Abstract
Whether for conventional pretargeting, amplification pretargeting or affinity enhancement pretargeting, it will be necessary to conjugate an anti-tumor antibody as the first injectate. This laboratory is investigating phosphorodiamidate morpholinos (MORFs) for pretargeting and, accordingly, we are examining methods of attaching MORFs to anti-tumor antibodies that provide at least one group per molecule (gpm) without adversely influencing antibody properties. The aim of this investigation was to evaluate the commercial Hydralink™ for the conjugation of the anti-CEA MN14 antibody with an 18 mer amine-derivitized MORF.
Methods
The conjugation was approached in both directions by first reacting MN14 with the NHS derivatives of 4-hydrozinonicotinate acetone hydrazone (SANH) or 4- formylbenzoate (SFB) and then combined with MORF previously reacted with SFB or SANH to yield MN14 (SANH)-MORF and MN14 (SFB)-MORF respectively. The storage stability, immunoreactive fraction and the biodistribution in normal mice were compared for both conjugates. Thereafter, MN14 (SANH)-MORF was used in a pretargeting study in tumored nude mice and the results compared to that obtained historically with MN14-MORF prepared by carbodiimide (EDC) coupling.
Results
Both new methods of conjugation provided between 1 and 2 gpm compared to 0.2 achieved previously by EDC. Furthermore, by repeat SE HPLC with and without CEA, both showed unimpaired immunoreactive fraction. MN14 (SANH)-MORF tolerated long-term storage best. More importantly, when labeled by hybridization with 99mTc-labeled complementary MORF (99mTc-cMORF), the biodistribution of MN14 (SANH)-MORF was more favorable than that of MN14(SFB)-MORF in normal mice with lower liver (5.7 vs 9.4 %ID/g at 18 h) and spleen (3.5 vs. 8.4 %ID/g) accumulations and higher blood levels (4.8 vs. 3.4 %ID/g). Accordingly, only MN14 (SANH)-MORF was used in a pretargeting study in tumored mice. When targeted with 99mTc -cMORF and at 2 days post injection of antibody-MORF, the results obtained with 6 μg of antibody prepared in this way were essentially identical to that obtained previously with 30 μg of antibody prepared via EDC.
Conclusions
Hydralink was used successfully to conjugate MORF to MN14 at higher gpm than that achieved earlier and without obvious compromise of properties. Using MN14 (SANH)-MORF, the influence of the higher gpm on pretargeting permitted lowering the dosages of MN14 administered and may permit administering higher levels of radioactivity in connection with therapy.
Keywords: Pretargeting, conjugates, morpholino, monoclonal antibody, affinity enhancement
Introduction
Pretargeting has become an important approach to improve tumor targeting. In pretargeting, the long-circulating anti-tumor antibody conjugate is first administered and allowed time for specific localization in tumor and clearance from blood and other normal tissues before the injection of a short-circulating small radiolabeled effector. This technique has been shown to provide tumor targeting comparable to that of conventional targeting with directly labeled antibody but much earlier at 1–3 h post-administration of radiolabeled effector and, moreover, to dramatically improve the target/non-target ratio. The three approaches to pretargeting that have been reported thus far use biotin-(strep)avidin, bi-specific antibodies or oligonucleotides. Regardless of the approach, the high affinity and binding specificity of a tumor associated antibody is employed as the first injectate (1–5). The effector molecule is usually monovalent but bivalent effectors can show greatly enhanced residence time in tumor (6) by what has been called affinity enhancement (3, 7–8). This laboratory has recently begun exploring DNA and other oligomers, in particular phosphorodiamidate morpholios (MORFs), for amplification pretargeting (9–10), conventional pretargeting (4–5) and, most recently, affinity enhancement pretargeting (11). Our preliminary in vitro studies of affinity enhancement using surface plasmon resonance has shown that the target density is an important determinant of affinity enhancement pretargeting (12). One method of achieving the required higher density in MORF pretargeting is to increase the number of MORFs attached to each antibody. It therefore has become important to develop methods of conjugating anti-tumor antibodies with several MORFs per molecule and without compromise of antibody immunoreactivity or adversely influencing antibody pharmacokinetics. We reported herein on the use of commercially available reagents (Hydralink™) for the conjugation of the anti-tumor antibody MN14 with MORF (Scheme 1).
Scheme 1.
