Abstract
Airway complications after anterior cervical surgery are rare but potentially lethal. The purpose of this study was to identify the natural course of prevertebral soft tissue swelling after one- or two-level anterior cervical discectomy and fusion (ACDF) in order to prevent lethal airway obstruction after ACDF. Eighty-seven patients scheduled for one- or two-level ACDF were studied prospectively. Lateral radiographs of the cervical spine were taken preoperatively, postoperatively on the day of surgery and on the first, second, third, fourth, and fifth days after operation. Prevertebral soft tissue was measured from C2 to C6 on cervical spine lateral radiographs. The anteroposterior (AP) thickness of the prevertebral soft tissue was measured at each cervical level from C2 to C6. Prevertebral soft tissue swelling occurred postoperatively and increased markedly on the second day after operation. The maximum swelling was found on the second and third days. In fusions above C5 swelling was most prominent at C2, 3. Gradual decrease in swelling was observed after the fourth postoperative day. Prominent swelling was noted at the second, third, and fourth cervical levels. There was no significant difference in swelling when comparing one-level and two-level ACDF. Only one patient required reintubation (1.1%). In conclusion, in this prospective study of 87 patients fused at one or two levels in the cervical spine peak prevertebral soft tissue swelling was observed on the second and third days after the surgery.
Résumé
Les complications aériennes après chirurgie cervicale antérieure sont rares mais potentiellement léthales. Le sujet de ce travail est d’étudier l’évolution de l’œdème prévertébral après discectomie antérieure et fusion à un ou deux niveaux ( ACDF) pour prévenir une obstruction aérienne. 87 patients devant avoir un ACDF a un ou deux niveaux étaient étudiés prospectivement. Des radiographies de profil de la colonne cervicale ont été faites avant l’opération, après l’opération le jour de la chirurgie, puis les premier, deuxième, troisième, quatrième et cinquième jours après. Les parties molles prévertébrales étaient mesurées de C2 à C6 sur ces radiographies. L’œdème prévertébral apparaissait en postopératoire et avait une augmentation marqué le deuxième jour après la chirurgie. Dans les fusions au-dessus de C5 l’œdème prédominait en C2, C3. La régression de l’œdème était observée après le quatrième jour post-opératoire. Un œdème prononcé était noté aux deuxième, troisième et quatrième niveau cervical. Il n’y avait pas de différence significative dans l’oedème en comparant un et deux niveaux de discectomie-fusion. Seulement 1 patient a eu besoin d’une ré-intubation (1,1%). En conclusion , dans cette série, l’acmé de l’œdème prévertébral était observée les deuxième et troisième jours après l’opération.
Introduction
Acute airway obstruction is a potentially lethal complication after anterior cervical spine surgery. The causes of acute airway obstruction are haematoma, cerebrospinal fluid, or prevertebral soft tissue swelling [1–3, 5–12]. Mortality due to prevertebral soft tissue swelling is very rare but does occur [5, 12]. Moreover, the airway obstruction due to prevertebral soft tissue swelling is unpredictable.
Airway obstruction after anterior cervical discectomy and fusion (ACDF) has not been prospectively studied. There were a few reports concerning airway obstruction after anterior cervical surgery, but most of the studies were retrospective and limited to multilevel surgical cases and other risk factors [1–3, 5–12].
The purpose of this study was to identify the occurrence of prevertebral soft tissue swelling after ACDF with the objective of preventing potentially lethal airway obstruction after ACDF.
Materials and methods
This study was a prospective study of 87 consecutive patients scheduled for one- or two-level ACDF for degenerative disc disease of the cervical spine. There were 62 male and 25 female patients. The mean age was 50.2 years (range: 30–76).
