Abstract
Lumbar burst fractures (L3–L5) represent a small percentage of all spinal fractures. The treatment of fractures involving the lumbar spine has been controversial. Lamina fractures may be complete or of the greenstick type. Dural tears and nerve root entrapment may accompany these lamina fractures. The aim of this retrospective study was to determine the incidence of dural tear in patients who had lumbar burst fractures with greenstick lamina fractures and the importance of these lamina fractures when choosing the optimum treatment. Twenty-six patients with 28 lumbar burst fractures were treated from 1995 through 2002. The average follow-up was 60 months (range 32–110 months). The male to female ratio was 21:5 and the mean age was 37 years (17–64). Dural tear was detected in seven (25%) out of 28 burst fractures. The functional outcome of the entire study group was assessed using the Smiley-Webster Scale. Good to excellent results were obtained in 24 (92%) of 26 patients. Lumbar burst fractures with greenstick lamina fractures occur mostly in the L2–L4 area. In the surgical treatment, any reduction manoeuvre will close the fracture and crush the entrapped neural elements. Therefore, it may be better to explore the greenstick lamina fracture whether there is any neural entrapment or not, before any reduction manoeuvre is attempted.
Résumé
Les fractures de la colonne lombaire basse représentent un petit pourcentage de toutes les fractures du rachis. Le traitement de ces fractures est controversé. Les fractures des arcs postérieurs peuvent être complètes ou en «bois vert». Des plaies durales ou des racines nerveuses peuvent être concomitantes de ces fractures. Le but de cette étude rétrospective a été de déterminer l’incidence des lésions durales chez les patients présentant une fracture lombaire basse, avec lésions des arcs postérieurs en «bois vert», de poser des indications sur le traitement optimum de ces fractures. Vingt-six patients avec 28 fractures basses ont été traités de 1995 à 2002. Le suivi de ces patients a été de 60 mois (32 à 110 mois), avec une prédominance masculine (5 femmes pour 21 hommes) et un âge moyen de 37 ans (17 à 64 ans). Des lésions durales ont été détectées chez 7 patients (25% des 28 fractures). Le résultat fonctionnel de tout le groupe a été analysé selon l’échelle de Smiley-Webster. Les résultats ont été bons ou excellents dans 92% des cas (24 des 26 patients). Le traitement des fractures lombaires basses avec lésions des arcs postérieurs incomplets en «bois vert» est surtout fréquent en L2, L3, L4. Le traitement chirurgical doit permettre de fixer les fractures lamaires et de libérer les éléments neurologiques. Pour cette raison nous recommandons d’explorer les fractures en «bois vert» des arcs postérieurs qu’il y ait ou non des lésions neurologiques et avant toute manœuvre de réduction.
Introduction
Burst fracture of the lumbar spine is defined as a failure of at least the anterior and middle columns of a vertebral segment because of axial compression, usually associated with some flexion [6].
Lumbar burst fractures (L3–L5) represent a small percentage of all spinal fractures. The treatment of fractures involving the lumbar spine has been controversial. Low lumbar burst fractures have distinct biomechanical and anatomical features. Treatment and management considerations for low lumbar fractures are somewhat different than for the rest of the axial skeleton. Burst fractures of the lumbar spine are the result of axial compressive forces with an associated flexion moment, creating a kyphotic deformity in a normally lordotic spine.
There is often a retropulsion of one or more bony fragments into the neural canal with or without fractures in the lamina. Lamina fractures may be complete or of the greenstick type. Dural tears and nerve root entrapment may accompany lamina fractures, but it is not possible to determine their existence unequivocally by clinical and radiological methods before surgical treatment [15, 17].
The aim of this retrospective study was to determine the incidence of dural tear in patients who had lumbar burst fractures with greenstick lamina fractures and the importance of greenstick lamina fractures in choosing the appropriate treatment.
Patients and methods
Twenty-six patients with 28 low lumbar burst fractures were treated from 1995 through 2002. Each patient had anteroposterior and lateral radiographs, computed tomography and/or magnetic resonance imaging scans.
