Abstract
The purpose of this meta-analysis was to compare the fixation outcome between the sliding hip screw (SHS) and intramedullary nails (IMN) in stable and unstable extracapsular proximal femoral fractures. All randomised controlled studies comparing IMNs with a SHS were considered for inclusion. Data was independently extracted and trial methodology assessed. Twenty-four randomised trials involving 3,202 patients with 3,279 fractures were included. Pooled results gave no statistically significant difference in the cut-out rate between the IMN and SHS (41/1,556 vs 37/1,626; relative risk 1.19; 95% confidence interval 0.78–1.82). Total failure rate (1,03/1,495 and 58/1,565, relative risk 1.83; 95% confidence interval 1.35–2.50) and re-operation rate (57/1,357 and 35/1,415, relative risk 1.63; 95% confidence interval 1.11–2.40) were greater with the IMN compared with the SHS. There was no evidence for a reduced failure rate with IMN in unstable trochanteric fractures.
Résumé
Le but de cette méta-analyse était de comparer le résultat de la fixation par vis glissante et clou centromédullaire dans les fractures extracapsulaires fémorales proximales stables et instables. Toutes les études randomisées et contrôlées qui comparent des clous centromédullaires avec une vis glissante ont été considérées pour l’inclusion. Les données ont été extraites indépendamment, et la méthodologie de l’étude étudiée. 24 essais randomisés qui concernent 3,202 malades avec 3,279 fractures ont été inclus. Les résultats mis en commun n’ont donné aucune différence statistiquement notable entre le clou centromédullaire et la vis glissante (41/1,556 vs 37/1,626; risque relatif 1.19; 95% intervalle de confidence 0.78–1.82). Le taux d’échec total (103/1,495 vs 58/1,565, risque relatif 1.83; 95% intervalle de confiance 1.35–2.50) et tle aux de la ré - opération (57/1,357 vs 35/1,415, risque relatif 1.63; 95% intervalle de confiance 1.11–2.40) étaient plus grands avec le clou centromédullaire comparé a la vis glissante. Il n’y avait aucune preuve qu’il y ait un taux de défaillance réduit avec le clou centromédullaire dans les fractures trochanterienne instables.
Introduction
Extracapsular hip fractures are increasingly common and most frequently occur in elderly patients. Operative treatment of extracapsular hip fractures was introduced in the 1950s using a variety of different implants. The foremost implant used for internal fixation is the sliding hip screw device (SHS), of which there are various equivalent models, such as the Dynamic, Richards, or Ambi hip screws. These implants can be described as an extramedullary fixation implant. Their dynamic nature allows for collapse at the fracture site, and they have superseded the older, fixed nail plates, which did not allow for collapse at the fracture site.
An alternative method of fixation of extracapsular hip fractures is an intramedullary nail (IMN). The early proximally inserted designs, such as the Kuntscher Y nail, did not allow for collapse at the fracture site. Within the last 20 years, a variety of newer, short IMN fixation devices that allow for sliding and therefore collapse at the fracture site have been introduced. The first of these to be commercially available was the gamma nail (Howmedica Ltd). Subsequently, the intramedullary hip screw (IMHS) (Richards Medical Ltd) was introduced in 1995 and the proximal femoral nail (PFN) (Synthes Ltd) in 1998.
A theoretical advantage of intramedullary fixation is that it provides a more biomechanically stable construct by reducing the distance between the hip joint and the implant. Potential disadvantages are related to greater risk of jamming of the sliding mechanism and stress risers at the site of the tip of the nail and distal locking bolts. It has been suggested, without supporting clinical data, that the IMNs are superior for unstable trochanteric fractures, reverse oblique fractures and sub-trochanteric fractures [2, 3]. Controversy, therefore, continues regarding the optimum choice of implant for these unstable fractures [14]. Several randomised controlled trials of fixation of extracapsular hip fractures comparing an IMN device with the SHS have been performed. An early summation of the results of ten of these studies demonstrated an increased risk of fixation failure and re-operation for the intramedullary devices [17]. A number of further randomised trials have since been undertaken. This has enabled a more extensive meta-analysis of prospective randomised controlled trials of nails versus SHS devices for the fixation of extracapsular hip fractures. In addition, it has now been possible to undertake a subgroup analysis for different fracture types.
