Abstract
Computed tomography image-guided surgery (CTGS) clearly improves the accuracy of pedicle screw insertion. Recent reports claim that a fluoroscopy-guided system (FGS) offered high accuracy and easy application. However, the superiority of either technique remains unclear in clinical application. This study compares the accuracy of pedicle screws installed using CTGS with that of screws installed using FGS. Seventy-four screws inserted using FGS in 13 patients and 76 screws inserted using CTGS in 11 patients were compared. The study population included ten cases of vertebral fracture, five cases of degenerative spondylolisthesis, three cases of spondylolytic spondylolisthesis, two cases of tuberculous spondylitis, two cases of failed earlier back surgery and two case of ankylosing spondylitis with pseudarthrosis. The installed vertebral levels ranged from T8 to S1. Screw positions were assessed with postoperative radiographs and computed tomography. Sixty-nine (93.2%) screws were correctly placed in the FGS group, and seventy-three (96.1%) screws were correctly placed in the CTGS group (P = 0.491). The results indicated that both image-guided systems offer high accuracy. However, the fluoroscope image-guided system could be considered the primary tool for lower thoracic and lumbosacral pedicle placement because it enables real-time navigation and does not require a preoperative CT scan.
Résumé
La chirurgie assistée par imagerie (CTGS) permet d’avoir une meilleure sécurité lors de l’implantation de vis pediculaires. Des articles récents montrent que le système avec amplificateur de brillance (fluoroscopie FGS) permet également cette implantation. Cependant, la supériorité d’une technique ou d’une autre n’apparaît pas clairement. Le but de cette étude est de comparer la bonne implantation des vis pediculaires en utilisant les deux systèmes. 74 vis ont été insérées avec le système FGS chez 13 patients et 66 vis avec le système CTGS chez 11 patients. Ces deux séries ont été comparées. Cette étude inclut 10 cas de fractures vertébrales, 5 cas de spondylolisthésis dégénératifs, 3 cas de spondylolisthésis avec spondylolyse, à 2 cas d’atteintes tuberculeuses, 2 cas d’échec de chirurgie par voie postérieure et 2 cas de spondylarthrite ankylosante avec pseudarthrose. Les niveaux d’instrumentation se sont échelonnés de T8 à S1. 69 (93.2%) vis ont été correctement mises en place dans le groupe FGS et, 73 (96.1%) avec le groupe CTGS (P = 0.491). Les résultats montrent que le système d’images guidées CTGS offre beaucoup plus de sécurité dans l’implantation des vis tant au niveau lombaire qu’au niveau thoracique ou lombosacré ceci ne nécessite pas par ailleurs un scanner pré opératoire.
Introduction
Although the clinical and biomechanical benefits of pedicle screws have been well documented, accurate placement remains a concern for spine surgeons. Traditionally, pedicle screws are inserted blindly and guided by tactile feel using a pedicle probe. High malposition rates have been reported for pedicle screws, reaching up to 40%, with associated increased risk of injury to the spinal cord, nerve roots and blood vessels [4, 6, 13]. Furthermore, screw insertion is more challenging in spines with obscured posterior anatomical landmarks, such as deformity, inflammatory spondyloarthropathy or previous spinal surgery.
The computer-assisted computed tomography image-guided system (CTGS) is clinically proven to increase accuracy of pedicle screw insertion and reduce radiation exposure during surgery [1, 8, 9, 15, 17]. This technique offers the advantages of three-dimensional (3D) images of the spine, which can reveal structures beneath the surface and also provides a real-time image-interactive means of navigation for pedicle screw insertion. However, this technique has not been widely adopted because of its steep learning curve, its high cost and the additional radiation exposure to the patient from pre-operative computed tomography (CT). The results of our previous investigation demonstrated that the CT-free fluoroscopy-guided system (FGS) offers highly accurate pedicle screw insertion in lower thoracic and lumbosacral levels, potentially eliminating the above disadvantages [7]. However, the superiority between these two techniques in clinical application remains uncertain although a few cadaver studies have been conducted [2, 10].
Therefore, the accuracy of the computer-assisted CT image-guided system for pedicle screw placement was compared with that of a CT-free fluoroscopy-guided system. We sought to determine whether FGS could be considered the first line image guided tool for lower thoracic and lumbosacral pedicle placement.
