Abstract
PURPOSE
In 2001, the World Health Organization published the International Classification of Functioning, Disability and Health (ICF). The ICF is just beginning to be used in a variety of clinical and research settings in Canada and worldwide. The purpose of the present article is to describe the initial use of the ICF at an Ontario children’s rehabilitation centre, and to consider further uses both within and outside the centre for enhancing services for children and youth with chronic physical health conditions and disabilities, as well as for their families.
METHOD
A description is provided on how the ICF has been used at the centre to guide clinical thinking and practice, and to justify and steer research directions. Plans underway to use the ICF to collect and record functional data at the centre are also described. Finally, recommendations for the use of the ICF to enhance communication among child health professionals across service settings are provided.
CONCLUSIONS
Used in conjunction with the International Classification of Diseases – Tenth Revision, the ICF’s conceptual framework and classification system shows great promise for enhancing the quality of services for children with chronic conditions and their families. This information may assist paediatric specialists, other child health professionals, researchers and administrators to use the ICF in similar settings. It may also stimulate exploration of the use of the ICF for general paediatricians and other service providers in the larger community.
Keywords: Canada, Children, Chronic illness, Disability, ICF, Paediatrics, Rehabilitation, Youth
Abstract
OBJECTIF
En 2001, l’Organisation mondiale de la santé a publié la Classification internationale du fonctionnement, du handicap et de la santé (CIF). La CIF commence tout juste à être utilisée dans divers milieux cliniques et de recherche au Canada et dans le monde. Le présent article vise à décrire l’utilisation initiale de la CIF dans un centre de réadaptation ontarien pour enfants et à envisager d’autres usages, à l’intérieur comme à l’extérieur du centre, afin d’améliorer les services aux enfants et aux adolescents atteints de troubles santé chroniques ou de handicaps, ainsi qu’à leur famille.
MÉTHODOLOGIE
Les auteurs fournissent une description du mode d’utilisation de la CIF au centre afin d’orienter la réflexion clinique et la pratique, ainsi que pour justifier et aiguiller les orientations de recherche. Ils décrivent également les projets d’utilisation de la CIF pour colliger et documenter les données fonctionnelles au centre. Enfin, ils font des recommandations sur l’utilisation de la CIF pour améliorer les communications entre professionnels de la santé infantile de divers services.
CONCLUSIONS
Utilisée conjointement avec la Classification internationale des maladies, 10e révision, le cadre théorique de la CIF est très prometteur pour améliorer la qualité des services aux enfants atteints d’un trouble chronique et à leur famille. Cette information peut aider les spécialistes en pédiatrie, les autres professionnels de la santé, les chercheurs et les administrateurs à utiliser la CIF dans des milieux similaires. Elle peut également inciter les pédiatres non spécialisés et d’autres dispensateurs de soins à explorer l’utilisation de la CIF dans l’ensemble de la collectivité.
Children with chronic physical health conditions and disabilities are increasing in prevalence and represent a substantial portion of the general population. Recent data indicate that just over 30% (approximately 700,000 children nationwide) of Canadian school-aged children have at least one chronic physical health condition or impairment (eg, asthma, epilepsy, heart disease or hearing loss) (1). Moreover, close to 4% of Canadian school-aged children are limited or prevented from participating in activities at home, school or elsewhere, due to a chronic physical health condition or impairment (1). The changing epidemiology of childhood disease and disability has had a dramatic impact on the daily practice and focus of child health professionals (2). Although diagnoses are important for defining cause and prognosis, assessment of function and the influence of context on function is often essential for planning interventions to optimize children’s community participation and quality of life (3).
Across the province of Ontario, 20 publicly funded rehabilitation centres provide services to children and youth with chronic physical health conditions and disabilities. The aim of the present article is to highlight how one of these centres, the Thames Valley Children’s Centre (TVCC) in London, Ontario, has utilized the World Health Organization’s (WHO) International Classification of Functioning, Disability and Health (ICF) (4) to guide clinical thinking and practice and to justify and steer research directions. Plans underway to use the ICF to aid health professionals and administrators in the collection and recording of functional data at the individual and aggregate level will also be described. Finally, recommendations for use of the ICF to encourage communication and collaboration among health professionals across service settings are provided.
