Abstract
Objective
It has been shown that girls from families in which mothers and fathers had high dietary intake and low physical activity (i.e., obesigenic families) were at increased risk of obesity from ages 5 to 7 years. This follow-up study uses additional data collected when girls were 9 and 11 years old to examine whether girls from obesigenic families continued to show greater increases in BMI over time and reported unhealthy dietary and activity patterns.
Research Methods and Procedures
Families from the original cohort were reexamined when girls were 9 and 11 years of age. Parents' and girls' BMI, dietary intake, and physical activity and girls' percentage body fat and television viewing were assessed.
Results
In comparison with girls from non-obesigenic families, girls from obesigenic families showed greater increases in BMI and BMI z score from ages 5 to 7 years that were maintained across ages 7 to 11 years. Furthermore, girls from obesigenic families had higher percentage body fat at ages 9 and 11 years. These results were independent of parents' BMI. Additional findings showed that girls from obesigenic families had diets higher in percentage fat and had higher levels of television viewing than girls from non-obesigenic families.
Discussion
The environment that parents create, by way of their own dietary and physical activity behaviors, may have a lasting negative effect on children's weight trajectories and their emerging obesity risk behaviors, such as their dietary patterns. These findings further highlight the importance of the family in establishing children's obesity risk and the necessity of targeting parents of young children in obesity prevention efforts.
Keywords: family environment, children, gene-environment correlation, mother, father
Introduction
Obesity has multiple genetic and environmental determinants and is the result of a chronic energy imbalance, with energy intake exceeding expenditure. Parents provide children with both genes and environments, so it is not surprising that there are strong family resemblances in adiposity (1). For a child, the most powerful risk factor for becoming obese is having overweight parents (2). Behavior genetic analyses reveal substantial genetic influence on adiposity (3). Other evidence points to the importance of environmental or behavioral factors, including the percentage of energy from fat in the diet and physical activity, in explaining variability in adiposity or weight status (4). Although there has been much discussion and speculation regarding the specific environmental factors that promote obesity, the evidence base regarding environmental influences on obesity is still very limited.
The dramatic secular increases in the prevalence of obesity in both adults and children provide strong evidence that environmental changes play a powerful role in the development of obesity through effects on eating and activity patterns (5). For children, the family environment plays a central role in shaping their eating and activity patterns (6 -14). Parents' eating and activity patterns are essential components of family environments; parents serve as role models for children's eating and physical activity and influence children's access to food and opportunities for physical activity. A clear description of how the family environment influences the development of obesity among children will inform the development of effective prevention and treatment programs for childhood obesity.
In previous studies, based on a longitudinal sample of girls and their parents, we have shown that parents' obesity-related behaviors, including their dietary intake and physical activity behaviors, aggregate within and across family members. Specifically, mothers and fathers who show poor dietary patterns also report low levels of physical activity (15). In addition, mothers and fathers showed similarities in their obesity-related behaviors, suggesting that children are often exposed to two parents modeling either healthy or unhealthy dietary and activity behaviors (15). Building on this information, we examined whether distinctive family groups could be identified using only information on mothers' and fathers' dietary and physical activity behaviors (4). Using data from the first time-point in the longitudinal study, when girls were 5 years old, two distinctive family clusters emerged, which were labeled obesigenic and non-obesigenic families. Mothers and fathers from obesigenic families reported significantly higher levels of total energy and dietary fat intake and significantly lower levels of physical activity than mothers and fathers from non-obesigenic families. More importantly, although girls from the obesigenic and non-obesigenic families did not differ in their BMI and their skinfold thickness at age 5, girls from obesigenic families showed greater increases in BMI and skinfold thickness between ages 5 and 7. As a consequence, they were significantly more overweight at age 7 than girls from non-obesigenic families. These findings were noteworthy because they tested and confirmed the idea that parents create environments by way of their own behaviors that can promote, or protect their children from, accelerated weight gain.
Additional data from when girls in this sample were 9 and 11 years old are now available, thus comprising four waves of assessment at 2-year intervals for girls, mothers, and fathers (i.e., when girls were 5, 7, 9, and 11 years old). Using these additional waves of data, this study builds on the findings of Davison and Birch (4) in a number of important ways. First, differences in parents' dietary intake and physical activity patterns for the obesigenic and non-obesigenic families that were reported in Davison and Birch (4) will be re-examined at Times 2 to 4 (when girls were 7, 9, and 11 years) to determine whether parents maintained the distinctive eating and activity patterns identified at the initiation of the study. Second, differences in girls' weight status trajectories from ages 5 to 11 years will be examined for the two family clusters to determine whether girls from obesigenic families continued to show more rapid increases in BMI and body fat relative to girls from non-obesigenic families. Finally, differences in girls' dietary intake and physical activity behaviors, and patterns of change in these behaviors, will be examined. Information on girls' behavioral patterns was not presented in the original paper.
Research Methods and Procedures
Participants
Families were from central Pennsylvania and were part of a longitudinal study of the health and development of young girls. Eligibility criteria for girls' participation at the time of recruitment included living with both biological parents, the absence of severe food allergies or chronic medical problems affecting food intake, and the absence of dietary restrictions involving animal products; families were not recruited based on weight status or concerns about weight. Families were recruited for participation in the study using flyers and newspaper advertisements. In addition, families with age-eligible female children within a five-county radius received mailings and follow-up phone calls (Metro-mail Inc., Lombard, IL).