Methods
We searched for relevant studies using the search strategy of the Cochrane collaboration. This included searching the Cochrane Musculoskeletal Injuries Group Trials Register, computer searching of MEDLINE, EMBASE, CINAHL and current contents, hand searching of orthopaedic journals, conference proceedings and reference lists of relevant articles. In addition, we contacted trialists, colleagues and implant manufacturers. All databases were searched from the earliest records to June 2004. All randomised and quasi-randomised controlled trials comparing fixation of all types of extracapsular hip fractures using SHS versus IMN were considered for inclusion. Articles in all languages were included and translated if required. Duplicate or multiple publications of the same study were not included. In order to meet the constraints for the reference section of this article, studies that have not been published as complete, peer-reviewed journal articles have been referenced to the Cochrane review [19].
For each identified study, data was extracted without masking of the name of the investigators or institution. Masking was not used. Two reviewers independently extracted data from each study, and differences were resolved by discussion. In situations where studies had both been published as conference abstracts and then journal articles, the latter were used as the primary reference. Each trial was assessed for its methodology using a check list. This had been adapted for use by the Cochrane Musculoskeletal Group from one suggested and validated from previous studies [8]. All trialists were contacted for clarification, and additional information as indicated. For each randomised trial identified, average patient age, gender ratio and type of implant were recorded.
The principle outcomes for the purpose of this study were those related to fracture fixation complications during the follow-up period of each study. Fixation outcomes assessed were screw cut out, fixation failure and re-operation for mechanical failure. Cut out was defined as penetration of the lag screw of the implant into the hip joint or the surrounding tissue. Total fracture fixation complications is the sum of screw cut outs, late femoral-shaft fractures, plate pull off, non-union and any other fixation failures as detailed in each study. Re-operations for fixation failure included all re-operations for fixation failure that occurred post-operatively as well as re-operations performed for intra-operative complications, such as femoral fracture, not recognised until the post-operative period. Re-operations for infection, haematoma, and elective removal were not included in the re-operation group.
The type of fracture classification used in each study was recorded. Where possible, using the published data, this was related to the type of fixation failure and re-operation rate for fixation failure. The majority of included studies classified fractures using either Evans classification or a modification thereof, such as Jensen’s modification or the AO/ASIF classification [18]. For the purposes of this meta-analysis, Jensen types 1 and 2 or AO 31A1 fractures have been classed as stable and Jensen types 3,4 and 5 or AO 31A2 and 31A3 as unstable. In studies in which both classifications were documented, Evans classification was used. Subtrochanteric fractures were included in a few studies, and wherever possible, data for the outcome of these fractures was extracted separately.
For each study, relative risks (RR) and 95% confidence intervals (CI) were calculated for dichotomous outcomes, and mean differences and 95% CIs were used for continuous outcomes. Results for comparable groups of trials and outcomes were pooled using a fixed-effect model. Effect size is an index that measures the magnitude of a treatment effect. Unlike significance tests, these indices are independent of sample size and can be used for pooled data. Heterogeneity (degree of similarity in the studies’ outcomes) between comparable trials was tested using a standard chi-squared test. The purpose of this was to ensure that the use of the fixed-effect model was appropriate.
Results
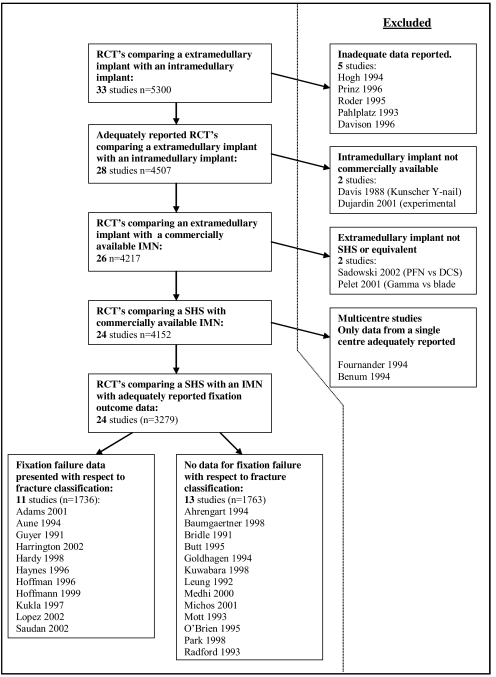
Thirty-three randomised or quasi-randomised studies comparing an IMN with an SHS were identified, for which 24 trials involving 3,459 fractures were included (Fig. 1). The included studies are summarised in Table 1. From the included studies, 18 trials with 2,626 fractures compared the gamma nail with the SHS, five studies of 627 fractures compared the IMHS with the SHS and one trial with 206 fractures compared the PFN with an SHS. The study of Aune et al. was a single-centre report of 378 fractures from a multi-centre study of 912 cases. Because of inadequate reporting of this multi-centre study, only the information presented in the report of Aune et al. could be used [4]. The study of Fornander et al. was also a single-centre report of a multi-centre study of 548 cases; again because of inadequate reporting of the full study, only that of the single-centre report for 209 cases could be used [9].