A recent review of the literature of current applications of the ICF found few articles documenting implementation of the ICF in clinical and research settings (5). The reviewers suggest that this is because the WHO’s endorsement of the ICF is quite recent. The present article is among the first to illustrate and consider the utilization of the ICF for clinical, research and administrative purposes in a paediatric rehabilitation setting. The information provided may assist paediatric specialists and other child health professionals, researchers and administrators in comparable environments to use the ICF in similar ways, and may stimulate exploration of the use of the ICF for general paediatricians and other service providers in the larger community.
THE ICF
Published in 2001, the ICF has been accepted by 191 countries as the international standard to describe and measure health and disability (6). Rigorous studies have been undertaken to ensure that the ICF is applicable across cultures, age groups and sexes, to collect reliable and comparable data on health outcomes of people and populations. Canada and the United States are represented by the North American Collaborating Center, with respect to international activities related to the study and ongoing revision of the ICF (6).
The ICF classification system extends on conventional interpretations of health. While traditional health indicators are based on the mortality (death) rates or morbidity (disease) rates of populations, the ICF shifts the focus from ‘consequences of disease’ to ‘components of health’ or ‘functioning’ and how they can be improved to achieve a productive, fulfilling life (6). It provides a system for coding and documenting human functioning as well as the impact of the social and physical environment on functioning. It is designed to be used together with the longstanding International Classification of Diseases and Related Health Problems – Tenth Revision (ICD-10) (7) to provide a more comprehensive picture of the health of people and populations (4).
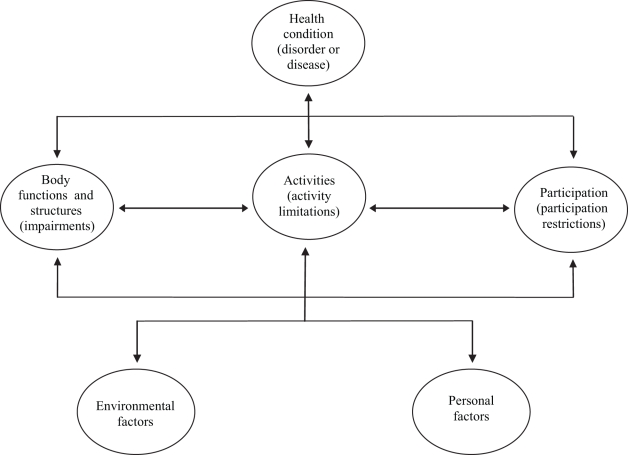
In addition to the classification system, the ICF provides a conceptual framework for understanding functioning and disability that is based on a biopsychosocial perspective of health (4). Functioning is considered to be an umbrella term that encompasses all aspects of human functioning at the body, individual and societal levels. Disability is an umbrella term that encompasses all functional difficulties at these three levels. Impairments are defined as problems in body function or structure; activity limitations are difficulties a person may have in carrying out daily activities; and participation restrictions are problems a person may experience when involved in life or social situations. A person’s functioning and disability, including a person’s participation in life, are depicted as arising from the interaction between health conditions and environmental and personal factors (4) (Figure 1). Environmental factors that may influence functioning include a number of domains related to the physical, social and attitudinal environment in which people live (eg, air quality, peer relationships, service availability and social norms). Personal factors include age, sex, ethnicity, personal beliefs, lifestyle, habits, etc.
Figure 1.
The World Health Organization’s (WHO) Model of Functioning and Disability. Source: The WHO, 2001
The ICF classification system and conceptual framework is intended for use within and across multiple sectors, such as health promotion, rehabilitation, education, insurance, policy and statistics (8). Within each sector, the ICF can be used for multiple clinical (eg, needs assessment), research (eg, outcome measurement), statistical (eg, collection and recording of data) and other purposes.
THE TVCC
The TVCC is one of 20 regional rehabilitation centres in Ontario that provide services for children and youth with physical disabilities, communication disorders and developmental delays. The TVCC serves over 6000 children living primarily in southwestern Ontario. The TVCC provides community-based rehabilitation services that support participation in all areas of life for children and youth.
Close to 300 health professionals provide services to clients and their families within these services and programs, and include a developmental paediatrician, a nurse, occupational therapists, physiotherapists, speech and language pathologists, psychometrists, psychologists, social workers, recreation therapists, behaviour therapists, ability educators, service coordinators, technical specialists and therapy assistants. Paediatric medical, surgical and dental specialists provide medical services at multidisciplinary clinics at the TVCC. Other health professionals also attend many of the clinics, acting as a resource to clients, families and community service providers. Moreover, the TVCC offers a range of family and community resources to clients and their families. Additional resources, such as community relations and research, support each of the clinical service areas.
