Abstract
The role of surface finish on the survivorship of cemented femoral stems continues to be debated. A total of 34 proximally roughened cemented stems were implanted in 33 consecutive patients undergoing total hip arthroplasty by a single surgeon. An alarmingly high failure rate was observed, prompting a retrospective chart review, analysis of radiographs, and evaluation of retrieved stems and pathological specimens. Nineteen patients were available with more than two years follow-up. Of these 19 patients, nine stems had failed (47%) due to severe osteolysis and stem loosening. Failures were significantly more common in the male gender (p<0.005), and young (p=0.05), tall (p<0.002), and heavy patients (p<0.004). All failed revised hips showed severe metallosis, with both gross and microscopic evidence of metallic shedding from the stems. Our findings suggest that this proximally roughened stem is susceptible to early failure. Failure is characterized by stem debonding, subsidence within the cement mantle, shedding of metallic and cement particles due to fretting, and rapidly progressive osteolysis. These findings have been observed with other rough surface finish cemented stems.
Résumé
Le rôle de l’état de surface des tiges fémorales cimentées sur leur survie est toujours discuté.34 tiges à la partie proximale rugueuse ont été implantées chez 33 patients au cours d’arthroplastie totale de la hanche faites par le même chirurgien. Un taux important d’échec était observé, conduisant à une étude rétrospective avec analyse radiographique, étude des pièces explantées et de l’aspect histologique. 19 patients ont été revus à plus de 2 ans de recul avec parmi eux 9 échecs dus à une ostéolyse avec descellement de la tige fémorale. Ces échecs étaient plus fréquents chez l’homme (p<0,005), le jeune (p=0,05) , le grand (p<0,002), et le lourd (p<0,004). Toutes les reprises ont montré une métallose sévère avec macroscopiquement et microscopiquement des débris de métal arrachés à la tige. L’échec est caractérisé par une mobilisation de la tige, un enfoncement dans le ciment, arrachage de particules métalliques et ostéolyse. Ces faits ont été observés avec d’autres tiges à revêtement rugueux.
Introduction
The effect of changes in the surface finish of femoral stems used for cemented total hip arthroplasty continues to be debated. The vast majority of clinical studies have shown an increased rate of aseptic loosening with precoated or rough stems, designed to bond or have mechanical interlock with the cement [1, 4, 5, 7, 9, 14, 18, 29, 33]. Only a few reports have shown no difference between rough and satin or polished stems [27, 28, 32].
The satin Spectron stem (Ra: 0.76 μm) (Smith & Nephew, Memphis, TN, USA) is one of the best performing stems in the Swedish National Hip Arthroplasty Register, with survivorship of 100% at seven years and 98.4% at ten years [24]. In 1989, a modified version of the stem was introduced (Spectron EF, Smith & Nephew, Memphis, TN, USA), with the addition of a distal centraliser, head modularity, and a rough surface finish (Ra: 7.3 μm) in the proximal third of the stem (Fig. 1).
Fig. 1.

The proximally rough Spectron EF stem
In 1996, the senior author (PP) implanted the Spectron EF stem in 33 consecutive patients who required a total hip arthroplasty. The aim of our study is to report on the clinical and radiographic results of that group, based on a retrospective chart and radiographic review.
Materials and methods
Thirty-four Spectron EF stems for primary total hip arthroplasty were implanted in 33 consecutive patients during the spring of 1996. This was a consecutive, non-selected series as the senior author (PP) used this stem for all primary total hip arthroplasties during that time.
All total hip arthroplasties were performed through a posterolateral approach with enhanced posterior soft tissue repair [25]. An uncemented cup with a 1-mm press fit implantation technique was used in 33 hips (28 Reflection Smith and Nephew, Memphis, TN, USA and five Trilogy Zimmer, Warsaw, IN,USA). One patient with post-traumatic arthritis following an acetabular fracture received a cemented all polyethylene cup (Kinamed, Amarillo, CA, USA). The femoral canals were broached to the size of the implanted stem, as is the senior author’s routine, and that of others [30]. The stems were implanted with Simplex P bone cement (Howmedica, Rutherford, NJ, USA) and modern cementing technique, including vacuum mixing, distal canal plugging, and retrograde filling with pressurisation of the cement. The stems were inserted with a distal centraliser. Initial component alignment was satisfactory in all cases.
