Abstract
Twenty-one patients with rheumatoid arthritis who underwent Swanson metacarpophalangeal (MP) arthroplasty from 1994 to 1999 were assessed for active flexion of individual MP joints an average of 59 months (range 27–114 months) postoperative. Published articles of Swanson MP arthroplasty were reviewed. Experienced hand surgeons were surveyed regarding outcomes of metacarpophalangeal arthroplasty. The MP joint of the little finger displayed significantly less flexion than that of the middle and index finger. Seven of eight published studies which present active MP flexion by individual digit demonstrated less flexion in the little finger compared to the index, middle, and ring finger. Half of surgeons surveyed reported that MP range of motion is shifted toward a more extended position, that MP flexion is limited in the ulnar digits, and that an implant that encourages MP flexion would be helpful. Our experience with this cohort, a review of published literature, and a survey of international experts suggest that Swanson arthroplasty frequently results in a range of flexion of the MP joint of the little finger that may be insufficient for its principal functions.
Keywords: Metacarpophalangeal joint; Arthroplasty, replacement, finger; Arthritis, rheumatoid; Range of motion, articular; Little finger
Introduction
Silicone arthroplasty of the metacarpophalangeal (MP) joints is a well-established treatment for patients who have advanced rheumatoid arthritis (RA). The goals of MP arthroplasty are to correct deformity, restore function, and relieve pain. The one-piece silicone implant designed by Swanson and first published in 1968 [1] is the most widely used and studied MP implant [2–4].
While some studies of the Swanson implant report no postoperative improvement in total range of motion (ROM), it has been demonstrated that the arc of motion usually shifts from predominant MP flexion preoperatively (due to fixed flexion deformity and MP joint and extensor tendon subluxation or dislocation) to a more extended range, which has been considered to be a more functional position [5–8].
A published report of the functional range of motion in the normal hand determined that the MP joint requires an average of 61° arc of motion to perform 11 different activities of daily living and an average of 72° arc of motion to perform power grip [9]. The minimum MP arc of motion required to perform all 11 activities of daily living is 33°.
The radial digits (index and long) are considered to function principally in relative extension for pinch functions, whereas the ulnar digits (ring and little) are considered to function principally in relative flexion for power grip [10, 11]. Accordingly, we consider that the desired outcome for maximum flexion of the MP joint following MP arthroplasty may differ from the radial to the ulnar side of the hand. Notwithstanding general statements in the literature regarding the different functional roles of the digits, we were unable to find any published articles supporting or testing this view. Furthermore, most published studies of MP arthroplasty do not report postoperative flexion and extension data by individual digit, but instead, provide data on range of flexion and extension (sometimes only the arc of motion) using the average of all four finger MP joints.
The purposes of our study are (1) to examine a cohort of patients with RA who underwent Swanson MP arthroplasty to determine postoperative active flexion at the MP joint of each digit, (2) to review published reports of postoperative active flexion at the MP joint by digit after MP arthroplasty in patients with RA, and (3) to survey the opinions of a sample of experienced hand surgeons regarding individual digit function after MP arthroplasty in this patient group.
Materials and Methods
Retrospective Patients Review
We undertook a retrospective review of one author’s patient records to identify eligible patients for this study. Inclusion criteria were a diagnosis of rheumatoid arthritis and primary Swanson metacarpophalangeal arthroplasty of all four fingers during a 6-year period from January 1994 to December 1999. An exclusion criterion was any previous surgery at the level of the MP joint. Data gathered included individual MP joint range of motion (active flexion and extension), proximal interphalangeal (PIP) joint range of motion (flexion and extension), composite flexion (distance from tip of finger to distal palmar crease), and grip strength using a Jamar dynamometer (positions 1 through 5).
Comparison of continuous variables was performed using multiple t tests, while accounting for multiple comparisons and Kruskal–Wallis tests (nonparametric) if normality of the data could not be assumed. Based on previous literature [9], maximum active MP flexion was also categorized as sufficient (>60°), borderline (30–60°), and insufficient (<30°) and compared between the digits using a chi-squared test. Correlation between continuous variables was assessed using Pearson (r) correlation coefficients.
This study was approved by the Ethics Review Board at St. Michael’s Hospital, Toronto, Canada.