Graft material was tricortical autogenous iliac bone in all patients. Plate and screw fixation was also performed in all patients. ACDF was performed at one level in 56 patients and two levels in 31 patients. ACDF was performed proximal to the C5 in 29 patients and distal to the C5 in 58 patients. Mean duration of surgery was 57 min for one-level and 79 min for two-level ACDF. A self-retaining retractor was used during discectomy and preparation of the end plate. The mean actual retraction time for the self-retaining retractor was 15 min for one level. A handheld retractor was used during tricortical iliac bone graft insertion and plate and screw fixation. A suction drain was used in all patients and remained for 24 h. An orogastric or nasogastric tube was not used. After the operation, steroids were not given for swelling.
Plain cervical spine lateral radiographs in the standing position were taken preoperatively, immediately postoperatively, and then daily for 5 days after the operation. The anteroposterior (AP) thickness of the prevertebral soft tissue was measured at each cervical level from C2 to C6 on the cervical spine lateral radiographs using a PACS digital measuring instrument. The distance from the cassette to the tube was standardised at three feet.
The measurement of the soft tissue space was made on the line parallel to the upper end plate from the midpoint of the anterior surface of each vertebral body to the border of the airway shadow (Fig. 1).
Fig. 1.
The prevertebral soft tissue was measured as the distance between the anterior surface of each vertebral body and the air shadow of the airway
This prospective study was approved by the University Institutional Review Board.
Three independent observers measured the prevertebral soft tissue space and the measurements were repeated by each observer two weeks later. Both inter- and intraobserver reliabilities were evaluated using Pearson’s correlation analysis.
Changes of prevertebral soft tissue swelling depending on time were analyzed using the paired sample t-test. Peak swelling time and time to decrease swelling were checked. We also checked the location of the most prominent swelling.
One-level and two-level groups, male and female groups, and proximal to C5 and distal to C5 surgery groups were compared using the independent sample t-test.
Results
The AP dimension of the prevertebral soft tissue at C2 was 3.5 mm preoperatively and significantly increased to 5.1 mm postoperatively (P=0.000), to 6.9 mm on the first day (P=0.010), and to 10.2 mm on the second day (P=0.000). This AP dimension at C2 decreased to 9.7 mm on the third day (P=0.349), to 7.2 mm on the fourth day (P=0.008), and to 5.9 mm on the fifth day (P=0.000).
The AP dimension of the prevertebral soft tissue at C3 was 3.7 mm preoperatively and significantly increased to 6.1 mm postoperatively (P=0.000), to 8.9 mm on the first day (P=0.000), to 12.7 mm on the second day (P=0.000), and to 12.9 mm on the third day (P=0.911). There was a significant decrease to 10.4 mm on the fourth day (P=0.011) and to 9.0 mm on the fifth day (P=0.019).
The AP dimension of the prevertebral soft tissue at C4 was 6.1 mm preoperatively and significantly increased to 9.7 mm postoperatively (P=0.000), to 12.0 mm on the first day (P=0.000), to 14.5 mm on the second day (P=0.002), and to 14.7 mm on the third day (P=0.936). It significantly decreased to 13.0 mm on the fourth day (P=0.037) and to 12.0 mm on the fifth day (P=0.002).
The AP dimension of the prevertebral soft tissue at C5 was 14.4 mm preoperatively and significantly increased to 16.2 mm postoperatively (P=0.000). It was 17.2 mm on the first day (P=0.161), 17.6 mm on the second day (P=0.332), 18.0 mm on the third day (P=0.608), 16.6 mm on the fourth day (P=0.056), and 16.8 mm on the fifth day (P=0.077). These measurements do not reflect a significant difference after the first postoperative day.
The AP dimension of the prevertebral soft tissue at C6 was 15.5 mm preoperatively and significantly increased to 17.2 mm postoperatively (P=0.000). It was 17.8 mm on the first day (P=0.339), 17.3 mm on the second day (P=0.459), 18.0 mm on the third day (P=0.608), 18.0 mm on the fourth day (P=0.756), and 18.0 mm on the fifth day (P=0.577). These measurements do not reflect a significant difference after the first postoperative day (Table 1).
Table 1.
