Abstract
BACKGROUND:
Health care workers have long observed increased rates of hospital admissions for respiratory illness in infants from the northern regions of Canada. Particularly high rates have been reported in the Inuit population. The purpose of the present study was to compare rates of hospital admission in Inuit versus non-Inuit infants from the perspective of a single northern health region.
METHODS:
A retrospective review of all hospital admissions for lower respiratory tract infections (LRTIs) in infants from the Northwest Territories and the Kitikmeot region of Nunavut between 2000 and 2004 was completed and admission rates were compared by health region.
RESULTS:
Hospital admission rates for LRTIs in infants were above the Canadian rate for all regions. The rate of hospital admission for LRTIs in infants from the Kitikmeot region of Nunavut was dramatically high at 590 hospital admissions/1000 live births in the first 12 months of life. The majority of hospitalized infants were previously healthy, non-breastfed term infants with no underlying disease.
INTERPRETATION:
The rate of hospital admission in the Kitikmeot region of Nunavut is the highest reported in the current literature. The reason for such significant morbidity is difficult to explain and raises the question of an underlying predisposition to severe disease in this infant population. The question warrants further study to gain a better understanding of risk factors as well as the role of prevention.
Keywords: Aboriginal, Bronchiolitis, Inuit, Lower respiratory tract infection, Respiratory syncytial virus
Abstract
HISTORIQUE :
Les dispensateurs de soins constatent depuis longtemps une augmentation du taux d’hospitalisation causée par les maladies respiratoires chez les nourrissons du Grand Nord du Canada. On a déclaré un taux particulièrement élevé au sein des populations inuites. La présente étude visait à comparer le taux d’hospitalisation des nourrissons inuits par rapport aux nourrissons non inuits, selon la perspective d’une seule région sanitaire du Grand Nord.
MÉTHODOLOGIE :
Les auteurs ont procédé à une analyse rétrospective de toutes les hospitalisations attribuables à une infection des voies respiratoires inférieures (IVRI) chez les nourrissons des Territoires du Nord-Ouest et de la région du Kitikmeot, au Nunavut, entre 2000 et 2004 et ont comparé les taux d’hospitalisation selon les régions sanitaires.
RÉSULTATS :
Le taux d’hospitalisation attribuable aux IVRI chez les nourrissons était supérieur au taux canadien pour toutes les régions, tandis que chez les nourrissons de la région du Kitikmeot, au Nunavut, il était extrêmement élevé, avec 590 hospitalisations pour 1 000 naissances vivantes au cours des 12 premiers mois de vie. La majorité des nourrissons hospitalisés étaient des bébés à terme non allaités et auparavant en santé, ne présentant pas de maladie sous-jacente.
INTERPRÉTATION :
Le taux d’hospitalisation dans la région du Kitikmeot, au Nunavut, est le plus élevé jamais déclaré dans les publications courantes. Il est difficile d’expliquer la raison d’une telle morbidité, ce qui soulève la possibilité d’une prédisposition sous-jacente à une grave maladie au sein de cette population de nourrissons. Cette question justifie l’approfondissement des recherches pour mieux comprendre les facteurs de risque et le rôle de la prévention.
Health care workers in northern Canada have long observed that infants from the north appear to suffer far more morbidity from respiratory illnesses than infants from southern populations (1,2). A recent Canadian study (3) found that the rate of hospital admission in Canadian infants for bronchiolitis was 60/1000 live births. In comparison, the rates of hospital admission for lower respiratory tract infections (LRTIs) (bronchiolitis and pneumonia) in the United States for the American Indian and Alaska Native infants were notably higher at 116.1/1000 live births versus 63.2/1000 live births compared with the general United States population (4). The RSV Alaska Study Group has reported (5) markedly higher rates of hospital admission for respiratory syncytial virus (RSV) (excluding other causes of bronchiolitis) of up to 249/1000 live births in infants from the Yukon-Kuskokwim Delta region. Investigators from the Baffin region of Nunavut have reported similar high hospital admission rates for bronchiolitis between 197/1000 live births and 484/1000 live births (1,6,7). The Northern Medical Unit from the University of Manitoba (Winnipeg, Manitoba) has made similar observations in the Kivalliq region of Nunavut (8).