Literature Review
We conducted a computerized search using Medline (from 1966), EMBASE (from 1980), and CINAHL (from 1982) to identify all citations of metacarpophalangeal arthroplasty in patients with rheumatoid arthritis published between 1966 and December 2006. Only original research studies were included. We eliminated studies of sites other than the MP joint of the finger (e.g., thumb, PIP) and conditions other than rheumatoid arthritis (e.g., trauma, systemic lupus erythematosus, psoriatic arthropathy). Full-text copies of all relevant original articles, systematic reviews, and review articles were obtained and each bibliography examined for original articles not identified during the computerized search.
Hand Surgeon Opinion Survey
We conducted an informal survey by mail questionnaire of 25 experienced hand surgeons from five countries (Canada, USA, UK, Switzerland, Spain) active in rheumatoid hand reconstruction. The survey utilized a 7-point Likert scale (from “Completely agree” to “Completely disagree”) to determine surgeon opinions on indications for MP reconstruction, outcome following MP reconstruction, and implant design. Surgeon opinions on indications for MP reconstruction have been published elsewhere [12], and we report herein on surgeon opinion regarding outcomes of MP reconstruction and implant design. Surgeons were asked to agree or disagree with the following questions:
Following MP reconstruction, MP flexion is consistently more restricted/limited in D4 (ring finger) and D5 (little finger) than in D2 (index finger) and D3 (middle finger);
Following MP reconstruction, increased MP extension is accompanied by a significant decrease in flexion;
Following MP reconstruction, the arc of motion does not significantly increase, but is shifted toward a more extended position;
There is need for a new implant design in MP reconstructive surgery;
An implant design that encourages MP flexion would be helpful;
An implant design that encourages MP extension would be helpful.
Results
Retrospective Patient Review
Thirty-four patients were identified from the chart review and invited by telephone to participate in our study. Twenty-one patients (62%) agreed to participate and attended an assessment visit. Mean age at the time of surgery was 66 years (range: 48–84), 20 of 21 patients (95%) were female (four patients underwent staged bilateral procedures during this period for a total of 25 hands and 100 joints), the average disease duration was 18.7 years, and the mean time to follow-up was 59.4 months (range: 27–114 months) (Tables 1 and 2).
Table 1.
Summary of patient chracteristics (n = 21).
| Variable | Mean | Range | SD |
|---|---|---|---|
| Age at surgery (years) | 66.0 | 48–84 | 8.8 |
| Disease duration at surgery (years) | 18.7 | 4–38 | 9.8 |
| Follow-up period (months) | 59.4 | 27–114 | 29.5 |
Table 2.
Summary of patient chracteristics (n = 21).
| By patient | Characteristics | Frequency | Percentage of total (%) |
|---|---|---|---|
| Gender | F | 20 | 95 |
| M | 1 | 5 | |
| Surgical side | Left | 6 | 29 |
| Right | 11 | 52 | |
| Bilaterala | 4 | 19 |
aFour patients underwent staged bilateral procedures for a total of 25 hands.
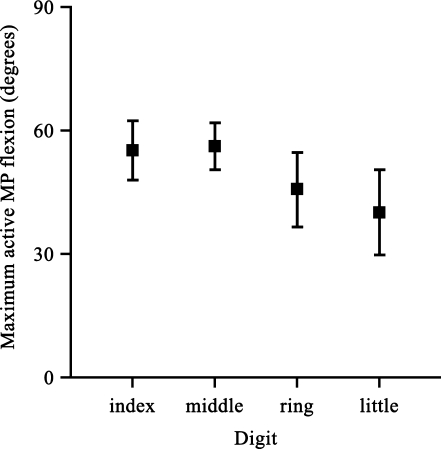
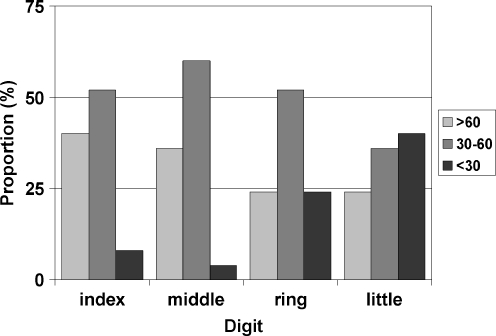
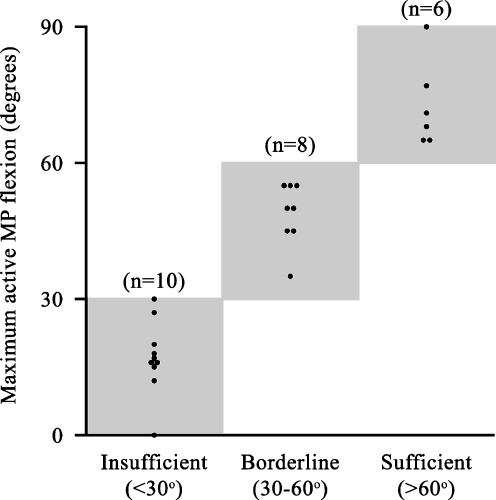
