Abstract
BACKGROUND
Pediatric hypertension is a field of increasing interest and importance. Early identification of children at risk for hypertension is important to prevent the serious, long-term complications associated with the condition. In Tunisia, there are no data available on the cardiovascular disease risk profile, such as hypertension, in the population of children.
OBJECTIVE
To establish the prevalence of hypertension, the percentile distribution of blood pressure and the inter-relationships between hypertension and other cardiovascular disease risk factors among school children.
METHODS
An epidemiological survey was conducted based on a representative sample of 1569 urban school children in Sousse, Tunisia.
RESULTS
The prevalence of arterial hypertension was 9.6%, with no significant difference between boys (9.2%) and girls (9.9%). The prevalence of systolic and diastolic hypertension was 6.4% and 4.5%, respectively. In both boys and girls, systolic pressure had a highly significant positive correlation with height (boys: r=0.33, P<0.001; girls: r=0.08, P=0.02), weight (boys: r=0.47, P≤0.001; girls: r=0.35, P<0.001) and triglyceride concentrations (boys: r=0.13, P<0.001; girls: r=0.10, P=0.006). Among boys, a positive correlation was found between systolic blood pressure and age (r=0.12, P=0.001) and, among girls, a negative correlation was found (r=−0.12, P=0.001).
CONCLUSION
This information will be used to help launch a regional program of heart health promotion in schools.
Keywords: CVD risk factor, Epidemiology, Hypertension, Tunisia, Urban school children
Abstract
CONTEXTE
L’hypertension artérielle (HA) chez les enfants est un domaine qui suscite de plus en plus d’intérêt et qui gagne en importance. Le repérage précoce des enfants prédisposés à l’HA est important pour prévenir les complications graves, liées à long terme à la maladie. Il n’existe pas, en Tunisie, de données sur les risques de maladies cardiovasculaires, par exemple l’hypertension artérielle, chez les enfants.
OBJECTIF
Établir la prévalence de l’HA, la distribution en percentiles de la pression artérielle et les liens réciproques entre l’hypertension et les autres facteurs de risque de maladies cardiovasculaires chez les enfants d’âge scolaire.
MÉTHODE
Une enquête épidémiologique a été menée auprès d’un échantillon représentatif d’enfants (n=1569) d’âge scolaire, en milieu urbain, à Sousse, en Tunisie.
RÉSULTATS
La prévalence de l’HA a été établie à 9,6 %, sans différence significative entre les garçons (9,2 %) et les filles (9,9 %). Pour ce qui est de la prévalence de l’HA systolique et de l’HA diastolique, elle était de 6,4 % et de 4,5 % respectivement. La pression systolique était en forte corrélation positive avec la taille (garçons : r=0,33, P<0,001; filles : r=0,08, P=0,02), le poids (garçons : r=0,47, P≤0,001; filles : r=0,35, P<0,001) et le taux de triglycérides (garçons : r=0,13, P<0,001; filles : r=0,10, P=0,006), et ce, tant chez les garçons que chez les filles. Enfin, une corrélation a été observée entre la pression artérielle systolique et l’âge (r=0,12, P=0,001), corrélation positive chez les garçons et négative chez les filles (r=−0,12, P=0,001).
CONCLUSION
Les données recueillies aideront à élaborer un programme régional de promotion de la santé du cœur dans les écoles.
Cardiovascular disease (CVD) is the main cause of death in virtually all industrialized countries (1). It is universally accepted that systemic hypertension is a distinct risk factor for CVDs, especially for coronary artery disease (2,3).
The importance of hypertension in the pediatric population has not been as well appreciated as it has been in adults. This may be due to the much lower prevalence of hypertension in children. Nevertheless, hypertension is an important clinical problem in pediatrics, and the approach to its management differs from that in adults in several major respects (4,5).
Pediatric hypertension is a field of increasing interest and importance. Early identification of children at risk for hypertension, proper evaluation and appropriate management are important to prevent the serious, long-term complications associated with the condition (6–9).
Tunisia is now facing the epidemiological transition phenomenon (10), with an increase in chronic, noncommunicable diseases such as diabetes, cancer and hypertension (11,12). There are no data available on the CVD risk profile for children, although it is well known that risk factor development takes place during childhood (13,14). Lacking valid data, we undertook an epidemiological survey to obtain information concerning the distribution of hypertension and other CVD risk factors in children and teenagers in Sousse, Tunisia.