Patients were followed-up clinically and radiographically at six weeks, four months, and yearly thereafter. In the postoperative radiograph obtained six weeks after surgery we measured the alignment of the stem in the frontal plane and classified the cement mantle according to Barrack et al. [2]. On the radiographs obtained at last follow-up we determined the radiographic fixation of the femoral stem according to Harris and McGann [16]. The presence, extent, and location of progressive radiolucent lines measuring more than 1 mm and the areas of femoral osteolysis were evaluated according to the zones defined by Gruen et al. [15]. Radiographic osteolysis was defined as so-called “punched-out” areas devoid of trabecular bone, usually with a sclerotic border. Total and annual wear was calculated using the method proposed by Livermore et al. [23], by means of a digital caliper with a precision of 0.01 mm (Absolute Digimatic, Mitutoyo, Japan). Our intra-observer error with this method has been previously reported [13]. All radiographs were evaluated and measured by a single observer (AG) who was not involved in the surgery, to avoid inter-observer variation and outcome bias.
Statistical analysis Descriptive statistics were calculated with means and standard deviations for continuous variables and frequency counts for discrete variables. Statistical comparisons were made between “success” and “failure” for continuous variables using a Mann-Whitney nonparametric test and for discrete variables using a Fisher’s exact test due to the small sample size. A critical p value of 0.05 was used for statistical significance. Multivariate analysis could not be performed due to the small sample size. All analyses were conducted using SPSS 11.0 for Windows (Chicago, IL, USA).
Results
There were 14 men (15 hips) and 19 women (19 hips). The average age of the patients at the time of surgery was 62 years (range: 36–88). The average weight was 76 kg (range: 41–118 kg), and body mass index (BMI) was 26.0 (range: 16–35). Twelve patients (12 hips) did not have a minimum follow-up of two years. One patient, who underwent a bilateral total hip arthroplasty, died two years after operation with an intact reconstruction. The remaining 20 hips had a minimum follow-up of two years (average: 5.7 years; range: 2–8 years) and comprised the study group. The diagnosis was osteoarthritis in 12 patients, degenerative joint disease secondary to abnormal developmental processes (developmental dysplasia of the hip and Legg-Calvé-Perthes disease) in two patients, osteonecrosis in two, post-traumatic arthritis in three, and femoral neck fracture in a patient with a painful bipolar arthroplasty that required conversion to a total hip arthroplasty.
Of the 20 patients with a minimum two-year follow-up, six have been revised. One patient was revised for deep infection 48 months after surgery. The remaining five (25%) were revised for aseptic loosening with extensive femoral osteolysis at an average of 5.2 years of follow-up (range: 2.9–7.8 years) (Fig. 2). One additional patient with the same radiographic findings is scheduled for revision. Three additional patients with six, seven, and eight years of follow-up, respectively, have progressive femoral osteolysis and are being closely monitored. Using radiographic loosening or osteolysis as an endpoint, nine of 20 patients available for follow-up had a failed reconstruction. All cementless cups were well fixed at last follow-up and none of them required revision. The single cemented cup was revised when it was found to be loose during stem revision.
Fig. 2.

Stem loosening subsidence and severe proximal femoral osteolysis observed in a patient, 6 years after surgery
Failures were significantly more common in young [50 (range: 36–73) vs 62 years (range: 43–79)] and heavy patients [90 kg (range: 65–118) vs 68 kg (range 41–90)] (Table 1). In addition, failures were significantly more common in men, as nine of 11 female patients (81.8%) had a successful outcome compared to just one of eight males (12.5%) (p<0.005).
Table 1.