Health care workers in the north are also under the impression that Inuit infants, in particular, have more severe LRTIs than infants from other Aboriginal populations (1). There are, however, no comparative studies of the severity of illness in Inuit versus non-Inuit populations from the perspective of a single health region. The purpose of the present study was to report the incidence of LRTI hospital admissions in northern Canadian communities and to compare the incidence in Inuit infants with that of other populations in northern Canada.
METHODS
A retrospective review of all LRTI hospital admissions of infants (up to 12 months of age) from the Northwest Territories (NWT) and the Kitikmeot region of Nunavut from January 1, 2000, to December 31, 2004, was completed. The NWT has a population of approximately 42,000 people living in 33 communities, with approximately 54% of the population being Aboriginal (30% Dene, 10% Inuit and 14% Métis). The Kitikmeot region of Nunavut has a population of approximately 5000 people living in five communities, with approximately 95% being Inuit. Health care services for the NWT and the Kitikmeot region are mainly provided by Stanton Territorial Hospital (Yellowknife, NWT), supplemented by three smaller regional hospitals in Hay River, Fort Smith and Inuvik. This provides an ideal opportunity to compare the hospitalization rates of various populations with similar social, economic and environmental circumstances living in the same region.
The health records databases from Stanton Territorial, Inuvik, Fort Smith and Hay River hospitals were searched for an International Classification of Diseases and Related Health Problems, 9th and 10th Revisions discharge diagnosis of bronchiolitis or a compatible viral LRTI diagnosis. Results were compared against the Canadian Institute for Health Information computerized discharge database to identify cases missed by this search strategy. The charts were reviewed to extract demographic and clinical information including date of birth, community, discharge diagnoses, length of admission, previous admissions, birth weight and gestation, breastfeeding status, household smoking status and any underlying illnesses. Because socioeconomic information was not available on individual patients, these data were obtained on a regional basis from the NWT Bureau of Statistics.
RESULTS
Over the five-year review period, 840 LRTI admissions were identified in 544 patients. The main criteria for admission were hypoxia documented on pulse oximetry, as well as concerns about hydration and feeding or potential respiratory failure. The discharge diagnosis was bronchiolitis in 69% of admissions, with most of the remainder being pneumonia (19%) or respiratory tract infection (9%). The median length of stay was four days.
Fifty-nine per cent of the patients were male and 64% of admissions occurred in the first six months of life. Only 15% of admitted infants were born before 37 weeks gestation, 9% of whom had low birth weight (less than 2500 g), with the majority being healthy term infants with no underlying risk factors or other health problems. Smoking status in the home was not recorded for 98% of admissions. Only 21% of the patients were breastfed at the time of admission.
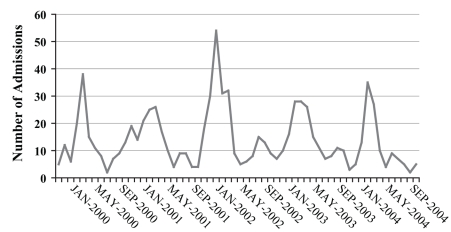
There was a seasonality to the admissions, with a peak occurring between January and May each year for the period reviewed (Figure 1). In most years, this peak corresponded with the peak in RSV activity in the region which tended to be in April or later for most years in which data were available (Government of Northwest Territories, Department of Health, unpublished data). RSV has been a reportable disease in the NWT since 1999, and admitted infants routinely had a nasopharyngeal aspirate sent for viral studies. Despite viral studies being performed on nearly all admitted infants, no pathogen was identified for the majority of patients; although a positive viral swab for RSV was documented in 29% of all admissions.
Figure 1.
