Abstract
We report the unusual case of a patient with systemic lupus erythematosus (SLE)-associated arthritis mutilans. Arthritis mutilans is a variant of erosive arthritis that is more commonly reported with psoriatic and rheumatoid arthritis and not with SLE. Joint fusion has been shown to be the most effective measure to preserve bone length and prevent further erosive joint changes in arthritis mutilans. We attempted to enhance success of a thumb interphalangeal joint fusion in our patient by adding compression across the fusion with implant screws, given the difficulty of achieving solid bone fusion ordinarily. Osteolysis around the compression screw resulted in arthrodesis failure. We were finally able to achieve successful fusion with iliac crest corticocancellous bone grafts and Kirschner wire fixation. Implant athroplasty in patients with bone loss is risky as it often furthers joint instability because of bone resorption around the prosthesis. This is a point of caution regarding use of any implant (including large screws) in patients with arthritis mutilans, as osteolysis around the implant may occur.
Keywords: Small joint arthrodesis, Compression screw, Lupus-associated arthritis mutilans
Introduction
Arthritis mutilans was first described in 1913 by Marie and Leri and is reported in the literature as a variant of several forms of arthritis being most commonly found among patients with psoriatic arthritis [1, 6, 7, 10]. About 7% of patients with psoriasis develop arthritis, and 5% of those, in turn, develop the severe osteolytic variant called arthritis mutilans [11, 15]. It is also said to develop in 4.4% of patients with rheumatoid arthritis [16]. The arthropathies which may manifest with arthritis mutilans include mixed connective tissue disease, juvenile rheumatoid arthritis, neuropathic arthropathy, gout, scleroderma, tuberculosis, vinyl chloride poisoning, tertiary syphilis, osteomyelitis, although prevalence data for these is totally lacking [14]. One would expect arthritis mutilans to be a rare occurrence in patients with systemic lupus erythematosus (SLE). While joint deformities are the predominant clinical manifestations of SLE, these are secondary to ligament and volar plate laxity and tendon subluxation, leading to joint imbalance [3, 4, 8]. The joint deformities in SLE characteristically occur without the erosive destruction of articular cartilage seen in other forms of arthritis.
Arthritis mutilans is a variant of erosive arthritis in which there is severe osteolysis of phalanges and metacarpals. It is rapidly progressive and causes significant deformity, with collapse and telescoping of the tubular bones of the hand, known as main en lorgnette or opera glass deformity [1, 3, 4, 8, 10–12, 14–16]. Radiographic manifestations show cupping in the bases of phalanges and narrowing and dissolution of the adjacent metacarpal and phalangeal heads (acro-osteolysis), which fit like pencil points into the phalangeal cups or the so-called “pencil in cup deformity”. Joint fusion is the only operative procedure which will preserve bone length and stop further shortening at that level [10]. We felt that interphalangeal joint fusion in our patient, using a compression screw, would help facilitate arthrodesis, but instead, osteolysis occurred around the prosthetic device and instability recurred, requiring repeat attempt at fusion to be done which was ultimately successful.
We present a case of arthritis mutilans in a patient with lupus arthritis in whom initial interphalangeal joint fusion failed because of continued osteolysis, which occurred around the prosthetic compression screw. Thus, the purpose of this case report is twofold: (1) to describe the unusual occurrence of arthritis mutilans in a patient with SLE; (2) to bring to awareness the potential for osteolysis occurring around large compression screws leading to relapse of joint instability and failure of the fusion attempt in patients with arthritis mutilans.
Case Report
A 45-year-old right-hand dominant female presented because of increasing weakness of her grip due to destructive changes with instability in her right thumb. She was unable to turn her car key in the ignition and had difficulty opening doors. SLE had been diagnosed 13 years previously. She also had inflammatory bowel disease and had a prior squamous cell carcinoma excised from her right leg.