Statistical comparison between successful and failed cases
| Variable | Success | Failure | p value |
|---|---|---|---|
| Demographics | |||
| Age (years) | 61.6±9.5 | 50.6±12.6 | 0.053 |
| Height (m) | 1.63±0.13 | 1.82±0.07 | 0.002 |
| Weight (kg) | 67.7±14.5 | 90.8±16.2 | 0.004 |
| Outcomes | |||
| Livermore wear rate | 0.89±0.62 | 1.21±0.68 | 0.44 |
| Livermore annual wear rate | 0.13±0.09 | 0.20±0.10 | 0.20 |
Radiographic analysis Of the 19 patients available after exclusion of the one who developed deep infection, nine patients (including the five who required revision) demonstrated radiographic loosening and/or ballooning osteolysis (Fig. 2). The location of the osteolytic lesions/radiolucent lines is depicted in Table 2. The cement mantle in these nine failed cases had been rated A in five and B in four [2]. These nine failed arthroplasties correspond to patients 1, 5, 13, 17, 21, 23, 24, 26, and 33 in the series. In comparing the stems that failed versus those that remain stable, there is no significant difference among quality of bone [8], cement mantle [2], linear wear rate of polyethylene [23], or stem alignment (Table 1).
Table 2.
Location of osteolysis/radiolucent lines [15]
| Patient | Gruen zones demonstrating osteolysis | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| 1 | X | X | X | X | |||
| 6 | X | X | X | X | X | X | X |
| 13 | X | X | X | ||||
| 17 | X | X | X | ||||
| 21 | X | X | X | X | X | X | X |
| 23 | X | X | X | X | |||
| 24 | X | X | |||||
| 26 | X | X | |||||
| 33 | X | X | X | X | |||
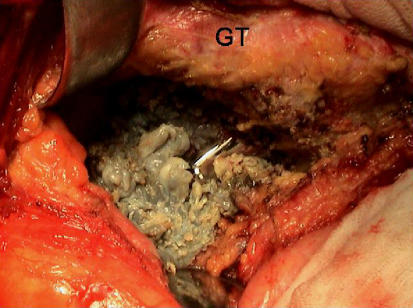
Analysis of retrieved implants and interface pseudomembrane During revision surgery, macroscopic metallosis was present in all hips (Fig. 3). Three femoral components were available for analysis. We examined the four facets of this rectangular stem, assessing macroscopically the surface fretting and polishing according to a previously designed protocol [12]. The three stems with subsidence had polishing in all four facets (Fig. 4). The damage in the surface of the stems was predominantly located in the posteromedial and anterolateral corners as the stems were forced into retroversion after loosening, thus fretting with the cement mantle [7, 14, 17]. The microscopic examination of the femoral pseudomembrane consistently revealed an inflammatory reaction characterised by the presence of multinucleated giant cells and metallic, cement, and polyethylene deposits.
Fig. 3.
Intraoperative metallosis due to fretting of the loose stem with the cement mantle (GT greater trochanter)
Fig. 4.
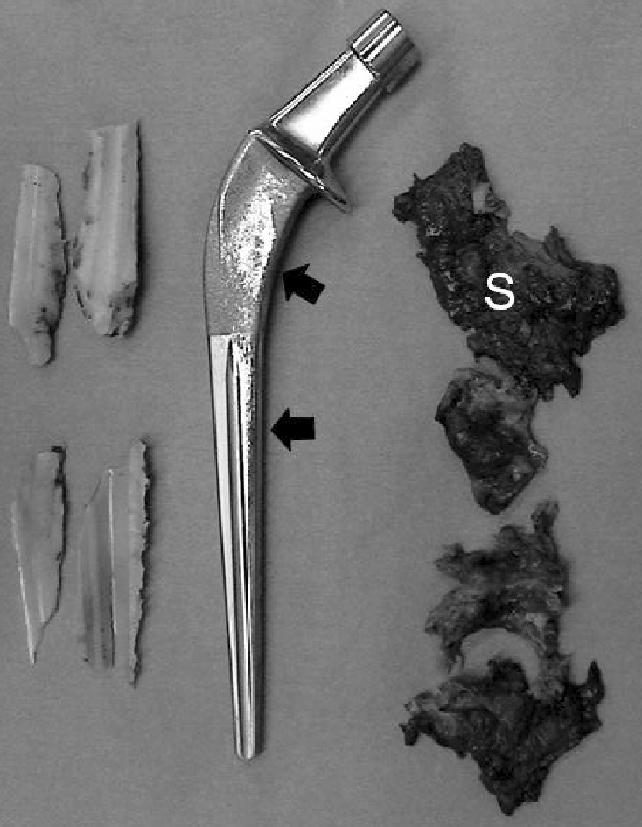
A retrieved implant demonstrates loss of surface roughness (black arrows). There is abundant metallic stained synovium (S)
Discussion
Our study reports an unexpectedly high incidence of fixation failure in the rough Spectron EF stem, with a characteristic mode of failure, which included debonding from the cement, subsidence, and massive femoral osteolysis.