At entry into the study, participants included 197 5-year-old girls (mean age 5.4 ± 0.4) and their parents, of whom 192 families were reassessed 2 years later when girls were 7 years old (mean age 7.3 ± 0.3). A third assessment with 183 families was conducted 2 years later when girls were 9 years old (mean age 9.3 ± 0.3), followed by a fourth assessment with 177 families when girls were age 11 (mean age 11.3 ± 0.3). Therefore, 92% of the original sample was retained over the four measurement occasions. No significant differences in girls', mothers', or fathers' BMI at baseline (i.e., when girls were 5) were noted for families who participated at all times of assessment in comparison with families who dropped out of the study before girls were 11 years old. The Pennsylvania State University Institutional Review Board approved all study procedures, and parents provided consent for their family's participation before the study began.
Measures
Table 1 outlines the measures collected at each time of assessment and highlights the measures that were included in Davison and Birch (4) and the measures that are unique to this study. A general explanation of each measure for parents and girls is provided below.
Table 1.
Measures of girls', mothers', and fathers' weight status, dietary intake, and physical activity obtained at each time of assessment
| Time 1 (age 5) | Time 2 (age 7) | Time 3 (age 9) | Time 4 (age 11) | |
|---|---|---|---|---|
| MOTHERS AND FATHERS | ||||
| Weight status | BMI | BMI | BMI | BMI |
| Activity patterns | Sport participation | Sport participation | Sport participation | Energy expenditure from top five activities |
| Enjoyment of physical activity | Enjoyment of physical activity | Enjoyment of physical activity | ||
| Weekly exercise freq. | Weekly exercise freq. | Weekly exercise freq. | ||
| Inclination to be active | Inclination to be active | |||
| Dietary patterns | Energy intake | Energy intake | Energy intake | Energy intake |
| Percentage of intake as fat | Percentage of intake as fat | Percentage of intake as fat | Percentage of intake as fat | |
| Disinhibited eating | ||||
| GIRLS | ||||
| Weight status | BMI | BMI | BMI | BMI |
| Percentage body fat (DXA) | Percentage body fat (DXA) | |||
| Activity patterns | TV viewing | TV viewing | TV viewing | |
| Fitness | Fitness | |||
| Dietary patterns | Energy intake | Energy intake | Energy intake | Energy intake |
| Percentage of intake as fat | Percentage of intake as fat | Percentage of intake as fat | Percentage of intake as fat |
Bolded items indicate measures included in the original paper (4).
Parents' and Girls' BMI
At each time of assessment, girls' and parents' height and weight were measured in triplicate, and the average height and weight were used to calculate their BMI [weight (kilograms)/height (meters squared)]. Girls' age- and sex-specific BMI z scores were calculated using the Centers for Disease Control 2000 growth charts (16). BMI percentiles were similarly calculated and used to classify girls at risk of overweight (≥85th and <95th BMI percentile) and overweight (≥95th BMI percentile). In this study, girls who were at risk of over-weight and who were overweight were examined as a single group (i.e., BMI percentile ≥ 85). To simplify the presentation and discussion of results, this group is referred to collectively as overweight. Parents were classified as over-weight or obese using well-established BMI cut-offs of 25 and 30 kg/m2, respectively (17).
Girls' Percentage Body Fat
Girls' percentage of body fat was determined by DXA. A trained technician obtained measurements while children were in a supine position, wearing a paper gown and no shoes. Whole-body scans were taken using the Hologic QDR 4500W (S/N 47261) in the array scan mode and were analyzed using whole-body software, QDR4500 Whole Body Analysis. All scans were conducted at the Pennsylvania State University's General Clinical Research Center.
Parents' Dietary Patterns
Parents' dietary intake measures included total energy intake adjusted for body weight [using criteria outlined by Allison et al. (18)], percentage of energy intake from fat, and dietary disinhibition, or eating in an out-of-control manner in the absence of hunger. Total energy intake and percentage fat intake were assessed using a food frequency questionnaire developed by Kristal et al. (19). Mothers' and fathers' energy intakes were adjusted for body weight by regressing weight in kilograms onto energy intake and saving the residuals; the residuals were used in all analyses (18). Parents' dietary disinhibition was assessed using the disinhibition subscales (including internal and external disinhibition) of the Dutch Eating Behavior Questionnaire (20). The internal consistency coefficient for the combined disinhibition subscale in this study at Time 1 was α = 0.95 for mothers and α = 0.93 for fathers.
Parents' Activity Patterns
Several measures of parents' physical activity were collected at each time of assessment, including parents' sport participation, weekly exercise frequency, enjoyment of activity, inclination to be active, and energy expenditure for their five most frequent activities. Parents' sport participation was assessed using an activity checklist developed in our laboratory, which included a list of 22 sports (e.g., aerobics, golf, hiking, swimming, and tennis). Parents were asked to indicate how frequently they participated in each sport (from 1, never to 5, always), and a total frequency score (ranging from 22 to 110) was derived by summing across each of the sports. Parents' weekly exercise frequency was assessed using the following question: “How many days a week do you exercise?” To assess enjoyment of physical activity, parents were asked to indicate how well the statement “I exercise for fun” described them using a three-point response option (1, does not describe me; 2, sort of describes me; 3, really describes me).