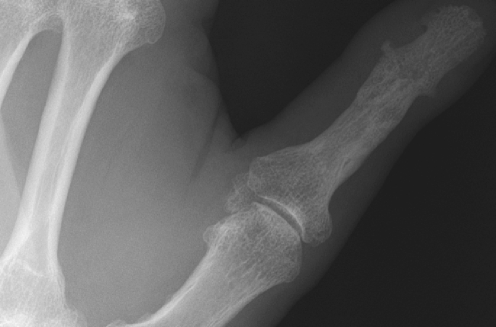
Findings on her right hand included ulnar deviation of the index finger, a sausage-like diffusely swollen middle finger, and radial deviation with gross instability of the interphalangeal joint of the thumb (Fig. 1). Grip strength was greatly reduced, and she could not oppose the thumb across to the little finger. The opposite hand had a telescoping deformity of the little finger and significant ulnar deviation of the ring finger distal phalanx (Fig. 2).
Figure 1.
Preoperative radiographs show the characteristics changes of “arthritis mutilans” at both the IP joint of the thumb and the PIP joint of the middle finger.
Figure 2.
The opposite hand also showed the clinical features with instability and ulnar deviation at the PIP joint of the ring finger and the “opera glass” deformity of the little finger.
The patient underwent fusion of the right thumb IP joint using an iliac crest corticocancellous interposition graft and Kirschner wire fixation. Unfortunately, despite prolonged thumb immobilization postoperatively, she developed a nonunion at the proximal end of the iliac bone graft.
Five months later, we repeated the fusion of the thumb, but felt that our success would be potentially improved by adding compression across the arthrodesis site. On that occasion, we utilized a mini-Acutrak® compression screw (Acumed LLC, Hillsboro, OR. 97124) and a bone graft taken from the distal radius. This fusion was seemingly initially successful in that the thumb was clinically stable (Fig. 3). Fixation was felt to be very secure, and the thumb was immobilized postoperatively for 8 weeks.
Figure 3.
Intraoperative radiograph showing the compression device in good clinical fixation across the thumb IP joint.
However, about 20 months later, the patient presented with progressive swelling, throbbing pain, and IP joint radial deviation of the previously operated right thumb. There was a 45° radial clinodactyly at the right thumb IP joint. Radiographs showed bone resorption around the Acutrak® screw, loosening at the joint and soft tissue swelling of the thumb (Fig. 4).
Figure 4.
Failed thumb IP joint fusion having used a compression screw, showing instability of the joint and osteolysis the screw.
After the failed joint implant screw, we attempted a third fusion of the thumb IP joint. In addition, by this time, the middle finger PIP joint was unstable and telescoping. Fusion of both the thumb IP joint and the middle finger PIP joint was performed once again using iliac crest corticocancellous bone grafts for each and Kirschner wire fixation. Both fusions were successful, and hand function is improved as a result of restoring joint stability (Fig 5).
Figure 5.
Successfully fused thumb IP joint after two prior attempts at arthrodesis.
Discussion
In patients with SLE, erosive changes of joints are a rarity. In an evaluation of 50 SLE patients (average disease duration of 8 years), radiographic examinations showed preservation of normal articular cartilage without erosive changes [2]. The joint deformities clinically resemble those of rheumatoid arthritis, but they are the consequence of ligament laxity and tendon subluxation, and they occur without the erosive destruction of articular cartilage seen in other forms of inflammatory arthritis [3, 4]. While arthritis mutilans is recognized to occur in patients with psoriatic arthritis and rheumatoid arthritis, it is not really reported in patients with SLE. Thus, our patient’s rare association between arthritis mutilans and SLE is in itself reportable.
More significant, in our opinion, is the fact that osteolysis continued to occur around the Acutrak ® implant and led to arthrodesis failure in this patient. Fusion is the only operative procedure which preserves bone length and stops further shortening in patients affected with arthritis mutilans [10]. However, obtaining solid bone fusion is not easy and often requires supplemental bone grafting to succeed. Tension band techniques and compression wires are said to be helpful in this regard [9]. Our initial failure at achieving stable arthrodesis of the thumb IP joint confirms the difficulty of achieving bone union in these patients. We felt that by adding a compression screw at our second attempt at arthrodesis, we would then be more likely to be successful. To our chagrin, osteolysis occurred around the implant, and failure of that fusion resulted once again.
