Abstract
BACKGROUND
Adults discharged from hospital on a Friday are more likely to be readmitted within 30 days than are adults discharged midweek. No study has examined readmission rates for children by day of discharge.
OBJECTIVE
To determine the risk of readmission within 30 days by day of discharge in the paediatric population.
METHODS
The Canadian Institute for Health Information provided data on children 29 days to 18 years of age who were discharged from hospitals in Ontario between January 1996 and December 2000. Two groups of children (those who were readmitted within 30 days and those who were not) were compared on demographic and clinical characteristics. Multivariable modelling was used to account for potential confounding variables: age, sex, length of hospital stay, number of diagnoses, in-hospital operative procedure, in-hospital complication and hospital admission in the previous six months.
RESULTS
A total of 506,035 hospitalizations (involving 334,959 children) occurred over the study period. Of these children, 3.4% were readmitted within 30 days of discharge. In total, 3.6% of children discharged on a Friday were readmitted within 30 days compared with 3.3% of children discharged on a Wednesday. After adjusting for patient and hospital factors, Friday discharge was not associated with readmission within 30 days (adjusted RR 1.07, 95% CI 0.99 to 1.15). More significant predictors of readmission included number of diagnoses, in-hospital complications and hospital admission in the six months previous to the index admission date.
CONCLUSION
Risk of readmission within 30 days is not significantly increased for children discharged on a Friday compared with children discharged midweek. Significant risk factors for hospital readmission are patient complexity and disease severity.
Keywords: Hospital, Paediatric, Patient discharge, Patient readmission, Risk factors
Abstract
HISTORIQUE
Les adultes qui reçoivent leur congé de l’hôpital un vendredi sont plus susceptibles d’être réhospitalisés dans les 30 jours que ceux qui obtiennent leur congé en milieu de semaine. Aucune étude n’a traité des taux de réhospitalisation des enfants selon leur jour de congé.
OBJECTIF
Déterminer le risque de réhospitalisation dans les 30 jours d’après le jour de congé au sein de la population pédiatrique.
MÉTHODOLOGIE
L’Institut canadien d’information sur la santé a fourni des données sur des enfants de 29 jours à 18 ans qui avaient obtenu leur congé d’hôpitaux ontariens entre janvier 1996 et décembre 2000. Deux groupes d’enfants (ceux qui avaient été réhospitalisés dans un délai de 30 jours et ceux qui ne l’avaient pas été) ont été comparés selon des caractéristiques démographiques et cliniques. La modélisation multivariable a permis de tenir compte des variables confusionnelles potentielles : l’âge, le sexe, la durée d’hospitalisation, le nombre de diagnostics, les interventions opératoires et les complications en milieu hospitalier, ainsi que les hospitalisations au cours des six mois précédents.
RÉSULTATS
Un total de 506 035 hospitalisations (de 334 959 enfants) a été enregistré pendant la période de l’étude. De ce nombre, 3,4 % d’enfants ont été réhospitalisés dans les 30 jours suivant leur congé. Au total, 3,6 % des enfants ayant obtenu un congé un vendredi ont été réhospitalisés dans les 30 jours suivant leur congé, par rapport à 3,3 % de ceux l’ayant obtenu un mercredi. Après rajustement compte tenu des facteurs reliés au patient et à l’hôpital, les congés du vendredi ne s’associaient pas à une réhospitalisation dans un délai de 30 jours (RR rajusté 1,07, 95 % IC 0,99 à 1,15). Les principaux prédicteurs de réhospitalisation sont le nombre de diagnostics, les complications en milieu hospitalier et les hospitalisations dans les six mois précédant la date d’admission à l’étude.
CONCLUSION
Le risque de réhospitalisation dans les 30 jours n’augmente pas de manière significative lorsque les enfants obtiennent leur congé un vendredi plutôt qu’en milieu de semaine. Les principaux facteurs de risque de réhospitalisation sont la complexité du cas et la gravité de la maladie.
