Abstract
Dislocation after total hip replacement is more common in the early, postoperative period. Postoperative intraarticular haematoma and remaining seroma fluid and/or weakened posterior soft tissue wall may be contributing factors. Our purpose was to compare and follow with sonography the resorption of the postoperative volume of intraarticular fluid/synovial oedema after total hip arthroplasty (THA) with or without posterior soft tissue repair. Thirty-three consecutive patients with hip osteoarthritis were admitted for THA. All of them received the same type of cemented implant. Patients were randomised for posterior soft tissue repair or not. Sonography, measuring the anterior capsular distension, indicating the volume of intraarticular fluid/synovial oedema in the prosthetic hip joints, was performed after six and 12 months in all patients. At six months postoperatively greater capsular distension, i.e., remaining volume of intraarticular fluid/synovial oedema, was observed in the group with posterior soft tissue repair than in the group without. After one year the capsular distension had decreased in both groups and there was no significant difference between the groups. Our results show that posterior soft tissue repair after THA is associated with increased capsular distension during the first six months. After 12 months the volume of intraarticular fluid/synovial oedema is the same with or without posterior soft tissue repair.
Résumé
La luxation après prothèse totale de la hanche est plus fréquente précocement, en période postopératoire. L’hématome intra-articulaire et /ou l’altération des tissus postérieurs peuvent être des facteurs de cette luxation. Nous avons étudiés par échographie la résorption postopératoire des fluides articulaires et de l’œdème synovial après arthroplastie totale de la hanche faite avec ou sans réparation des tissus postérieurs. 33 patients consécutifs, opérés avec le même type d’implant cimenté furent randomisés vis-à-vis de la réparation, ou non, des tissus postérieurs. L’échographie, mesurant la distension capsulaire antérieure a été faite après 6 et 12 mois chez tous les patients. A 6 mois de l’intervention une augmentation de la distension capsulaire c’est à dire du volume liquidien résiduel était observée dans le groupe avec réparation des tissus postérieurs comparé au groupe sans réparation. Après 1 an la distension décroît dans les deux groupes sans différence significative entre les deux.
Introduction
Dislocation after total hip replacement is one of the common postoperative complications. Dislocation following the posterior approach has been reported to occur in 4–8% of cases [1, 4]. Dissatisfaction with these rates of dislocation resulted in the introduction of different posterior soft tissue repair techniques. Many authors reported statistically significant differences in dislocation rates with and without posterior soft tissue repair [6, 7, 9]. The typical finding when revising a hip for recurrent dislocation is a large fluid-filled dead space immediately behind the fascia lata with no posterior pseudocapsular structure. The purpose of posterior soft tissue repair is to eliminate this fluid-filled space and to create a mechanical support for the prosthetic hip joint posteriorly.
Though rarely used in the examination of symptomatic hip joint and prosthetic hip joint, sonography, measuring the anterior capsular distension due to increased volume of fluid and subsequently pressure, has proven valuable in diagnosing haematoma, synovitis and infection [2, 8, 10, 12]. Capsular distension, i.e., the distance between the anterior joint capsule and the anterior surface of the prosthetic femoral neck measured with sonography, reflects the volume of intraarticular fluid/synovial oedema in the THA and the intracapsular pressure.
The purpose of this study was to determine how the posterior soft tissue repair in THA affects the volume of intraarticular fluid/synovial oedema (capsular distension) in the prosthetic hip at six and 12 months after the operation.
Patients and methods
Thirty-three consecutive, unselected patients were admitted to our department for total hip replacement. The preoperative diagnosis was osteoarthritis in all cases. All patients were operated upon by two experienced hip surgeons using the same surgical technique with a posterior approach, the same implant (ScanHip Classic II cemented stem and ScanHip Standard all-polyethylene cemented cup). Randomising envelopes were drawn prior to surgery selecting the patients for posterior soft tissue repair or not.
The posterior soft tissue repair included reattaching the piriformis and conjoined tendons together with the remaining posterior capsule to the greater trochanter through drill holes after the prosthesis had been implanted and the joint reduced. In the second group of patients the posterior soft tissues were not reattached. In all cases The posterior capsular incision was similar and no anterior capsule resection or release was performed. An active wound drainage system was used for a period of one day in all cases.