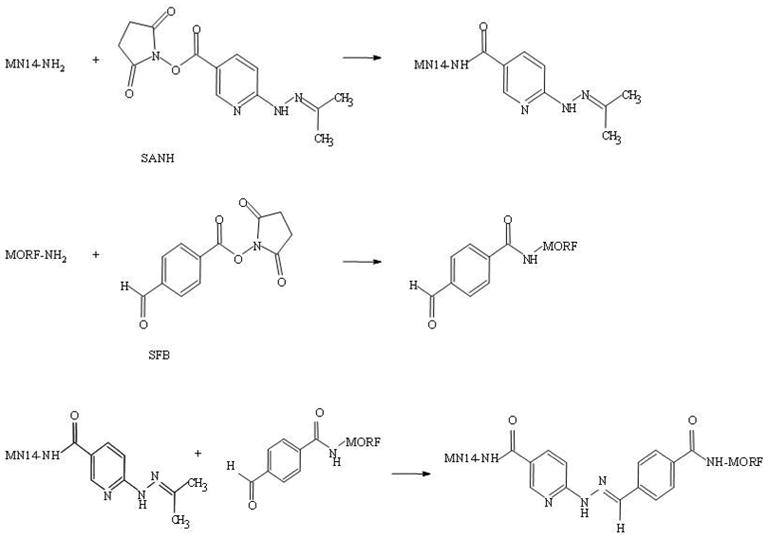
Hydralink approach to conjugation of MN14 with MORF.
Materials and Methods
Reagents
All MORFs were purchased from Gene Tools (Philomath, OR) with an amine group on the 3′ equivalent terminal for conjugation with either SANH/SFB or S-Acetyl mercaptoacetyltriglycine (MAG3). Each MORF was analyzed by the manufacturer using size-exclusion high-performance liquid chromatography (HPLC) and MALDI-TOF MS to ensure quality. The base sequences and molecular weights of the 18 mer MORF and its complement (cMORF) are shown below:
| MORF: | 5′-TCTTCTACTTCACAACTA-linker-amine, 6, 164 Da |
| cMORF: | 5′-TAGTTGTGAAGTAGAAGA-linker-amine, 6, 422 Da |
The linker is -C(O)CH2CH2NH2 for primary amine modification. A high-affinity murine anti-CEA antibody (MN14, IgG 1 subtype, MW 160 kDa) was a gift from Immunomedics (Morris Plains, NJ). The CEA antigen from human liver metastasis of a primary colon carcinoma (180 kDa) was purchased from Scripps Laboratories (San Diego, CA). NHS-MAG3 was synthesized in house [13] and the structure confirmed by elemental analysis, proton NMR and mass spectroscopy. The PD-10 column was purchased from Amersham Pharmacia Biotech (Piscataway, NJ). The 99mTc-pertechnetate was eluted from a 99Mo-99mTc generator (Bristol-Myers Squibb Medical Imaging Inc., North Billerica, MA). A commercially available conjugation kit (Hydralink™) consisting of acetone 5-(succinimidyloxycarbonyl)-pyridine-2-ylhydrazone (NHS-SANH), succinimidyl 4-formylbenzoate (NHS-SFB) and other reagents were purchased from Solulink (San Diego, CA). All other chemicals were reagent grade and were used without purification.
High Performance Liquid Chromatography
Size-exclusion HPLC analysis was performed on a Superose-12 HR10/30 column with an optimal separation range between 1 ×103 and 3 ×105 Da (Amersham Pharmacia Biotech, Piscataway, NJ) using 0.10 M pH 7.2 phosphate buffer as eluant at a flow rate of 0.6 ml/min. The HPLC was equipped with both an in-line radioactivity detector and a Waters 2487 dual wavelength absorbance detector (Milford, MA).
MN14-MORF Conjugation, evaluation and radiolabeling
For the preparation of MN14(SANH)-MORF, typically the MN14 antibody was incubated with a five to ten fold molar excess of NHS-SANH in 100 mM PBS (pH=8.0) for 1 h at room temperature. The reaction mixture was purified on a PD-10 column using conjugation buffer (pH 5, 100 mM MES, 150 mM NaCl) as eluant. At the same time, the MORF was incubated with a 50 fold molar excess of NHS-SFB in 100 mM PBS (pH=8.0) and after 1 h at room temperature, this reaction mixture was also purified on a PD-10 column with the same conjugation buffer. The degree of modification of both the SANH (hydrazine) modified MN14 (i.e. MN14(SANH)) and SFB (aldehyde) modified MORF (i.e. MORF(SFB)) were determined as described below. Thereafter, conjugation was achieved simply by mixing solutions of modified antibody with a five fold molar excess of modified MORF in conjugation buffer (pH=5.0) overnight. The product was purified by dialysis against 100 mM PBS buffer (pH=7.2) at 4 °C for 72 h and the purity of MN14-MORF established by HPLC. A similar procedures was applied to the conjugation and evaluation of MN14(SFB)-MORF.