Serial measurements (mm) of prevertebral soft tissue
| Level | Preop | Postop | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 |
|---|---|---|---|---|---|---|---|
| C2 | 3.5 | 5.1 | 6.9 | 10.2 | 9.7 | 7.2 | 5.9 |
| C3 | 3.7 | 6.1 | 8.9 | 12.7 | 12.9 | 10.4 | 9.0 |
| C4 | 6.1 | 9.7 | 12.0 | 14.5 | 14.7 | 13.0 | 12.0 |
| C5 | 14.4 | 16.2 | 17.2 | 17.6 | 18.0 | 16.6 | 16.8 |
| C6 | 15.5 | 17.2 | 17.8 | 17.3 | 18.0 | 18.0 | 18.0 |
The mean Pearson’s correlation coefficient for single observer was 0.988 (range: 0.984–0.992). The mean Pearson’s correlation coefficient between observers was 0.946 (range: 0.932–0.964).
The prevertebral soft tissue swelling was increased postoperatively and continuously increased till the second day. On the 3rd day the swelling reached a plateau. The peak swelling was found on the 2nd and 3rd days after the operation, and after the third day, the swelling subsided. These changes were obvious at the second, third, and fourth cervical levels.
There were no significant differences between the one-level surgery group and the two-level surgery group (P=0.116–0.984). There were also no significant differences between the male and female groups (P=0.259–0.801).
Prevertebral soft tissue swelling was significantly more severe in the groups fused proximal to C5 than in the fusions distal to C5. These changes were prominent at the C2 and C3 levels (P<0.05). However, there were no significant differences in prevertebral soft tissue swelling at the C4, C5, and C6 levels between the two groups (Table 2).
Table 2.
Comparison of prevertebral soft tissue between the proximal to C5 surgery group (Prox) and distal to C5 surgery group (Dist) in mm
| Level | Preop | Postop | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prox | Dist | Prox | Dist | Prox | Dist | Prox | Dist | Prox | Dist | Prox | Dist | Prox | Dist | |
| C2 | 3.6 | 3.5 | 6.4 | 4.5 | 8.4 | 5.0 | 13.1 | 8.5 | 11.2 | 8.7 | 9.2 | 6.1 | 8.1 | 4.9 |
| C3 | 3.9 | 3.6 | 7.3 | 5.6 | 11.7 | 6.8 | 15.5 | 11.0 | 14.1 | 12.0 | 10.8 | 10.1 | 11.1 | 7.9 |
| C4 | 5.9 | 6.2 | 9.8 | 9.7 | 13.0 | 11.1 | 16.6 | 13.2 | 15.1 | 14.5 | 13.5 | 12.6 | 13.9 | 11.1 |
| C5 | 13.7 | 14.8 | 15.6 | 16.4 | 17.6 | 16.9 | 17.9 | 17.4 | 17.7 | 18.2 | 16.4 | 16.8 | 17.8 | 16.3 |
| C6 | 15.6 | 15.3 | 17.2 | 17.1 | 18.5 | 17.6 | 17.7 | 17.0 | 18.0 | 18.1 | 17.8 | 18.1 | 18.9 | 17.6 |
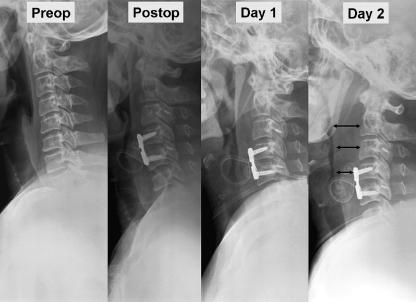
One patient (1.1%) needed reintubation due to acute airway obstruction caused by prevertebral soft tissue swelling (Fig. 2).
Fig. 2.