The patients were called for review with sonography six and 12 months postoperatively. The sonographic examinations were performed in a sagittal plane, from the anterior aspect of the hip along the axis of the femoral neck [3]. The anterior capsular distance, i.e., the capsular distension, was defined as the distance between the metallic echo from the anterior surface of the prosthetic femoral neck and the echo from the anterior surface of the anterior capsule (Figs. 1 and 2). The capsular distension was measured three times in all hips. The sonographic measurements were performed by the same examiner (S.T.), experienced in prosthetic hip ultrasound, at six and 12 months without prior knowledge of the randomisation. At 12-month follow-up 27 patients were examined. All measurements are presented in Table 1. Two patients in the nonrepair group and four patients in the repair group did not attend the follow-up and were excluded from calculations at 12 months.
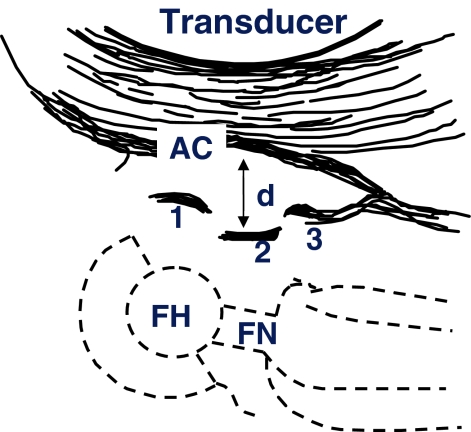
Fig. 1.
Schematic drawing showing sonographic findings in THA patients. FH Prosthetic femoral head; FN prosthetic femoral neck; AC anterior capsule; d distance between anterior capsule and prosthetic femoral neck; 1 echo from FH; 2 echo from FN; 3 echo from prosthetic collar (not always present)
Fig. 2.
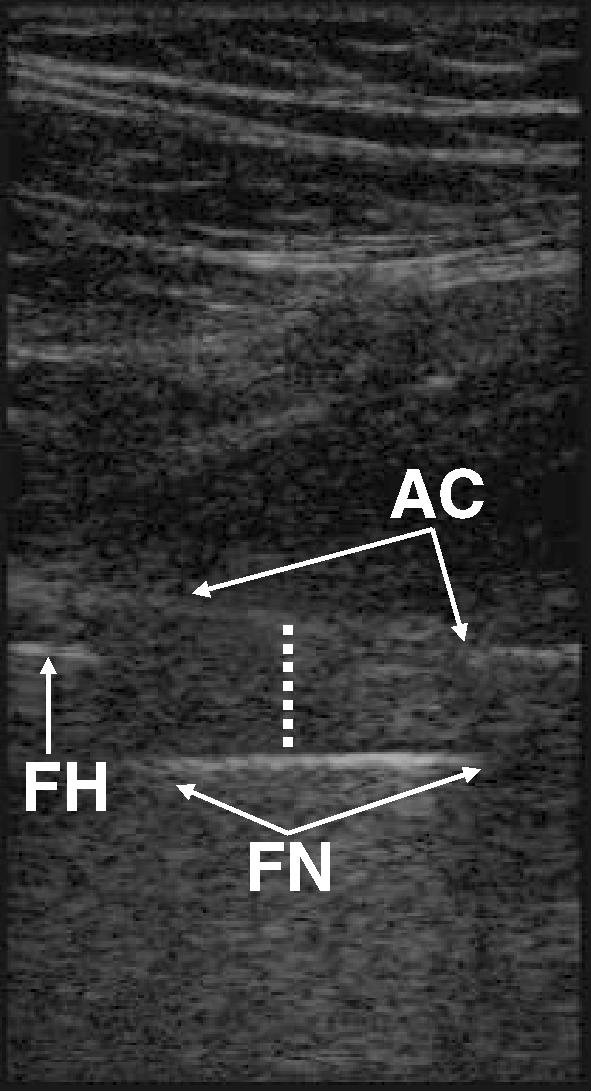
Sonographic measurement of the “capsular distance” in THA. AC Echo from anterior surface of anterior hip joint capsule; FN echo from anterior surface of prosthetic femoral neck; FH echo from anterior surface of prosthetic femoral head; dotted line distance between anterior capsule and prosthetic femoral neck
Table 1.