MN14-MORF Immunoreactivity
A measurement of immunoreactivity (i.e. immunoreactive fraction) of the antibody conjugated by both methods was obtained by a HPLC shift assay of the antibody, radiolabeled by addition of trace 99mTc-cMORF, before and after the addition of a three fold molar excess of CEA. In this assay, immunoreactive antibody will bind to the excess CEA and shift to shorter elution times
Quantitation of hydrazine and aldehyde modification and MN14 conjugation
Originally, the intermediate incorporation of hydrazine or aldehyde on MN14 and the incorporation of MORF on MN14 was quantiated according to the manufacture’s recommendations. In the course of these measurements, a modified and simpler approach to quantitation was developed as described below.
Alternative quantitation of hydrazine and aldehyde modification of MN14
To the 10ul MN14 and NHS-SANH reaction mixture was added p-nitrobenzaldehyde in the 200ul conjugation buffer at a 10 fold molar excess and the solution incubated at room temperature for 2 h. The free and antibody-bound hydrazone was then analyzed by size exclusion HPLC. The average number of SANH groups on MN14 (gpm) was then calculated from the initial molar ratio of SANH to MN14 corrected by the molar ratio of the MN14-bound SANH peak to that of free SANH quantitated by UV absorbance at 380 nm. The quantitation of purified MN14 (SANH) was taken as the initial MN14 concentration times the dilution factor of hydrazone [i.e. MN14(SANH)] concentration before and after purification and assuming the same loss of MN14 and MN14(SANH) during purification. The quantitation of the aldehyde modification of MN14 was achieved in a similar fashion but with corresponding solution of 0.50 mM 2-hydrazinopyridine (2-HP) in 100 mM MES, pH 4.7.
Quantitation of MORF modification of MN14
Complete charcterization of the antibody-MORF conjugate requires measuring both the MORF gpm attached and the antibody concentration. In addition, for pretargeting, the “accessible” MORF gpm must also be measured since the number of MORF attached may not be equal to the number accessible. In this investigation, a method using UV absorbance at 265 nm and 280 nm was employed to measure the average number of attached groups (16).
Using a scanning UV spectrophotometer (U-2000, Hitachi Instruments, Inc, Danbury, CT), the maximum absorbance of MN14 was found to be at 280 nm and that of MORF at 265 nm (16). However since the SANH or SFB groups on MORF-conjugated MN14 contributes to UV absorbance, the UV absorbance of SANH and SFB was also measured by subtracting the absorbance of NHS from NHS-SANH or NHS-SFB at both wave lengths. Thus concentration curves were constructed by measuring the absorbance at different concentrations of native MN14, MORF, SANH and SFB at both 280 and 265 nm. Under the assumption that the absorbance coefficients of MN14 and MORF do not change after conjugation, it was possible to plot the ratio of MN14-MORFs absorbance at 265 nm and 280 nm vs. apparent gpm (i.e. molar ratio) of MORFs to MN14. This plot was also in agreement with the calculation based on derived equations from the relevant molar extinctions coefficients at 280 and 265 nm and then used to determine the MORF gpm “attached” in the conjugation solution by the absorbance ratio of 265 nm/280 nm of the MN14-MORF peak by size exclusion HPLC. The number of “accessible” groups was then determined by a size exclusion HPLC shift assay in which trace radiolabeled cMORF is added to the conjugation reaction mixture before purification.
Radiolabeling of cMORF
As previously described, cMORFs were conjugated with NHS-MAG3 via the 3′ derivatized amine [5]. Briefly, 1 mg of cMORF in 200 μl of 0.2 M pH 8.0 HEPES buffer was added to a vial containing 1.7–2.0 mg of S-acetyl NHS-MAG3. The vial was vortexed immediately and incubated for 1 h at room temperature. The cMORF was then purified on a 0.7×20 cm P4 column with 0.25 M pH 5.2 NH4OAc buffer as eluant. The peak fractions were pooled and were then adjusted from pH 5.2 to pH 7.6 with a pH 9.2 buffer (0.5 M Na2HCO3, 0.25 M NH4OAc, 0.175 M NH3). After heating for 20 min, the solution was again purified over P4 using the pH 5.2 NH4OAc buffer as eluant. The peak fractions were again pooled as before and the concentration quantitated by UV absorbance at 265 nm [5]. The 99mTc-cMORF-MAG3 was prepared and analyzed as described previously (5). Radiolabeling was achieved by first adding 99mTc-pertechnetate generator eluant to a solution of 25 uL of either cMORF-MAG3 (concentrations 0.2–0.4 μg/μL), 25 μL 0.25 mol/L ammonium acetate buffer, pH 5.2, 10 μL pH 9.2 tartrate solution (50 μg sodium tartrate dehydrate per μL), and 4 μL stannous chloride solution (1 μg stannous chloride dihydrate and 1 μg sodium ascorbate per μL in 10mmol/L HCl), followed by heating in boiling water for 20 min. The product was purified on a P-4 column with 0.1mol/L phosphate buffer, pH 7.2, as eluant.