Monthly infant admissions for acute respiratory illness in the Northwest Territories and the Kitikmeot region of Nunavut between 2000 and 2004. Jan January; Sep September
Admission rates/1000 live births (with CIs) were recorded by health region (Table 1). Of note is the exceptionally high rate of admission for the Kitikmeot region with 590 admissions/1000 live births. Of the non-Inuit communities, the Tlicho region has a notably high rate of admission at 371/1000 live births.
TABLE 1.
Infant admission rates by health regions between 2000 and 2004 for lower respiratory tract infections/1000 live births
| Health region (territories) | Admissions/1000 live births | CI range |
|---|---|---|
| Hay River/Fort Smith (NWT) | 63 | 41–93 |
| Yellowknife (NWT) | 68 | 56–83 |
| Deh Cho (NWT) | 97 | 63–144 |
| Beaufort-Delta (NWT) | 185 | 155–219 |
| Sahtu (NWT) | 218 | 163–284 |
| Tlicho (NWT) | 371 | 320–425 |
| Kitikmeot (Nunavut) | 590 | 552–627 |
NWT Northwest Territories
Of the patients admitted to hospital during the review, 58 (6.9%) required transfer to the regional tertiary care centre for paediatric intensive care. Of the patients from the Kitikmeot region, nearly 10% of the admissions required paediatric intensive care, representing 70% of the total transfers.
Socioeconomic risk factor data were obtained from the NWT Bureau of Statistics and reported on a regional basis for a single point in time (Table 2).
TABLE 2.
Socioeconomic factors by health region
| Health region (territories) | Total population | Households with six or more persons (%) | High school education or greater (%) | Employment (%) | Average household income ($) | Current smokers (%) | Admission/1000 live births |
|---|---|---|---|---|---|---|---|
| Hay River/Fort Smith (NWT) | 6025 | 5.1 | 66.7 | 69.5 | 66,359 | 36.8 | 63 |
| Yellowknife (NWT) | 17,496 | 4.5 | 75.9 | 79.0 | 85,565 | 32.2 | 68 |
| Deh Cho (NWT) | 2878 | 7.4 | 46.7 | 58.4 | 54,902 | 51.1 | 97 |
| Beaufort-Delta (NWT) | 6210 | 9.8 | 54.9 | 60.6 | 56,640 | 57.6 | 185 |
| Sahtu (NWT) | 2326 | 12.2 | 55.7 | 61.3 | 58,974 | 54.8 | 218 |
| Tlicho (NWT) | 2410 | 26.4 | 30.7 | 44.9 | 49,669 | 49.7 | 371 |
| Kitikmeot (Nunavut) | 4816 | 17.6 | 34.4 | 52.3 | 51,282 | 68.6 | 590 |
DISCUSSION
A five-year retrospective review of all LRTI admissions in the first year of life for the NWT and Kitikmeot region was undertaken to gain a better understanding of the disease characteristics in these regions. Hospital admissions were used as an easily measured clinical end point, as well as a proxy for severity of illness, recognizing that the threshold for admission may vary in different centres. However, the main criterion for admission was hypoxia, defined by an oxygen saturation of less than 92% as measured objectively by pulse oximetry, a tool routinely used in all health centres and hospitals in the region. Median length of admission (four days) was similar to that of 3.1 days reported in a recent Canadian study (3), suggesting that the severity of illness was comparable with that of previous bronchiolitis studies (3).
It is notable that the rates of LRTI admission to hospital for all health regions of the NWT and the Kitikmeot region were generally higher than the overall Canadian rate (3). Inuit infants represented nearly two-thirds of the total admissions and similar proportion of paediatric intensive care unit transfers, although this group accounts for less than one-fifth of the total population. The Inuit population is concentrated in the Kitikmeot region of Nunavut, but also represents a small proportion of the population of the Inuvik region in the NWT. Both of these regions had high rates of admission to hospital but significant variability between the regions (185 admissions/1000 live births versus 590 admissions/1000 live births, respectively). The Tlicho region, which is primarily a First Nations (non-Inuit) population, had the highest rate of hospital admission (371 admissions/1000 live births) in the NWT. The admission rates for the Kitikmeot region are by far the highest rates reported in the literature, including those previously reported from the Inuit population of the Baffin Region (1).