Parents' inclination to be active was measured using a revised version of the Children's Physical Activity scale. The Children's Physical Activity scale was developed by Tucker (1997) (21) as a measure of children's physical activity and participation in sedentary activities, such as television (TV)1 viewing. Slight wording changes were made to make the scale appropriate for use with adults. This measure showed good internal consistency in this study, with α ranging between 0.82 and 0.87 for mothers and fathers across measurement occasions. Parents' energy expenditure for their top five activities was calculated by asking parents to list their top five physical activities (including exercise, sports, and leisure activities involving physical activity) and for each activity to indicate whether the activity was moderate or vigorous, how long on average they typically did the activity, and how many days of the week they did the activity. An activity score, as outlined by Booth et al. (22), was created for each activity using the following formula: activity score (kilocalories per day) = intensity of activity (metabolic equivalent score) × duration of activity (hours) × frequency (days per week). Metabolic equivalent values were obtained from the Compendium of Physical Activities (23). The activity scores were then summed across the five activities.
Girls' Dietary Patterns
Girls' total daily energy intake and percentage of energy intake from fat were measured using three 24-hour recalls. Recalls were conducted with mothers and their daughters by trained staff at the Pennsylvania State University's Diet Assessment Center. Randomly selected days (two weekdays and 1 weekend day) were used to collect dietary data over a 2-week period during the summer and fall months.
Girls' Activity Patterns
Girls' fitness level (aerobic capacity) was assessed using the Progressive Aerobic Cardiovascular Endurance Run test developed by Leger and Lambert (24). The reliability and validity of the Progressive Aerobic Cardiovascular Endurance Run has been previously illustrated (25,26). Girls' inactivity was measured from mothers' reports of girls' TV viewing habits. Mothers were asked to report the number of hours girls watched TV on an average weekday and weekend day. The reports were used to derive girls' average daily hours of TV viewing [(5 × weekday hours + 2 × weekend hours)/7 days].
Statistical Analyses
Data were analyzed using SAS version 8.2 (SAS Institute, Inc., Cary, NC). Significance for all relationships was determined at a level of p < 0.05.
Identification of the Original Family Clusters
The original family clusters (or family groups) identified in Davison and Birch (4) were used as the basis of this study. A detailed description of the analyses used to identify the clusters is provided in the original paper. In summary, using the measures of parents' dietary intake and physical activity at Time 1, cluster analysis was used to identify groups of parents who showed similarity in their dietary and activity patterns. Grouping took place at the level of the family. Two family clusters were identified. These two groups displayed distinctive and contrary patterns of dietary and activity-related behavior and were given the labels of obesigenic and non-obesigenic. In the original paper, families in the obesigenic cluster reported significantly lower incomes than families in the non-obesigenic families. Thus, all analyses that follow were adjusted for income at study entry.
Attrition and Missing Data
The obesigenic and non-obesigenic family clusters were originally created using data from 192 of the 197 families at study entry (five families did not have sufficient data to be included or had outlying or unrealistic values) (4). At study entry, 94 families were classified as obesigenic and 98 families as non-obesigenic. The sample sizes for the obesigenic and non-obesigenic groups at each time of assessment were, respectively, 93 and 95 at Time 2 (age 7), 89 and 90 at Time 3 (age 9), and 89 and 84 at Time 4 (age 11). As previously mentioned, there were no differences in girls', mothers', or fathers' BMI for families who dropped out of the study before Time 4 and families who participated at all phases. The use of multilevel modeling for analyses assessing girls' growth, dietary, and physical activity trajectories (see below) enabled the use of all available data. That is, families with incomplete data were not dropped from the analyses.
Parents' Dietary and Physical Activity Patterns at Each Time of Assessment
Differences in parents' dietary intake and physical activity patterns at each time of assessment for the obesigenic and non-obesigenic families were examined to determine whether the groups remained distinctive over time. To this end, analyses were performed within time. Differences in selected dietary and physical activity variables (total energy intake, percentage of energy from fat, and weekly exercise frequency) for parents from obesigenic vs. non-obesigenic families were assessed at each time of assessment using analysis of covariance (ANCOVA) (see Tables 2 and 3). Group differences were not assessed for all dietary and activity variables due to the large number of variables measured. However, similar to Davison and Birch (4), a single dietary intake and physical activity score was created at each time of assessment using principal component analysis, which specified a single component. Differences in the mothers' and fathers' dietary intake and physical activity components at each time of assessment for the obesigenic vs. non-obesigenic families were assessed using ANCOVA (see Figure 1).
Table 2.
Mean dietary intake and physical activity scores for mothers from obesigenic and non-obesigenic families: group differences at each time of assessment
| Variable | Time | Obesigenic | Non-obesigenic | p |
|---|---|---|---|---|
| MOTHERS | ||||
| Total energy intake (kcal) | 1 | 1971.8 (78.4) | 1633.3 (55.6) | <0.001 |
| 2 | 1909.4 (81.5) | 1588.3 (58.8) | <0.001 | |
| 3 | 1777.3 (72.3) | 1615.4 (57.0) | <0.10 | |
| 4 | 1833.4 (73.2) | 1608.6 (60.1) | <0.05 | |
| Fat in diet (%) | 1 | 39.6 (0.6) | 31.7 (0.7) | <0.001 |
| 2 | 38.4 (0.7) | 33.6 (0.7) | <0.001 | |
| 3 | 40.2 (0.7) | 35.4 (0.7) | <0.001 | |
| 4 | 40.6 (0.6) | 37.0 (0.8) | <0.001 | |
| Weekly exercise frequency | 1 | 2.4 (0.2) | 3.5 (0.2) | <0.001 |
| 2 | 2.2 (0.2) | 3.3 (0.2) | <0.001 | |
| 3 | 2.1 (0.2) | 3.2 (0.2) | <0.001 | |
| 4 | No data | No data | ||
| BMI | 1 | 27.7 (0.7) | 25.1 (0.5) | <0.01 |
| 2 | 28.1 (0.7) | 25.5 (0.5) | <0.01 | |
| 3 | 28.7 (0.7) | 26.1 (0.5) | <0.01 | |
| 4 | 29.2 (0.8) | 26.1 (0.5) | <0.01 |
Obesigenic families, N = 94; non-obesigenic families, N = 98 (at study entry). Bolded items indicate data presented in the original paper (4).