Fig. 1.
Flow diagram for identification of studies
Table 1.
Details of included studies
| Characteristics of the studies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | Year | Implant | No. of patients | Nail | SHS | Mean agea (range) | % female | Length of follow-up | Stability/ failure | Methodology score |
| Adams [1] | 2001 | Gamma | 400 | 203 | 197 | 81/80 (32-102) | 78 | 12 | Yes | 12 |
| Fornander [9] | 1994 | Gamma | 209 | 105 | 104 | 79 | 72 | 6 | No | 7 |
| Aune [4] | 1994 | Gamma | 378 | 177 | 201 | 81 (45-46) | 59 | 6 | Yes | 3 |
| Bridle [6] | 1991 | Gamma | 100 | 49 | 51 | 81/83 | 84 | 6 | No | 5 |
| Butt [7] | 1995 | Gamma | 95 | 47 | 48 | 79/78 (47-101) | 69 | <6 | No | 3 |
| Goldhagen [19] | 1994 | Gamma | 75 | 34 | 38 | 78 (28-91) | 69 | 6 to 9 | No | 5 |
| Guyer [19] | 1993 | Gamma | 100 | 50 | 50 | 80 | 85 | 3 | Yes | 1 |
| Haynes [19] | 1996 | Gamma | 50 | 19 | 31 | 80 | 72 | 6 | Yes | 4 |
| Hoffman [12] | 1996 | Gamma | 67 | 31 | 36 | 83/79 | 76 | 6 | Yes | 12 |
| Kukla [19] | 1997 | Gamma | 120 | 60 | 60 | 83.4 | 85 | 6 | Yes | 10 |
| Kuwabara [19] | 1998 | Gamma | 43 | 20 | 23 | 83/80 | 72 | 6 | No | 3 |
| Leung [13] | 1992 | Gamma | 226 | 113 | 113 | 81/78 | 70 | 7 | No | 3 |
| Lopez [19] | 2002 | Gamma | 103 | 43 | 60 | 84 | 65 | 12 | Yes | 3 |
| Michos [19] | 2001 | Gamma | 52 | 26 | 26 | 79/78 | NA | 3 to 6 | No | 1 |
| Mott [19] | 1993 | Gamma | 69 | 35 | 34 | 76 (19-99) | 58 | NA | No | 6 |
| O’Brien [15] | 1995 | Gamma | 102 | 53 | 49 | 83/77 (39-95) | 74 | 12 | No | 7 |
| Park [16] | 1998 | Gamma | 60 | 30 | 30 | 74/72 (39-95) | 60 | 18.5 | No | 5 |
| Radford [20] | 1993 | Gamma | 200 | 100 | 100 | 74/72 | 77 | 12 | No | 4 |
| Baumgartner [5] | 1998 | IMHS | 135 | 67 | 68 | 79 (40-99) | 65 | 28 | No | 9 |
| Hardy [10] | 1998 | IMHS | 100 | 50 | 50 | 82/80 | 77 | 12 | Yes | 8 |
| Harrington [11] | 2001 | IMHS | 102 | 50 | 52 | 84/81 | 79 | 12 | Yes | 10 |
| Hoffmann [19] | 1999 | IMHS | 110 | 56 | 54 | 82 | 80 | 3.7 | Yes | 8 |
| Mehdi [19] | 2000 | IMHS | 180 | 90 | 90 | 78 | NA | NA | No | 2 |
| Saudan [22] | 2002 | PFN | 206 | 100 | 106 | 83/84 | 78 | 12 | Yes | 11 |
SHS sliding hip screw, IMHS intramedullary hip screw, PFN proximal femoral nail, NA not available
aIf overall mean age not available, mean age of nail group and mean age of SHS group displayed, respectively
Nine randomised studies were excluded. Three studies of 546 patients comparing the gamma nail with a SHS screw were excluded, as they presented data without the numbers of patients in each group (Hogh 1994, Prinz 1996, Roder 1995). The study by Pahlplatz (1993) compared the gamma nail with the SHS for 113 cases, but no data with regard to fixation outcome was given. One study of 134 cases comparing the IMHS with a SHS was excluded (Davison 1996), as only interim data was reported. One study of the PFN was excluded, as it compared the PFN to a dynamic condylar plate and another compared the gamma nail with a 90° condylar blade plate (Pelet 2001) [21]. Two further studies were excluded: One compared the Kuntschner Y nail (Davis 1988), which is no longer in common use, with an SHS; the other compared an experimental static design of IMN, which is not commercially available, with an SHS (Dujardin 2001).