The aim of the survey was to establish the prevalence of hypertension, the percentile distribution of blood pressure, and the inter-relationships between hypertension and other CVD risk factors among school children, with the goal to help promote healthy lifestyles early in life.
METHODS
Study design and sampling method
The studied population was composed of school children aged 13 to 19 years, in colleges and public secondary schools in the urban region of Sousse during the 1998/1999 school year. A cross-sectional study was carried out on a representative sample of these pupils, which were recruited in randomly selected cluster samples (the first cluster was comprised of randomly selected establishments and the second cluster was comprised of randomly selected classes within these establishments). The sample size calculation was based on the estimation of an unknown prevalence (50% assumed) with a precision of ±2.5% and a confidence level of 95%. The required sample size was 1600 children. The total population of school children aged between 13 and 19 years was 7975.
Data collection
General information
All participants completed a questionnaire on their family history of CVDs (eg, hypertension) and their lifestyle characteristics (eg, smoking, usual physical activity and dietary intake).
Anthropometric measurements
Research technicians measured body weight to the nearest 0.1 kg using a standard beam balance scale with participants barefoot and wearing light indoor clothing. Body height was measured to the nearest 0.5 cm. Body mass index (BMI) was defined as the ratio of body weight to body height squared, expressed in kg/m2. Obesity was defined according to the published standards by the International Obesity Task Force (15).
Arterial blood pressure
Due to the risk of observational bias, an electronic system was used to measure blood pressure. The reproducibility of measures and the precision of the device have previously been demonstrated (16,17). After 10 min of rest, blood pressure was measured using an appropriate cuff size on the right arm while in a sitting position. Blood pressure was measured again after 15 min of rest, and the average was used in the analysis.
Blood lipids analysis
Participants had to fast 12 h before their blood was taken. A breakfast was served thereafter. The blood samples were taken by a trained nurse, who had experience with a pediatric population. Five millilitres of blood were collected in a tube containing 1 mg/mL EDTA, and then rapidly centrifuged. Plasma concentrations of high density lipoprotein (HDL) cholesterol were measured after precipitation of apolipoprotein B-containing lipoproteins using the phosphotungstate-magnesium chloride method (Roche Diagnostics, USA), and concentrations of low density lipoprotein cholesterol were calculated using Friedewald’s formula (18). Lipid and lipoprotein concentrations were expressed in mmol/L. The analyses were performed at Medical Policlinic, a clinical chemistry laboratory at the University of Lausanne, Lausanne, Switzerland.
Definition of high blood pressure
The observations of systolic and diastolic blood pressure were statistically analyzed for various percentiles (fifth, 10th, 25th, 50th, 75th, 90th, 95th and 99th percentiles). To define high blood pressure (higher than the 95th percentile according to age and sex) and severe hypertension (higher than the 99th percentile according to age and sex), the criteria used were similar to those of the Second Task Force on Blood Pressure Control in Children (19). All of these values were based on the age and sex of the children.
Statistical analysis
The data were further analyzed by using the Student’s t test for unpaired values between boys and girls, as well as between different binary groups. ANOVA was used for mean differences between more than two groups. The correlation coefficients of systolic and diastolic pressure and of either of these with other quantitatively measured variables were studied. Multivariate logistic regression analysis was used to identify independent predictors of hypertension in the studied population. All statistical analyses were conducted by using the statistical package SPSS (version 10.0, SPSS Inc, USA).
Ethical considerations
Because of the young age of the target population, the present study was undertaken with caution and with respect for the rights and the integrity of people. Authorization was requested from the Tunisian Ministry of National Education, teachers, the directors of schools and from the parents of selected children. Parents were free to refuse their child’s participation; however, this was extremely rare (only five individuals refused to participate).
RESULTS
Among the 1569 sampled children (748 boys and 821 girls), biological measurements were obtained from 1497 children, for a global participation rate of 95.4%.
Table 1 gives the sample size, and the number of examined children by age and sex.
TABLE 1.
