI] [PubMed] [Google Scholar]
- Horbar J. D., Soll R. F., Sutherland J. M., Kotagal U., Philip A. G., Kessler D. L., Little G. A., Edwards W. H., Vidyasagar D., Raju T. N. A multicenter randomized, placebo-controlled trial of surfactant therapy for respiratory distress syndrome. N Engl J Med. 1989 Apr 13;320(15):959–965. doi: 10.1056/NEJM198904133201502. [DOI] [PubMed] [Google Scholar]
- Houston A. B., Lim M. K., Doig W. B., Gnanapragasam J., Coleman E. N., Jamieson M. P., Pollock J. C. Doppler flow characteristics in the assessment of pulmonary artery pressure in ductus arteriosus. Br Heart J. 1989 Oct;62(4):284–290. doi: 10.1136/hrt.62.4.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Käpä P., Seppänen M., Kero P., Saraste M. Pulmonary hemodynamics after synthetic surfactant replacement in neonatal respiratory distress syndrome. J Pediatr. 1993 Jul;123(1):115–119. doi: 10.1016/s0022-3476(05)81553-7. [DOI] [PubMed] [Google Scholar]
- Musewe N. N., Smallhorn J. F., Benson L. N., Burrows P. E., Freedom R. M. Validation of Doppler-derived pulmonary arterial pressure in patients with ductus arteriosus under different hemodynamic states. Circulation. 1987 Nov;76(5):1081–1091. doi: 10.1161/01.cir.76.5.1081. [DOI] [PubMed] [Google Scholar]
- Raju T. N., Vidyasagar D., Bhat R., Sobel D., McCulloch K. M., Anderson M., Maeta H., Levy P. S., Furner S. Double-blind controlled trial of single-dose treatment with bovine surfactant in severe hyaline membrane disease. Lancet. 1987 Mar 21;1(8534):651–656. doi: 10.1016/s0140-6736(87)90414-4. [DOI] [PubMed] [Google Scholar]
- Seppänen M. P., Käpä P. O., Kero P. O., Saraste M. Doppler-derived systolic pulmonary artery pressure in acute neonatal respiratory distress syndrome. Pediatrics. 1994 May;93(5):769–773. [PubMed] [Google Scholar]
- Skinner J. R., Boys R. J., Hunter S., Hey E. N. Pulmonary and systemic arterial pressure in hyaline membrane disease. Arch Dis Child. 1992 Apr;67(4 Spec No):366–373. doi: 10.1136/adc.67.4_spec_no.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidyasagar D., Maeta H., Raju T. N., John E., Bhat R., Go M., Dahiya U., Roberson Y., Yamin A., Narula A. Bovine surfactant (surfactant TA) therapy in immature baboons with hyaline membrane disease. Pediatrics. 1985 Jun;75(6):1132–1142. [PubMed] [Google Scholar]
- Walther F. J., Benders M. J., Leighton J. O. Early changes in the neonatal circulatory transition. J Pediatr. 1993 Oct;123(4):625–632. doi: 10.1016/s0022-3476(05)80966-7. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Benders M. J., Leighton J. O. Persistent pulmonary hypertension in premature neonates with severe respiratory distress syndrome. Pediatrics. 1992 Dec;90(6):899–904. [PubMed] [Google Scholar]