Abstract
The ABG I uncemented hip prosthesis has demonstrated an unacceptably high failure rate and poor functional outcome in our patients. A prospective review was performed of 38 implanted hips with a mean follow-up of 11 years. Sixteen hips have been revised or are candidates for revision hip surgery, due principally to polyethylene wear and pelvic osteolysis. Contributing factors were likely to be the poor wear characteristics of the polyethylene liners—which were gamma irradiated in air—and the thinness of these liners. Of further concern were the poor pain and function scores in the remaining hips [mean Harris Hip Scores (HHS) of 70 (SD 22) at 11-year follow-up]. The influence of the surgical learning curve on clinical results may have been an important factor. Undersized femoral components were associated with poor pain and functional scores in five patients with HHS < 60. All ABG I hip implants must remain under careful, long-term review.
Résumé
La prothèse de hanche non cimentée ABG I a montré un taux d’échec inacceptable et un mauvais résultat fonctionnel chez nos patients. Une revue prospective de 38 hanches opérées avec un suivi moyen de 11 ans est présentée. Seize hanches ont été réopérées ou vont l’être, principalement à cause de l’usure du polyethylène et de l’ostéolyse pelvienne. Les facteurs principaux étaient la mauvaise résistance à l’usure du composant PE qui était gamma-irradié et de faible épaisseur. De plus, les hanches restantes avaient un mauvais résultat pour la douleur et la fonction (score moyen de Harris de 70 à 11 ans). La courbe d’apprentissage était peut-être un facteur important du résultat clinique. Les implants fémoraux sous-dimensionnés étaient associés à des mauvais scores chez cinq patients (<60). Tous ces implants doivent rester sous surveillance étroite pour le suivi à long terme.
Introduction
Concerns have been raised about the ABG I uncemented hip replacement. Premature acetabular wear and pelvic osteolysis have resulted in early failure of the implant [1, 2]. In the United Kingdom, National Institute for Clinical Excellence (NICE) guidelines suggest that the ‘benchmark’ for the selection of prostheses for primary hip replacements should be a revision rate of 10% or less at 10 years [4].
The ABG I hip prosthesis (Anatomique Benoist Gerard; Stryker Howmedica Osteonics, Newbury, UK) is an uncemented anatomical design comprising an hydroxyapatite(HA)-coated titanium stem, designed for proximal metaphyseal fixation, and an acetabular component which consists of an HA-coated hemispherical titanium shell with an ultra-high-density polyethylene liner. It was the implant of choice in the younger patients (age <65 years) at our unit.
The purpose of our study was to determine the long-term functional and radiographic results of the ABG I uncemented hip implant, and to determine factors which may be associated with suboptimal results.
Patients and methods
Between 1992 and 1996, 48 consecutive ABG primary arthroplasties were performed on 46 patients in our orthopaedic department. Ten patients were dead at the most recent follow up, and were excluded from the present analysis. All of the ten patients (with ten hip replacements) excluded from the analysis had a preoperative diagnosis of primary hip osteoarthritis. The remaining 38 hips in 36 patients (25 females) were followed up with a minimum nine-year follow up. Mean age of patients at the time of operation was 53.7 years (range 26–63 years). The preoperative diagnosis was primary osteoarthritis in 32 hips, secondary osteoarthritis from rheumatoid arthritis in three hips, previous Perthes disease in one hip, avascular necrosis in one hip, and previous septic arthritis in one hip. Failure was defined as revision surgery or its recommendation.
Serial radiographs were examined for component position, alignment, fit and fill, evidence of loosening and migration of the component, wear and osteolysis. All 36 patients were invited to a dedicated clinic where radiographic and clinical evaluation using the Harris Hip Score [7] was performed. All patients provided consent to be involved in the study apart from five patients who were lost to follow up. A total of 33 hip implants in 31 patients were therefore available for review. An anteroposterior (AP) weight-bearing radiograph of the pelvis was performed. Intra-operative and post-operative complications were recorded. Any symptoms, particularly pain, was noted at the most recent clinical review.
