Abstract
We present the method for management of syndactyly based on guided gradual and coordinated separation of finger phalanges and metacarpal bones by means of an original external fixator in order to grow soft tissue stock in the interdigital web spaces for their subsequent Z-plasty. Unlike traditional methods of treatment, the interdigital soft tissue bulk is grown by distraction only at the expense of local tissues. Cutaneofascial grafting is avoided as it damages the donor site and causes ugly scarring.
Résumé
Nous présentons la méthode de traitement des syndactilies en utilisant la séparation osseuse des doigts et des méta par un fixateur externe original qui permet d’augmenter le stock tissulaire des tissus mous. Cette technique augmente le capital tissulaire ce qui permet d’exclure les lambeaux du traitement et donc les séquelles des sites donneurs.
Introduction
The hand fulfils static, dynamic and sensory functions, and its diseases considerably impair professional abilities and the social life of an individual. The literature reports the incidence of syndactyly as 1 case per 2,000–3,000 newborn babies [6, 8]. Syndactyly is present in half of the upper-limb congenital anomalies. Bilateral symmetrical involvement is noted in 41% of cases [1, 2, 7]; hereditary cases occur quite often [6]. Syndactyly causes not only a cosmetic defect, but also joint contractures, as the skin binds the phalanges with the joints that are located at different levels, and are frequently malpositioned. The older the age when syndactyly is treated, the more marked and consistent the hand dysfunction, and the longer the rehabilitation time.
Conventional operative treatment of hand syndactyly is performed mainly by various types of free skin plasty. Its drawbacks are trophic disorders in the transferred skin flap and trauma to the donor site.
The external fixator for growing soft tissue bulk was first used in 1978 [3]. It included the wires inserted in the sagittal plane that put the integrity of the flexor or extensor tendons at risk. The device was big both in size and weight. The surgeons of the Russian Ilizarov Scientific Centre for Restorative Traumatology and Orthopaedics started to use external fixators that provided skin distraction for syndactyly management in 1979, and in 1984 Gavriil Ilizarov, its director at that time, proposed a special fixator for treating hand pathology. The assemblies of the Ilizarov fixator were versatile, included practically all known distraction systems, and enabled the insertion of wires in the frontal plane. It caused less damage to the tissues, but the insertion itself was technically difficult. The fixator was also large and heavy, so it could not be used in very young patients [4, 5]. With the great variety of assemblies available, there are no clear guidelines yet for their usage aimed at not only a good cosmetic outcome, but also at a best possible functional result.
The authors took on the task of finding a solution for the treatment of syndactyly with an external fixator design which could avoid the mentioned drawbacks and allow its use in very young patients.
Materials and methods
In 1999, we developed and introduced into clinical practice a novel external fixator design for management of hand pathology. Each of the supports of this fixator is a threaded rod to which the wires inserted into the hand bones are attached by slotted washers and nuts. These supports can be moved apart with two or four other threaded rods. Corkscrew-like bent wires are used that can only minimally traumatise the soft tissues. Unlike other known fixators for the hand with the wires inserted in the sagittal or frontal planes, the wires of our fixator are inserted at 45°. It is known that the functional ability of the hand is mainly its ability to produce different types of gripping and pinching where the thumb plays the most important role. To improve hand function, it is essential to create the first interdigital web space. If it exists, then the second web space is created, and the sequence can be continued. The fixator with two supports is used in cases of syndactyly in one or two neighbouring web spaces. If three neighbouring web spaces are involved, three supports are used in the assembly followed by the assembly with two supports (Fig. 1). Four affected web spaces require two assemblies, each consisting of three supports.
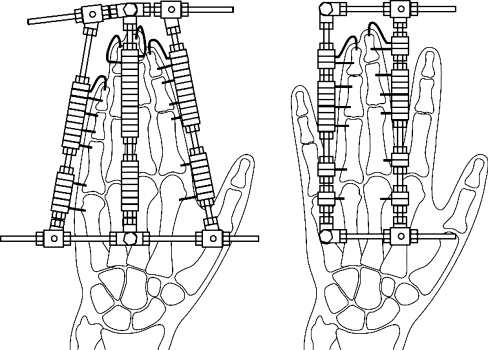
Fig. 1.