ACDF C4-5 was performed due to disc herniation at C4-5 in a 42-year-old male patient. The second day after the surgery, he complained of severe dyspnea. Cervical spine lateral radiography showed severe prevertebral soft tissue swelling
Discussion
Acute airway obstruction is a potentially lethal complication after anterior cervical spine surgery, and accordingly, many authors have studied airway obstruction due to haematoma or prevertebral soft tissue swelling in patients with cervical spine trauma [4]. However, airway obstruction after anterior cervical spine surgery has not been prospectively investigated, probably because of the low incidence of acute airway obstruction in these cases. Prevertebral soft tissue swelling can happen in any patient, and mortality due to prevertebral soft tissue swelling may occur [5, 12]. Moreover, the airway obstruction due to prevertebral soft tissue swelling is unpredictable.
There have been a few reports concerning airway obstruction after anterior cervical surgery. Emery et al. reported upper airway obstruction after multilevel cervical corpectomy in seven patients. The airway obstruction was due to oedema rather than haematoma, and their risk factors were smoking and asthma [5]. Fujiwara et al. reported that four of 171 patients who had undergone anterior cervical spine surgery needed reintubation. The four patients were fused to C3. They surmised that the upper airway obstruction due to the intense swelling of the soft tissue at C3 may have been the reason for postoperative reintubation [7]. Epstein et al. used direct fiberoptic visualization of reactive tracheal swelling before extubation to decrease the emergency reintubation rate after multilevel cervical corpectomy and fusion. Their risk factors were prolonged operative time, obesity, transfusion, reoperations, surgery at C2, four-level corpectomy and fusion, and asthma [6]. Sagi et al. retrospectively studied 311 patients who had undergone anterior cervical spine surgery. Their incidence of airway obstruction was 6.1% and reintubation rate was 1.9%. Their risk factors were prolonged operation time, three-level surgery, and blood loss of more than 300 ml [12].
As mentioned above, all of the previous studies relating to airway obstruction following anterior cervical spine surgery were retrospective and limited to multilevel surgery cases and risk factors. However, airway obstruction after anterior cervical spine surgery can occur in one- or two-level cases [7].
Our study was performed prospectively with 87 consecutive patients who were scheduled for one- or two-level ACDF due to degenerative disc disease of the cervical spine. Haematoma formation may cause acute airway obstruction after anterior cervical spinal surgery [11] but can be prevented by meticulous haemostasis and the use of a suction drain.
In this study the main cause of acute airway obstruction was considered to be prevertebral soft tissue swelling as Emery et al. suggested [5] because a suction drain was used routinely in all patients. The prevertebral soft tissue was measured on plain cervical spine lateral radiographs. This method was derived from a study by DeBehnke and Havel, who measured prevertebral soft tissue to identify cervical spinal fracture [4]. We concluded that this method was useful for evaluating prevertebral soft tissue swelling not only in patients with cervical trauma but also in patients after anterior cervical spinal surgery.
There have been no prospective studies concerning the natural history of the swelling of the prevertebral soft tissue after anterior cervical spinal surgery. Therefore, in this study, we measured prevertebral soft tissues serially (preoperatively, postoperatively, on the 1st, 2nd, 3rd, 4th, and 5th days) to identify the short-term natural course of the prevertebral soft tissue swelling. Prevertebral soft tissue swelling occurred in all patients.
The peak prevertebral soft tissue swelling was found on the second and third days after the operation. Therefore, if a patient is going to remain intubated after a long and difficult procedure above C5, we maintain intubation until after the peak swelling at three days rather than just overnight.
Uppal and Akmakjian presented outpatient cervical fusion at the NASS meeting in 1999. They discharged the patients who underwent ACDF within 23 h. They reported that outpatient ACDF was a cost-effective method with excellent overall patient satisfaction [13]. Considering the low rate of reintubation (1.1%) in the current study, routine close observation of the patients for three days would seem to be unnecessary. However, the peak prevertebral soft tissue swelling occurs on the 2nd and 3rd days after surgery as shown in our study. Therefore, after a long and difficult procedure, we observe the patients for two or three days after the operation.