Historically, many infants admitted to hospital for bronchiolitis have one or more risk factors for severe respiratory disease. A Canadian tertiary care study (9) of RSV admissions identified these risks as cardiac disease, chronic lung disease, immunocompromise or other chronic diseases, prematurity (gestation less than 37 weeks), Aboriginal ethnicity and infants younger than six weeks of age. Other risk factors for admission to hospital with RSV have been identified as household or maternal smoking (10), household crowding (10) and lower socioeconomic status (11). The effect of umbilical cord blood RSV neutralizing antibody levels has been inconclusive (10,12). Breastfeeding has been found to be protective in some studies (5,12). In the current study, the vast majority of infants admitted to hospital were healthy, term, non-breastfed infants with no underlying disease.
Because the study was retrospective in design, there was no mechanism to clearly track household and environmental factors for individual patients. Table 2 compares socioeconomic indicators by health region at a point in time during the review period (or before the review period for smoking data). A statistical analysis was not undertaken; however, the health regions with the highest rates of hospitalization tended to have a greater degree of environmental risk, particularly in measures of crowding, employment, education and smoking.
The dramatically high rate of admission for the Kitikmeot region is difficult to explain, although it is reasonably consistent across the five years of the review and comparable with rates reported in previous reports from northern Canada (1,6). Previous studies (13) that examined rates of RSV infection noted that virtually all children had been infected with RSV at least once by 24 months of age. Of those infected infants, 25% to 40% will be symptomatic with 0.5% to 2% requiring hospital admission (14). The difference in this population does not appear to be the rate of infection with RSV or other respiratory pathogens but rather the high rate of hospital admission as a result. It seems unlikely that such dramatically elevated rates of hospital admission could be explained solely on the basis of environmental factors, although it is likely that social and economic factors play a role. With the entire population reviewed living in remote, northern communities, it is striking that the Inuit infants had such significantly elevated rates of hospital admission compared with all other groups in the region. High rates of hospital admission have been reported in Inuit infants from other regions (1,5,6,7) but without the benefit of comparison populations. The present study raises the question as to whether there could be a genetic predisposition to more severe disease in Inuit infants.
The present study has several limitations. The retrospective study design limited the ability to quantify household and environmental factors contributing to the severity of illness and risk for hospitalization. The study was based on hospitalization of infants as an outcome rather than total disease incidence in the population at risk and is, therefore, an underestimate of the total burden of LRTI on the communities and the health care system. On data validation with the Canadian Institute of Health Information database, there was a significant amount of missing data (80 admissions) compared with directly obtaining chart lists from hospital medical records. These admissions were included in the analysis. There were a small number of infants transferred directly from their home community or hospital to the tertiary care centre without a recorded admission in the NWT. In most cases, these admissions were recorded when the infants were repatriated to the NWT for convalescence in hospital before discharge to their home communities.
Future studies should analyze risk factors for LRTI hospitalizations in northern infants. The role of public health campaigns that stress the importance of a nonsmoking environment, hand washing in the home and of ongoing breastfeeding needs to be established. With the highest rates of hospital admissions occurring during the RSV season, a case could be made for a clinical trial of RSV monoclonal antibody in all Inuit infants during the RSV season.
Acknowledgment
The authors would like to thank Dr Joan Robinson, Department of Paediatrics, University of Alberta (Edmonton, Alberta) for her editorial assistance.
Footnotes
DISCLOSURE: Funding for the present study was supported by a research grant from Abbott Pharmaceuticals (USA).
ETHICAL REVIEW: The present study was reviewed and approved by the ethics committee of the Stanton Territorial Health Authority (Yellowknife, Northwest Territories).