Distribution by age and sex of 1569 examined school children in Sousse, Tunisia
| Sex | 13 years of age, n (%) | 14 years of age, n (%) | 15 years of age, n (%) | 16 years of age, n (%) | 17 years of age, n (%) | 18 years of age, n (%) | 19 years of age, n (%) | Total sampled, n (%) |
|---|---|---|---|---|---|---|---|---|
| Boys | 204 (27.3) | 103 (13.8) | 91 (12.2) | 197 (26.3) | 92 (12.3) | 30 (4.0) | 31 (4.1) | 748 (100.0) |
| Girls | 233 (28.4) | 77 (9.4) | 118 (14.4) | 228 (27.8) | 109 (13.3) | 41 (5.0) | 15 (1.8) | 821 (100.0) |
| Total | 437 (27.8) | 180 (11.5) | 209 (13.3) | 425 (27.1) | 201 (12.8) | 71 (4.5) | 46 (2.9) | 1569 (100.0) |
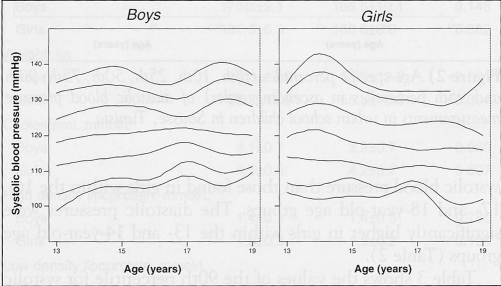
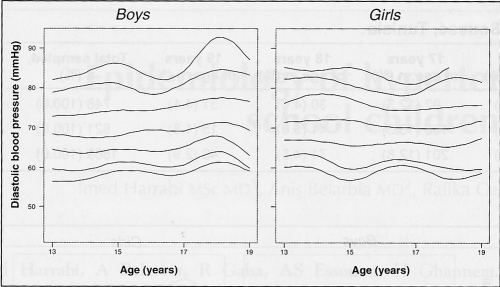
The various percentile curves of systolic and diastolic pressures are shown in Figures 1 and 2. Boys had significantly higher systolic blood pressure than those found in girls within the 16-, 17- and 18-year-old age groups. The diastolic pressures were significantly higher in girls within the 13- and 14-year-old age groups (Table 2).
Figure 1).
Age-specific percentiles (fifth, 10th, 25th, 50th, 75th, 90th and 95th percentiles in ascending order) of systolic blood pressure measurements in urban school children in Sousse, Tunisia
Figure 2).
Age-specific percentiles (fifth, 10th, 25th, 50th, 75th, 90th and 95th percentiles in ascending order) of diastolic blood pressure measurements in urban school children in Sousse, Tunisia
TABLE 2.
Systolic and diastolic blood pressure means in 1569 school children in Sousse, Tunisia
| Systolic blood pressure (mmHg), mean ± SD
|
Diastolic blood pressure (mmHg), mean ± SD
|
|||||
|---|---|---|---|---|---|---|
| Age (years) | Boys | Girls | P | Boys | Girls | P |
| 13 | 117.9±12.9 | 120.2±12.2 | 0.040 | 68.3±7.7 | 75.2±34.6 | 0.003 |
| 14 | 120.2±10.7 | 121.4±11.4 | 0.475 | 68.4±8.1 | 72.1±7.8 | 0.003 |
| 15 | 121.3±10.7 | 119.2±10.4 | 0.157 | 71.8±24.2 | 70.8±8.2 | 0.689 |
| 16 | 121.0±9.6 | 117.6±12.2 | 0.002 | 68.9±8.4 | 70.1±7.5 | 0.145 |
| 17 | 121.7±7.8 | 117.3±8.1 | <0.001 | 70.0±8.1 | 72.9±33.3 | 0.424 |
| 18 | 122.1±9.6 | 116.5±9.5 | 0.002 | 72.5±8.4 | 70.4±7.9 | 0.280 |
| 19 | 121.4±8.3 | 116.1±11.5 | 0.070 | 69.6±8.4 | 70.9±7.1 | 0.599 |
Table 3 shows the values of the 90th percentile for systolic blood pressure and diastolic blood pressure distributed by age and sex.
TABLE 3.
The 90th percentile of systolic and diastolic blood pressure (BP) in 1569 school children in Sousse, Tunisia
| Systolic BP (mmHg)
|
Diastolic BP (mmHg)
|
|||
|---|---|---|---|---|
| Age (years) | Boys | Girls | Boys | Girls |
| 13 | 132.0 | 132.0 | 78.8 | 82.0 |
| 14 | 133.8 | 137.9 | 80.3 | 82.5 |
| 15 | 134.0 | 134.0 | 80.8 | 80.6 |
| 16 | 131.6 | 130.5 | 78.1 | 78.5 |
| 17 | 130.8 | 129.5 | 81.0 | 78.5 |
| 18 | 135.8 | 128.8 | 84.4 | 82.4 |
| 19 | 134.0 | 135.9 | 83.2 | 81.4 |
The prevalence of arterial hypertension was 9.6%, with no significant difference between boys (9.2%) and girls (9.9%). The prevalences of systolic and diastolic hypertension were 6.4% and 4.5%, respectively.