Animal studies
All animal studies were performed with the approval of the UMMS Institutional Animal Care and Use Committee. The biodistribution of both MN14-MORFs radiolabled with trace 99mTc complementary MORF were evaluated in normal CD-1 mice (Charles River, Wilmington, MA). Each mouse was injected with 10 μg MN14-MORF in 200 μl with 3.70 MBq (100 μCi). After sacrifice either at 1 h or 18 h postinjection, blood and selected organs were removed, weighed, and counted in a NaI(Tl) well counter (Cobra II, Packard Instrument Company, CT) along with a standard of the injectate. Blood and muscle were assumed to constitute 7% and 40% of the body weight respectively. In the case of tumored mice, the tumored thigh was also excised for counting but after the skin and as much as possible of the muscle and bone had been removed. Radioactivity remaining in the carcass was measured in a dose calibrator. Summation of radioactivity in all organs sampled and in the remaining carcass was taken as the whole-body radioactivity.
Pretargeting comparison
Pretargeting studies were conducted in Swiss NIH nude mice (Taconic Farms, Germantown, NY) bearing LS174T tumors of 0.6–0.8 g. Each animal received either 6 or 30 μg MN14(SANH)-MORF 2 days before the administration of 0.2 μg or 1.0 μg respectively of 99mTc-cMORF with 3.70 MBq (100 μCi). Thus the ratio of pretarget to effector was kept constant. The animals were sacrificed at 3 h post injection of the radioactivity. The results are compared below with those obtained in the laboratory earlier in identical studies using MN14-MORF conjugate via EDC approach (5).
Results
Preparation and characterization of MN14-MORF conjugates
The average number of SANK and SFB groups per antibody was betweent 2–4 for both while the average number of MORFs incorporated was 1–2 per antibody. The yield in the modification of both the MORF and the antibody with SANH or SFB was 80–90% and the antibody yield in the final conjugation step was 50–80%. The immunoreactivity measurements showed that greater than 86% of both MN14-MORFs were shifted by the addition of the antigen. In the only apparent difference, MN14 (SFB)-MORF solution was cloudy and MN14 (SANH)-MORF clear after storage at refrigerator temperatures for 6 months. Analysis by HPLC of the former conjugate also showed lower recoveries. Typical HPLC profiles of radiolabeled MN14(SANH)-MORF before (panel A) and after (panel B) the addition of CEA antigen are presented in Figure 1 and show a shift of 86% the radioactivity to higher molecular weight as the antibody binds to its antigen. The profiles for MN14(SFB)-MORF) were essentially identical.
Figure 1.
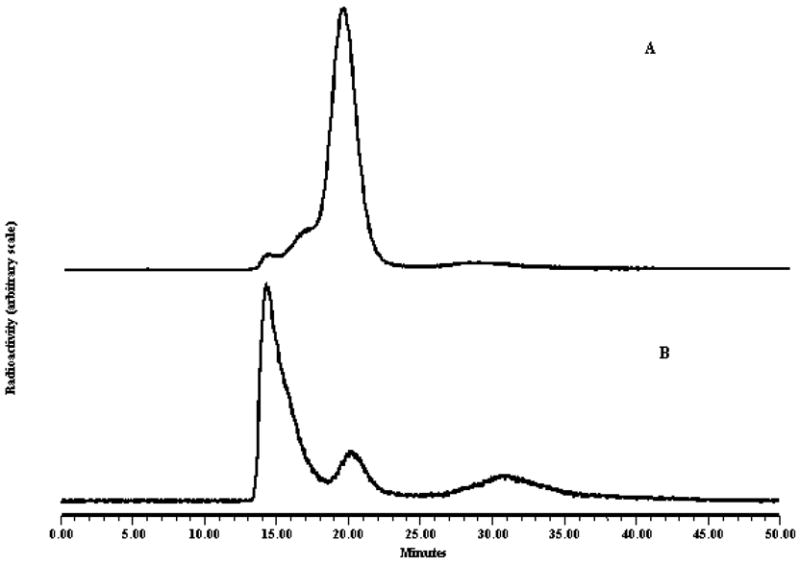
Size exclusion HPLC radiochromatograms of MN14(SANH)-MORF before (panel A) and after (panel B) the addition of CEA.
Both MN14 (SANH)-MORF and MN14(SFB)-MORF) were found to be virtually identical in properties. Averaged over two to six preparations, the attached MORFs per MN14 was identical within experimental error at 1.1–2.0 gpm while the average accessible MORF per MN14 was also identical at 1.0–2.0 gpm.