Anteroposterior and lateral radiographs were used to determine the local kyphotic angle, widening of interpedicular distance, sagittal index and the percentage loss of height of the anterior and middle column. The amount of bony retropulsion to the spinal canal was calculated from the computed tomography scans and recorded.
All the patients with burst fractures and greenstick lamina fracture were explored using the open book laminoplasty technique with the posterior approach; if there was any dural tear and nerve root entrapment, it was then repaired [8–10]. After posterior stabilisation (if indicated) anterior decompression and fusion were performed.
Functional results for all patients were based on comparison of the patients’ occupational and recreational status before and after the injury. These results were classified as excellent, good, fair or poor according to the Smiley-Webster Scale.
Results
Twenty-six patients (28 low lumbar burst fractures) were treated with an average follow-up of 60 months (range 32–110 months). The male to female ratio was 21:5 and the mean age was 37 years (range 17–64). The most common aetiological factor was a fall from a height (24 out of 26). Indications for surgery were neurological impairment in nine patients and/or instability/deformity in 19 patients. Four patients were treated with the anterior, 12 patients with the posterior and ten patients with the combined approach.
Dural tear was detected in seven (25%) out of 28 burst fractures (Fig. 1). We observed that the mean separation of the edges in greenstick fractures with and without dural tear was 4.35 mm (range 2.1–8 mm) and 1.89 mm (range 1–2.5 mm) respectively. All patients with green stick lamina fractures underwent open book laminectomy, replacement of the roots within the dural sac, and primary dural repair in addition to instrumentation and fusion procedures. Six patients showed complete neurological recovery at follow-up and one was neurologically intact prior to surgery and remained the same.
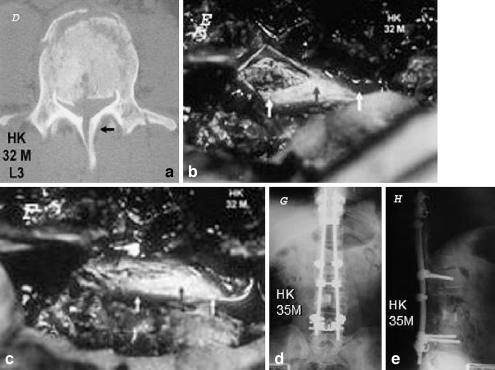
Fig. 1.
a A 32-year-old man with an L2–L3 burst fracture (with neurological deficit) with green stick lamina fracture at both sites. Open book laminoplasty was performed and b dural tear with nerve root entrapment was c repaired. d, e The patient is neurologically intact after 3 years’ follow-up
The functional outcome of the entire study group was assessed using the Smiley-Webster Scale. Good to excellent results were obtained in 24 (92%) out of 26 patients.
Discussion
Posterior dural tears associated with lumbar burst fractures were first reported by Miller et al. [14]. They documented the presence of dural lacerations and the herniation of the cauda equina in patients with thoracolumbar burst fractures associated with the separation of pedicles, and pointed out that neural elements were often entrapped between the fracture fragments of lamina. Denis and Burkus [8] noted a vertical lamina fracture that had occurred secondary to splaying of the posterior arch of the vertebra under axial loading, and described these as a greenstick fractures of the anterior cortex of the lamina. In our cases, the percentage increase in interpedicular distance was significantly higher (p< 0.01) in patients with dural tear than in patients without dural tear. Recently, these injuries have been well demonstrated with CT scan and MRI techniques.
Under axial loading (fall from a height) the pedicles and the posterior elements splay laterally and the bone is retropulsed from the vertebral body, which can cause the dura to protrude between the lamina fracture fragments. After dissipation of axial loading, the nerve roots and the dura are entrapped [2].