The mean postoperative maximum active MP flexion of each digit is presented with standard deviation, median, and range in Table 3 and with 95% confidence intervals in Fig. 1. The MP joint of the little finger displayed significantly less active flexion than the MP joint of the index (40.1 vs 55.2°, p < 0.05) and middle finger (40.1 vs 56.2°; p = 0.03). The MP joint of the ring finger displayed a trend to less active flexion than the MP joint of the index (45.8 vs 55.2°, p = 0.21) and middle finger (45.8 vs 56.2°; p = 0.15), but there was no statistical significance. No other significant differences were found between the MP joints of the index and middle or ring and little fingers (p > 0.9). Nonparametric analysis of maximum active MP flexion found significant difference among the four MP joints (chi-squared statistic: 8.12, p = 0.04). The proportion of patients with sufficient (>60°), borderline (30–60°), and insufficient (<30°) maximum active MP flexion is presented in Fig. 2, which showed significant differences (Chi-squared statistic: 13.8, p = 0.03) among the digits. The number of patients with insufficient active MP flexion was 2 (8%), 1 (4%), 6 (24%), and 10 (40%) for the index, middle, ring, and little finger, respectively. The number of patients with sufficient active MP flexion was 10 (40%), 9 (36%), 6 (24%), and 6 (24%) for the index, middle, ring, and little finger, respectively. Individual values of postoperative maximum active MP flexion of the little finger are plotted in Fig. 3 to highlight predominately insufficient MP flexion of the little finger.
Table 3.
Mean postoperative maximum active metacarpophalangeal flexion by digit (n = 25).
| Digit | Mean (°) | SD | Median (°) | Range (°) |
|---|---|---|---|---|
| Index | 55.2 | 17.4 | 55.0 | 10 to 95 |
| Middle | 56.2 | 13.8 | 55.0 | 22 to 81 |
| Ring | 45.8 | 21.1 | 50.0 | −10 to 78 |
| Little | 40.1 | 25.1 | 45.0 | −10 to 90 |
Figure 1.
Mean postoperative maximum active metacarpophalangeal flexion after Swanson arthroplasty by digit with 95% confidence intervals (n = 25 hands).
Figure 2.
Proportion of patients with sufficient (>60°), borderline (30–60°), and insufficient (<30°) active metacarpophalangeal flexion by digit (n = 25 hands).
Figure 3.
Distribution of maximum active flexion of the metacarpophalangeal joint of the little finger (n = 24 hands).
The mean postoperative maximum active PIP flexion of each individual digit is presented with standard deviation, median, and range in Table 4. There were no significant differences between the mean maximum active PIP flexion of each digit. Jamar grip strength was 6.8 (median: 6.0, SD: 4.2), 13.2 (median: 15.0, SD: 7.2), 16.8 (median: 18.0, SD:7.5), 14.7 (median: 14.5, SD: 7.8), and 12.8 (median: 14.0, SD: 4.9) pounds at positions one (1 3/8” wide) through five (3 3/8” wide), respectively.
Table 4.
Mean postoperative maximum active proximal interphalangeal joint flexion by digit (n = 25).
| Digit | Mean (°) | SD | Median (°) | Range (°) |
|---|---|---|---|---|
| Index | 81.0 | 27.9 | 87.5 | 0 to 110 |
| Middle | 91.0 | 15.7 | 95.0 | 60 to 115 |
| Ring | 94.3 | 23.5 | 100.0 | 0 to 115 |
| Little | 90.3 | 22.9 | 95.5 | 0 to 110 |
Jamar grip strength showed no correlation with maximum active MP flexion (∣r∣ < 0.2 between all five Jamar grip positions and all joints) and weak correlation with maximum active flexion of individual PIP joints (r < 0.4 between all five Jamar grip positions and all joints). Correlation between composite flexion and maximum active MP flexion declined from the index finger (r = 0.31) to the little finger (r = 0.09). Composite flexion and maximum active PIP flexion showed moderate negative correlation in the index finger (r = −0.45), middle finger (r = −0.68), and ring finger (r = −0.61), and no correlation in the little finger (r = −0.04).