Measurements of capsular distension values
| Patient number | Posterior soft tissues | Capsular distance at 6 months | Capsular distance at 12 months |
|---|---|---|---|
| 1 | Not repaired | 1.95 | 1.49 |
| 2 | Not repaired | 1.29 | 1.91 |
| 3 | Not repaired | 1.12 | 1.13 |
| 4 | Not repaired | 1.19 | 1.28 |
| 5 | Not repaired | 1.32 | 1.21 |
| 6 | Not repaired | 0.90 | 0.62 |
| 7 | Not repaired | 1.64 | 1.42 |
| 8 | Not repaired | 1.10 | 0.93 |
| 9 | Not repaired | 1.06 | 1.12 |
| 10 | Not repaired | 1.66 | 0.60 |
| 11 | Not repaired | 1.28 | 1.13 |
| 12 | Not repaired | 1.68 | 1.30 |
| 13 | Not repaired | 1.33 | 1.49 |
| 14 | Repaired | 1.71 | 1.21 |
| 15 | Repaired | 1.75 | 1.65 |
| 16 | Repaired | 1.78 | 1.55 |
| 17 | Repaired | 1.78 | 1.42 |
| 18 | Repaired | 2.03 | 1.43 |
| 19 | Repaired | 1.99 | 2.14 |
| 20 | Repaired | 1.45 | 1.60 |
| 21 | Repaired | 1.78 | 1.04 |
| 22 | Repaired | 1.67 | 1.51 |
| 23 | Repaired | 1.18 | 1.40 |
| 24 | Repaired | 2.05 | 0.83 |
| 25 | Repaired | 1.73 | 1.63 |
| 26 | Repaired | 1.47 | 1.29 |
| 27 | Repaired | 1.36 | 0.99 |
The study design was approved by the ethics committee of the institution.
Statistics
To assess the differences in capsular distension values between the two groups, the Mann–Whitney test was used. To assess the differences in measurements within the groups after six and 12 months, the nonparametric Wilcoxon signed-rank test was used. A p value of 0.05 or lower was considered significant.
Results
Patients’ related data are presented in Table 2. The median capsular distension measured in 33 patients after six months in the posterior soft tissue repair patients was 1.695 cm( SD 0.25), whereas in the patients whose posterior soft tissues were not repaired it was 1.347 cm (SD 0.30), (p=0.001); power coefficient 0.87. After 12 months the median capsular distension was 1.406 cm (SD 0.33) and 1.202 cm (SD 0.36), (p=0.11), respectively, in 27 hips (Fig. 3). Exclusion from the study of the six patients lost at the 12 months follow-up would not have affected the statistical significance of the results.
Table 2.
Patient’s related data
| Characteristic | With posterior soft tissue repair | Without posterior soft tissue repair | ||
|---|---|---|---|---|
| Six months after THA (n=18) | Twelve months after THA (n=14) | Six months after THA (n=15) | Twelve months after THA (n=13) | |
| Age (mean) | 70.1 (SD 7.9) | 70 (SD 5.7) | 70.5 (SD 8.0) | 70.6 (SD 8.5) |
| Gender | Male 7, female 11 | Male 6, female 8 | Male 4, female 11 | Male 4, female 9 |
| Weight (mean) | 79 (SD 13.7) | 78 (SD 15.2) | 82 (SD 12.2) | 81(SD 13.0) |
| Height (mean) | 1.69 (SD 0.2) | 1,70 (SD 0.2) | 1.66 (SD 9.9) | 1,65 (SD 9.7) |
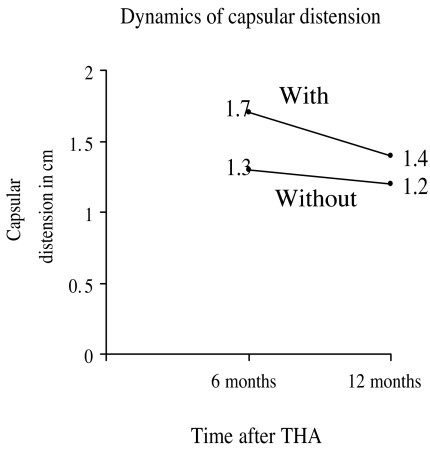
Fig. 3.
The dynamic of changes in capsular distension with and without posterior soft tissue repair at 6 and 12 months after THA
We evaluated the dynamics of capsular distension changes over time in both groups: the decrease in capsular distension from six to 12 months postoperatively was significant in the posterior soft tissue repair group (p=0.046), power coefficient 0.64, but not in the nonrepaired group (p=0.13).
One patient in the nonrepaired group suffered dislocation of the hip three times after we evaluated her at six months. The positioning of prosthetic components was good. All dislocations occurred during the eighth postoperative month and were treated with closed reduction. On continued sonography in this case at 12 months postoperatively the capsular distension was 0.6 cm, compared with 1.66 cm at six months.