For the 24 included studies, only 11 studies presented or made data available regarding “screw cut outs” with respect to fracture classification, ten studies for “all failures of fixation” and eight studies for “re-operation for fixation failure”.
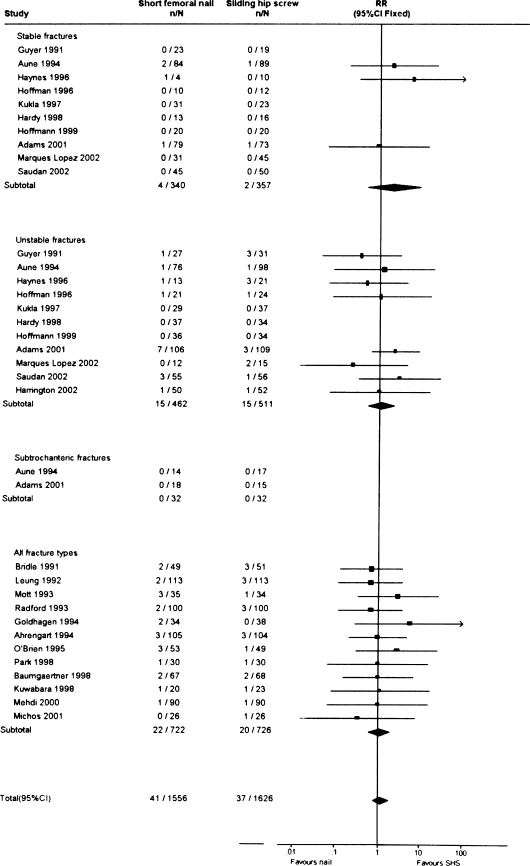
Screw cut out
The incidence of screw cut out was reported in 23 of the included studies. There were 11 studies in which the incidence of screw cut out could be correlated to fracture stability. This subgroup included 1,736 fractures. The results are detailed in Fig. 2. There were no statistically significant differences between the two groups, either when all fractures were considered or in the stable and unstable subgroups. The overall cut-out rate was 41/1,556 (2.6%) for the IMN versus 37/1,626 (2.3%) for the SHS (RR 1.19, 95% CI 0.78–1.82, test for heterogeneity chi-squared=10.03, degrees freedom=22, p=0.99). In the unstable fracture subgroup, the cut-out rate was 15/462 (3.2%) for the IMN vs 15/511 (2.9%) for the SHS.
Fig. 2.