Of the 20 Ontario children’s rehabilitation centres, the TVCC is one of two centres to have an in-house research program. Over a 17-year period, 95 research projects have been completed and have involved various combinations of research, clinical and administrative staff, clients of TVCC and their family members, and external partners as study investigators.
EMPLOYING THE ICF AT THE TVCC
Clinical thinking and practice
To date, the ICF’s conceptual framework (and earlier versions of the framework) has had a clear impact on clinical thinking and practice at the TVCC at the service delivery model level and the services and programs level, and is beginning to have an influence at the client assessment level.
In 2000, the TVCC adopted the ‘Life Needs Model’ of paediatric service delivery (9,10). The Life Needs Model was developed by the research director of the TVCC, in collaboration with clinical directors, service providers and centre administrators. It is based on research evidence relating to the particular needs of children with disabilities, their families and their communities. The Life Needs Model has been instrumental in moving the TVCC away from a model of service delivery that focuses on diagnosis and impairment-based interventions toward a service delivery model based on a broader view of children, family and community needs.
The ICF’s conceptual framework (and its predecessors) was one of the frameworks, along with a number of other frameworks, theories and models, such as quality of life frameworks for persons with developmental disabilities (11), theories of human development (12) and models of family-centred care (13) that influenced the development of the TVCC’s unique model of service delivery. The Life Needs Model, like the ICF, adopts a biopsychosocial model of disability and recognizes the importance of addressing functional difficulties at the body function and structure, activity and participation levels. The model also recognizes the need to identify personal and environmental factors that support the participation of children and youth with chronic conditions and disabilities. Moreover, the model extends on the ICF conceptual framework by specifying a broad range of services required to meet clients needs at all of these levels.
The TVCC’s model of service delivery, like the ICF, focuses on the strengths of children and their families, rather than on the consequences of disease. The TVCC espouses a philosophy of enablement and equality for all children and youth. Services and programs are provided on a continuum that meets the ongoing needs of clients as they progress from infancy to early adulthood. The ultimate goal of the Life Needs Model is to meet the needs of children and youth so that they are personally satisfied with their level of participation in their communities and, therefore, with their quality of life.
Informed by the ICF and other frameworks and theories, the TVCC’s model of service delivery has broadened awareness of how and where services can be provided and the types of outcomes that are important. Before 1997, only eight summer group programs were available and none were community based. Since 2000, services have become increasingly community based, focusing on children, family and community needs. By 2006, services and programs were being provided in over 400 community settings, as well as in hundreds of families’ homes. Functioning in daily activities and participation are targeted as primary outcomes for children. Community partners have included schools, recreation centres, gymnasiums, karate centres, libraries and musical academies.
The TVCC has started to use the ICF for client assessment purposes. Assessment measures are being used at intake that capture ICF components, and include questions about children’s functioning at the body, individual and social level, as well as questions about personal and environmental factors that may influence functioning. Service coordinators and other health professionals have included these questions in their assessments of strengths and needs to ensure a holistic intervention approach is taken toward each child and family.
Research applications
Evaluation of the utility of the ICF as a foundation for health research is only just beginning (3). The TVCC has used the ICF in research, thus far, as a tool to justify the focus on multiple components of disability, and on environmental factors in studies of child health; to define study constructs; and to identify desirable outcomes of services in program evaluation. For example, researchers at the TVCC undertook an epidemiological investigation to examine the effect of health status, environmental and child factors on children’s prosocial behavior and academic performance (14), using the National Longitudinal Survey of Children and Youth (Statistics Canada, funded by Health Canada). The study also involved producing a national profile of chronic physical health conditions and disabilities among school-aged children in Canada (1). Health conditions, impairments, activity limitations and participation were all defined based on the distinct definitions provided by the ICF. Survey items in the National Longitudinal Survey of Children and Youth representing these constructs had previously been identified for use in the study by mapping survey items onto ICF codes (15). Study findings indicated the usefulness of defining health constructs in terms of the ICF.