Table 3.
Mean (SE) dietary intake and physical activity scores for fathers from obesigenic and non-obesigenic families: group differences at each time of assessment
| Variable | Time | Obesigenic | Non-obesigenic | p |
|---|---|---|---|---|
| FATHERS | ||||
| Total energy intake (kcal) | 1 | 2412.0 (79.0) | 1860.7 (63.4) | <0.001 |
| 2 | 2146.7 (82.1) | 1957.4 (79.9) | NS | |
| 3 | 2024.5 (76.4) | 2047.5 (79.9) | NS | |
| 4 | 1983.0 (85.5) | 2021.9 (79.8) | NS | |
| Fat in diet (%) | 1 | 38.7 (0.6) | 32.9 (0.7) | <0.001 |
| 2 | 39.4 (0.6) | 35.3 (0.6) | <0.001 | |
| 3 | 38.0 (0.6) | 36.1 (0.6) | <0.10 | |
| 4 | 39.5 (0.6) | 37.1 (0.8) | <0.05 | |
| Weekly exercise frequency | 1 | 1.9 (0.2) | 3.7 (0.2) | <0.001 |
| 2 | 2.2 (0.2) | 3.4 (0.2) | <0.001 | |
| 3 | 2.0 (0.2) | 3.4 (0.2) | <0.001 | |
| 4 | No data | No data | ||
| BMI | 1 | 28.6 (0.5) | 27.5 (0.4) | NS |
| 2 | 29.1 (0.5) | 27.8 (0.4) | <0.05 | |
| 3 | 29.5 (0.5) | 28.3 (0.4) | <0.10 | |
| 4 | 29.7 (0.5) | 28.6 (0.4) | NS |
Obesigenic families, N = 94; non-obesigenic families, N = 98 (at study entry). Bolded items indicate data presented in the original paper (4). NS, not significant.
Figure 1.
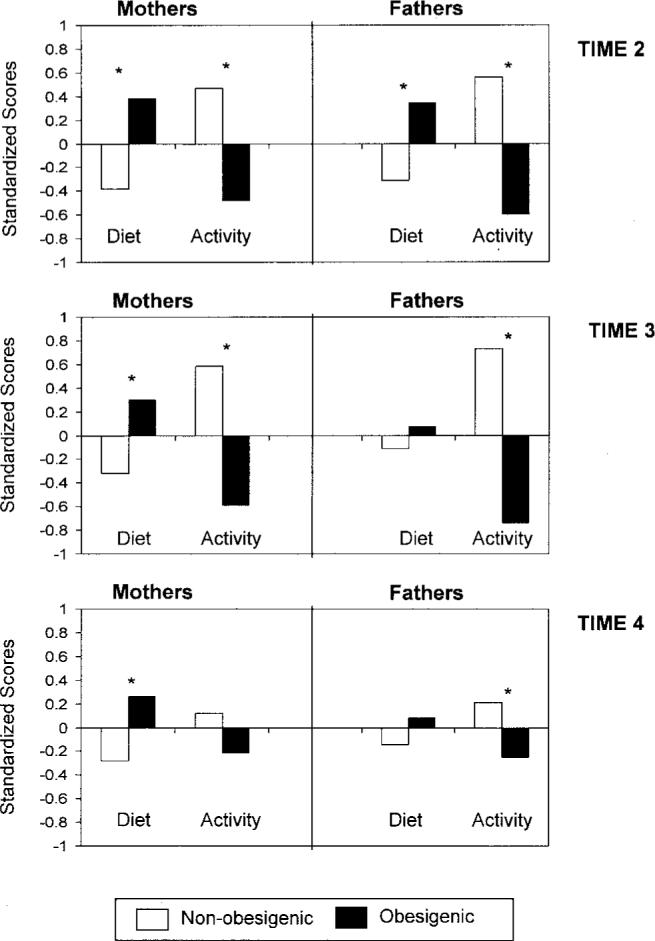
Physical activity and dietary intake component scores for mothers and fathers from obesigenic and non-obesigenic families at Times 2 to 4. * Means are significantly different (p < 0.05) across the family clusters.