Neurological injury has been reported to occur in 30–60% of patients with thoracolumbar burst fractures [12, 18]. The content and size of the neural canal distinguish the lumbar area from other regions. The cauda equina alone occupies the spinal canal caudal to the second lumbar level and injury in this area simulates a peripheral nerve injury with the potential for spontaneous recovery, unlike injuries above this level which affect the spinal cord or conus medullaris. Additionally, the dimensions of the spinal canal are greater here than in any other region and, indeed, there have been several reports of decreases of as much as 90% in the cross-sectional area of the spinal canal without a neurological deficit especially at L4–L5. These features help to explain the infrequency of severe neurological deficits and the potential neurological recovery when such a fracture is present [1].
It has been reported that there is a significant association between a dural tear and neurological deficit [1, 5, 14, 16]. In our series, only one of our patients with dural tear and nerve root entrapment was neurologically normal before surgical treatment. Often the cause of neurological deficit in low lumbar burst fractures may be the displacement of nerve roots through the vertical lamina fracture rather than from direct anterior compression from retropulsed bony fragments [2, 4]. The neurological status of the patient in burst fractures with greenstick lamina fractures depends on the degree of compression of nerve roots and on which nerve roots were entrapped.
It is not always possible to predict by preoperative investigation methods whether a patient without neurological deficit, but with a greenstick lamina fracture, has dural tear and/or entrapment of nerve roots [7, 13, 15]. Myelography does not add significant information, and because of the positioning of the patient, it may be harmful [3, 13]. In CT and MRI posterior fat pad signals disappeared in axial views when there was a greenstick lamina fracture and nerve root entrapment.
In the series of Cammisa et al. [5], 36% and in the series of Miller et al. [14], 44% of patients who had a dural tear did have entrapment of nerve roots, and Cammisa et al. [5] observed neurological deficit in all of the patients with dural tear. One of our patients with a greenstick lamina fracture was neurologically intact before surgery, but operation revealed dural tear and nerve root entrapment. Denis and Burkus [8] described a case of an L4 burst fracture with a greenstick lamina fracture and observed immediate postoperative neurological deterioration, which they attributed to the anterior approach being performed first, which possibly entrapped the nerve roots. This occurred in one of our patients where the greenstick lamina fracture was ignored despite using the posterior approach.
Karaikovic et al. [11] used Kaneda instrumentation even in cases with minor lamina fractures, and in a series of 110 anterior approach cases they did not observe any neurological deterioration after surgery. They did not report any dural tear or nerve root entrapment, although they included minor midline lamina fractures (greenstick lamina fractures), which is contrary to findings in the literature. They reported 15.5% unchanged motor function and in 33.3% of their patients bladder function did not recover. If anterior decompression were performed first in the treatment of burst fractures with greenstick lamina fractures and if dural tear and nerve root entrapment were also present, neurological status would not improve or might even deteriorate, which indicates improper surgical planning.
A fall from a height is the major aetiology of the greenstick lamina fracture with or without dural tear and nerve root entrapment. A treatment algorithm is very important for burst fractures with a greenstick lamina fracture. The absence of neurological deficit does not exclude either dural tear or nerve root entrapment. During surgery the greenstick lamina fracture cannot be consistently exposed by inspecting the dorsal surface of the lamina alone. There is no cerebrospinal fluid leakage because the lamina fracture is often of the greenstick type. We believe that the anatomical findings we observed during the operations should be taken seriously because these may be signs of dural tear and nerve root entrapment. More studies are needed to confirm this.
Any reduction manoeuvre will close the greenstick lamina fracture and crush the entrapped neural elements. Therefore, it is important to evaluate whether there is any neural entrapment. We found that there is an association between the occurrence of dural tear and the separation of fragments (mean, 4.35 mm). This finding may alert the surgeon if he or she observes a greenstick fracture with wide separation. We could not find any specific absolute clinical or radiological (plain radiograph, CT, or MRI) indicators that would make it clear whether there is a dural tear and neural entrapment with greenstick lamina fractures before surgery. Therefore, if there is any suspicion of a lamina fracture, it should be the rule to begin with the posterior approach and use the open book technique to expose the dura safely. Entrapped neural elements can be successfully extracted from the greenstick lamina fracture by an open book laminoplasty of the posterior neural arch.