Figure 2 provides the standard curve (semilog scale) of gpm vs. the 265 nm and 280 nm absorbance ratio for mixtures of MN14 to which MORF was added at designated molar ratios. The results obtained in this manner show a 90% agreement with the results obtained by the hydrazone bond method described by the Hydralink manufacturer (data not presented).
Figure 2.
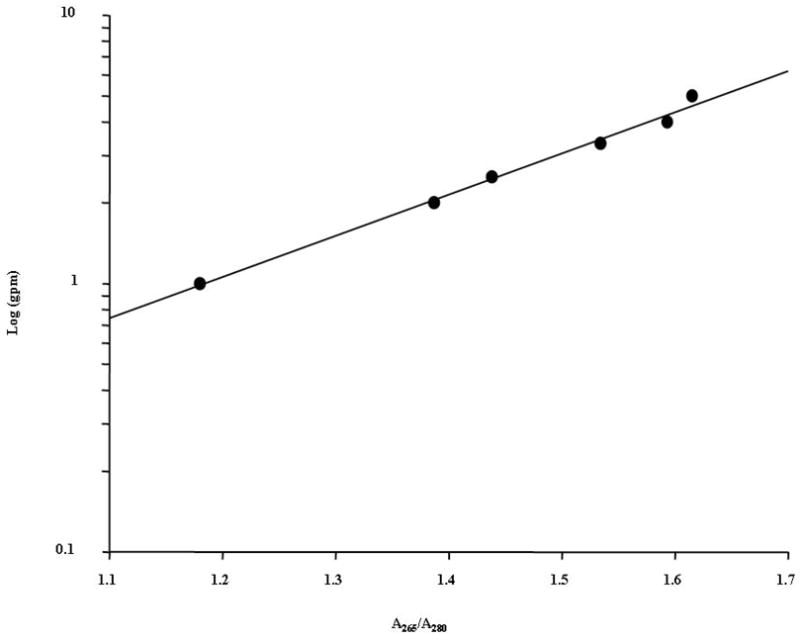
A standard curve for determination of MORF groups on MN14.
Animal studies
Table 1 compares the biodistribution in normal mice at 1 h and 18 h post-injection of both MN14(SFB)-MORF and MN14(SANH)-MORF radiolabeled by hybridization with 99mTc-cMORF. The results show no significant differences between the two conjugates except in the statistically higher liver and spleen values at 18h post-injection in the case of MN14 (SFB)-MORF (p < 0.05). Because of the lower liver and spleen accumulations and because of the higher storage stability mentioned above, the MN14(SANH)-MORF conjugate was used in all subsequent studies.
Table 1.
Biodistribution of both 99mTc- cMORF-MN14 (SAHN)-MORF and 99mTc- cMORF-MN14(SFB)-MORF conjugates in normal mice at 1 and 18 h postinjection. Results presented as %ID/g and %ID/organ with one sd of the mean. N = 4.
| Organs | MN14(SANH)-MORF | MN14(SFB)-MORF | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 h | 18 h | 1 h | 18 h | |||||
| mean | s.d. | mean | s.d. | mean | s.d. | mean | s.d. | |
| %ID/g | ||||||||
| Liver | 6.86 | 1.67 | 5.67 | 0.57 | 8.40 | 1.23 | 9.36 | 0.96 |
| Heart | 2.65 | 0.29 | 1.39 | 0.45 | 3.13 | 0.53 | 1.71 | 0.19 |
| Kidney | 4.65 | 0.46 | 2.02 | 0.64 | 4.97 | 0.59 | 2.50 | 0.19 |
| Lung | 3.89 | 0.98 | 1.80 | 0.69 | 4.63 | 1.17 | 1.79 | 0.41 |
| Spleen | 2.98 | 0.57 | 3.54 | 0.44 | 4.90 | 1.45 | 8.42 | 1.52 |
| Muscle | 0.32 | 0.01 | 0.47 | 0.14 | 0.33 | 0.07 | 0.32 | 0.04 |
| Blood | 10.8 | 0.59 | 4.76 | 1.46 | 15.2 | 1.93 | 3.39 | 0.96 |
| %ID/organ | ||||||||
| Liver | 14.5 | 3.74 | 13.5 | 2.41 | 18.1 | 3.62 | 23.4 | 2.40 |
| Heart | 0.49 | 0.06 | 0.26 | 0.07 | 0.51 | 0.10 | 0.33 | 0.05 |
| Kidney | 3.03 | 0.45 | 1.56 | 0.32 | 3.17 | 0.30 | 1.84 | 0.22 |
| Lung | 0.96 | 0.22 | 0.42 | 0.17 | 1.04 | 0.19 | 0.41 | 0.08 |
| Spleen | 0.38 | 0.04 | 0.43 | 0.11 | 0.64 | 0.08 | 1.25 | 0.30 |
| Stomach | 0.56 | 0.07 | 0.30 | 0.04 | 0.49 | 0.07 | 0.52 | 0.14 |
| Sm. Int. | 1.95 | 0.12 | 1.30 | 0.17 | 2.03 | 0.36 | 2.33 | 0.50 |
| Lg. Int. | 0.49 | 0.04 | 0.50 | 0.11 | 0.37 | 0.14 | 0.82 | 0.17 |
| Muscle | 4.79 | 0.39 | 7.43 | 2.33 | 5.01 | 1.01 | 5.37 | 0.88 |
| Blood | 28.3 | 3.11 | 12.9 | 3.77 | 40.6 | 2.96 | 10.1 | 2.99 |
| Whole body | 63.5 | 1.34 | 51.3 | 1.09 | 74.8 | 2.90 | 59.9 | 0.89 |