Changes in Girls' BMI, Body Fat, Dietary Intake, and Physical Activity Patterns over Time
Initial analyses, using ANCOVA, examined family differences in girls' BMI and BMI z scores at each age. Differences in girls' BMI z score were assessed in addition to girls' BMI, the key outcome variable in the original study, to examine differences in girls' weight status independent of expected developmental changes in BMI. A mixed modeling approach (PROC MIXED using SAS) was used to perform the primary analyses of interest. Specifically, mixed modeling was used to assess patterns of change in BMI, BMI z scores, percentage body fat, energy intake, percentage of energy from fat, TV viewing, and fitness for girls from obesigenic vs. non-obesigenic families with children from ages 5 to 11 years (see Table 4 and Figure 2). Mixed modeling is a useful tool for analyzing repeated measures over time, and a major advantage is its ability to retain cases with one or more missing data points (27). For each outcome, differences in the average value over time and change over time were assessed for the two groups. For the purposes of this study, only the main effect of family membership and the interaction between family membership and time were of interest. A significant family membership effect indicates that, on average, girls in one family group had higher scores on the outcome variable over time than girls in the opposing family group. A significant interaction effect provides evidence for a differential pattern of change (or rate of growth) for girls from obesigenic and non-obesigenic families. Davison and Birch (4) found that parents in obesigenic families had significantly higher BMI scores than parents in non-obesigenic families when girls were 5 years old. Thus, mixed models were separately adjusted for mothers' and fathers' BMI.
Table 4.
Mean scores (SE) across time for each outcome variable for girls from obesigenic and non-obesigenic families
| Outcome | Family group | Time 1 | Time 2 | Time 3 | Time 4 | Main effect of family cluster | Interaction effect cluster*time |
|---|---|---|---|---|---|---|---|
| BMI | Obesigenic | 15.9 (0.1) | 16.9 (0.2) | 19.0 (0.3) | 20.6 (0.4) | No | Yes |
| Non-obesigenic | 15.7 (0.1) | 16.1 (0.2) | 17.8 (0.3) | 19.2 (0.4) | |||
| BMI z score | Obesigenic | 0.4 (0.1) | 0.5 (0.1) | 0.7 (0.1) | 0.7 (0.1) | No | Yes |
| Non-obesigenic | 0.2 (0.1) | 0.2 (0.1) | 0.3 (0.1) | 0.3 (0.1) | |||
| Body fat (%) | Obesigenic | 27.6 (0.7) | 28.2 (0.8) | Yes | No | ||
| Non-obesigenic | 25.2 (0.7) | 26.6 (0.8) | |||||
| Energy as fat intake (%) | Obesigenic | 31.2 (0.5) | 32.0 (0.5) | 32.7 (0.5) | 32.4 (0.5) | Yes | No |
| Non-obesigenic | 29.7 (0.5) | 30.3 (0.5) | 30.9 (0.5) | 32.3 (0.5) | |||
| Total energy intake (kcal) | Obesigenic | 1504.1 (35.6) | 1700.0 (36.8) | 1832.5 (35.8) | 1867.1 (48.9) | No | No |
| Non-obesigenic | 1548.4 (32.6) | 1695.9 (35.4) | 1808.8 (36.6) | 1807.2 (48.0) | |||
| TV viewing (h/d) | Obesigenic | 1.9 (0.1) | 2.0 (0.1) | 1.9 (0.1) | Yes | Yes | |
| Non-obesigenic | 1.7 (0.1) | 1.9 (0.1) | 1.9 (0.1) | ||||
| Fitness (no. of laps) | Obesigenic | 16.7 (0.7) | 17.6 (0.9) | No | No | ||
| Non-obesigenic | 16.2 (0.7) | 19.0 (0.9) |
Obesigenic families, N = 94; non-obesigenic families, N = 98 (at study entry). Bolded items indicate data presented in the original paper (4).
Figure 2.
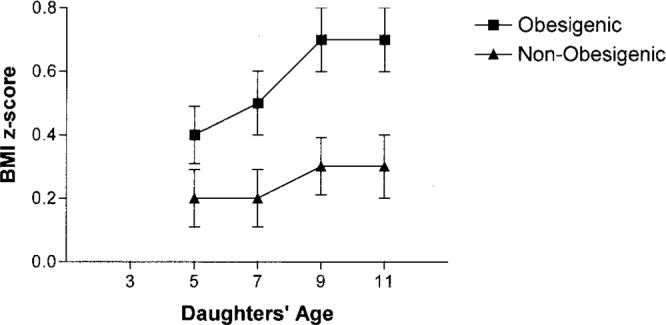
Mean BMI z score (SE) at each age for girls from obesigenic and non-obesigenic families. BMI z score trajectories were significantly different for girls from obesigenic vs. non-obesigenic families.
Results
Background Characteristics
On average, parents were in their mid 30s at the time of recruitment (mothers, 35.4 ± 4.8 years; fathers, 37.4 ± 5.4), when girls were age 5. Ninety-seven percent of fathers and 63% of mothers were employed when girls were 5. Fathers reported working an average of 45 hours a week, and mothers, an average of 18 hours a week. Approximately equal numbers of families reported incomes in the following ranges: $20,000 to $35,000, $35,000 to $50,000, and above $50,000 when girls were 5. At age 11, 62% of the families reported an income greater than $50,000. Parents were well-educated, with mothers reporting a mean of 15 ± 2 years (range, 12 to 20) of education and fathers reporting a mean of 15 ± 3 years (range, 12 to 20). In terms of parents' weight status, 52% of mothers and 73% of fathers were overweight at Time 1 and 55% and 79% respectively were overweight at Time 2. These figures increased to 60% and 82% at Time 3 and 58% and 87% at Time 4. Among girls, 18% (age 5), 20% (age 7), 30% (age 9), and 28% (age 11) had a BMI percentile ≥ 85.