Incidence of cut out for the different implant types related to fracture stability
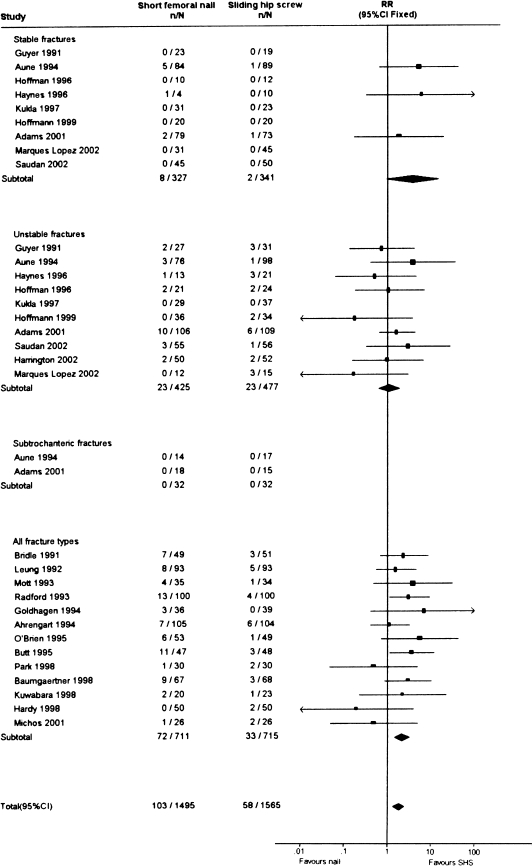
Total fracture fixation failures
The reporting of all causes of fixation failure was reported in 23 studies, as shown in Fig. 3. There were ten studies in which these failures could be correlated to fracture stability. No statistically significant difference could be demonstrated for the stable or unstable fracture subgroups. When all studies were considered, an increased failure rate was noted for the nails. The total fixation failure rate when considering all fractures was 103/1,495 (6.9%) in the IMN group and 58/1,565 (3.7%) in the SHS group (RR 1.83, CI 1.35–2.50, test for heterogeneity chi-squared=20.81, degrees freedom=24, p=0.65). In the unstable fracture subgroup, the fixation failure rate was 23/425 (5.4%) for the IMN vs 23/477 (4.8%) for the SHS.
Fig. 3.
Total fracture-healing complication rate for the different implant types related to fracture stability
The main reason for the additional fracture-healing complications detailed in Fig. 3 were femoral fractures at the tip of the implant. This occurred in 38/1,495 (2.5%) of nailed cases and 2/1,565 (0.12%) of SHS fixation cases. Other less-frequently encountered complications were detachment of the plate from the femur, non-union of the fracture, secondary displacement of the fracture and failure of the implant.
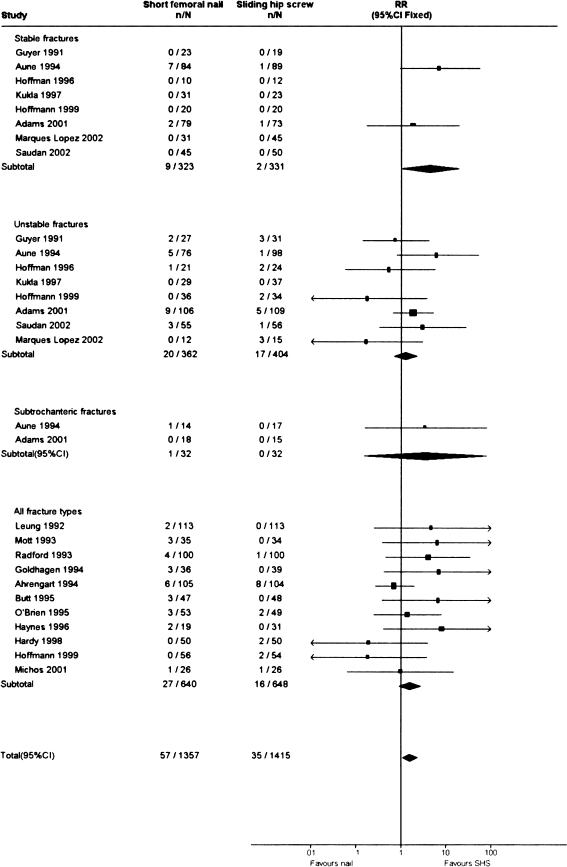
Re-Operation for fracture fixation failure
The number of re-operations performed for failure of fixation was reported in 19 studies and summarised in Fig. 4. There were eight studies in which these re-operations could be correlated to fracture stability. Again, no statistically significant difference was seen between the fracture subgroups, but with inclusion of all studies, a lower re-operation rate was seen for the SHS. The re-operation rate was 57/1,357 (4.2%) the IMN group and 35/1,415 (2.5%) for the SHS (RR 1.63, CI 1.11–2.40, test for heterogeneity chi-squared =21.52, degrees freedom=20, p=0.37). In the unstable fracture subgroup, the re-operation rate was 20/362 (5.5%) for the IMN and 17/404 (4.2%) for the SHS.
Fig. 4.
Re-operation rate for fracture healing complications for the different implant types related to fracture stability
Discussion
We were only able to provide details of outcome related to fracture stability for 11 of the 24 included randomised studies from which data could be extracted. There were five additional randomised studies involving 793 patients from which no data could be extracted due to unavailability of adequate data. Furthermore, there were two multi-centre studies of 1,460 cases that reported adequate data from only a single centre, leaving only 587 cases that could be included in this meta-analysis. The trialists for all these studies were contacted for additional information. This was either unavailable or we received no response. It is hoped that in future, with improved trial reporting, this will not occur. If all the trial data from all studies were fully reported, then data for an additional 1,666 randomised patients would be available, enabling more definite conclusions to be made for each type of implant.