A study by van Walraven and Bell (1) showed that adult patients discharged from hospital on a Friday were more likely to be readmitted or to die within 30 days following discharge, compared with patients discharged midweek. Hypothesized explanations included premature discharge (ie, before the patient was medically stable), incomplete discharge preparation and delays in the implementation of social services for patients discharged on a Friday (1).
Paediatric research on this topic has focused on the association between brief maternal postpartum stay and readmission rates in neonates (2). To our knowledge, no study has addressed readmission rates for children by day of discharge. Furthermore, results from adult studies may not be generalizable to children. For example, it has been shown that only one-third of adult patients are able to name an informal caregiver on discharge (3). Children, however, are always sent home with a parent or guardian, whose continuing care at home may provide an effective transition from hospital discharge to complete recovery. Qualitative research has also suggested that supportive relationships between patients and their informal caregivers (usually family members) decrease the rate of unplanned readmission (3).
We hypothesized that the increased risk of readmission associated with a Friday discharge (compared with a Wednesday discharge) in adults would not be replicated in the paediatric population. Therefore, the objective of the present study was to examine the risk of hospital readmission by day of discharge in children.
METHODS
Data were obtained from the Canadian Institute for Health Information (CIHI) Discharge Abstract Database (DAD). This database contains demographic and clinical information on all hospital admissions in the province of Ontario. The data are entered by trained coders using standard CIHI definitions. Patient diagnoses in DAD are coded according to the ninth revision of the International Classification of Diseases (ICD-9). In-hospital procedures are coded using the Classification of Diagnostic, Therapeutic and Surgical Procedures developed by Statistics Canada (4).
All children, 29 days to 18 years of age inclusive, who were discharged from an acute care hospital in Ontario between January 1996 and December 2000 were included in the study. Only acute care facilities were included; in accordance with CIHI’s classification system, children admitted to chronic care facilities or psychiatric institutions, as well as those admitted for day surgeries, general rehabilitation, organized outpatient visits, special disability services or whose facility was unclassified, were excluded. Children with ICD-9 V codes were also excluded because these codes represent planned admissions for a specific treatment, such as chemotherapy or dialysis. Neonates were excluded because of unique factors that may influence readmission, such as maternal health, length of postpartum stay and gestational age.
Over the five-year study period, 334,959 children had 506,035 hospital admissions in Ontario. One admission per patient was randomly selected and prospectively followed for a subsequent admission. Patients were then categorized into two groups, according to whether they were readmitted within 30 days of discharge. Children with a readmission within 30 days of discharge were compared with all other children (those who were readmitted more than 30 days following discharge and those with only one admission over the study period) by day of discharge, and on demographic and clinical factors.
For the primary analysis, Friday discharge was considered the ‘exposure’, with Wednesday discharge (ie, midweek) used as the reference day. The adult study (1) on this topic used the same exposure and reference days. Potential risk factors for hospital readmission included age (measured as a continuous variable), sex, number of diagnoses (greater than one versus one), length of hospital stay (two days or longer versus less than two days), operative procedure (yes versus no), in-hospital complication (yes versus no), and one or more hospital admission in the six months before the index admission (yes versus no).
The relative risk (RR) of readmission by day of discharge (Friday versus Wednesday) was estimated along with the 95% CI. Potential confounding variables (see above) were taken into account using multivariable logistic regression modelling. The adjusted odds ratio estimates provided by logistic regression were considered to approximate relative risks, given the large sample size and infrequent event rate (ie, readmission within 30 days) (5).
Secondary analyses estimated the adjusted RR of readmission within 30 days for all other days, using Wednesday as the reference day. In addition, a subgroup analysis was conducted on the five most common diagnoses (grouped by three-digit ICD-9 codes). SAS software (SAS Institute, USA) was used for all statistical analyses.
The study was approved by The Hospital for Sick Children Research Ethics Board (Toronto, Ontario).
RESULTS
Of the 334,959 children, 11,228 (3.4%) were readmitted within 30 days of discharge; the median time to readmission in this group was eight days (interquartile range three to 17 days). Another 32,034 children (9.6%) were readmitted more than 30 days after discharge (median time to readmission 255 days, interquartile range 105 to 526 days). The majority of children (n=291,697 [87.1%]) did not have a readmission over the study period.