The predominant swelling of the prevertebral soft tissue was observed at the C2, C3, and C4 levels. These findings were similar to those of Fujiwara et al. which stated that upper airway obstruction was due to serious swelling of the soft tissue surrounding C3 [7]. There were no significant differences between the one-level surgery group and two-level surgery group. We attributed this finding to the lack of significant differences between the two groups in operating time and amount of blood loss. The studies of Sagi et al. [12] and Epstein et al. [6] suggest that if three- or four-level corpectomy and fusion cases had been included in this study, there would have been significant differences between the groups depending on the number of fusion levels.
In this study, prevertebral soft tissue swelling was significantly more severe in the proximal to C5 surgery group than in the distal to C5 surgery group and the swelling was predominant at the C2 and C3 levels. These findings were similar to the study of Fujiwara et al. in which all of the reintubated patients had fused to C3 [7].
A limitation of the current study was the lack of correlation between respiratory difficulty and prevertebral soft tissue swelling. We could not determine the correlations because of individual variations between patients.
Conclusion
In this prospective study of 87 patients fused at one or two levels in the cervical spine, peak prevertebral soft tissue swelling was observed on the second and third days after the operation.
References
- 1.Arimune M, Sanjou H, Yamada T, Yabe M, Miyake H (2004) Minitracheostomy in treating upper airway obstruction after anterior cervical fusion. Masui 53(10):1193–1196 [PubMed]
- 2.Chang HS, Kondo S, Mizuno J, Nakagawa H (2004) Airway obstruction caused by cerebrospinal fluid leakage after anterior cervical spine surgery. A report of two cases. J Bone Joint Surg Am 86:370–372 [DOI] [PubMed]
- 3.Coe JD, Vaccaro AR (2005) Complications of anterior cervical plating. In: Clark CR (ed) The cervical spine. Lippincott Williams & Wilkins, Philadelphia, PA, pp 1163–1164
- 4.DeBehnke DJ, Havel CJ (1994) Utility of prevertebral soft tissue measurements in identifying patients with cervical fracture. Ann Emerg Med 24(6):1119–1124 [DOI] [PubMed]
- 5.Emery SE, Smith MD, Bohlman HH (1991) Upper-airway obstruction after multilevel cervical corpectomy for myelopathy. J Bone Joint Surg Am 73:544–551 [PubMed]
- 6.Epstein NE, Hollingsworth R, Nardi D et al (2001) Can airway complications following multilevel anterior cervical surgery be avoided? J Neurosurg 94(2s):185–188 [DOI] [PubMed]
- 7.Fujiwara H, Nakayama H, Takahashi H et al (1998) Postoperative respiratory disturbance after anterior cervical fusion. Masui 47(4):475–478 [PubMed]
- 8.Harris OA, Runnels JB, Matz PG (2001) Clinical factors associated with unexpected critical care management and prolonged hospitalization after elective cervical spine surgery. Crit Care Med 29:1889–1902 [DOI] [PubMed]
- 9.Krnacik MJ, Heggeness MH (1997) Severe angioedema causing airway obstruction after anterior cervical surgery. Spine 22(18):2188–2190 [DOI] [PubMed]
- 10.Penberthy A, Roberts N (1998) Recurrent acute upper airway obstruction after anterior cervical fusion. Anesth Intensive Care 26(3):305–307 [DOI] [PubMed]
- 11.Riew KD, Won DS, DellaRocca GJ (2001) Parameters for maintaining intubation postoperative following anterior cervical procedures. Paper presented at the Cervical Spine Research Society 29th Annual Meeting 2001, Monterey, CA
- 12.Sagi HC, Beutler W, Carroll E (2002) Airway complications associated with surgery on the anterior cervical spine. Spine 27(9):949–953 [DOI] [PubMed]
- 13.Uppal GS, Akmakjian J (1999) Outpatient cervical spine fusions. Abstract book of 1fourth Annual Meeting of North American Spine Society, p 158