Two reviews have recently been published on the optimum choice of implant for fixing unstable trochanteric fractures. A limited meta-analysis of randomised trials of nails versus the SHS for unstable intertrochanteric fractures summarised the results of three trials of 251 patients with unstable fractures [2, 3]. They concluded on the basis of this limited analysis that there was a tendency to less-frequent cut out with the intramedullary devices. A subsequent non-systematic review of the literature concluded that whilst IMNs may have biomechanical advantages, there were insufficient clinical studies to determine whether nails were superior to extramedullary fixation [23].
In this meta-analysis, we have analysed fracture-healing outcomes with relation to fracture stability. Other outcomes have already been adequately assessed in a Cochrane review, but this review neglected to undertake a specific analysis in relation to fracture type. The Cochrane review of randomised comparisons between IMNs and extramedullary implants involves an extensive search of the literature and a thorough systematic review [19]. In addition, this review has recently been updated with the latest studies. The principle outcomes for this review are summarised in Table 2. Binary outcomes were analysed by relative risk and continuous outcomes by weighted mean difference. These figures in Table 2 incorporate the data from the study of Mott 1993, which has been made available since the last update of the Cochrane review [19]. The results showed no notable difference between IMNs and the SHS other than for those outcomes related to fracture-healing complications.
Table 2.
Summary of outcomes (excluding those listed in Figs. 1, 2, and 3) from the Cochrane review comparing three nails [gamma, intramedullary hip screw (IMHS), proximal femoral nail (PFN)] with the sliding hip screw (SHS) for proximal femoral fractures. Statistically significant differences are highlighted in bold [95% confidence intervals (CI)]
| Outcome | Number of studies | Number of patients | Incidence for nails | Incidence for SHS | Effect size |
|---|---|---|---|---|---|
| Mean length of surgery (min) | 8 | 1,232 | 2.96 (−3.78 to 9.69) | ||
| Mean operative blood loss (mls) | 6 | 1,042 | −34.9 (−58.0 to −11.8) | ||
| Number of patients transfused | 3 | 709 | 181/353 | 182/355 | 1.00 (0.87–1.16) |
| Mean radiographic screening time (min) | 6 | 787 | 0.92 (0.63–1.21) | ||
| Non-union | 11 | 1,405 | 5/697 | 5/708 | 1.00 (0.36–2.84) |
| Operative fracture of the femur | 20 | 3,058 | 30/1,547 | 4/1,580 | 3.44 (1.68– 7.05) |
| Later fracture of the femur | 20 | 2,662 | 37/1,360 | 2/1,371 | 5.38 (2.53– 11.45) |
| Deep wound infection | 12 | 1,822 | 11/945 | 9/946 | 1.20 (0.54–2.64) |
| Wound infection (any type) | 15 | 1,946 | 36/961 | 36/985 | 1.03 (0.66–1.60 |
| Thromboembolic complications | 12 | 1,770 | 35/875 | 25/895 | 1.37 (0.85–2.22) |
| Wound haematoma | 9 | 938 | 12/462 | 12/476 | 1.01 (0.50–2.04) |
| All medical complications | 9 | 1,003 | 146/497 | 139/506 | 1.08 (0.90–1.30) |
| Mean days hospital stay | 7 | 917 | −0.45 (−1.55 to 0.66) | ||
| Mortality | 19 | 2,599 | 258/1,316 | 278/1,354 | 0.96 (0.83–1.11) |
| Pain at follow-up | 7 | 734 | 113/364 | 106/370 | 1.10 (0.89–1.37) |
| Impaired walking | 8 | 1,270 | 265/632 | 275/638 | 0.98 (0.86–1.11) |
| Failure to return to previous residence | 8 | 966 | 204/468 | 213/498 | 1.02 (0.88 to 1.18) |
In performing the subgroup analysis, we initially intended to classify fractures using the AO/ASIF classification. Fractures with a transverse and reverse oblique fracture pattern (type A3) are the most unstable configuration of intertrochanteric fracture. The theoretical advantages of the IMNs may be greatest for this fracture type, as they resist medialisation of the femur. Unfortunately, it was not possible to isolate this group in a satisfactory number of studies. Consequently, we were only able to classify fractures as either stable or unstable as opposed to stable trochanteric (A1), unstable trochanteric (A2) and transtrochanteric (A3). We also attempted to separate the results for subtrochanteric fractures. This was possible for the studies of Fornander (2002) and Aune (1994) [4, 9]. Haynes (1996) reported two subtrochanteric fractures within the IMN group and none in the SHS group. These two patients were excluded from the analysis. The other studies that included subtrochanteric fractures failed to provide separate data for subtrochanteric fractures. Although our results show no significant differences between the SHS and an IMN in unstable fractures, there may be an advantage in the particularly unstable transverse and reverse oblique fractures. A randomised controlled trial has been reported that confirmed that the PFN was superior to the 90° dynamic condylar screw for the fixation of reverse oblique and transverse fractures [21], but further studies are required to compare the SHS with a IMN in this fracture type.