Table 2 presents the pretargeting results obtained in nude mice bearing LS174T tumors in one thigh and receiving either 0.2 or 1.0 μg of 99mTc-cMORF 3 h earlier to tumored mice having received 2 d earlier the MN14 (SANH)-MORF conjugate at dosages of 6 μg or 30 μg respectively. No significant differences in radiolabeled cMORF accumulation between the two dosages of antibody occurred in tissues (p>0.05). Further, when compared with earlier study using antibody conjugate with EDC (5), these results showed comparable tumor uptake (3.96±0.76 Vs 3.62±0.45).
Table 2.
Biodistribution by pretargeting at 3 h of either 0.2 or 1.0 μg of 99mTc-cMORF administered to tumored mice having received 2 d earlier the MN14(SANH)-MORF conjugate at 6 or 30 μg respectively. Results presented as %ID/g and %ID/organ with one sd of the mean. N = 4
| Organs | 30 μg MN14 (1.0 μg cMORF) | 6 μg MN14 (0.2 μg cMORF) | ||
|---|---|---|---|---|
| Mean | sd | mean | sd | |
| %ID/g | ||||
| Liver | 1.93 | 0.24 | 1.94 | 0.17 |
| Heart | 0.80 | 0.11 | 0.61 | 0.02 |
| Kidney | 8.79 | 1.38 | 10.2 | 1.19 |
| Lung | 1.01 | 0.17 | 0.86 | 0.08 |
| Spleen | 1.13 | 0.18 | 1.01 | 0.08 |
| Muscle | 0.36 | 0.12 | 0.17 | 0.02 |
| Tumor | 3.96 | 0.70 | 3.00 | 0.72 |
| Blood | 1.98 | 0.24 | 1.37 | 0.23 |
| %ID/organ | ||||
| Liver | 3.23 | 0.11 | 2.92 | 0.17 |
| Heart | 0.12 | 0.01 | 0.08 | 0.01 |
| Kidney | 5.51 | 1.00 | 5.63 | 0.74 |
| Lung | 0.17 | 0.04 | 0.16 | 0.01 |
| Spleen | 0.12 | 0.00 | 0.13 | 0.01 |
| Stomach | 0.85 | 0.13 | 0.73 | 0.08 |
| Sm. Int. | 1.22 | 0.21 | 1.27 | 0.06 |
| Lg. Int. | 1.20 | 0.12 | 1.03 | 0.15 |
| Muscle | 4.60 | 1.24 | 2.05 | 0.25 |
| Tumor | 3.09 | 0.56 | 1.85 | 0.60 |
| Blood | 4.43 | 0.44 | 2.97 | 0.56 |
| Whole body | 33.8 | 1.87 | 29.4 | 3.37 |
Discussion
Some of the existing methods to couple DNA oligonucleotides and other oligomers to antibodies use biotin-streptavidin, or use glutaraldehyde to cross-link amino groups (17–22), or react sulfhydryl group-containing oligonucleotides with maleimide-modified antibodies (23–25) or cross-link a carboxyl group on an antibody with an amine derivatized oligomer using EDC (4–5). The goal of this study was to evaluate Hydralink, a commercially available conjugation kit to conjugate the MN14 anti-CEA antibody with MORF for use in tumor pretargeting studies.
A novel and convenient method to determine the average gpm of attached MORF per MN14 conjugate was employed based on differential absorbance at 265 nm and 280 nm. By plotting the ratio of MN14-MORFs absorbance at 265 nm and 280 nm vs. gpm, the degree of conjugation during the conjugation reaction could be monitored by size-exclusion HPLC. The measurement of the degree of modification of an antibody or MORF in this manner by HPLC is possible because the UV absorbance of hydrazone is not affected by the presence of either the antibody or MORF.