Literature Review
We identified 49 published trials of MP arthroplasty in patients with rheumatoid arthritis. Fourteen trials on implants other than Swanson were excluded. Of the remaining 35 trials, only eight [7, 8, 13–18] report active MP flexion ROM for individual digits presented alongside our results in Table 5. Active MP flexion of the little finger was less than active MP flexion of the index, middle, and ring fingers in seven of eight trials and in the left-handed subset of the eighth trial [15].
Table 5.
Published reports of individual maximum active metacarpophalangeal flexion following Swanson arthroplasty.
| Authors | Journal | Year | Number of joints (N) | Mean F/U | Hand | Mean active MP flexion (°) | |||
|---|---|---|---|---|---|---|---|---|---|
| Years (range) | Index | Middle | Ring | Little | |||||
| Bogoch | – | 2007 | 20 (96) | 5 (2–10) | – | 55 | 57 | 47 | 41a |
| Parkkila | J Hand Surg (Am) | 2005 | 23 (89) | 5 (3–6.5) | – | 54 | 59 | 59 | 44a |
| Goldfarb | JBJS (Am) | 2003 | 36 (208) | 14 (6–21) | – | 60 | 66 | 60 | 49a |
| Kirschenbaum | JBJS (Br) | 1993 | 19 (76) | 8.5 (5–16) | L | 67 | 69 | 74 | 54a |
| 17 (68) | R | 50 | 55 | 58 | 54 | ||||
| Wilson | J Hand Surg (Br) | 1993 | 35 (185) | 9.6 (5–14) | L | 55 | 55 | 51 | 49a |
| R | 47 | 44 | 46 | 40a | |||||
| Bieber | JBJS (Am) | 1986 | 46 (210) | 5.25 (2–8) | – | 41 | 43 | 36 | 35a |
| Vahvanen | J Hand Surg (Am) | 1986 | 32 (107) | – | 42 | 40 | 42 | 40a | |
| Mannerfelt | JBJS (Am) | 1975 | 50 (144) | 2.5 (1.5–3.5) | – | 51 | 55 | 50 | 39a |
| Gschwend | Handchirurgie | 1974 | 46 (200) | 1.5 (?–?) | – | 51 | 51 | 48 | 41a |
aIndicates mean active MP flexion less than that of index, middle, and ring fingers
The data analysis for this paper was performed using SAS/STAT® software, Version 8.2 of the SAS System for Windows (Copyright© 1999-2001 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA).
A review of functional outcomes in all 35 published trials of Swanson MP arthroplasty from the literature review found three studies that reported significant quantitative improvement in hand function following MP arthroplasty [19–21]. Numerous other studies reported subjective improvement of function in patients after MP arthroplasty, but little or no improvement in objective functional measures, such as grip strength, pinch strength, or function-related assessment scores such as the Jebsen–Taylor test or Sollerman hand function test [5, 7, 13, 22–25].
Newer MP implants have been designed to more closely mimic the kinematics of the natural MP joint [23, 26]. Despite this emerging interest in improving postoperative MP flexion, we have not found any published discussion or analysis that focuses on diminished MP flexion of the little finger and its potential functional or cosmetic significance after MP arthroplasty for RA.
Hand Surgeon Opinion Survey
Twenty-three of 25 surgeons responded to our survey. Of the 23 surgeons responding, 12 agreed that MP flexion is more limited in the ring and little fingers compared to the index and middle fingers after MP reconstruction. Opinions were mixed on whether increased postoperative MP extension is accompanied by a significant decrease in postoperative MP flexion following MP reconstruction (ten agreed, six disagreed, seven neither agreed nor disagreed), but 15 responded that the arc of motion does not increase and is shifted toward a more extended position. Furthermore, 17 responded that an implant design that encourages flexion would be helpful, while only one disagreed (five neither agreed nor disagreed).