Materials and methods
Twenty-eight patients who had received computer-assisted CT image-guided or fluoroscopy-guided pedicle screw insertions were retrospectively reviewed. Only those patients who had undergone pedicle screw insertion below the T8 level were selected in this study. The inclusion criteria were chosen because of the difficulty obtaining good quality fluoroscopic images of the upper thoracic spine for fluoroscopic navigation. Therefore, 24 consecutive adult patients (15 female, nine males) were enrolled in the study group. The mean patient age was 50.2 years (range 19–79 years). Medical charts were reviewed and diagnosis, surgical procedures and postoperative complications were recorded. The indications for surgery included ten cases of vertebral fracture, five cases of degenerative spondylolisthesis, three cases of spondylolytic spondylolisthesis, two cases of tuberculous spondylitis, two cases of failed earlier back surgery and two case of ankylosing spondylitis with pseudarthrosis.
Optoelectronic navigator (Vector Vision, Brain LAB GmbH, Germany) was used for pedicle screw insertion in all patients. Thirteen procedures were assisted by the VectorVision2 Fluoro fluoroscopy-guided system, and eleven were assisted by CT-based image-guided technology. Typically, 5.5-mm diameter titanium screws were used for the lower thoracic vertebra, and 6.5-mm diameter screws were used for the lumbar vertebra.
Fluoroscopy-navigation TPS insertion
Pedicle screw insertion was assisted by the VectorVision2 Fluoro fluoroscopy-guided system. The VectorVision2 Fluoro consists of a fixation ring, an X-ray cone, dynamic reference clamps, reflective marker spheres for use with surgical instruments and the VectorVision2 central workstation with a computer and monitor. Surgery was performed with each patient in a prone position. The relevant segments were surgically exposed according to conventional methods. The pedicle screws were then inserted into the relevant vertebra via computer-assisted fluoroscopic navigation described previously [7].
CT-based image-guided TPS insertion
All eleven patients received preoperative spiral mode CT scans (Siemens, Forchheim, Germany) of the spinal segment to be instrumented with a slice thickness of 2.0 mm, an interval of 2.0 mm, and a pitch of 3.0°. Image data were obtained and transferred via the network from the CT scanner to the navigation computer to produce a three-dimensional (3D) image of the relevant spinal segment.
With the patient in a prone position, the relevant segments were surgically exposed in the conventional manner. A dynamic reference clamp fitted with three infrared diodes was attached securely to the spinal process of the vertebra to be instrumented. Registration was completed via surface matching procedures. Eight to twenty nonidentified points on the dorsal surface of the vertebra of interest were used for registration. Infrared cameras and the workstation space digitiser identified the diodes on the pointer and automatically completed registration. Any registration errors were then displayed on the workstation monitor. Navigation was continued when the registration procedure was acceptable (inaccuracy below 1.9). Single registration was preferred for navigation of one vertebral segment (two vertebra, four screws) since it is faster than separate registration. Surgical instruments such as pedicle awl, probe and screwdriver were tracked using an adapter with infrared diodes. The relative positions of these instruments and their trajectory lines were then simultaneously displayed on the CT images in real-time mode.
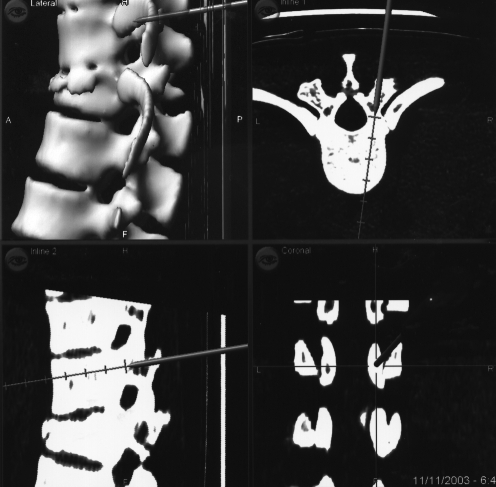
Following completion of matching procedures, the surgeon located the entry point of the pedicle screw using the registered pointer. After locating the entry point, the monitor displayed the trajectory line on the axial, sagittal and coronal images through the localised point (Fig. 1). By subtly moving the pointer, the best entry point and alignment for screw insertion could be determined. The screw channel was prepared using a registered pedicle probe guided by the real-time trajectory line. The walls of the screw channel were checked for perforation with a flexible sounding-probe. A pedicle screw of sufficient length and diameter was also inserted under the real-time guiding trajectory.
Fig. 1.