Lumbar burst fractures with greenstick lamina fractures occur mostly in the L2–L4 area. In the surgical treatment, any reduction manoeuvre will close the greenstick lamina fracture and crush the entrapped neural elements. Therefore, it may be better to explore the greenstick lamina fracture whether there is any neural entrapment or not, before any reduction manoeuvre is performed.
References
- 1.Andreychik DA, Alander DH, Senica KM (1996) Burst fractures of the second through fifth lumbar vertebrae. J Bone Joint Surg Am 78:1156–1166 [DOI] [PubMed]
- 2.Aydinli U, Karaeminogullari O, Ozerdemoglu RA, Ozturk C (2001) Dural tears in lumbar burst fractures with greenstick lamina fractures. Spine 26:E410–E415 [DOI] [PubMed]
- 3.Brant-Zawadzki M, Jeffrey RB, Minagi H (1982) High resolution CT of thoracolumbar fractures. AJR Am J Roentgenol 138:699–704 [DOI] [PubMed]
- 4.Bridwell KH (1993) Low lumbar (L3-L4-L5) burst fractures. In: Floman Y, Farcy JPC, Argenson C (eds) Thoracolumbar spine fracture. Raven, New York, pp 223–234
- 5.Cammisa FP, Eismont FJ, Green BA (1989) Dural laceration occurring with burst fractures and associated laminar fractures. J Bone Joint Surg Am 71:1044–1052 [PubMed]
- 6.Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 8:817–831 [DOI] [PubMed]
- 7.Denis F (1984) Spinal instability as defined by the three column spinal concept in acute spinal trauma. Clin Orthop 189:65–76 [PubMed]
- 8.Denis F, Burkus JK (1991) Diagnosis and treatment of cauda equina entrapment in the vertical lamina fracture of lumbar burst fractures. Spine 16 [Suppl 8]:433–439 [PubMed]
- 9.Eismont FJ, Wiesel SW, Rothman RH (1981) Treatment of dural tears associated with spinal surgery. J Bone Joint Surg Am 63:1132–1136 [PubMed]
- 10.Eismont FJ, Green BA (1984) Surgical treatment of spinal injuries: anterior vs. posterior approaches. Adv Orthop Surg 1:24–34
- 11.Karaikovic EE, Kaneda K, Akbarnia BA (1997) Kaneda instrumentation for spinal fractures. In: Bridwell KH, DeWald RL (eds) The textbook of spinal surgery. Lippincott-Raven, Philadelphia, pp 1899–1924
- 12.Keene JS, Fischer SP, Drummond DS (1985) The neurological consequences of post traumatic impingement. Presented at the 52nd Annual Meeting of American Academy of Orthopaedic Surgeons, Las Vegas, Nevada
- 13.McAfee PC, Yuan HA, Frederickson BE (1983) The value of computed tomography in thoracolumbar fractures. J Bone Joint Surg Am 65:461–479 [PubMed]
- 14.Miller CA, Dewey RC, Hunt WE (1980) Impaction fracture of the lumbar vertebra with dural tear. J Neurosurg 53:765–771 [DOI] [PubMed]
- 15.Pau A, Silvestro C, Carta F (1994) Can the lacerations of the thoracolumbar dura be predicted on the basis of radiological patterns of the spinal fractures? Acta Neurochir 129:186–187 [DOI] [PubMed]
- 16.Pickett J, Blumenkopf B (1989) Dural lacerations and thoracolumbar fractures. J Spinal Disord 2:99–103 [DOI] [PubMed]
- 17.Silvestro C, Francaviglia N, Bragazzi R (1991) On the predictive value of radiological signs for the presence of dural laceration related to fractures of the lower thoracic or lumbar spine. J Spinal Disord 1:49–53 [PubMed]
- 18.Trafton PG (1984) Computed tomography of thoracic and lumbar spine injuries. J Trauma 24:506–515 [DOI] [PubMed]