Intra-operative fracture of the femur was not included within the category of fixation failure. This was because this complication varied from minor comminution of the fracture site to major fractures of the femur, and it was not possible to determine which fractures should be considered clinically significant. Operative fracture of the femur occurred in 35 cases of IMN and four cases of SHS. The more minor fractures required no specific treatment whilst the more extensive fractures necessitated the use of a longer nail or plate. Seven cases led to a secondary operation, and these are included within the data presented for re-operation in Fig. 4.
Our review included three types of IMN: gamma nail, IMHS and PFN. Whilst it is possible that there are differences in the complication rates between these different types of implant, the Cochrane review on IMNs demonstrated no difference between these three different types of implant [19]. A randomised trial comparing the gamma nail and the PFN reported no statistically significant difference in cut outs, fixation failures or re-operations for the two implants [24].
The intramedullary implants, being more recently developed, may have an increased risk of complications, either because the design of the implant and/or instruments is still being developed or because surgeons are still learning to use them. There is, however, no evidence to support this from our study. The studies in Figs. 2, 3, and 4 are presented in chronological order for the different fracture types. There is no suggestion of an improvement for the results of the intramedullary devices with time. The data in Figs. 2, 3, and 4 demonstrate that cut out, fixation failure and re-operations are all uncommon for stable fractures. In total, there were only ten failures out of 668 stable fractures (1.5%), and six of these were within one study, which may have used a more liberal definition of a stable fracture [9]. By comparison, there were a total of 46 failures out of 902 unstable fractures (5.1%). Therefore, we believe that in the studies that did not present results with relation to fracture stability, it is likely that the majority of cases of fixation failure encountered would have occurred in unstable fractures. Therefore, when considering the pooled results for all studies, which demonstrated significantly more failures and re-operations in patients treated with an IMN, it is likely that the majority of these failures occurred in unstable fractures.
In summary, reported studies to date demonstrate that the only notable differences in outcome between intramedullary and extramedullary fixation devices are those related to the fracture fixation failure rate and re-operation rate. The rate of fracture fixation failure and re-operation is increased for the intramedullary implants when considering all fracture types. The results of this study show that intramedullary implants cannot be recommended for stable trochanteric fractures and that they do not offer any advantage for unstable trochanteric fractures. Intramedullary fixation may be advantageous in transverse and reverse oblique fractures. However, there is currently no evidence from randomised controlled trials to support this. With future modifications to the design of short femoral nails, further studies will be required to see if these changes result in outcomes for IMNs becoming equivalent or even superior to that off the SHS.