One of the strategic directions of the research program at the TVCC is to evaluate the centre’s clinical interventions and programs. As described, the ICF has provided justification for targeting children’s functioning in daily activities and participation as primary outcomes of these interventions and programs. Therefore, several evaluation studies (16–18) conducted at the TVCC have focused on examining the extent to which these outcomes have been realized. In addition, due to the recognition of the potential influence of various environmental factors on children’s functioning, client and family satisfaction with services, the process of service delivery and family outcomes have also been assessed in evaluation studies.
Administrative applications
At the TVCC, and other Ontario children’s rehabilitation centres, client demographic and medical data (including ICD codes) are maintained within a client information system especially designed for rehabilitation centres. There is a growing recognition among disability researchers and administrators of Ontario children’s rehabilitation centres of the utility of also collecting functional data for clients and including it within such a system (19,20). Along with other children’s rehabilitation centres in Ontario, the TVCC has participated in a project working to develop a system-wide method for collecting client functional data that incorporates the ICF framework (20).
Researchers and administrators at the TVCC are in the process of developing an abbreviated version of the ICF in a form similar to that of the WHO’s ICF checklist (21), which includes ICF categories and codes relevant to paediatric rehabilitation services. As previously described, the ICF framework has been used at the TVCC as a general guideline for choosing the types of questions to include in the assessments of clients functioning at intake. The checklist could be used as a more standardized approach to assess individual client functioning at intake and for aggregating functional data across clients. Analyzing client functional data at the aggregate level is important for the determination of service utilization, need for care, effectiveness and cost-effectiveness of services, or functional outcomes (22), and can serve to strengthen and support the findings of other research activities. Diagnostic data alone cannot answer these types of questions. Moreover, ICD-10 and ICF codes can be used together to provide important health information about children. Recent research has demonstrated that ICD-10 and ICF codes can be jointly used as a common language to document disability characteristics of children in early intervention (23).
Table 1 provides a list of the chapters in the ICF and their level 1 codes. Personal factors have not been assigned codes in the current edition of the ICF (4). Their method of assessment is left to the user. However, future directions for the ICF include development of a personal factors component (4). Level of severity of functioning can be quantified for all chapters using the same generic scale provided in the ICF, ranging from 0 (no problem) to 4 (complete problem), or at the users discretion, coding scales can be created to capture positive aspects of functioning (4). The level 2 codes falling within those chapters most relevant to paediatric rehabilitation services are being included in the checklist for use at TVCC. Plans are to supplement the checklist with codes from the International Classification of Functioning, Disability and Health – Children and Youth (24), that was just published in 2007.
TABLE 1.
List of chapters in the International Classification of Functioning, Disability and Health and their level 1 codes
| Body functions and structures | |
|---|---|
| b1 | Mental functions |
| b2 | Sensory functions and pain |
| b3 | Voice and speech functions |
| b4 | Functions of the cardiovascular, hematological, immunological and respiratory systems |
| b5 | Functions of the digestive, metabolic and endocrine systems |
| b6 | Genitourinary and reproductive functions |
| b7 | Neuromusculoskeletal and movement-related functions |
| b8 | Functions of the skin and related sturctures |
| s1 | Structures of the nervous system |
| s2 | Eye, ear and related structures |
| s3 | Voice and speech structures |
| s4 | Cardiovascular, immunological and respiratory structures |
| s5 | Digestive, metabolic and endocrine structures |
| s6 | Genitourinary and reproductive structures |
| s7 | Structures related to movement |
| s8 | Skin structures |
|
Activity and participation | |
| d1 | Learning and applying knowledge |
| d3 | Communication |
| d5 | Self-care |
| d6 | Domestic life |
| d7 | Interpersonal relationships |
| d8 | Major life areas |
| d9 | Community and social life |
|
Environmental factors | |
| e1 | Products and technology |
| e2 | Natural environment |
| e3 | Support and relationships |
| e4 | Attitudes |
| e5 | Services, systems and policies |
Source: The WHO, 2001
Extending clinical applications
In addition to using the abbreviated checklist to collect individual client functional data at intake to support a holistic intervention approach, the checklist could also be modified as required and used by the centre’s paediatric medical, surgical and dental specialists, and other health professionals for multidisciplinary assessment of individual clients at specialized clinics. Rentsch et al (25) developed similar checklists based on relevant categories and codes from the ICF for use by different specialized teams in an acute care neurorehabilitation unit.