Computed tomography assisted spinal navigation begins by using the registration pointer to touch the planned entry point. The monitor on the workstation displays the location and trajectory line on the axial, sagittal, and coronal images through the localised point in real time
Assessment of pedicle screws
The final pedicle screw positions were evaluated on antero-posterior and lateral plain radiographs. A postoperative thin-cut CT scan (2 mm contiguous non-overlapping images) of the instrumented vertebra was obtained. Transverse and sagittal sections were generated to assess the screw position in all planes of the pedicle shaft. Moreover, the distance between the edge of the screw and the pedicle wall was measured. The location and degree of pedicle wall violation was assessed using a modified grading system for wall violation [17]. Screws violating the cortex without extending beyond the cortical margin were defined as grade I. A grade II violation was defined as a screw extending less than 2 mm beyond the cortex. Furthermore, screws extending more than 2 mm beyond the cortex were considered grade III violations. Grade II and III screws were considered to represent true cortical violations.
Statistical analysis
The final accuracy of the pedicle screw position of the two study groups was assessed. Differences in accuracy between the two groups were statistically analysed using two-tailed Fischer exact test. Statistical analyses were performed using the SPSS computer software package (Version 12.0, Chicago, IL, USA). The level of statistical significance was set at a p-value of less than 0.05.
Results
Table 1 lists the results of the postoperative plane radiograph and CT imaging evaluation of the pedicle screw positions. The installed vertebral levels ranged from T9 to S1 in the FGS group and from T8 to S1 in the CTGS group. Seventy-four pedicle screws were installed in the 13 patients with FGS, and 76 were installed in the 11 patients with CTGS.
Table 1.
Screw placement outcomes distributed among groups
| FGS | CTGS | |
|---|---|---|
| Total no. of patients | 13 | 11 |
| Total no. of screws inserted | 74 | 76 |
| Total no. of screws categorised as good | 69 (93.2%) | 73 (96.1%) |
| Total no. of screws categorised as error | 5 (6.8%) | 3 (3.9%) |
Percentages are given relative to the total number of screws in a particular group. The difference in screw placement between the two groups was not statistically significant using the Fisher’s exact test (P = 0.491).
FGS fluoroscopy-guided system, CTGS computed tomography image-guided system
In the FGS group, 69 (93.2%) pedicle screw placements were fully contained within the cortical boundaries of the installed pedicles and were categorised as accurate. In the CTGS group, 73 (96.1%) screws were considered accurately installed. The total numbers of screw positions categorised as accurate and inaccurate (grade II and III pedicle wall violation) between the two groups were analysed using two-tailed Fischer exact test. The data revealed no statistical difference (P = 0.491). In the thoracic spine, no pedicle violations occurred after FGS whereas one (2.7%) violation occurred after CTGS. Furthermore, five (9.3%) pedicle violations occurred in the lumbosacral spine when using FGS in comparison to two (5.3%) violations when using CTGS. Subgroup analysis revealed no statistical difference (P = 0.695).
Five screws exhibited true cortical violation in the FGS group, including three grade II and two grade III screws. All five violations occurred in earlier cases and the most common trajectory was towards the medial pedicle wall. Four violations were located in the medial cortex, and one was located in the lateral pedicle cortex. No superior or inferior pedicle wall violations were observed. No postoperative complications such as infection, neurological deficit or vascular injury occurred. In the CTGS group, four screws demonstrated true cortical violation, involving three grade II screws and one grade III screw. The trajectory of all four of these violations was towards the lateral pedicle wall. No superior or inferior pedicle wall violations were observed. Furthermore, the subjects revealed no postoperative neurological deficits or vascular injuries other than one deep wound infection that was resolved after debridement and implant removal. Table 2 lists the trajectory and severity of pedicle wall violations in the involved vertebral levels.
Table 2.