References
- 1.Adams CI, Robinson CM, Court-Brown C, McQueen MM (2001) Prospective randomised controlled trial of an intramedullary nail versus dynamic hip screw and plate for intertrochanteric fractured femur. J Orthop Trauma 15 (6):394–400 [DOI] [PubMed]
- 2.Audige L, Hanson B, Swiontkowski MF (2004) Answer to Handoll and Parker. Int Orthop 28:62–63 [DOI]
- 3.Audige L, Hanson B, Swiontkowski MF (2003) Implant-related complications in the treatment of unstable intertrochanteric fractures: meta-analysis of dynamic screw-plate versus dynamic screw-intramedullary nail devices. Int Orthop 27:197–203 [DOI] [PMC free article] [PubMed]
- 4.Aune AK, Ekeland A, Odegaard B, Grogaard B, Alho A (1994) Gamma nail vs compression screw for trochanteric femoral fractures. 15 reoperations in a prospective, randomized study of 378 patients. Acta Orthop Scand 65:127–130 [DOI] [PubMed]
- 5.Baumgaertner MR, Curtin SL, Lindskog DM (1998) Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res 348:87–94 [DOI] [PubMed]
- 6.Bridle SH, Patel AD, Bircher M, Calvert PT (1991) Fixation of intertrochanteric fractures of the femur: a randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br 73:330–334 [DOI] [PubMed]
- 7.Butt MS, Krikler SJ, Nafie S, Ali MS (1995) Comparison of dynamic hip screw and gamma nail: a prospective, randomized, controlled trial. Injury 26(9):615–618 [DOI] [PubMed]
- 8.Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384 [DOI] [PMC free article] [PubMed]
- 9.Fornander P, Thorngren K-G, Tornqvist H, Ahrengart L, Lindgren U (1994) Swedish experience with the gamma nail vs. sliding hip screw in 209 randomised cases. International Journal of Orthopaedic Trauma 4(3):118–122
- 10.Hardy DC, Descamps P, Krallis P, Fabeck L, Smets P, Bertens CL et al (1998) Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am 80(5):618–630 [DOI] [PubMed]
- 11.Harrington P, Nihal A, Singhania AK, Howell FR (2002) Intramedullary hip screw versus sliding hip screw for unstable intertrochanteric femoral fractures in the elderly. Injury 33(1):23–28 [DOI] [PubMed]
- 12.Hoffman CW, Lynskey TG (1996) Intertrochanteric fractures of the femur: a randomized prospective comparison of the gamma nail and the Ambi hip screw. Aust NZ J Surg 66(3):151–155 [DOI] [PubMed]
- 13.Leung KS, So WS, Shen WY, Hui PW (1992) Gamma nails and dynamic hip screws for peritrochanteric fractures. A randomised prospective study in elderly patients. J Bone Joint Surg Br 74(3):345–351 [DOI] [PubMed]
- 14.Lorich DG, Geller DS, Nielson JH (2004) Osteoporotic pertrochanteric hip fractures; management and current controversies. J Bone Joint Surg Am 86:398–410 [PubMed]
- 15.O’Brien PJ, Meek RN, Blachut PA, Broekhuyse HM, Sabharwal S (1995) Fixation of intertrochanteric hip fractures: gamma nail versus dynamic hip screw. A randomised, prospective study. Can J Surg 38(6):516–520 [PubMed]
- 16.Park SR, Kang JS, Kim HS, Lee WH (1998) Treatment of intertrochanteric fracture with the gamma AP locking nail or by a compression hip screw-a randomised prospective trial. Int Orthop 22(3):157–160 [DOI] [PMC free article] [PubMed]
- 17.Parker MJ, Pryor GA (1996) Gamma nailing verses DHS for extracapsular femoral fractures: meta-analysis of ten randomised trails. Int Orthop 20:163–168 [DOI] [PubMed]
- 18.Parker MJ (1999) Proximal Femoral Fractures. In: Pynsent PB, Fairbank JCT, Carr AJ (eds) Classification of musculoskeletal trauma, Butterworth Heinemann, Oxford
- 19.Parker MJ, Handoll HHG (2004) Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures (Cochrane Review). In: The Cochrane Library, Issue 3. John Wiley & Sons, Chichester [DOI] [PubMed]
- 20.Radford PJ, Needoff M, Webb JK (1993) A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br 75(5):789–793 [DOI] [PubMed]
- 21.Sadowski C, Lubbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P (2002) Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degree screw-plate. J Bone Joint Surg Am 84(3):372–381 [PubMed]
- 22.Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P (2002) Pertrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma 16(6):386–393 [DOI] [PubMed]
- 23.Schipper IB, Marti RK, van der Werken C (2004) Unstable trochanteric femoral fractures: extramedullary or intramedullary fixation review of literature. Injury 35:141–151 [DOI] [PubMed]
- 24.Schipper IB, Steyerberg EW, Castelein RM, van der Heijden FHWM, den Hoed PT, Kerver AJH, van Vugt AB (2004) Treatment of unstable trochanteric fractures: randomised comparison of the gamma nail and the Proximal Femoral Nail. J Bone Joint Surg Br 86:86–94 [PubMed]