The Spectron stem, with an homogeneous satin finish (Ra: 0.76 μm), has been one of the best performing stems in the Swedish Hip Arthroplasty Register [24] and one of the few to outperform the Charnley stem [10, 20]. Garellick et al., in a prospective, randomized study, reported five femoral revisions for aseptic loosening among 206 Charnley total hip arthroplasties, and none among 204 Spectron, at ten years of follow-up [10]. Radiographic analysis of the same series revealed that ten Charnley stems and one Spectron stem were radiographically loose [11].
Despite its excellent track record, the satin, non-modular Spectron stem underwent a design modification in an attempt to improve centralization and enhance stem-cement bonding. This led to the creation of the Spectron EF. The EF design has a circumferentially roughened proximal area with an Ra of 7.3 μm. In the 2002 report of the Swedish Hip Arthroplasty Register, the survivorship of both the original and the EF version of the Spectron stems was similar [24]. We were unable to find other studies evaluating the performance of this modified, rough stem.
The findings in our series contrast with that reported by the Swedish National Hip Register. Though we do not have a historical control group of satin Spectron total hip arthroplasties for comparison, the high prevalence of failure in the Spectron EF stem prompted us to report our results.
In a review of the published series of satin finish Spectron stems, there is no mention of metallosis, severe femoral osteolysis, or the surface finish changes that we observed in our study. Kale et al. communicated the five to 13-year follow-up of a consecutive series of primary total hip replacements performed with the satin, monoblock Spectron stem with a 32-mm head [20]; three of 152 stems were revised for aseptic loosening, and focal femoral osteolysis was present in five other hips. Recently, Issack et al. communicated a 4.2% (five of 120) rate of revision for late aseptic loosening occurring between ten and 16 years after surgery, with the satin Spectron stem in patients followed-up for an average of 16 years (range: 13–17) [19]. Extensive osteolysis and loosening occurring four to seven years after surgery, such as that observed in our patients, was not reported in these studies. We believe that the addition of a proximally rough surface finish adversely affected the clinical performance of the stem.
Additionally, numerous reports of early fixation failure of roughened stems have been published. Collis and Mohler reported on 244 stems of the same geometry implanted over a two-year period, half of which were polished and half roughened. The roughened group had six failures whereas the polished group had only one failure out of 122 stems [6]. Sporer et al. reported on the poor outcome of the Iowa hip stems that had been bead blasted (11-year average follow-up and 6% failure rate) or grit blasted and then precoated (8-year follow-up and 18% failure rate). To date, this is the highest failure rate we are aware of in the literature for a stem designed to bond to the cement [31].
In a recent study from our institution, a rough, modern cemented stem with an Ra of 2–2.5 μm (VerSys, Zimmer, Warsaw, IN, USA) had a 11% revision rate for femoral osteolysis and loosening at four to seven years of follow-up, when compared to one with identical metallurgy and geometry, but with a satin finish (Ra: 0.5 μm), which demonstrated no failure for aseptic loosening [14].
Our nine failed cases did not have a deficient cement mantle that could have explained the poor clinical performance. Kawate et al. suggested that an incomplete cement mantle may contribute to early osteolysis in precoated stems [21]. All seven of the hips that failed in their series (a rate of 12%) had a grade C2 or D cement mantle. Other reports have linked the early failure of femoral stems to specific areas of a thin cement mantle and an associated increase in local micromotion [26]. Although the technique of under-broaching is not widely used, support for this technique can also be found in the literature. Skinner et al. recently reported the ten-year follow-up of 189 patients who received a Freeman prosthesis in whom the canal was prepared for either a standard cement mantle or a thin mantle (via broaching line-to-line with the implant) [30]. In this report, the survivorship of the two groups was similar (98 vs 97% success at ten years).
The macroscopic findings in our retrievals are consistent with those of our earlier study of other 13 failed Spectron EF stems, which required revision for aseptic loosening in our institution [12]. As micromotion occurs at the implant cement interface and the stems subsides, metallic and cement particles are generated due to fretting between cement and the rough surface of the implant. This process releases biologically active cement and metallic particles that we detected in our microscopic analysis and also diminishes the conformity between the implant and the cement, which leads to further loosening and loss of bone stock [17].