Review of the side and level of cortical violations
| Method/Case | Side/level | Direction | Grade |
|---|---|---|---|
| FGS/1 | Right/L3 | Lateral | III |
| FGS/2 | Left/L4 | Medial | II |
| FGS/2 | Left/L5 | Medial | II |
| FGS/4 | Left/L4 | Medial | III |
| FGS/5 | Right/L5 | Medial | II |
| CTGS/6 | Right/L1 | Lateral | III |
| CTGS/7 | Left/L3 | Lateral | II |
| CTGS/11 | Right/T11 | Lateral | II |
FGS fluoroscopy-guided system, CTGS computed tomography image-guided system
Discussion
Pedicle screw instrumentation is a technically demanding procedure. Although most well-trained spinal surgeons generally do not require image-guidance systems, the procedure is extremely challenging for inexperienced surgeons or in spines with obscured posterior anatomical landmarks, such as cases of inflammatory spondyloarthropathy, deformity, and previous spinal surgery. These results indicate that pedicle screws can be inserted successfully and safely with the aid of computer-assisted navigation in relatively simple as well as technically challenging cases. Because it offers the same accuracy as CTGS and does not require preoperative CT scan images, FGS should be considered the first line image guided tool for lower thoracic and lumbosacral pedicle screw placement.
The accuracy of pedicle screw placement in the thoracolumbosacral spine using image-guided methods and the superiority of the CTGS over the FGS has been reported in a previous cadaver study [2]. The results of the current clinical study revealed no significant difference in accuracy between the two methods. This phenomenon may result from the vertebral levels selected for instrumentation. In the FGS group, the inserted vertebra were limited to the lower thoracic and lumbosacral spine. In clinical practice, the quality of pre-acquired fluoroscopic images is extremely important during computer-assisted fluoroscopic navigation. Obtaining satisfactory fluoroscopic images of the upper thoracic spine is difficult because the vertebral and pedicle cortical margins are obscured by the shadows of the shoulder, scapula and ribs. Therefore, it remains uncertain whether accuracy would be impacted if FGS were applied in the higher thoracic levels. This uncertainty is one of the limitations of the fluoroscopy-guided technique.
In the thoracic spine, pedicle screw insertion via the tactile manual method still carries a significantly higher risk of pedicle wall violation [5, 16]. One study using postoperative CT scans to examine 279 pedicle screws placed at T1 to T12 revealed that up to 43% of the screws perforated the cortical margins [3]. Analysis of the 58 thoracic (T8 to T12) pedicle screws inserted by CTGS and FGS in the current study revealed that only one (1.7%) violated the pedicle wall. Our data demonstrates that computer-assisted surgery provides a high accuracy rate for lower thoracic pedicle screw insertion.
A previous study reported an 89.1% success rate for pedicle screw insertion with the assistance of lateral plain radiography in the T11 to L5 vertebral levels [12]. In fact, conventional fluoroscope assisted pedicle screw placement exposes the spine surgeon to significant radiation levels. Radiation dose rates are up to 10–12 times greater than other nonspinal musculoskeletal procedures that involve the use of a fluoroscope [14]. In our study, 69 (93.2%) pedicle screws were inserted successfully from the T9 to S1 vertebral levels using FGS. Although radiation dosages were not recorded in this study, we believe radiation exposure would be lower than in the conventional method since continual repositioning of the C-arm for repeat checking screw position is not required during surgery.
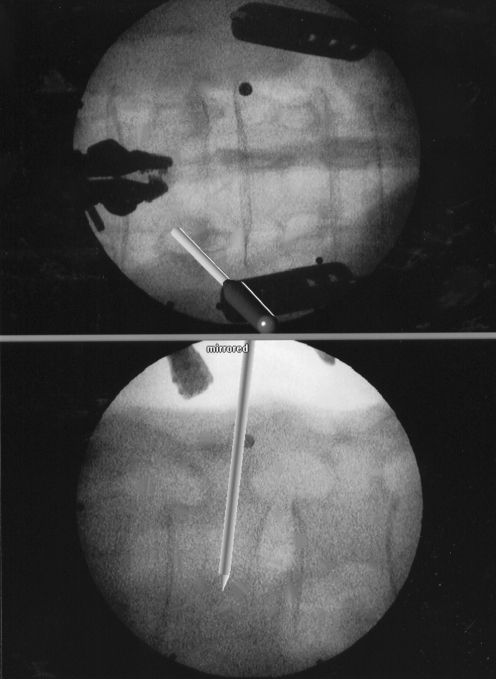
Although no pedicle wall violation on the sagittal plane resulted from the fluoroscopic image guided technique, five out of 74 screws still exhibited pedicle violations on the axial plane. These violations demonstrate the limitations of the fluoroscopy-guided system, which only provides real-time two-dimensional images of a complex three-dimensional spinal structure (Fig. 2). Axial plane information was lacking and likely led to perforation of the medial or the lateral pedicle wall as usually occurs in the conventional fluoroscope-guided procedures [4]. Multiple registered fluoroscopic images were suggested prior to screw placement to provide multi-directional control (pseudo-3D effect) during surgery [11]. After completing several cases, images were obtained in several different planes rather than relying only on antero-posterior and lateral images for navigation. As a result, there was no subsequent perforation of the pedicle wall in our series.