The antibody conjugation was approached in both directions by first reacting MN14 with the NHS-SANH or NHS-SFB and then combined with MORF previously reacted with NHS-SFB or NHS-SANH respectively to yield MN14 (SANH)-MORF and MN14 (SFB)-MORF. We demonstrate that both approaches are effective and provide an average gpm of between 1–2 and therefore higher than the 0.2 value achieved earlier in this laboratory using a conventional EDC carbodimiimide method [5]. Because the pharmacokinetics in normal mice was slightly more favorable for the MN14(SANH)-MORF compared to the MN14 (SFB)-MORF and because the former was more stable to storage presumably due to side reaction from excess SFB on antibody which would require a blocking agent to eliminate, subsequent studies concentrated on MN14(SANH)-MORF. The MN14(SANH)-MORF was found to retain more than 86% immunorectivity (i.e. immunoreactive fraction) and when used in a pretargeting strategy, the biodistribution of MN14-MORF conjugates in tumored mice following a pretargeting strategy showed only minor difference in terms of tumor uptake between the two methods despite the order of magnitude difference in gpm.
In conclusion, the commercial Hydralink was shown to be an efficient and convenient method to conjugate MORF and probably other oligomers to antibodies or other biomolecules under mild condition without compromising their properties.
Acknowledgments
Financial support for this investigation was provided, in part, by the National Institutes of Health (CA 94994).
References
- 1.Goodwin DA, Meares CF, McTigue M, Mccall MJ, David GS. Rapid localization of haptens in sites containing previously administrated antibody for immunoscintigraphy with short half-life tracers [abstract] J Nucl Med. 1986;27(suppl):959. [Google Scholar]
- 2.Hnatowich DJ, Virzi F, Rusckowski M. Investigations of avidin and biotin for imaging applications. J Nucl Med. 1987;28:1294–1302. [PubMed] [Google Scholar]
- 3.Chang CH, Sharkey RM, Rossi EA, Karacy H, McBride W, Hansen HJ, Chatal J-F, Barbet J, Goldenberg DM. Molecular advances in pretargeting radioimmunotherapy with bispecific antibodies. Mol Cancer Ther. 2002;1:553–563. [PubMed] [Google Scholar]
- 4.Liu G, Mang’era K, Liu N, Gupta S, Rusckowski M, Hnatowich DJ. Tumor pretargeting in mice using 99mTc labeled morpholinos, a DNA analog. J Nucl Med. 2002;43:384–391. [PubMed] [Google Scholar]
- 5.Liu GZ, He J, Dou SP, Gupta S, Vanderheyden J-L, Rusckowski M, Hnatowich DJ. Pretargeting in tumored mice with radiolabeled morpholino oligomer showing low kidney uptake. Eur J Nucl Med Mol Imaging. 2004;31:417–424. doi: 10.1007/s00259-003-1393-9. [DOI] [PubMed] [Google Scholar]
- 6.Le Doussal JM, Martin M, Gautherot E, Delaage M, Barbet J. Invitro and in vivo targeting of radiolabeled monovalent and divalent haptens with dual specificity monoclonal antibody conjugates. J Nucl Med. 1989;30:1358–1366. [PubMed] [Google Scholar]
- 7.Goodwin DA, Meares CF, McTigue M, Chaovapong W, Diamanti CI, Ransone CH, McCall MJ. Pretargeted immunoscintigraphy: effect of hapten valency on murine tumor uptake. J Nucl Med. 1992;33:2006–2013. [PubMed] [Google Scholar]
- 8.Boerman OC, Kranenborg MHGC, Oosterwijk E, Griffiths GL, McBride WJ, Oyen WJ, de Weijert M, Oosterwijk J, Hansen HJ, Corstens FHM. Pretargeting of renal cell carcinoma: Improved tumor targeting with a bivalent chelate. Cancer Res. 1999;59:4400–4405. [PubMed] [Google Scholar]
- 9.Wang Y, Chang F, Zhang Y, Liu N, Liu G, Gupta S, Rusckowski M, Hnatowich DJ. Pretargeting with amplification using polymeric peptide nucleic acid. Bioconjug Chem. 2001;12:807–816. doi: 10.1021/bc0100307. [DOI] [PubMed] [Google Scholar]
- 10.He J, Liu GZ, Gupta S, Zhang YM, Rusckowski M, Hnatowich DJ. Amplification Targeting: A Modified Pretargeting Approach with Potential for Signal Amplification—Proof of a Concept. J Nucl Med. 2004;45:1087–1095. [PubMed] [Google Scholar]