Parents' Dietary Intake, Physical Activity, and BMI at Each Time of Assessment: Differences for Obesigenic and Non-obesigenic Families
Many of the differences in activity and dietary intake patterns for mothers and fathers from obesigenic and non-obesigenic families that were previously noted at baseline (4) persisted over the 6-year period from Times 1 to 4. In comparison with mothers from non-obesigenic families, mothers from obesigenic families reported significantly higher total energy intake and percentage fat intake and significantly lower weekly exercise frequency at all times of assessment; the only exception was differences in energy intake at Time 3, which was a trend (see Table 2). Similarly, in comparison with fathers from non-obesigenic families, fathers from obesigenic families reported significantly higher percentage fat intake and significantly lower weekly exercise frequency at all times of assessment; the one exception was differences in fathers' percentage fat intake at Time 3, which approached significance (see Table 3). Group differences in fathers' total energy intake did not persist beyond Time 1.
To examine whether overall dietary and physical activity patterns differed for the family groups, differences in the summary dietary intake and physical activity scores were also assessed (see Figure 1). Although differences in the summary scores for obesigenic and non-obesigenic families appeared to decrease over time, many of the group differences identified when girls were 5 years old remained statistically significant when girls were 7, 9, and 11 years old (Times 2 to 4). Mothers in obesigenic families had significantly higher intake component scores and significantly lower activity component scores than mothers in non-obesigenic families at all times of assessment; the only exception was differences between mothers' activity scores at Time 4, which fell short of significance (p < 0.10). Differences in fathers' intake component scores did not persist over time. That is, significant differences were noted at Time 2, but not at Times 3 and 4. Regarding fathers' activity component scores, however, compared with fathers in non-obesigenic families, fathers in obesigenic families had significantly higher activity scores at all time-points.
In the original study, mothers from obesigenic families had significantly higher BMI values when girls were 5 and 7 years old. Differences for fathers' BMI were only significant when girls were 7 years old. In the follow-up analyses, differences in mothers', but not fathers', BMI were maintained over time. Mothers from obesigenic families had significantly higher BMI values than mothers in the non-obesigenic group when girls were 9 and 11 years old (Table 2). Fathers from obesigenic families had marginally higher BMI values when girls were 9 years old; differences at age 11 did not approach significance (Table 3). Both family groups had a substantial proportion of members who were either overweight or obese. Specifically, over time, between 62% and 67% of mothers from obesigenic families and 43% and 53% of mothers from non-obesigenic families had BMI ≥ 25. Similar figures for fathers were 73% to 90% for non-obesigenic families and 73% to 83% for obesigenic families. Although both groups appeared to be gaining weight over time, there were no significant differences between obesigenic and non-obesigenic families in BMI change between baseline and Time 4 for mothers (1.5 ± 2.2 vs. 1.3 ± 2.7 kg/m2; F = 0.03, p > 0.05) or fathers (1.1 ± 2.0 vs. 1.1 ± 1.9 kg/m2; F = 0.01, p = 0.82).
Changes in Girls' BMI, Body Fat, Dietary Intake, and Physical Activity over Time: Differences between Obesigenic and Non-obesigenic Families
Data illustrating differences in measures of body composition, dietary intake, and physical activity across Times 1 to 4 for girls from obesigenic and non-obesigenic families are presented in Table 4. Previously, no family group differences in girls' BMI were noted when girls were 5 years old, but by age 7, girls from obesigenic families had significantly higher BMI values than girls from non-obesigenic families (4). In this study, differences evidenced at age 7 were also present at ages 9 (F = 6.5, p ≤ 0.05) and 11 (F = 7.6, p < 0.01) years; girls from obesigenic families had significantly higher BMI values than girls from non-obesigenic families. Similarly, no differences in girls' BMI z score were identified at age 5 (F = 0.98, p = 0.32). However, girls from obesigenic families had significantly higher BMI z scores at ages 7 (F = 5.3, p < 0.05), 9 (F = 6.2, p < 0.05), and 11 (F = 9.2, p < 0.05) than girls from non-obesigenic families.
Results from the mixed-model analyses revealed a significant interaction between family membership and time for girls' BMI (F = 5.8, p < 0.05) and BMI z score (F = 7.7, p < 0.01) with more rapid increases in each measure noted for girls from obesigenic families. These results remained significant after controlling for mothers' and fathers' BMI. The pattern of change in girls' BMI z score for each family group is illustrated in Figure 2. To examine whether the interaction between family membership and time was consistent over time or limited to particular time periods, differences in BMI z score change between consecutive time periods for girls from each family group were assessed using ANCOVA. Results showed that girls from obesigenic families exhibited significantly greater increases in BMI z score between ages 5 and 7 years (F = 7.2, p < 0.01) but not between ages 7 and 9 (F = 0.2, p = 0.62) or between ages 9 and 11 years (F = 0.2, p = 0.63). Differences in girls' percentage body fat over time were also examined. Results from the mixed model identified a significant family membership effect for girls' percentage body fat from ages 9 to 11 indicating that, on average, girls in obesigenic families had significantly higher levels of body fat over time (27.9%) than girls from non-obesigenic families (25.9%). The results for body fat were unaffected after controlling for fathers' BMI but were reduced to a trend after controlling for mothers' BMI (p < 0.10).