Diagrams of the fixator consisting of three and two supports for skin growth in three webspaces
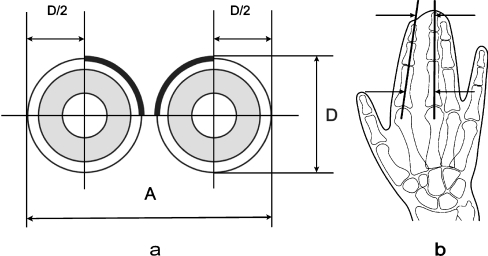
In order to obtain the required skin stock for one web space plasty, we make calculations according to the formula: A = D(π/2 + 1). The transverse distance between the opposite edges of the accreted fingers (A) are two quarters of the circumferential length of the skin that fully covers the finger after Z-plasty and two halves of the diameter before treatment. This diameter (D) is the dorso-volar thickness of the accreted fingers at their base and ends. (Fig. 2a).
| D | Dorso-volar thickness of the accreted fingers |
| A | Required transverse distance obtained by distraction between the opposite sides of fingers |
| π | Equal to 3.14 |
Fig. 2.
(a, b) Diagrams explaining calculations for obtaining required skin coverage
A more complex calculation is used for skin growth in syndactyly of several neighbouring interdigital web spaces when it is impossible to define the distance between the opposite edges of accreted fingers. AP hand radiographs are used to draw the lines along the finger phalanges (Fig. 2b). The distance between these lines at the bottom and at the level of the distal syndactyly rim is calculated according to the following formula: A = πD/2;
| D | Dorso-volar thickness of accreted fingers at the level of the bottom of an interdigital space and the distal end of syndactyly |
| A | Required transverse distance obtained by distraction between the middle lines of the finger phalanges at two levels measured in the radiograph |
| π | Equal to 3.14 |
The depth of interdigital spaces for normal function and good cosmetic appearance should correspond to the norm; in other words, the bottom should be located approximately at the level between the proximal and middle part of the basic phalanx of the second, third, fourth and fifth digits. The bottom of the first web space should be located at the level of the base of the proximal phalanx of the thumb or at the middle of the second metacarpal bone. Skin plasty in the second, third and fourth web spaces is done through the incisions providing the optimal anatomical and functional outcomes. The beginning of two incisions should be at the base of web spaces. The change in the distance between the incisions allows us to change the width of the web space base. We believe that this distance should be equal to the planned diameter of the base of one of the fingers between which this web space sits.
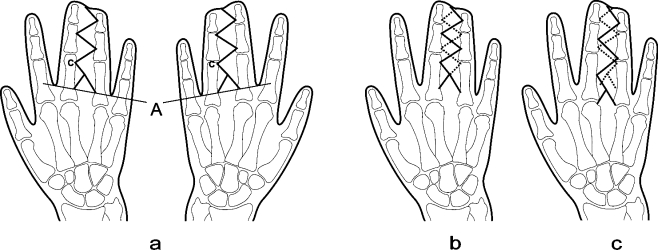
The point of connection of these two incisions should be located distally at the distance equal to the thickness of the palm at the site of the web space base. The apices C should face the same direction if the hand is turned to the dorsal or volar sides. The number of apices and cutting lines should be the same on the dorsal and volar sides (Fig. 3a,b). However, this skin-plasty variant does not achieve the cosmetic reconstruction of interdigital folds to the normal appearance as it forms a rectangular shape instead of the almost triangular shape characteristic of the normal hand. Therefore, recently we have used an improved variant of cutting the skin (Fig. 3c).
Fig. 3.
(a–c) Diagrams of skin plasty techniques
Results
Forty patients with different types of syndactyly were treated using this fixator.
The technique for the management of syndactyly that was described above provided positive outcomes in all cases: interdigital web spaces were created, desmogenic contractures of finger joints were eliminated, hand function and cosmetic appearance were improved. Recurrences due to scars were not observed in either the short- or long-term follow-ups.