REFERENCES
- 1.Banerji A, Bell A, Mills EL, et al. Lower respiratory tract infections in Inuit infants on Baffin Island. CMAJ. 2001;164:1847–50. [PMC free article] [PubMed] [Google Scholar]
- 2.Morrell RE, Marks MI, Champlin R, Spence L. An outbreak of severe pneumonia due to respiratory syncytial virus in isolated Arctic populations. Am J Epidemiol. 1975;101:231–7. doi: 10.1093/oxfordjournals.aje.a112090. [DOI] [PubMed] [Google Scholar]
- 3.Langley JM, LeBlanc JC, Smith B, Wang EE. Increasing incidence of hospitalization for bronchiolitis among Canadian children, 1980–2000. J Infect Dis. 2003;188:1764–7. doi: 10.1086/379740. [DOI] [PubMed] [Google Scholar]
- 4.Peck AJ, Holman RC, Curns AT, et al. Lower respiratory tract infections among american Indian and Alaska Native children and the general population of US Children. Pediatr Infect Dis J. 2005;24:342–51. doi: 10.1097/01.inf.0000157250.95880.91. [DOI] [PubMed] [Google Scholar]
- 5.Karron RA, Singleton RJ, Bulkow L, et al. Severe respiratory syncytial virus disease in Alaska native children. RSV Alaska Study Group. J Pediatr Infect Dis. 1999;180:41–9. doi: 10.1086/314841. [DOI] [PubMed] [Google Scholar]
- 6.Banerji A. High rates of hospitalization for bronchiolitis in Inuit Children on Baffin Island. Int J Circumpolar Health. 2001;60:375–9. [PubMed] [Google Scholar]
- 7.Creery D, Lyer P, Samson L, Coyle D, Osborne G, MacDonald A. Costs associated with infant bronchiolitis in the Baffin region of Nunavut. Int J Circumpolar Health. 2005;64:38–45. doi: 10.3402/ijch.v64i1.17952. [DOI] [PubMed] [Google Scholar]
- 8.Orr P, Mcdonald S, Milley D, Brown R. Bronchiolitis in Inuit children from a Canadian central arctic community, 1995–1996. Int J Circumpolar Health. 2001;60:649–58. [PubMed] [Google Scholar]
- 9.Wang EE, Law BJ, Stephens D. Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr. 1995;126:212–9. doi: 10.1016/s0022-3476(95)70547-3. [DOI] [PubMed] [Google Scholar]
- 10.Bulkow LR, Singleton RJ, Karron RA, Harrison LH Alaska RSV Study Group. Risk factors for severe respiratory syncytial virus infection among Alaska native children. Pediatrics. 2002;109:210–6. doi: 10.1542/peds.109.2.210. [DOI] [PubMed] [Google Scholar]
- 11.Jansson L, Nilsson P, Olsson M. Socioeconomic environmental factors and hospitalization for acute bronchiolitis during infancy. Acta Paediatr. 2002;91:335–8. doi: 10.1080/08035250252834021. [DOI] [PubMed] [Google Scholar]
- 12.Nielsen HE, Siersma V, Andersen S. Respiratory syncytial virus infection – risk factors for hospital admission: A case-control study. Acta Paediatr. 2003;92:1314–21. [PubMed] [Google Scholar]
- 13.Glezen WP, Taber LH, Frank AL, Kasel JA. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;140:543–6. doi: 10.1001/archpedi.1986.02140200053026. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Infectious Diseases, Centers for Disease Control and Prevention. Respiratory syncitial virus. < http://www.cdc.gov/ncidod/dvrd/revb/respiratory/rsvfeat.htm> (Version current at August 16, 2007)
- 15.Stats Link Canada. Canadian census 2001: Historic Canadian demographics. < http://www.stats-link-canada.com/Census-2001.html> (Version current at August 16, 2007)
- 16.NWT Bureau of Statistics. Labour force survey. < http://www.stats.gov.nt.ca/Statinfo/Labour/99LFS/99LFS.html> (Version current at August 16, 2007)