Our failure rate of 47% far surpasses any reported for either roughened or precoated stems. Though 11 patients are lost to follow-up, several studies have demonstrated that those patients do not necessarily have a worse outcome than those not lost [3, 22]. Even in the best case scenario in which all patients lost to follow-up are surviving and have excellent clinical and radiographic outcomes, the failure rate would be 25%. The mode of failure observed in our patients is similar to that reported for other rough and precoated cemented stems [1, 4, 5, 9, 14, 18, 29, 33].
In our study the subset of patients who experienced early loosening were younger, more likely to be male, and significantly heavier than the patients with surviving implants. We recognise the shortcomings of reporting on such a small cohort of patients reviewed retrospectively. Though we continue to search for the lost patients, the failure rate has been so high that we feel compelled to present our findings.
References
- 1.Agins HJ, Alcock NW, Bansal M, Salvati EA, Wilson PD Jr, Pellicci PM, Bullough PG (1988) Metallic wear in failed titanium-alloy total hip replacements. A histological and quantitative analysis. J Bone Joint Surg Am 70:347–356 [PubMed]
- 2.Barrack RL, Mulroy RD Jr, Harris WH (1992) Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br 74:385–389 [DOI] [PubMed]
- 3.Bordini B, Toni T, Stea S, Paderni S (2004) Statistical analysis in hip prosthesis evaluation. Hip Int 12:86–93 [DOI] [PubMed]
- 4.Buly RL, Huo MH, Salvati E, Brien W, Bansal M (1992) Titanium wear debris in failed cemented total hip arthroplasty. An analysis of 71 cases. J Arthroplasty 7:315–323 [DOI] [PubMed]
- 5.Collis DK, Mohler CG (1998) Loosening rates and bone lysis with rough finished and polished stems. Clin Orthop 355:113–122 [DOI] [PubMed]
- 6.Collis DK, Mohler CG (2002) Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented stems with essentially the same geometry. J Bone Joint Surg Am 84–A:586–592 [DOI] [PubMed]
- 7.Comba F, Gonzalez Della Valle A, Salvati EA (2005) The role of surface finish on the survivorship of cemented femoral stems for total hip arthroplasty. Minerva Ortop Traumatol 56:65–79
- 8.Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH (1993) Structural and cellular assessment of bone quality of proximal femur. Bone 14:231–242 [DOI] [PubMed]
- 9.Dowd JE, Cha CW, Trakru S, Kim SY, Yang IH, Rubash HE (1998) Failure of total hip arthroplasty with a precoated prosthesis. 4- to 11-year results. Clin Orthop 355:123–136 [DOI] [PubMed]
- 10.Garellick G, Malchau H, Herberts P (1999) The Charnley versus the Spectron hip prosthesis: clinical evaluation of a randomized, prospective study of 2 different hip implants. J Arthroplasty 14:407–413 [DOI] [PubMed]
- 11.Garellick G, Malchau H, Regner H, Herberts P (1999) The Charnley versus the Spectron hip prosthesis: radiographic evaluation of a randomized, prospective study of 2 different hip implants. J Arthroplasty 14:414–425 [DOI] [PubMed]
- 12.Valle AG, Rana A, Nestor B, Bostrom M, Westrich G, Salvati EA (2006) Metallic shedding, surface finish changes, and extensive femoral osteolysis in the loose Spectron EF stem. Clin Orthop 442:165–170 [DOI] [PubMed]
- 13.Gonzalez Della Valle A, Su E, Zoppi A, Sculco TP, Salvati EA (2004) Wear and periprosthetic osteolysis in a match-paired study of modular and nonmodular uncemented acetabular cups. J Arthroplasty 19:972–977 [DOI] [PubMed]
- 14.Della Valle AG, Zoppi A, Peterson MG, Salvati EA (2005) A rough surface finish adversely affects the survivorship of a cemented femoral stem. Clin Orthop 436:158–163 [DOI] [PubMed]