- 11.He J, Liu GZ, Vanderheyden J-L, Dou SP, Rusckoswki M, Hnatowich DJ. Affinity enhancement bivalent morpholino for pretargeting: Initial evidence by surface plasmon resonance. Bioconjug Chem. 2005;16:338–45. doi: 10.1021/bc049719c. [DOI] [PubMed] [Google Scholar]
- 12.He J, Liu XR, Zhang SR, Liu GZ, Hnatowich DJ. Bivalent morpholinos for affinity enhancement pretargeting: Surface plasmon resonance studies of molecular dimensions. Bioconjug Chem. 16:1098–1104. doi: 10.1021/bc050061s. [DOI] [PubMed] [Google Scholar]
- 13.Winnard P, Jr, Chang F, Rusckowski M, Mardirossian G, Hnatowich DJ. Preparation and use of NHS-MAG3 for technetium-99m labeling of DNA. Nucl Med Biol. 1997;24:425–432. doi: 10.1016/s0969-8051(97)00027-9. [DOI] [PubMed] [Google Scholar]
- 14.He J, Liu G, Zhang S, Rusckowski M, Hnatowich DJ. Pharmacokinetics in mice of four oligomer-conjugated polymers for amplification targeting. Cancer Biother Radiopharm. 2003;18:941–947. doi: 10.1089/108497803322702905. [DOI] [PubMed] [Google Scholar]
- 15.Liu G, Liu C, Zhang S, He J, Liu N, Gupta S, Rusckowski M, Hnatowich DJ. Investigations of technetium-99m morpholino pretargeting in mice. Nucl Med Commun. 2003;24:697–705. doi: 10.1097/00006231-200306000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Liu G, Zhang S, He J, Liu N, Gupta S, Rusckowski M, Hnatowich DJ. The influence of chain length and base sequence on the pharmacokinetic behavior of 99mTc-morpholinos in mice. Quart J Nucl Med. 2002;46:233–243. [PubMed] [Google Scholar]
- 17.Niemeyer CM, Adler M, Pignataro B, Lenhert S, Gao S, Chi L, Fuchs H, Blohm D. Self-assembly of DNA-streptavidin nanostructures and their use as reagents in immuno-PCR. Nucleic Acids Res. 1999;27:4553–4561. doi: 10.1093/nar/27.23.4553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sano T, Smith CL, Cantor CR. Immuno-PCR: very sensitive antigen detection by means of specific antibody-DNA conjugates. Science. 1992;258:120–122. doi: 10.1126/science.1439758. [DOI] [PubMed] [Google Scholar]
- 19.Sugawara K, Kobayashi D, Saito K, Furuya D, Araake H, Yagihashi A, Yajima T, Hosoda K, Kamimura T, Watanabe N. A highly sensitive immuno-polymerase chain reaction assay for human angiotensinogen using the identical first and second polyclonal antibodies. Clin Chim Acta. 2000;299:45–54. doi: 10.1016/s0009-8981(00)00265-5. [DOI] [PubMed] [Google Scholar]
- 20.Brem RB, Yvert G, Clinton R, Kruglyak L. Genetic dissection of transcriptional regulation in budding yeast. Science. 2002;296:752–755. doi: 10.1126/science.1069516. [DOI] [PubMed] [Google Scholar]
- 21.Niemeyer CM, Sano T, Smith CL, Cantor CR. Oligonucleotide-directed self-assembly of proteins: semisynthetic DNA--streptavidin hybrid molecules as connectors for the generation of macroscopic arrays and the construction of supramolecular bioconjugates. Nucleic Acids Res. 1994;22:5530–5539. doi: 10.1093/nar/22.25.5530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang HT, Kacharmina JE, Miyashiro K, Greene MI, Eberwine J. Protein quantification from complex protein mixtures using a proteomics methodology with single-cell resolution. Proc Natl Acad Sci USA. 2001;98:5497–5502. doi: 10.1073/pnas.101124598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hendrickson ER, Truby TM, Joerger RD, Majarian WR, Ebersole RC. High sensitivity multianalyte immunoassay using covalent DNA-labeled antibodies and polymerase chain reaction. Nucleic Acids Res. 1995;23:522–529. doi: 10.1093/nar/23.3.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schweitzer B, Wiltshire S, Lambert J, O’Malley S, Kukanskis K, Zhu Z, Kingsmore SF, Lizardi PM, Ward DC. Inaugural article: immunoassays with rolling circle DNA amplification: a versatile platform for ultrasensitive antigen detection. Proc Natl Acad Sci USA. 2000;97:10113–10119. doi: 10.1073/pnas.170237197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bos ES, Kuijpers WHA, Meesters-Winters M, Pham DT, Haan AS, Doornmalen AM, Kaspersen FM, Boeckel CAA, Gougeon-Bertrand F. In vitro Evaluation of DNA-DNA hydridization as a two-step approach in radioimmunotherapy of cancer. Cancer Research. 1994;54:3479–3486. [PubMed] [Google Scholar]