Fig. 2.
The virtual pointer trajectory lines superimposed on the pre-acquired fluoroscopic images. The fluoroscopy-guided system only provides real-time 2D images for navigation
Our data indicates that both image-guided systems are highly accurate for pedicle screw placement even in challenging cases. The two methods also revealed no statistical difference in results. Based on the results of this comparative study, the fluoroscope image-guided system should be considered the first line image guided tool for lower thoracic and lumbosacral pedicle placement because it offers the advantages of real-time navigation and simple application and does not require preoperative CT scan images.
References
- 1.Amiot LP, Lang K, Putzier M, Zippel H, Labelle H (2000) Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine 25:606–614 [DOI] [PubMed]
- 2.Austin MS, Vaccaro AR, Brislin B, Nachwalter R, Hilibrand AS, Albert TJ (2002) Image-guided spine surgery: a cadaver study comparing conventional open laminoforaminotomy and two image-guided techniques for pedicle screw placement in posterolateral fusion and nonfusion models. Spine 27:2503–2508 [DOI] [PubMed]
- 3.Belmont PJ Jr, Klemme WR, Dhawan A, Polly DW Jr (2001) In vivo accuracy of thoracic pedicle screws. Spine 26:2340–2346 [DOI] [PubMed]
- 4.Castro WHM, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S (1996) Accuracy of pedicle screw placement in lumbar vertebrae. Spine 21:1320–1324 [DOI] [PubMed]
- 5.Cinotti G, Gumina S, Ripani M, Postacchini F (1999) Pedicle instrumentation in the thoracic spine. Spine 24:114–119 [DOI] [PubMed]
- 6.Esses SI, Sachs BL, Dreyzin V (1993) Complications associated with the technique of pedicle screw fixation: a selected survey of ABS members. Spine 18:2231–2239 [DOI] [PubMed]
- 7.Fu TS, Chen LH, Wong CB, Lai PL, Tsai TT, Niu CC, Chen WJ (2004) Computer-assisted fluoroscopic navigation of pedicle screw insertion: an in vivo feasibility study. Acta Orthop Scand 75:730–735 [DOI] [PubMed]
- 8.Kothe R, Strauss JM, Deuretzbacher G, Hemmi T, Lorenzen M, Wiesner L (2001) Computer navigation of parapedicular screw fixation in the thoracic spine. Spine 26:E496–E501 [DOI] [PubMed]
- 9.Merloz P, Tonetti J, Pittet L, Coulomb M, Lavallee S, Sautot P (1998) Pedicle screw placement using image guided techniques. Clin Orthop 354:39–48 [DOI] [PubMed]
- 10.Mirza SK, Wiggins GC, Kuntz C, York JE, Bellabarba C, Knonodi MA, Chapman JR, Shaffrey CI (2003) Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance: a cadaver study. Spine 28:402–413 [DOI] [PubMed]
- 11.Nolte LP, Slomczykowski MA, Berlemann U, Strauss MJ, Hofstetter R, Schlenzka D, Laine T, Lund T (2000) A new approach to computer-aided spine surgery: fluoroscopy-based surgical navigation. Eur Spine J 9(suppl 1):78–88 [DOI] [PMC free article] [PubMed]
- 12.Odgers CJ IV, Vaccaro AR, Pollack ME, Cotler JM (1996) Accuracy of pedicle screw placement with the assistance of lateral plain radiography. J Spinal Disord 9:334–338 [DOI] [PubMed]
- 13.Pinto MR (1992) Complications of pedicle screw fixation. Spine 6:45–54
- 14.Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M (2000) Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine 25:2637–2645 [DOI] [PubMed]
- 15.Schwarzenbach O, Berlemann U, Jost B, Visarius H, Arm E, Langlotz F, Nolte LP, Ozdoba C (1997) Accuracy of computer-assisted pedicle screw placement. An in vivo computed tomography analysis. Spine 22:452–458 [DOI] [PubMed]
- 16.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS (1995) Placement of pedicle screws in the thoracic spine. J Bone Joint Surg [Am] 77:1200–1206 [DOI] [PubMed]
- 17.Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM (2001) Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery 48:771–779 [DOI] [PubMed]