A single surgeon, recently retired, performed all operations. The surgical approach was anterolateral (Hardinge approach) in all cases. Polyethylene hooded inserts and cobalt chromium heads (28 mm in 37 cases, one alumina head) were used in our series. Shell diameters of between 48 and 60 mm were used in the series. Cups with external diameter between 48 to 54 mm were used in 22 hips, and cups with external diameter between 56 to 60 mm were used in 16 hips. All 36 patients were followed prospectively. Mean follow-up was 132 months (range 110–143 months).
Results
At the latest follow up, 16 hips (48.5%) of the 33 hips available for follow-up have been revised or were candidates for revision hip surgery. Eleven hip revisions were performed. Of the 11 revisions, five were performed for excessive wear of the acetabular component, three for recurrent dislocation, one for persistent thigh pain and one for femoral osteolysis; one revision was performed for ceramic component failure. Five other hips required revision of the acetabular component due to excessive polyethylene wear and pelvic osteolysis. Of these five other hips which required revision surgery, three were awaiting surgery, one patient declined further surgery and another was not fit for surgery.
There was one postoperative periprosthetic fracture which required open reduction internal fixation with cables. Pulmonary embolism occurred in one patient who required anticoagulation, without any further complication. Five hips dislocated, which included two hips which did not require further surgery. For the 33 hips which were available for follow-up, the mean preoperative Harris Hip Score was 53 (SD 7.4). Mean postoperative Harris Hip Score at 4.7 years follow-up was 93.6 (SD 7.3), which deteriorated to a mean of 70 (SD 22) at mean of 11 years follow-up. The breakdown of the pain (mean score 31) and function (mean score 32) components of the HHS at the latest follow-up suggested deterioration in both pain and function. Ten of the 13 hips which had a cup external diameter of 52 mm or less were revised or listed for revision due to excessive acetabular wear. Five hips which were not revised or listed for revision surgery, and which had HHS of <60 (mean 46), had undersized femoral components.
Discussion
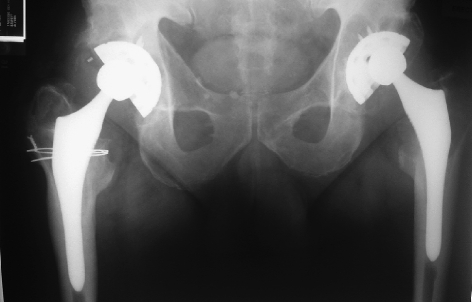
The Medicines and Healthcare products Regulatory Agency (MHRA) recently issued a hazard warning regarding the ABG I hip implants [9]. The results from this series of patients with a mean of 11 years follow-up provide further evidence of accelerated acetabular wear and pelvic osteolysis resulting in premature failure of the ABG I hip implant (Fig. 1). Several factors have been identified as contributing to the failure of this implant. Gamma irradiation in air has been shown to cause increased oxidative degradation, thereby adversely affecting its wear properties [11]. All ABG I polyethylene liners were gamma irradiated in air.
Fig. 1.

Patient with bilateral ABG I uncemented hip replacements. Bilateral pelvic osteolysis is noted
Non-articulating modular junctions create new interfaces for the generation of particulate debris (backside wear) [6]. Polyethylene liners have been found to be loose within the acetabular shell, possibly due to poor locking mechanism of the liner to the shell [2]. The ABG I cup had many holes, which may reduce the potential area for osteointegration of the HA coating, and may be an entry site for polyethylene into the acetabular bone. Excessive polyethylene wear may be associated with metal backing of the acetabular component, although this may be because the polyethylene has to be thinner within the metal backing [3, 12]. Thin liners contributed to failure of several implants in our series, with a 77% failure of all external cup diameters of <52 mm.