- 15.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141:17–27 [PubMed]
- 16.Harris WH, McGann WA (1986) Loosening of the femoral component after use of the medullary-plug cementing technique. Follow-up note with a minimum five-year follow-up. J Bone Joint Surg Am 68:1064–1066 [PubMed]
- 17.Howell JR Jr, Blunt LA, Doyle C, Hooper RM, Lee AJ, Ling RS (2004) In vivo surface wear mechanisms of femoral components of cemented total hip arthroplasties: the influence of wear mechanism on clinical outcome. J Arthroplasty 19:88–101 [DOI] [PubMed]
- 18.Howie DW, Middleton RG, Costi K (1998) Loosening of matt and polished cemented femoral stems. J Bone Joint Surg Br 80:573–576 [DOI] [PubMed]
- 19.Issack PS, Botero HG, Hiebert RN, Bong MR, Stuchin SA, Zuckerman JD, Di Cesare PE (2003) Sixteen-year follow-up of the cemented spectron femoral stem for hip arthroplasty. J Arthroplasty 18:925–930 [DOI] [PubMed]
- 20.Kale AA, Della Valle CJ, Frankel VH, Stuchin SA, Zuckerman JD, Di Cesare PE (2000) Hip arthroplasty with a collared straight cobalt–chrome femoral stem using second-generation cementing technique: a 10-year-average follow-up study. J Arthroplasty 15:187–193 [DOI] [PubMed]
- 21.Kawate K, Ohmura T, Hiyoshi N, Natsume Y, Teranishi T, Tamai S (1999) Thin cement mantle and osteolysis with a precoated stem. Clin Orthop 365:124–129 [DOI] [PubMed]
- 22.King PJ, Malin AS, Scott RD, Thornhill TS (2004) The fate of patients not returning for follow-up five years after total knee arthroplasty. J Bone Joint Surg Am 86–A:897–901 [DOI] [PubMed]
- 23.Livermore J, Ilstrup D, Morrey B (1990) Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am 72:518–528 [PubMed]
- 24.Malchau H, Herberts P, Eisler T, Garellick G, Soderman P (2002) The Swedish Total Hip Replacement Register. J Bone Joint Surg Am 84–A(Suppl 2):2–20 [DOI] [PubMed]
- 25.Pellicci PM, Bostrom M, Poss R (1998) Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop 355:224–228 [DOI] [PubMed]
- 26.Ramaniraka NA, Rakotomanana LR, Leyvraz PF (2000) The fixation of the cemented femoral component. Effects of stem stiffness, cement thickness and roughness of the cement-bone surface. J Bone Joint Surg Br 82:297–303 [DOI] [PubMed]
- 27.Rasquinha VJ, Ranawat CS (2004) Durability of the cemented femoral stem in patients 60 to 80 years old. Clin Orthop 419:115–123 [DOI] [PubMed]
- 28.Rasquinha VJ, Ranawat CS, Dua V, Ranawat AS, Rodriguez JA (2004) A prospective, randomized, double-blind study of smooth versus rough stems using cement fixation: minimum 5-year follow-up. J Arthroplasty 19:2–9 [DOI] [PubMed]
- 29.Salvati EA, Betts F, Doty SB (1993) Particulate metallic debris in cemented total hip arthroplasty. Clin Orthop 293:160–173 [PubMed]
- 30.Skinner JA, Todo S, Taylor M, Wang JS, Pinskerova V, Scott G (2003) Should the cement mantle around the femoral component be thick or thin? J Bone Joint Surg Br 85:45–51 [DOI] [PubMed]
- 31.Sporer SM, Callaghan JJ, Olejniczak JP, Goetz DD, Johnston RC (1999) The effects of surface roughness and polymethylmethacrylate precoating on the radiographic and clinical results of the Iowa hip prosthesis. A study of patients less than fifty years old. J Bone Joint Surg Am 81:481–492 [DOI] [PubMed]
- 32.Vail TP, Goetz D, Tanzer M, Fisher DA, Mohler CG, Callaghan JJ (2003) A prospective randomized trial of cemented femoral components with polished versus grit-blasted surface finish and identical stem geometry. J Arthroplasty 18:95–102 [DOI] [PubMed]
- 33.Vaughn BK, Fuller E, Peterson R, Capps SG (2003) Influence of surface finish in total hip arthroplasty. J Arthroplasty 18:110–115 [DOI] [PubMed]