The outcomes of all 40 patients were evaluated. Eight cases (20%) were assessed as excellent with complete restoration of cosmetic appearance and function. Twenty-four patients (60%) had good results with complete restoration of cosmetic appearance and partial limitation of hand function due to contractures in the interphalangeal joints. Satisfactory outcomes due to contractures in the interphalangeal joints and insufficient quality of cosmetic appearance (narrow base of the interdigital web space caused by limited skin stock for plasty) were obtained in eight cases (20%). There were no poor outcomes or failed treatment due to infection and untimely removal of the fixator (0%). We present the treatment outcomes of two clinical cases (Figs. 4, 5).
Fig. 4.
Congenital syndactyly of the third webspaces in the left hand in a 1-year-old patient. Skin plasty in the third interdigital space was performed after osteotomy in the syndesmosis of the distal phalanges, 55 days of distraction and 25 days of fixation
Fig. 5.
Congenital syndactyly of the third web spaces, cosmetic defect and functional disorder in a 12-year-old patient who had the fixator placed on the third and fourth digits, distraction during 20 days and fixation during 25 days followed by skin plasty in the third web space
Discussion
To our knowledge, external fixation for growing skin to manage syndactyly is a rare practice. Few references have been found in the available databases [3–7]. The external fixator for treatment of syndactyly proposed by us provides sufficient rigidity, despite the fact that it is small in size and weight. This external fixator creates optimal conditions for soft tissue regeneration due to a low degree of trauma, preserved blood supply and innervation when a proper rate of distraction is used for growing the skin. The technique of its usage is minimally-traumatic and universal. The hand functions and cosmetic appearance improve considerably after treatment. The period of treatment can be notably reduced as very young patients are treated when their hand is small and less soft tissue stock is required for plastic surgery. It means that distraction and fixation take less time. Moreover, the joint motion is limited for a shorter period, so the risk of developing contractures or infection is lower. Rehabilitation is faster as well.
The technique is being constantly perfected. It has been proposed to insert a wire in the nail plate to prevent its displacement into the web space. In cases of rough scars, osseous involvement or osteoporosis, additional paraosseous wires are used to avoid cutting out of the wire or for preservation of joints. In order to decrease trauma in cases of basal syndactyly, we use obliquely inserted cantilever wires. These wires are also helpful in other types of syndactyly.
It should be noted that the cosmetic appearance of the hand depends greatly on the proper performance of the technique, whereas functional results are influenced by the condition of the joints before treatment as partial contractures of the joints still remain after a desmogenic contracture has been eliminated.
The fixator described features minimal size, weight and considerable rigidity and a universal application technique which can be successfully applied for syndactyly in toes and without hindering ambulation.
References
- 1.Benua NI (1964) Assessment of combined skin plasty in operative treatment of congenital syndactyly. In: Prophylaxis of traumatism, treatment of injuries and their consequences. Materials of scientific conference. Gorki, pp 140–142
- 2.Godunova GS (1971) Age indications to operative treatment of different types of hand syndactyly. In: Outpatient assistance to children with orthopaedic diseases. Collected scientific papers. Leningrad, pp 67–74
- 3.Gudushauri ON, Tvaliashvili LA (1983) Distraction method of preparing for skin plasty in syndactyly. Ortop Travmatol Protez 11:25–27 [PubMed]
- 4.Gudushauri ON, Tvaliashvili LA (1991) Local epidermoplasty for syndactyly. Int Orthop 15(1):39–43 [DOI] [PubMed]
- 5.Ilizarov GA (1990) Syndactyly In: Transosseous osteosynthsis. Springer, Berlin Heidelberg New York, pp 658–668
- 6.Nettov GG, Lerner PI (1991) Management of congenital syndactyly of the hand with distraction method. In: Current issues of Ilizarov transosseous osteosynthesis. Kazan, pp 115–116
- 7.Volkova AM (1993) Surgery of hand diseases. In: Hand surgery. Uralski rabochiy. Ekaterinburg, pp 256
- 8.Yerofeeva GI, Goryuniv OF (1986) Long-term outcomes of operative treatment of syndactyly. In: Current methods for treating children with diseases and injuries of the locomotor system. Yaroslavl, pp 50–51