Among both boys and girls, the study of systolic blood pressure means in the different quartiles of BMI, HDL concentrations and triglyceride concentrations showed a significant regular progression from the first to the fourth quartiles (P<0.0001). The study of diastolic blood pressure means in the different quartiles of BMI, HDL concentrations and triglyceride concentrations showed a regular significant increase from the first to the fourth quartiles only for BMI among girls (P=0.03).
In both boys and girls, systolic pressure had a highly significant positive correlation with height (boys: r=0.33, P<0.001; girls: r=0.08, P=0.02), weight (boys: r=0.47, P≤0.001; girls: r=0.35, P<0.001) and triglyceride concentrations (boys: r=0.13, P<0.001; girls: r=0.10, P=0.006). Among boys, a positive correlation was found between systolic blood pressure and age (r=0.12, P=0.001) and, among girls, a negative correlation was found (r=−0.12, P=0.001).
High blood pressure in girls was significantly associated with high weight, high cholesterol concentration and high low density lipoprotein concentration (Table 4).
TABLE 4.
High blood pressure and other cardiovascular risk factors in 1569 school children in Sousse, Tunisia
| Risk factor | Hypertensive children (mean ± SD) | Normotensive children (mean ± SD) | P |
|---|---|---|---|
| Age, years | |||
| Boys | 14.9±1.8 | 15.1±1.7 | 0.431 |
| Girls | 14.5±1.5 | 15.2±1.6 | <0.001 |
| Height, cm | |||
| Boys | 170.3±9.1 | 168.5±10.1 | 0.148 |
| Girls | 161.3±6.3 | 160.6±6.0 | 0.302 |
| Weight, kg | |||
| Boys | 69.2±17.9 | 58.9±13.3 | <0.001 |
| Girls | 63.8±15.2 | 55.5±10.3 | <0.001 |
| Cholesterol, mmol/L | |||
| Boys | 4.1±0.7 | 3.9±0.7 | 0.060 |
| Girls | 4.5±0.8 | 4.2±0.7 | 0.007 |
| High density lipoprotein, mmol/L | |||
| Boys | 1.4±0.3 | 1.4±0.3 | 0.780 |
| Girls | 1.6±0.3 | 1.5±0.2 | 0.103 |
| Low density lipoprotein, mmol/L | |||
| Boys | 2.2±0.6 | 2.1±0.5 | 0.050 |
| Girls | 2.5±0.7 | 2.3±0.6 | 0.032 |
| Triglycerides, mmol/L | |||
| Boys | 1.0±0.2 | 0.9±0.3 | 0.021 |
| Girls | 0.9±0.3 | 0.9±0.2 | 0.199 |
| Glycemia, mmol/L | |||
| Boys | 4.8±0.7 | 4.9±0.7 | 0.911 |
| Girls | 5.3±2.4 | 4.8±0.7 | 0.123 |
Triglyceride concentrations and weight of boys with high blood pressure were significantly more than that of boys with normal blood pressure (Table 4). In a multivariate logistic regression analysis that included smoking status, family history of hypertension, obesity, sex, dyslipidemia and physical inactivity as categorical variables, obesity was found to be the main independent risk factor associated with hypertension in the studied population. The risk of hypertension was significantly increased by 6.31-fold among obese school children compared with nonobese school children (adjusted OR=6.31, 95% CI 4.07 to 9.79).
DISCUSSION
For an epidemiological study, a global participation rate of 95.4% (the participation rate in the present study) is highly interesting and rarely observed. The study of hypertension and other CVD risk factors among school children in a developing country such as Tunisia was of a great interest for several reasons. The only available data at the population level were focused on the CVD risk profile of adults older than 20 years of age in an urban context (11,12) or in a rural area of Tunisia (20). There is an obvious lack of valid data on CVD risk factors among children in Tunisia and, even for clinical purposes, we do not have national reference values for the percentile distribution of the main CVD risk factors, such as children’s blood pressure.
Although the prevalence of clinical hypertension is far less in children than in adults, there is enough evidence to suggest that the ‘roots’ of essential hypertension extend into childhood.