With respect to differences in dietary and physical activity patterns, a significant family membership effect was noted for girls' percent of energy intake from fat (F = 5.8, p < 0.05); girls in obesigenic families had a significantly higher percentage fat intake over time, compared with girls in non-obesigenic families (32.1% vs. 30.8%). These results were unaffected after controlling for mothers' and fathers' BMI. No significant differences emerged between obesigenic and non-obesigenic families for girls' total energy intake (1721.9 vs. 1705.5 kcal). A family membership effect was noted for girls' TV viewing (F = 4.5, p < 0.05), indicating that girls in obesigenic families watched more TV, on average, than girls in non-obesigenic families (1.9 vs. 1.8 hours). A significant interaction effect was also noted for girls' TV viewing (F = 4.4, p < 0.05); girls' increase in TV viewing from age 7 to 11 was significantly higher in girls in non-obesigenic families, compared with girls in obesigenic families. These differences remained significant after controlling for mothers' and fathers' BMI. For girls' fitness, neither the main effect of family membership nor the interaction between family membership and time were significant.
Discussion
Building on our previous work that showed that parents' eating and activity behaviors clustered within families to create obesigenic vs. non-obesigenic family environments (4,15), results from this study illustrate that these early family environments can have long-term effects on children's weight status and their dietary and activity patterns. Specifically, using the non-obesigenic and obesigenic family clusters identified in Davison and Birch (4), this study found that in comparison with girls from non-obesigenic families, girls from obesigenic families showed greater increases in BMI and BMI z score from ages 5 to 7 years that were maintained from ages 7 to 11 years. In addition, girls from obesigenic families had a higher percentage of body fat and had diets higher in fat. Results from this study in combination with our previous work confirm the necessity of focusing obesity prevention efforts on families and the importance of intervening before children enter school.
As reported in Davison and Birch (4), parents from obesigenic families had higher dietary intake scores and lower physical activity scores than parents from non-obesigenic families at the onset of the study when their daughters were 5 years old. This finding was a natural result of the cluster analysis that used information about dietary and activity behaviors to create distinctive family groups. The current study examined whether parents from each group maintained their distinctive behavioral patterns when girls were 7, 9, and 11 years old. With few exceptions, results indicated that the groups remained distinct over time, with parents from obesigenic families reporting less healthy dietary and physical activity patterns than parents from non-obesigenic families. As illustrated in Figure 1, however, group differences in parents' behaviors were less noteworthy over time. Given that parents from both groups gained weight over time and that a substantial proportion of parents from both groups were overweight, it appears that the non-obesigenic group adopted more obesity-promoting behaviors over time rather than obesigenic families adopting healthier lifestyles. Although the group differences in parents' behaviors were less apparent over time, results from this study suggest that early exposure to an obesity-promoting family environment can have long-lasting negative effects on children's BMI trajectories.
Accelerated increases in girls' BMI and BMI z score that were previously noted from ages 5 to 7 years among girls from obesigenic families were maintained, but not exacerbated, from ages 7 to 11 years. This pattern is noteworthy given that there were no differences in girls' BMI when they were 5 years old (4) and that their parents' dietary and physical activity behaviors became more similar over time. Differences in BMI trajectories for girls from each family group can be explained by both genetic and environmental factors. Girls from obesigenic families had parents who were more overweight and who adopted less healthy eating and activity behaviors. Thus, not only did their parents create an obesity-promoting family environment, they may also have passed on a genetic propensity to gain weight, providing a clear example of a gene-environment correlation (28). Separating genetic and environmental contributions in this situation is virtually impossible. However, when analyses controlled for parents' BMI, the general pattern of findings did not differ, indicating that the role of the family environment in children's obesity risk should not be underplayed or assumed to simply reflect genetic similarity.
Living in an obesity-promoting environment negatively affected girls' emerging dietary and activity behaviors. Girls from obesigenic families consumed a higher percentage of their energy intake from fat over time and reported higher levels of TV viewing. Surprisingly, girls from non-obesigenic families showed greater increases in TV viewing from ages 9 to 11 years than girls from obesigenic families. Given that the divergence in girls' BMI trajectories occurred between ages 5 and 7, it is possible that early years of TV viewing (similar to the early family environment) have long-lasting effects on children's obesity risk.
The primary strength of this study is its longitudinal design with data being collected on mothers, fathers, and daughters at four occasions over a 6-year period. Furthermore, a gold standard measure of body composition (i.e., DXA) and multiple measures of dietary intake and physical activity for girls and their parents were obtained. The key limitation of this study is the inability to generalize results beyond white, middle-income families. Additional work among families from different ethnic and educational backgrounds is needed to determine the applicability of the findings from this study to other family groups. In addition, findings from this study only pertain to girls. Although results are likely to be similar to boys, additional work is needed to confirm this possibility. Although measures were collected for girls and their parents, methods of assessment often differed for girls and their parents with less rigorous methods adopted for parents. On a related note, measures of girls' dietary intake were more rigorous than those for physical activity. Future work could expand on these findings using similar methods of assessment for all family members and by including objective measures of physical activity.
In conclusion, previous research from our laboratories highlights the influential role that parents' behaviors and parenting styles play in shaping children's obesity-related behaviors, including their dietary intake (6,7,14), physical activity (11,12), and TV viewing (13). Findings from Davison and Birch (4) and the current study corroborate and extend this body of research by showing that mothers' and fathers' eating and activity behaviors (and likely their parenting styles) cluster within families and that living in an environment in which mothers and fathers exhibit unhealthy dietary and physical activity patterns can have a negative effect on children's BMI trajectories and their obesity risk behaviors such as their dietary patterns. These findings clearly highlight the necessity of focusing obesity prevention efforts on parents and children and beginning such programs when children are young and their dietary and activity patterns are still being established.
Acknowledgments
This study was supported by NIH Grants HD 46567−01, HD 32973, and M01 RR10732.