The benefits of using the ICF for individual client assessment are not limited to paediatric rehabilitation professionals and settings. Medical professionals in the area of child health, such as general paediatricians, and other community service providers may also benefit from approaching a patient’s health concerns in terms of the ICF conceptual framework or using similar abbreviated checklists based on the ICF, in conjunction with the ICD-10, to ensure a comprehensive assessment of an individual child’s health and functioning (23).
Changing rates and survival of children with chronic health conditions and disabilities are changing the nature of paediatric practice (2). All general paediatricians will either treat children with chronic conditions and disabilities themselves or provide referrals for rehabilitation or other types of community services. The ICF offers a way to communicate across the continuum of care from acute to community care (26). The ICF (and the recently published ICF – Children and Youth) provides a common language for assessing the functional status of children and youth that can enhance communication and collaboration among general paediatricians, paediatric subspecialists, other health care professionals, social service professionals and community agencies regarding the changing needs of children and youth, and their families. This is not to suggest that medical, rehabilitation and social service professionals will all change the idiosyncratic terminology of their respective disciplines. Lollar and Simeonsson (3) suggest, however, that it is reasonable for a second language to be a part of the interaction among professionals across service settings and systems so that intervention efficiency can be increased. The opportunity for identifying, classifying and coding impairments, activity limitations, participation restrictions and environmental factors related to functioning, in addition to diagnosis, opens a crucial clinical dimension (3).
CONCLUSION
The WHO’s most recently published classification system, the ICF, has been accepted by hundreds of countries around the world, including Canada, as the international standard to describe and measure functioning, disability and health. Applications of the ICF have just begun to occur in a wide variety of clinical and research settings (6). The present article has described how the ICF (and its predecessors) has been used to date at the TVCC, a children’s rehabilitation centre in Ontario. Researchers and program directors have played a primary role in introducing and incorporating the ICF into centre activities. The initial and greatest impact of the ICF, thus far, has been at the conceptual and services and programs level, influencing the centre’s service delivery model, the focus of services and programs and research directions. As the ICF becomes better known by clinical and administrative staff, it is the expectation that the ICF’s conceptual framework and classification system will be further integrated into everyday practice, serving as a common language for multidisciplinary client assessment, goal setting and evaluation (26), and the collection of functional data. The ICF has the potential to not only provide a common conceptual approach and terminology for addressing children and youth health and functioning across disciplines within the centre, but across associated service settings and systems as well. Essential to the adoption and broader use of the ICF are dissemination of the system and education and training of potential users (3). Additional information about and training materials for the ICF can be accessed from the ICF’s homepage (6). The employment of the ICF in one of Ontario’s children’s rehabilitation centres indicates that this conceptual framework and classification system shows great promise for enhancing the quality of services for children and youth with chronic physical health conditions and disabilities and their families, and ultimately, their quality of life.
REFERENCES
- 1.McDougall J, King G, deWit DJ, et al. Chronic physical health conditions and disability among Canadian school-aged children: A national profile. Disabil Rehabil. 2004;26:35–45. doi: 10.1080/09638280410001645076. [DOI] [PubMed] [Google Scholar]
- 2.Perrin JM. Advocacy and child health. Ambul Pediatr. 2004;4:267–8. doi: 10.1367/1539-4409(2004)4<267:AACH>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Lollar DJ, Simeonsson RJ. Diagnosis to function: Classification for children and youths. J Dev Behav Pediatr. 2005;26:323–30. doi: 10.1097/00004703-200508000-00012. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. International Classification of Functioning, Disability and Health. Geneva: World Health Organization; 2001. [Google Scholar]