Simple univariate analyses are shown in Table 1. The two groups of children (readmission within 30 days of discharge or not) were similar with respect to age and sex. These unadjusted analyses suggested that children who were readmitted within 30 days of discharge were more likely to have more than one diagnosis, a longer hospital stay, an in-hospital complication or a hospital admission within the previous six months. They were less likely to have had an operative procedure.
TABLE 1.
Patient and hospital admission factors for children 29 days to 18 years of age discharged from Ontario hospitals between January 1996 and December 2000
| Factor | Readmission within 30 days of discharge (n=11,228) | No readmission within 30 days of discharge (n=323,731) |
|---|---|---|
| Patient | ||
| Median age, years (interquartile range) | 6 (1 to 15) | 6 (2 to 14) |
| Male, n (%) | 5640 (50) | 170,207 (53) |
| More than one diagnosis, n (%) | 5849 (52) | 137,859 (43) |
| Hospital admission | ||
| Length of stay two days or longer, n (%) | 7289 (65) | 185,664 (57) |
| Procedure during stay, n (%) | 2162 (19) | 106,503 (33) |
| In-hospital complication, n (%) | 608 (5) | 11,170 (3) |
| Hospital admission within six months before index admission, n (%) | 2924 (26) | 20,969 (6) |
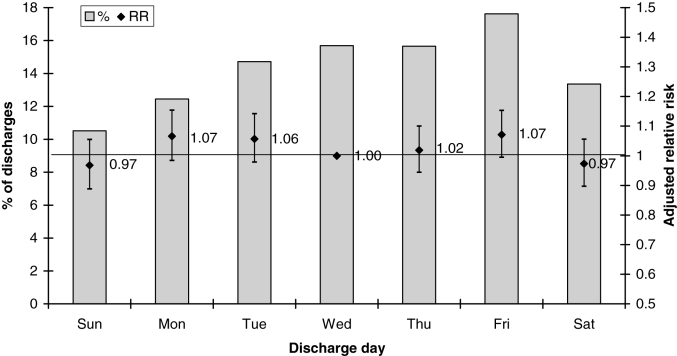
As shown in Figure 1, Friday was the most common day for discharge (17.6%). In total, 3.6% of children discharged on a Friday were readmitted within 30 days of discharge, compared with 3.3% of children discharged on a Wednesday (RR 1.09, 95% CI 1.03 to 1.17). After controlling for potential confounding variables (age, sex, number of diagnoses, length of hospital stay, operative procedure, in-hospital complication and admission in the previous six months), the adjusted RR of readmission within 30 days (Friday versus Wednesday) was not statistically significant (adjusted RR 1.07, 95% CI 0.99 to 1.15).
Figure 1.
Percentage of discharges by day of the week, along with adjusted relative risks (RRs) for readmission within 30 days of discharge. Bars indicate per cent of discharges by day of the week. Diamonds and error bars represent RRs with 95% CIs for risk of readmission within 30 days of discharge for each day of the week compared with Wednesday. RRs are adjusted for age, sex, number of diagnoses, length of hospital stay, operative procedure, in-hospital complication and admission in the previous six months
Table 2 shows the results of the multivariable logistic regression, including the adjusted RR of readmission within 30 days of discharge for each variable. Hospital admission within six months before the index admission, an in-hospital complication and more than one diagnosis were the strongest predictors of readmission within 30 days. A procedure during the hospital stay was the strongest protective factor.
TABLE 2.