The indications for total hip arthroplasty has extended to increasingly younger patients with higher functional requirements and expectations. The use of the uncemented ABG hip implant was an attempt, in our unit, to increase the longevity of total hip arthroplasty in these younger patients. However, the outcome of total hip replacement is not only dependent on the prosthesis but on surgical technique. It has been estimated that the surgeon accounts for >90% of the end result in arthroplasty, with the implant accounting for <10% [8].
The influence of the surgical learning curve on clinical results in our series may have been an important factor. The surgeon implanting the prostheses was trained in the implantation of prostheses with cement; implantation without cement using a new implant was an alteration in the surgical technique of the surgeon. A dislocation rate higher than the surgeon's average dislocation rate, as occurred in this series, would support this suggestion. Undersized femoral components were associated with poor pain and functional scores in five patients with HHS < 60, all of whose operations were performed early in the series, which would suggest technical inexperience (Fig. 2).
Fig. 2 .
Undersized femoral component. Note eccentric superolateral acetabular wear
The recent establishment of a national arthroplasty register in the United Kingdom should facilitate the identification of poorly performing prostheses; however, registration of all hip or knee arthroplasty into the register is not compulsory at present. Compliance is therefore poor (approximately 60%) [10]. This study emphasises the importance of careful and repeated clinical surveillance and audit, as the initial results of the ABG I implant in our unit was good [5]. Clinical record keeping must include batch number and manufacturer of the implant, as failure may occur years after implantation of the device. Long-term radiological review is critical to identify early failure.
A 42% failure rate represented poor results of a primary hip implant, albeit in a younger population. Of additional concern would be the poor pain and functional outcome (mean HHS of 70) at a mean of 11 years follow-up. Femoral component undersizing may account for persistent thigh pain and poor functional results.
References
- 1.Blacha J (2004) High osteolysis and revision rate with the hydroxy-apatite-coated ABG hip prostheses. Acta Orthop Scand 75(3):276–282 [DOI] [PubMed]
- 2.Duffy P, Sher JL, Partington PF (2004) Premature wear and osteolysis in an HA-coated uncemented total hip arthroplasty. J Bone Joint Surg Br 86(1):34–38 [PubMed]
- 3.Devane PA, Bourne RB, Rorabeck CH, MacDonald S, Robinson EJ (1995) Measurement of polyethylene wear in metal-backed acetabular cups II: clinical application. Clin Orthop 319:317–326 [PubMed]
- 4.Guidance on the selection of prostheses for primary total hip replacement. http://www.nice.org.uk
- 5.Giannikas KA, Din R, Sadiq S, Dunningham TH (2002) Medium-term results of the ABG total hip arthroplasty in young patients. J Arthroplasty 17:184–188 [DOI] [PubMed]
- 6.Huk O, Bansal M, Betts F (1994) Polyethylene and metal debris generated by non articulating surfaces of modular acetabular components. J Bone Joint Surg Br 76-B:568–574 [PubMed]
- 7.Harris H (1969) Traumatic arthritis of the hip after dislocation and acetabular fracture: treatment by mould arthroplasty: an end result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755 [PubMed]
- 8.Katz JN, Losina E, Barrett J et al (2001) Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am 83:1622–1629 [DOI] [PubMed]
- 9.Medical Device Alert (Ref. MDA/2004/011). http://www.mhra.gov.uk
- 10.National Joint Registry. Summary report to the 2nd Annual report, Sept 2005. Section 4.3 Data completeness. http://www.njrcentre.org.uk
- 11.Sutula LC, Collier JP, Saum KA et al (1995) Impact of gamma sterilization on clinical performance of polyethylene in the hip. Clin Orthop 319:28–40 [PubMed]
- 12.Shih CH, Lee PC, Chen JH et al (1997) Measurement of polyethylene wear in cementless total hip arthroplasty. J Bone Joint Surg Br 79B:361–365 [DOI] [PubMed]