Discussion
A substantial portion of our patient cohort receiving Swanson implants achieved insufficient active flexion in the MP joint of the little finger (Fig. 3) when compared to the other digits. This results in a “reverse cascade” appearance of the hand with flexion diminishing from the radial to ulnar digits rather than increasing as in the normal hand. Our review of the literature yielded similar results finding less flexion in the MP joint of the little finger than in the other fingers in the majority of published studies. While there are informal references to the importance of range of motion to hand function [27], we have not found a published discussion that identifies decreased MP flexion, specifically of the little finger, as an issue of importance in rheumatoid hand reconstruction. Furthermore, our international survey found that nearly three-quarters of rheumatoid hand surgeons thought that an MP implant that encouraged flexion would be helpful.
In this study, we found that Jamar grip strength correlated poorly with MP flexion. In the rheumatoid hand, other factors such as PIP flexion, pain, and flexor tendon function may have a substantial effect on grip strength independent of MP flexion.
Causes of postoperative lack of flexion after MP joint surgery of the little finger are not known. These may include inadvertent release of the insertion of flexor digiti quinti brevis during release of abductor digiti quinti, the extended (0°) resting position of the Swanson implant, postoperative care (immobilization, splinting, and therapy protocols), and patient factors. Lack of flexion in the MP joint of the little finger might be mitigated to a small degree by the greater carpometacarpal mobility in this ray. While increased active PIP flexion may also mitigate the lack of MP flexion in select patients, our study did not find significantly higher PIP flexion in the little finger compared to the ulnar digits.
One limitation of this study is the use of a retrospective cohort. However, our focus is on a specific range of motion at final outcome irrespective of preoperative status or selection. Also, although Jamar grip strength was recorded, we did not employ a standardized functional instrument, which would have been of interest to correlate with range of motion. The sample size was small but sufficient to identify differences in active flexion of the different MP joints.
In summary, our experience with a cohort of patients undergoing rheumatoid hand reconstruction, a review of published literature, and a survey of international experts suggest that Swanson arthroplasty frequently results in a range of flexion of the MP joint of the little finger that may be insufficient for its principal functions.
Acknowledgements
The authors thank the hand surgeons who provided responses to the survey: T. Axelrod, R. Beckenbaugh, P. Binhammer, A. Freiberg, B. Graham, P. T. Gropper, N. Gschwend, D. Hastings, G. H. Johnston, G. J. W. King, I. Leslie, A. Lluch, J. Mahoney, R. T. Manktelow, R. McGraw, M. McKee, E. Nalebuff, W. Rennie, R. S. Richards, R. Richards, J. H. Roth, B. Simmen, J. Stanley, A. Thoma, C. S. Wright III.
The authors thank Dagmar Gross for assistance with preparation of the manuscript.
Grant declaration This study was internally funded and did not receive any grant support.
References
- 1.Swanson AB. Silicone rubber implants for replacement of arthritis or destroyed joints in the hand. Surg Clin North Am 1968; 48:1113–27. [DOI] [PubMed]
- 2.el-Gammal TA, Blair WF. Motion after metacarpophalangeal joint reconstruction in rheumatoid disease. J Hand Surg [Am] 1993; 18:504–11. [DOI] [PubMed]
- 3.Linscheid RL. Implant arthroplasty of the hand: retrospective and prospective considerations. J Hand Surg [Am] 2000;25:796–816. [DOI] [PubMed]
- 4.Sollerman C. Endoprosthetic replacement of the metacarpophalangeal joints in rheumatoid arthritis. Tech Orthop 2003;18:233–8. [DOI] [PubMed]
- 5.Blair WF, Shurr DG, Buckwalter JA. Metacarpophalangeal joint arthroplasty with a metallic hinged prosthesis. Clin Orthop Relat Res 1984;184:156–63. [PubMed]
- 6.Chung KC, Kowalski CP, Myra KH, et al. Patient outcomes following Swanson silastic metacarpophalangeal joint arthroplasty in the rheumatoid hand: a systematic overview. J Rheumatol 2000;27:1395–402. [PubMed]
- 7.Mannerfelt L, Andersson K. Silastic arthroplasty of the metacarpophalangeal joints in rheumatoid arthritis. J Bone Joint Surg Am 1975;57:484–89. [PubMed]
- 8.Vahvanen V, Viljakka T. Silicone rubber implant arthroplasty of the metacarpophalangeal joint in rheumatoid arthritis: a follow-up study of 32 patients. J Hand Surg [Am] 1986;11:333–9. [DOI] [PubMed]
- 9.Hume MC, Gellman H, McKellop H, et al. Functional range of motion of the joints of the hand. J Hand Surg [Am] 1990;15:240–3. [DOI] [PubMed]
- 10.Chase RA. Anatomy of the upper extremity. In: Callahan AD, Hunter JM, Mackin E, editors. Rehabilitation of the hand: surgery and therapy. 3rd ed. St. Louis: Mosby; 1995. p. 13–4.