Footnotes
Nonstandard abbreviations: TV, television; ANCOVA, analysis of covariance.
References
- 1.Maes HH, Neale MC, Eaves LJ. Genetic and environmental factors in relative body weight and human adiposity. Behav Genet. 1997;27:325–51. doi: 10.1023/a:1025635913927. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 3.Faith MS, Johnson SL, Allison DB. Putting the behavior into the behavior genetics of obesity. Behav Genet. 1997;27:423–39. doi: 10.1023/a:1025648316652. [DOI] [PubMed] [Google Scholar]
- 4.Davison KK, Birch LL. Obesigenic families: parents' physical activity and dietary intake patterns predict girls' risk of overweight. Int J Obes Relat Metab Disord. 2002;26:1186–93. doi: 10.1038/sj.ijo.0802071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–4. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 6.Birch L, Fisher J, Davison K. Learning to overeat: maternal use of restrictive feeding practices promotes girls' eating in the absence of hunger. Am J Clin Nutr. 2003;78:215–20. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Birch LL, Fisher JO. Mothers' child-feeding practices influence daughters' eating and weight. Am J Clin Nutr. 2000;71:1054–61. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Maternal milk consumption predicts the trade-off between milk and soft drinks in young girls' diets. J Nutr. 2001;131:246–50. doi: 10.1093/jn/131.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Parental influences on young girls' fruit and vegetable, micronutrient, and fat intakes. J Am Diet Assoc. 2002;102:58–64. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisher J, Mitchell D, Smiciklas-Wright H, Mannino M, Birch L. Meeting calcium recommendations from ages 5–9 reflects mother-daughter beverage choices and predicts bone mineral status. Am J Clin Nutr. 2004;79:698–706. doi: 10.1093/ajcn/79.4.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davison K, Cutting T, Birch L. Parents' activity-related parenting practices predict girls' physical activity. Med Sci Sports Exerc. 2003;35:1589–1595. doi: 10.1249/01.MSS.0000084524.19408.0C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davison K. Links between parent, peer and sibling activity-related support and adolescents' physical activity. J Phys Act Health. 2004;1:363–76. [Google Scholar]
- 13.Davison K, Francis L, Birch L. Parents' TV viewing and children's risk of exceeding television viewing recommendations. J Pediatr. 2005;147:436–42. doi: 10.1016/j.jpeds.2005.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Francis L, Birch L. Maternal influences on daughters' restrained eating behavior. Health Psychol. doi: 10.1037/0278-6133.24.6.548. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davison KK, Birch LL. Child and parent characteristics as predictors of change in girls' body mass index. Int J Obes Relat Metab Disord. 2001;25:1834–42. doi: 10.1038/sj.ijo.0801835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC Growth Charts: United States: Advance Data from Vital and Health Statistics: Report No. 314. National Center for Health Statistics; Hyattsville, MD: 2000. [PubMed] [Google Scholar]
- 17.World Health Organization . Obesity: Preventing and Managing the Global epidemic: Report of a WHO Consultation on Obesity: Report No.: WHO/NUT/NCD/98.1. World Health Organization; Geneva, Switzerland: 1998. [PubMed] [Google Scholar]
- 18.Allison D, Goran M, Poehlman E, Heymsfield S. Statistical considerations regarding the use of ratios to adjust data. Int J Obes Relat Metab Disord. 1995;19:644–52. [PubMed] [Google Scholar]
- 19.Kristal AR, Shattuck AL, Williams AE, Beresford SAA. Food frequency questionnaires for diet intervention research.. Proceedings of the 17th National Nutrient Database Conference.; Baltimore, MD: International Life Sciences Institute. 1992.pp. 110–25. [Google Scholar]
- 20.Van Strien T, Fritjers JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional and external eating behavior. Int J Eat Disord. 1986;5:295–315. [Google Scholar]
- 21.Tucker LA, Seljaas GT, Hager RL. Body fat percentage of children varies according to their diet composition. J Am Diet Assoc. 1997;97:981–6. doi: 10.1016/S0002-8223(97)00237-X. [DOI] [PubMed] [Google Scholar]
- 22.Booth M, Owen N, Bauman A, Gore C. Retest reliability of recall measures of leisure-time physical activity in Australian adults. Int J Epidemiol. 1996;25:153–9. doi: 10.1093/ije/25.1.153. [DOI] [PubMed] [Google Scholar]
- 23.Ainsworth B, Haskell W, Leon A, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Leger LA, Lambert J. A maximal multistage 20-m shuttle run test to predict VO2max. Eur J Appl Physiol. 1982;49:1–12. doi: 10.1007/BF00428958. [DOI] [PubMed] [Google Scholar]
- 25.van Mechelen W, Hlobil H, Kemper H. Validation of two running tests as estimates of maximal aerobic power in children. Eur J Appl Physiol. 1986;55:503–6. doi: 10.1007/BF00421645. [DOI] [PubMed] [Google Scholar]
- 26.Liu NYS, Plowman SA, Looney MA. The reliability and validity of the 20-meter shuttle test in American students 12 to 15 years old. Res Q Exerc Sport. 1992;63:360–5. doi: 10.1080/02701367.1992.10608757. [DOI] [PubMed] [Google Scholar]
- 27.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;23:323–55. [Google Scholar]
- 28.Wachs TD. The use and abuse of environment in behavior-genetic research. Child Dev. 1983;54:396–407. [PubMed] [Google Scholar]