Adjusted relative risk (RR) of readmission within 30 days of discharge for each factor in the multivariable model
| Factor | Adjusted RR (95% CI) |
|---|---|
| Patient | |
| Age (per one year increasing increment) | 1.03 (1.02 to 1.03) |
| Sex (male versus female) | 0.92 (0.85 to 0.99) |
| Number of diagnoses (more than one versus one) | 1.18 (1.09 to 1.27) |
| Hospital admission | |
| Length of stay (two days or more versus less than two days) | 1.05 (0.97 to 1.13) |
| Procedure during stay (yes versus no) | 0.48 (0.44 to 0.53) |
| In-hospital complication (yes versus no) | 1.43 (1.16 to 1.75) |
| Hospital admission within six months before index admission (yes versus no) | 3.93 (3.58 to 4.30) |
The five most common diagnoses, accounting for 24% of all ‘most responsible’ diagnoses, were asthma, acute bronchitis or bronchiolitis, chronic disease of the tonsils and adenoids, gastroenteritis or colitis, and pneumonia. Analysis of this subset showed similar results, with an adjusted RR of readmission within 30 days of discharge of 1.02 (95% CI 0.88 to 1.19; Friday versus Wednesday).
Adjusted RRs for each day of the week (compared with Wednesday) are presented in Figure 1. No day of the week was associated with a significantly increased or decreased risk of readmission within 30 days.
DISCUSSION
In contrast to van Walraven and Bell’s study in adults (1), the present study showed that children discharged on a Friday did not have a statistically significantly increased risk of hospital readmission within 30 days of discharge. Factors associated with an increased risk of readmission within 30 days included age, more than one discharge diagnosis, an in-hospital complication and a hospitalization within the past six months. Protective factors included male sex and having an operative procedure.
We modelled the present study after a similar one involving an adult population (1). We hypothesized that day of discharge would be less important in children because children go home with a caregiver, thus bridging the transition to home. The point estimates for both the adult study and the present study were greater than 1.0 (1.04 and 1.07, respectively). Only the adult study, however, showed a statistically significant difference in readmission rates between Friday and Wednesday discharges. Differences between the two studies included sample size and confounding variables included in the analysis. For example, the sample size for the present study was smaller than that for the adult study, and this is reflected in wider CIs. In addition, the adult study accounted for more confounding variables than did the present study. Of note, other unmeasured variables, such as parental anxiety and access to a primary care physician, were not included in either analysis. Beyond statistical significance, the issue is whether the finding of an elevated risk of readmission within 30 days for Friday discharges (compared with Wednesday discharges) is clinically important. Although paediatric discharge is common (approximately 100,000 per year) in Ontario, readmission within 30 days is uncommon (3.4%). This is in contrast to the adult study (1), which reported a 5.4% rate of readmission within 30 days of discharge. Therefore, a modest RR (1.07 for Friday versus Wednesday) would translate into relatively few paediatric readmissions within 30 days annually because of Friday discharge.
Important predictors of readmission within 30 days of discharge in the multivariable model included more than one discharge diagnosis, an in-hospital complication and a hospital admission in the previous six months. Strikingly, children with at least one hospital admission in the six months before the index admission were almost four times as likely to be readmitted within 30 days of hospital discharge. These findings emphasize the importance of disease severity and chronicity on successful discharge planning. More complex patients may be more likely to be readmitted within 30 days of discharge simply because of their underlying disease process. In other words, this patient population often requires multidisciplinary care and complex coordination of services at home, which contribute to the challenge of the discharge planning process. Of note, our findings of significant predictors of readmission are similar to those in the adult study (1).
Children who had an operative procedure were less likely to be readmitted within 30 days of discharge than were children whose hospital stay did not include a procedure. In our population, appendectomy and tonsillectomy with ade-noidectomy were the two most common procedures, accounting for 14% of all procedures. Tonsillectomies are often elective, and studies have shown a predictable postoperative course for both of these surgeries (6–8), which usually involve otherwise healthy children. These issues –healthy patients and routine surgery – likely make the discharge planning process a straightforward one. Additionally, when procedures are performed frequently, the organization and teaching around both discharge and follow-up become routine. This may lead to fewer oversights, and perhaps higher patient and parent confidence, ultimately decreasing the rate of unplanned readmissions.
Our finding that Friday was the most common day for discharge is in keeping with the adult literature (1). This is likely attributable to both patient and physician factors. Families often wish to be home for the weekend, and physicians are likely to discharge their patients by the week’s end, in anticipation of handing care over to a different weekend team. Each day of the week carried an approximately equal risk of readmission. This is supportive of our finding that patient factors indicative of complexity and chronicity represent strong risk factors for readmission within 30 days because these factors are unrelated to the day of the week.