- 5.Bruyère S, VanLooy S, Peterson D. The International Classification of Functioning, Disability and Health: Contemporary literature overview. Rehabil Psychol. 2005;50:113–21. [Google Scholar]
- 6.World Health Organization. International Classification of Functioning, Disability and Health. < http://www.who.int/classifications/icf/site/icftemplate.cfm> (Version current at February 4, 2008)
- 7.World Health Organization. International Statistical Classification of Diseases and Related Health Problems – 10th revision. Geneva: World Health Organization; 1992. [Google Scholar]
- 8.Stucki G, Cieza A, Ewert T, Kostanjsek N, Chaterji S, Üstün TB. Application of the International Classification of Functioning, Disability and Health (ICF) in clinical practice. Disabil Rehabil. 2002;24:281–2. doi: 10.1080/09638280110105222. [DOI] [PubMed] [Google Scholar]
- 9.King G, Tucker MA, Baldwin P, Lowry K, LaPorta J, Martens L. A life needs model of pediatric service delivery: Services to support community participation and quality of life for children and youth with disabilities. Phys Occup Ther Pediatr. 2002;22:53–77. [PubMed] [Google Scholar]
- 10.King GA, Tucker MA, Baldwin PJ, LaPorta JA. Bringing the Life Needs Model to life: Implementing a service delivery model for pediatric rehabilitation. Phys Occup Ther Pediatr. 2006;26:43–70. [PubMed] [Google Scholar]
- 11.Raphael D, Brown I, Renwick R, Rootman I. Assessing the quality of life of persons with developmental disabilities: Description of a new model, measuring instruments, and initial findings. Int J Disabil Dev Educ. 1996;43:25–42. [Google Scholar]
- 12.Bronfenbrenner U, Morris P. The ecology of developmental processes. In: Damon W, Lerner R, editors. Handbook of Child Psychology: Volume 1 – Theoretical Models of Human Development. 5th edn. New York: John Wiley; 1998. pp. 993–1028. [Google Scholar]
- 13.Rosenbaum P, King S, Law M, King G, Evans J. Family-centred service: A conceptual framework and research review. Phys Occup Ther Pediatr. 1998;18:1–20. [Google Scholar]
- 14.King G, McDougall J, DeWit DJ, et al. Pathways to children’s academic performance and prosocial behavior: Roles of physical health status, environment, family, and child factors. Int J Disabil Dev Educ. 2005;52:313–44. [Google Scholar]
- 15.McDougall J, Miller LT. Measuring chronic health condition and disability as distinct concepts in national surveys of school-aged children in Canada: A comprehensive review with recommendations based on the ICD-10 and ICF. Disabil Rehabil. 2003;25:922–39. doi: 10.1080/0963828031000122249. [DOI] [PubMed] [Google Scholar]
- 16.Evans J, McDougall J, Baldwin P. An evaluation of the “Youth en Route” program. Phys Occup Ther Pediatr. 2006;26:63–87. [PubMed] [Google Scholar]
- 17.King G, McDougall J, Tucker MA, et al. An evaluation of functional, school-based therapy services for children with special needs. Phys Occup Ther Pediatr. 1999;19:5–29. [Google Scholar]
- 18.McDougall J, Servais M, Sommerfreund J, et al. An evaluation of the Paediatric Acquired Brain Injury Community Outreach Programme (PABICOP) Brain Inj. 2006;20:1189–205. doi: 10.1080/02699050600975541. [DOI] [PubMed] [Google Scholar]
- 19.Rosenbaum P, Jaffer S, Russell D. Measuring outcomes for children with special needs and their families: Part 2. McMaster University. Hamilton: CanChild – Centre for Childhood Disability Research; 2006. [Google Scholar]
- 20.Rosenbaum P, Jaffer S, Russell D, et al. Measuring outcomes for children with complex needs and their families. McMaster University, Hamilton: CanChild – Centre for Childhood Disability Research; 2005. [Google Scholar]
- 21.World Health Organization. ICF checklist. Geneva: World Health Organization; 2001. [Google Scholar]
- 22.Ustün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: A tool for understanding disability and health. Disabil Rehabil. 2003;25:565–71. doi: 10.1080/0963828031000137063. [DOI] [PubMed] [Google Scholar]
- 23.Simeonsson RJ, Scarborough AA, Hebbeler KM. ICF and ICD codes provide a standard language of disability in young children. J Clin Epidemiol. 2006;59:365–73. doi: 10.1016/j.jclinepi.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. International Classification of Functioning, Disability and Health: Child and youth version. Geneva: World Health Organization; 2007. [Google Scholar]
- 25.Rentsch H, Bucher P, Dommen Nyffler I, et al. The implementation of the ‘International Classification of Functioning, Disability and Health’ (ICF) in daily practice of neurorehabilitation: An interdisciplinary project at the Kantonsspital of Lucerne, Switzerland. Disabil Rehabil. 2003;25:411–21. doi: 10.1080/0963828031000069717. [DOI] [PubMed] [Google Scholar]
- 26.Stucki G, Ewert T, Cieza A. Value and application of the ICF in rehabilitation medicine. Disabil Rehabil. 2003;25:628–634. doi: 10.1080/09638280110070221. [DOI] [PubMed] [Google Scholar]