- 11.Tubiana R. Architecture and functions of the hand. In: Mackin E, Thomine JM, editors. Examination of the hand and wrist. 2nd ed. St. Louis: Mosby; 1996. p. 71–3.
- 12.Bogoch ER, Judd MGP. The hand: a second face? J Rheumatol 2002;29:2477–83. [PubMed]
- 13.Bieber EJ, Weiland AJ, Volenec-Dowling S. Silicone–rubber implant arthroplasty of the metacarpophalangeal joints for rheumatoid arthritis. J Bone Joint Surg Am 1986;68:206–9. [PubMed]
- 14.Goldfarb CA, Stern PJ. Metacarpophalangeal joint arthroplasty in rheumatoid arthritis: a long-term assessment. J Bone Joint Surg Am 2003;85:1869–78. [DOI] [PubMed]
- 15.Kirschenbaum D, Schneider LH, Adams DC, et al. Arthroplasty of the metacarpophalangeal joints with use of silicone–rubber implants in patients who have rheumatoid arthritis. Long-term results. J Bone Joint Surg Am 1993;75:3–12. [DOI] [PubMed]
- 16.Parkkila T, Belt EA, Hakala M, et al. Comparison of Swanson and Sutter metacarpophalangeal arthroplasties in patients with rheumatoid arthritis: a prospective and randomized trial. J Hand Surg [Am] 2005;30:1276–81. [DOI] [PubMed]
- 17.Wilson YG, Sykes PJ, Niranjan NS. Long-term follow-up of Swanson’s silastic arthroplasty of the metacarpophalangeal joints in rheumatoid arthritis. J Hand Surg [Br] 1993;18:81–91. [DOI] [PubMed]
- 18.Gschwend N, Zimmerman J. Analyse von 200 MCP Arthroplastiken. Handchirurgie 1974;6:7–15.
- 19.Rothwell AG, Cragg KJ, O’Neill LB. Hand function following silastic arthroplasty of the metacarpophalangeal joints in the rheumatoid hand. J Hand Surg [Br] 1997;22:90–3. [DOI] [PubMed]
- 20.Moller K, Sollerman C, Geijer M, et al. Osseointegrated silicone implants. 18 patients with 57 MCP joints followed for 2 years. [see comment]. Acta Orthop Scand 1999;70:109–15. [DOI] [PubMed]
- 21.Pereira JA, Belcher HJ. A comparison of metacarpophalangeal joint silastic arthroplasty with or without crossed intrinsic transfer. J Hand Surg [Br] 2001;26:229–34. [DOI] [PubMed]
- 22.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg [Am] 2004;29:646–53. [DOI] [PMC free article] [PubMed]
- 23.Moller K, Sollerman C, Geijer M, et al. Avanta versus Swanson silicone implants in the MCP joint—a prospective, randomized comparison of 30 patients followed for 2 years. J Hand Surg [Br] 2005;30:8–13. [DOI] [PubMed]
- 24.Schmidt K, Willburger RE, Miehlke RK, et al. Ten-year follow-up of silicone arthroplasty of the metacarpophalangeal joints in rheumatoid hands. Scand J Plast Reconstr Surg 1999;33:433–8. [DOI] [PubMed]
- 25.Synnott K, Mullett H, Faull H, et al. Outcome measures following metacarpophalangeal joint replacement. J Hand Surg [Br] 2000;25:601–3. [DOI] [PubMed]
- 26.Delaney R, Trail IA, Nuttall D. A comparative study of outcome between the Neuflex and Swanson metacarpophalangeal joint replacements. J Hand Surg [Br] 2005;30:3–7. [DOI] [PubMed]
- 27.Chauhan C, Howard A, Norris SH, et al. Prognostic indicators for Swanson metacarpophalangeal arthroplasty in rheumatoid arthritis. J Orthop Rheumatol 1995;8:106–10.