Several epidemiological studies have reported on blood pressure in children; however, there is a great variability in the methodology and the definition of normal and high blood pressure used (21,22). As in adults, blood pressure in children is influenced by a number of environmental and genetic factors, and there is a need for population studies to obtain normative data on blood pressure in children.
In the present study, the data concerning the readings of blood pressure of a representative sample of urban school children in Sousse, Tunisia, at different ages are presented. We found the overall prevalence of high blood pressure to be 9.6% based on a casual reading. In other reports (23–25), the prevalence in this same age group was found to vary from 2% to 13%. In the same population, we have also found that the prevalence of high blood pressure was higher, although not significantly, in girls than in boys. Systolic blood pressure showed a positive correlation with increased age among boys, consistent with findings reported by several other studies of children (26–28). The negative correlation found between systolic blood pressure and age among girls could be explained by the hormonal modifications related to puberty, which starts earlier among girls than among boys. Obesity was the main independent risk factor for hypertension in the studied population and this has been shown in other studies of children (29,30).
In regard to the effect of height and weight on blood pressure, most cross-sectional studies of children have shown a strong, positive correlation (29–32). In a similar study in adolescents (24), a correlation was found between weight and systolic pressure in both boys (r=0.167, P≤0.01) and girls (r=0.112, P<0.01) (29).
In a developing country facing the epidemiological transition like Tunisia, it would seem logical that CVD prevention should start early in life (in childhood) (30) by promoting healthy lifestyles in schools.
Despite the potential weaknesses of the present study, such as its cross-sectional design and the single measurement of blood pressure, the data will help health officials adopt a national strategy to prevent the extension of high blood pressure in the population.
REFERENCES
- 1.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 2.Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol, and stroke in eastern Asia. Lancet. 1998;352:1801–7. [PubMed] [Google Scholar]
- 3.Jousilahti P, Vartiainen E, Tuomilehto J, Pekkanen J, Puska P. Effect of risk factors and changes in risk factors on coronary mortality in three cohorts of middle-aged people in eastern Finland. Am J Epidemiol. 1995;141:50–60. doi: 10.1093/oxfordjournals.aje.a117345. [DOI] [PubMed] [Google Scholar]
- 4.Sadowski RH, Falkner B. Hypertension in pediatric patients. Am J Kidney Dis. 1996;27:305–15. doi: 10.1016/s0272-6386(96)90351-0. [DOI] [PubMed] [Google Scholar]
- 5.Sorof JM. Prevalence and consequence of systolic hypertension in children. Am J Hypertens. 2002;15:57S–60S. doi: 10.1016/s0895-7061(01)02303-2. [DOI] [PubMed] [Google Scholar]
- 6.Coody DK, Yetman RJ, Portman RJ. Hypertension in children. J Pediatr Health Care. 1995;9:3–11. doi: 10.1016/s0891-5245(05)80041-0. [DOI] [PubMed] [Google Scholar]
- 7.Morgenstern B. Blood pressure, hypertension, and ambulatory blood pressure monitoring in children and adolescents. Am J Hypertens. 2002;15:64S–66S. doi: 10.1016/s0895-7061(01)02307-x. [DOI] [PubMed] [Google Scholar]
- 8.Misra A. Risk factors for atherosclerosis in young individuals. J Cardiovasc Risk. 2000;7:215–29. doi: 10.1177/204748730000700309. [DOI] [PubMed] [Google Scholar]
- 9.McCrindle BW. Cardiovascular risk factors in adolescents: Relevance, detection, and intervention. Adolesc Med. 2001;12:147–62. [PubMed] [Google Scholar]
- 10.Omran AR. The epidemiologic transition: A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49:509–38. [PubMed] [Google Scholar]
- 11.Ghannem H, Fredj AH. Epidemiological transition and cardiovascular risk factors in Tunisia. Rev Epidemiol Santé Publique. 1997;45:286–92. [PubMed] [Google Scholar]