Arthrodesis using bone graft to distract the telescoping digits out to length has previously been shown to be successful in these patients [5, 14]. Success of fusion was also confirmed by Nalebuff in treating these patients with arthritis mutilans.
Arthroplasty in these patients with bone loss is risky because osteolysis continues, and the prosthesis eventually becomes uncovered by bone resorption, resulting in loss of all stability. While Swanson has shown bone build up around MP implants in cases of rheumatoid arthritis, the reverse occurs in patients with arthritis mutilans [10, 13].
In our patient, it seemed like the compression screw behaved like joint implants do in patients with arthritis mutilans. Our intention was to enhance the likelihood of achieving fusion, by applying compression across the joint, but the implant failed.
Prolonged observation of patients with arthritis mutilans should be avoided as osteolysis continues unabated. Selective fusion of joints restores functional length, improves the appearance of the hand, and most importantly, halts the disease progress at that digit [5, 9, 14]. Arthroplasties of the interphalangeal joints do not stop bone loss and should not be used in association with the osteolysis type of inflammatory arthritis [10]. Arthrodesis may be difficult to achieve. A compression screw was not helpful, and in fact, osteolysis occurred around the screw, much as it does around implants used for arthroplasty in patients with arthritis mutilans.
References
- 1.Belsky MR, Feldon PF, Millender LN, Nalebuff EA, Phillips C. Hand involvement in psoriatic arthritis. J Hand Surg 1982;7:203–7. [DOI] [PubMed]
- 2.Bleifeld CJ, Inglis AE. The hand in systemic lupus erythematosus. J Bone Joint Surg 1974;56A:1207–15. [PubMed]
- 3.Dray GJ. The hand in systemic lupus erythematosus. Hand Clin 1989;5:145–55. [PubMed]
- 4.Dray GJ, Millender LH, Nalebuff EA, Phillips C. The surgical treatment of hand deformities in systemic lupus erythematosus. J Hand Surg 1981;6:339–45. [DOI] [PubMed]
- 5.Froimson AI. Hand reconstruction in arthritis mutilans. A case report. J Bone Joint Surg 1971;53A:1377–82. [PubMed]
- 6.Golding DN. Arthritis mutilans. Rheumatism 1965;21(4):86–90. [PubMed]
- 7.Kapasi OA, Ruby LK, Calney K. The psoriatic hand. J Hand Surg 1982;7:492–7. [DOI] [PubMed]
- 8.Nalebuff EA. Surgery of systemic lupus erythematosus arthritis of the hand. Hand Clin 1996;12:591–602. [PubMed]
- 9.Nalebuff EA. Surgery of psoriatic arthritis of the hand. Hand Clin 1996;12:603–14. [PubMed]
- 10.Nalebuff EA, Garrett J. Opera-glass hand in rheumatoid hand. J Hand Surg 1976;1:210–20. [DOI] [PubMed]
- 11.Roberts ME, Wright V, Hill AG, Mehra AC. Psoriatic arthritis. Ann Rheum Dis 1976;35:206–12. [DOI] [PMC free article] [PubMed]
- 12.Rose JH, Belsky MR. Psoriatic arthritis in the hand. Hand Clin 1989;5:137–44. [PubMed]
- 13.Swanson AD. Flexible implant arthroplasty for arthritic finger joints. Rationale, technique, and results of treatment. J Bone Joint Surg 1971;54A:435–55. [PubMed]
- 14.Walton RL, Brown RE, Giansiracusa DF. Psoriatic arthritis mutilans: digital distraction lengthening: pathophysiologic and current therapeutic review. J Hand Surg 1988;13:510–5. [DOI] [PubMed]
- 15.Wright V. Psoriasis and arthritis, a re-evaluation. Am J Med 1959;27:454. [DOI] [PubMed]
- 16.Yoshida M, Belt EA, Kaarela K, Kauppi MJ, Shimamura T. Prevalence of mutilans-like hand deformities in patients with seropositive rheumatoid arthritis. A prospective 20-year study. Scand J Rheumatol 1999;28:38–40. [DOI] [PubMed]