Discussion
It has been suggested that the “dead space” with a large amount of fluid which is a common finding during hip revision for recurrent dislocations is the result of the dislocation trauma [4], whereas other authors propose another interpretation, i.e., that the dead space is in itself the cause of the dislocation [6]. Based on findings by Wingstrand and Wingstrand [12], enclosed and increased postoperative amounts of free fluid may be one contributing factor in dislocations of the THA hip due to the fact that the stabilising effect of the atmospheric pressure is eliminated if there is a significant volume of free fluid remaining in the joint.
According to Pellicci et al. [6] posterior soft tissue repair should eliminate the “dead space” and decrease the amount of fluid in the hip joint. We found the opposite, i.e., increased capsular distension in the posterior soft tissue repair group six months after surgery. Thus, it seems that posterior soft tissue repair resulted in enclosure of the postoperative hematoma and consequently a longer-lasting intraarticular seroma in the postoperative period. Closing the hip joint with posterior soft tissue repair may thus result in a closed cavity that delays the resorption of the seroma.
The anterior capsular distance in the posterior soft tissue repair group decreases with time, as demonstrated by our significantly lower capsular distension 12 months postoperatively. The majority of postoperative dislocations following THA occur within the first three months after operation [6, 9]. Our measurements suggest that posterior soft tissue repair has not eliminated the dead space after six months compared with the nonrepaired group. The decreased dislocation rates in previous studies [6,9] thus could be explained only by the posterior mechanical support. The significant difference in capsular distension at six months between patients with and without posterior repair supports the idea that the soft tissue reattachment is strong enough and remains intact postoperatively. Mihalko and Whiteside [5] reported that the posterior soft tissue repair can remain intact event if the hip dislocates.
One patient in the nonrepaired group experienced dislocation three times at eight months. The capsular distension was drastically reduced after 12 months, possibly due to pseudocapsule rupture after the third dislocation and spontaneous evacuation of the fluid from the hip joint.
We conclude that posterior soft tissue repair in THA does not eliminate, but actually increases, the postoperative intraarticular dead space.
Acknowledgement
This study was supported by the Pfizer EU ARTICULUM Fellowship.
References
- 1.Fackler CD, Poss R (1980) Dislocation in total hip arthroplasties. Clin Orthop 151:169–178 [PubMed]
- 2.Földes K, Gaal M, Balint P, Nemenyi K, Kiss C, Balint G, Buchanan W (1992) Ultrasonography after hip arthroplasty. Skeletal Radiol 21(5):297–299 [DOI] [PubMed]
- 3.Kesteris U, Jonsson K, Robertsson O, Onnerfalt R, Wingstrand H (1999) Polyethylene wear and synovitis in total hip arthroplasty: A sonographic study of 48 hips. J. Arthroplasty 14(2):138–143 [DOI] [PubMed]
- 4.McCollum DE, Gray WJ (1990) Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop 261:159–170 [PubMed]
- 5.Mihalko WM, Whiteside LA (2004) Hip mechanics after posterior soft tissue repair in total hip arthroplasty. Clin Orthop Relat Res 420:194–198 [DOI] [PubMed]
- 6.Pellicci PM, Bostrom M, Poss R (1998) Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res 355:224–228 [DOI] [PubMed]
- 7.Suh KT, Park BG, Choi YJ (2004) A posterior approach to primary total hip arthroplasty with soft tissue repair. Clin Orthop Relat Res 418:162–167 [DOI] [PubMed]
- 8.van Holsbeeck MT, Eyler WR, Sherman LS, Lombardi TL, Mezger E, Verner JJ, Schurman JR, Jonsson K (1994) Detection of infection in loosened hip prostheses: efficacy of sonography. AJR Am J Roentgenol 163(2):381–384 [DOI] [PubMed]
- 9.Weeden SH, Paprosky WG, Bowling JW (2003) The early dislocation rate in primary total hip arthroplasty following the posterior approach with posterior soft-tissue repair. J Arthroplasty 18(6):709–713 [DOI] [PubMed]
- 10.Wingstrand H, Egund N, Nilsson L T, Strömqvist B (1998) Acetabular fracture causing hip joint tamponade. Acta Orthop Scand 59(3):323–325 [DOI] [PubMed]
- 11.Wingstrand H, Strömqvist B, Egund N, Gustafson T, Nilsson LT, Thorngren KG (1986) Hemarthrosis in undisplaced cervical fractures. Tamponade may cause reversible femoral head ischemia. Acta Orthop Scand 57(4):305–308 [DOI] [PubMed]
- 12.Wingstrand H, Wingstrand A (1997) Biomechanics of the hip joint capsule—a mathematical model and clinical implications. Clin Biomech 22(5):273–280 [DOI] [PubMed]