- 12.Ghannem H, Hadj Fredj A. Prevalence of cardiovascular risk factors in the urban population of Soussa in Tunisia. J Public Health Med. 1997;19:392–6. doi: 10.1093/oxfordjournals.pubmed.a024666. [DOI] [PubMed] [Google Scholar]
- 13.Newman WP, III, Freedman DS, Voors AW, et al. Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis. The Bogalusa Heart Study. N Engl J Med. 1986;314:138–44. doi: 10.1056/NEJM198601163140302. [DOI] [PubMed] [Google Scholar]
- 14.Daniels SR. Cardiovascular disease risk factors and atherosclerosis in children and adolescents. Curr Atheroscler Rep. 2001;3:479–85. doi: 10.1007/s11883-001-0038-3. [DOI] [PubMed] [Google Scholar]
- 15.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beevers G, Lip GY, O’Brien E. ABC of hypertension. Blood pressure measurement. Part I – sphygmomanometry: Factors common to all techniques. BMJ. 2001;322:981–5. doi: 10.1136/bmj.322.7292.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: Recommendations of the European Society of Hypertension. BMJ. 2001;322:531–6. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Cholesterol Education Program (NCEP): Highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992;89:495–501. [PubMed] [Google Scholar]
- 19.Report of the Second Task Force on Blood Pressure Control in Children – 1987. Task Force on Blood Pressure Control in Children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics. 1987;79:1–25. [PubMed] [Google Scholar]
- 20.Papoz L, Ben Khalifa F, Eschwege E, Ben Ayed H. Diabetes mellitus in Tunisia: Description in urban and rural populations. Int J Epidemiol. 1988;17:419–22. doi: 10.1093/ije/17.2.419. [DOI] [PubMed] [Google Scholar]
- 21.Agarwal R, Mandowara SL, Bhandari B. Blood pressure pattern in school children. Indian Pediatr. 1982;19:597–600. [PubMed] [Google Scholar]
- 22.Monge R, Beita O. Prevalence of coronary heart disease risk factors in Costa Rican adolescents. J Adolesc Health. 2000;27:210–7. doi: 10.1016/s1054-139x(99)00017-8. [DOI] [PubMed] [Google Scholar]
- 23.Rosner B, Prineas R, Daniels SR, Loggie J. Blood pressure differences between blacks and whites in relation to body size among US children and adolescents. Am J Epidemiol. 2000;151:1007–19. doi: 10.1093/oxfordjournals.aje.a010129. [DOI] [PubMed] [Google Scholar]
- 24.Sinaiko AR, Gomez-Marin O, Prineas RJ. Prevalence of “significant” hypertension in junior high school-aged children: The Children and Adolescent Blood Pressure Program. J Pediatr. 1989;114:664–9. doi: 10.1016/s0022-3476(89)80718-8. [DOI] [PubMed] [Google Scholar]
- 25.Soyannwo MA, Gadallah M, Kurashi NY, et al. Studies on preventive nephrology: Systemic hypertension in the pediatric and adolescent population of Gassim, Saudi Arabia. Ann Saudi Med. 1997;17:47–52. doi: 10.5144/0256-4947.1997.47. [DOI] [PubMed] [Google Scholar]
- 26.Forrester TE, Wilks RJ, Bennett FI, et al. Fetal growth and cardiovascular risk factors in Jamaican schoolchildren. BMJ. 1996;312:156–60. doi: 10.1136/bmj.312.7024.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klumbiene J, Sileikiene L, Milasauskiene Z, Zaborskis A, Shatchkute A. The relationship of childhood to adult blood pressure: Longitudinal study of juvenile hypertension in Lithuania. J Hypertens. 2000;18:531–8. doi: 10.1097/00004872-200018050-00004. [DOI] [PubMed] [Google Scholar]
- 28.Marques-Vidal P, Llobet S, Carvalho Rodrigues JA, Halpern MJ. Cardiovascular risk factor levels in Portuguese students. Acta Cardiol. 2001;56:97–101. doi: 10.2143/AC.56.2.2005624. [DOI] [PubMed] [Google Scholar]
- 29.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics. 1999;103:1175–82. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 30.Mueller WH, Grunbaum JA, Labarthe DR. Anger expression, body fat, and blood pressure in adolescents: Project HeartBeat! Am J Hum Biol. 2001;13:531–8. doi: 10.1002/ajhb.1085. [DOI] [PubMed] [Google Scholar]
- 31.Flynn JT. What’s new in pediatric hypertension? Curr Hypertens Rep. 2001;3:503–10. doi: 10.1007/s11906-001-0013-y. [DOI] [PubMed] [Google Scholar]
- 32.Bradbury J. Early weight gain patterns may affect adult blood pressure. Lancet. 2002;359:501. doi: 10.1016/s0140-6736(02)07703-6. [DOI] [PubMed] [Google Scholar]