Strengths of the present study include population-based data and a large sample size. In addition, Canadian health care administrative databases have been shown to be reliable and valid. For example, studies examining data quality have found high rates of agreement between the medical charts and administrative databases on demographic, diagnostic and procedural information (4). Finally, potential confounding factors were taken into account in the analyses.
Limitations of the study relate to the data source. For example, patient complexity was difficult to measure. To our knowledge, there is no validated score to measure comorbidity in children using administrative data. Therefore, we used the number of diagnoses as a crude marker of patient complexity and the presence of a hospital admission within the previous six months as an indicator of chronicity. In addition, there was no variable for elective admissions. Only acute care admissions, however, were selected, and children with ICD-9 V codes were excluded. Finally, we were unable to examine mortality because the DAD only records in-hospital deaths. Of note, of the 334,959 children in the data set, 1290 patients (0.4%) died during a hospital stay.
CONCLUSION
The risk of readmission within 30 days for children discharged on a Friday, compared with children discharged on a Wednesday, was modestly elevated and not statistically significant. Of note, Friday was the most common discharge day. More important, factors that reflect patient complexity and disease severity were key risk factors for hospital readmission within 30 days. To reduce the risk of readmission for such patients, clinicians need to be cognizant of all patient and hospital factors, and ensure that key continuity of care issues are addressed before hospital discharge.
ACKNOWLEDGEMENTS
Parts of this material are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the authors and not necessarily those of the Canadian Institute for Health Information.
Footnotes
FINANCIAL SUPPORT: Dr Beck is supported through a studentship, fully or in part, by the Ontario Student Opportunity Trust Fund – The Hospital for Sick Children Foundation Student Scholarship Program, and by a Canadian Institutes of Health Research Fellowship. The Paediatric Outcomes Research Team is supported by a grant from The Hospital for Sick Children.
REFERENCES
- 1.van Walraven C, Bell CM. Risk of death or readmission among people discharged from hospital on Fridays. CMAJ. 2002;166:1672–3. [PMC free article] [PubMed] [Google Scholar]
- 2.Liu S, Wen SW, McMillan D, Trouton K, Fowler D, McCourt C. Increased neonatal readmission rate associated with decreased length of hospital stay at birth in Canada. Can J Public Health. 2000;91:46–50. doi: 10.1007/BF03404253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Procter S, Wilcockson J, Pearson P, Allgar V. Going home from hospital: The carer/patient dyad. J Adv Nurs. 2001;35:206–17. doi: 10.1046/j.1365-2648.2001.01838.x. [DOI] [PubMed] [Google Scholar]
- 4.Williams JI, Young W. A summary of studies on the quality of health care administrative databases in Canada. In: Goel V, Williams JI, Anderson GM, Blackstien-Hirsch P, Fooks C, Naylor CD, editors. Patterns of Health Care in Ontario. The ICES Practice Atlas. 2. Ottawa: Canadian Medical Association; 1996. pp. 339–46. [Google Scholar]
- 5.Kleinbaum DG. Logistic Regression. New York: Springer-Verlag; 1994. pp. 15–6. [Google Scholar]
- 6.Fredelius L, Olin AO, Grenroth C, Axelsson G, Hemlin C. Pediatric tonsillectomy can be performed as day surgery. Lakartidningen. 1999;96:194–6. [PubMed] [Google Scholar]
- 7.Lord RV, Sloane DR. Early discharge after open appendicectomy. Aust N Z J Surg. 1996;66:361–5. doi: 10.1111/j.1445-2197.1996.tb01211.x. [DOI] [PubMed] [Google Scholar]
- 8.Velhote CE, de Oliveira Velhote TF, Velhote MC, Moura DC. Early discharge after appendicectomy in children. Eur J Surg. 1999;165:465–7. doi: 10.1080/110241599750006712. [DOI] [PubMed] [Google Scholar]