Abstract
Although several surgical techniques for midclavicular fractures have been reported, Knowles pinning has rarely been compared with plating. The purpose of this study is to compare the clinical results of these two alternative techniques. There were 88 patients with midclavicular fractures surgically treated with either a Knowles pin or a plate. All patients were followed up for 12 months with a shoulder score evaluation. The Knowles pin group included 56 patients, with an average age of 40.1 years. The plate group included 32 patients, with an average age of 38.2 years. Both groups were similar in injury mechanism and fracture types (all p values>0.5). Plating has a significantly longer operation time, larger wound incision, higher pain level, more analgesic use, more complications and more symptomatic hardware (all p value<0.05). The shoulder score, union rate and healing time are not significantly different between the two groups (all p values>0.2). In conclusion, if the surgery of mid-third clavicular fractures is indicated, fixation with a Knowles pin has more advantages than plate fixation.
Résumé
Plusieurs techniques chirurgicales ont été rapportées pour traiter les fractures de la partie moyenne de la clavicule, l’embrochage étant rarement comparé avec l’ostéosynthèse par plaque. Le propos de cette étude est de comparer les résultats cliniques de ces deux techniques. 88 patients présentant une fracture du tiers moyen de la clavicule ont été traités chirurgicalement par broches de Knowles ou par ostéosynthèses par plaque. Tous les patients ont été suivis pendant une période d’un an avec évaluation clinique de l’épaule. Le groupe broche comportait 56 patients dont l’âge moyen était de 40,1 ans et le groupe des plaques, 32 patients dont l’âge moyen était de 38,2 ans. Les deux groupes avaient le même mécanisme de fracture et le même type de fracture. Les ostéosynthèse par plaques ont conduit un temps opératoire plus important, une incision plus grande et une douleur également plus importante avec utilisation d’un algésique et plus de complications. Par contre l’évaluation de l’épaule, quel que soit le groupe était la même quel que soit le groupe de traitement, plaque ou broche (0.26). En conclusion, l’embrochage par broches de Knowles est une technique plus avantageuse que la fixation par plaque dans les fractures du tiers moyen de la clavicule.
Introduction
Clavicular fractures are common injuries. It has been reported that fractures of the clavicle account for 5–10% of all fractures and 35–45% of all shoulder girdle injuries [22]. Only one fifth of all fractures of the clavicle are located outside the middle third [2]. Nonoperative treatment of an acute midclavicular fracture can usually be successful, owing to its rich vascularity and the inherent fragment stability. Although usually unnecessary for surgical treatment of an acute midclavicular fracture [7, 9, 19], general agreement exists on the indications for open reduction and internal fixation. Indications for operative treatment include: (1) painful nonunion; (2) multiple trauma; (3) open fracture (4) severe malposition and tenting the skin; (5) neurovascular injuries; and (6) persistent separation of the fracture with a gap of more than half of the diameter of the clavicle [4, 7–10, 17, 19].
A plate is commonly used for a clavicular fracture. However, more soft tissue dissection can result in nonunion [3]. Although attempts have been made to find less invasive techniques to minimise complications, most of these techniques are associated with either implant migration or unstable fixation [14, 15]. The purpose of this study was to evaluate Knowles pinning (a minimally invasive technique for the stable fixation of midclavicular fractures) and to compare the clinical outcomes and complications of the Knowles pinning with those of plating.
Materials and methods
Between 2002 and 2005, 115 consecutive patients with midclavicular fractures were operatively treated at our orthopaedic department. All patients who had associated injuries, such as head injuries, internal bleeding, haemo- or pneumo-thorax etc. (in 12 patients), that required intensive care or required other departments for treatment were excluded. The inclusive 103 patients who were treated either with a Knowles pin or a plate were distributed to five senior surgeons according to their assigned shifts. Three surgeons favoured a Knowles pin and the remaining two surgeons favoured a plate to treat a midclavicular fracture. Owing to our orthopaedic surgeons’ assigned shift according to the schedule, the patient distribution could be regarded as randomised.
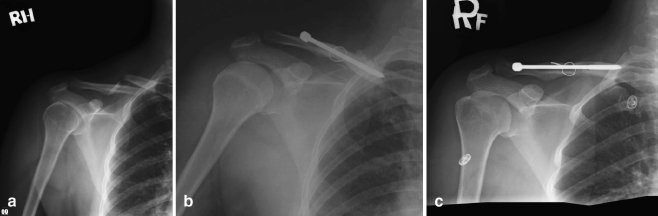
The Knowles pin technique has been described previously in [5]. In this study, a horizontal incision over the anterosuperior aspect of the clavicle was performed. A Knowles pin of 4 mm in diameter was retrogradely inserted through the posterolateral side to the anteromedial side of the clavicle. In comminuted fractures of more than 50%, fixation by cerclage wires or sutures were permitted in addition to the Knowles pin (Fig. 1a–c). The plate technique with a horizontal incision has been reported previously in [1, 21]. In our study, the types of plates used included dynamic compression, tubular and reconstruction plates.
Fig. 1.
A 45-year-old female patient with right midclavicular comminuted fracture that presented with severe displacement and tenting of the skin was treated with a Knowles pin and cerclage wire. a Preoperative shoulder anterior–posterior (AP) view showed a displaced and comminuted clavicle fracture. b Plain film at the immediate postoperative period showed good fracture reduction. c Radiography at 12 weeks postoperatively showed fracture healing without Knowles pin migration
Fifteen patients could not be followed up regularly owing to mortality (one case), co-morbid psychological disorders (two cases) or relocation (12 cases) and they were excluded. The mean age of the remaining 88 patients at the time of their operations was 39.4 years. There were 57 men (average 35.1 years of age) and 31 women (average 47.3 years of age). The indications for surgery included persistent separation of the fracture with a gap of more than half of the diameter of the clavicle (in 21 patients), severe displacement and tenting of the skin (in 20), associated fractures (in 14) (seven ribs, four scapulas, two upper extremities and one lower extremity), painful nonunions (in six), open fractures (in four) and intolerable pain and election to undergo surgery (in 23). The patients with intolerable pain were selected by the following criteria: after the figure-of-eight bandage and appropriate analgesics had been used for 72 h, the pain had not subsided and disturbed the clinical status (increased blood pressure or heart rate, insomnia, anxiety etc.). Bone grafts were used around the fracture sites of nine patients who had severe comminuted fractures or nonunion.
The Knowles pin group included 56 patients, whose mean age was 40.1 years. The plate group included 32 patients, whose mean age was 38.2 years. The injury mechanism, fracture patterns and demographics related to the groups are shown in Table 1. All patients received postoperative arm sling protection for 1 to 3 weeks after surgery and were told to avoid work with heavy loads or aggressive exercise using the involved extremities during the following two months.
Table 1.
Injury mechanism, fracture patterns and demographics
| Knowles pin (number of patients) | Plate (number of patients) | p value | |
|---|---|---|---|
| Injury mechanism | |||
| Simple fall | 2 | 1 | 1.0 |
| Fall from a great height | 2 | 2 | 0.62 |
| Vehicular trauma | 52 | 29 | 0.70 |
| Fracture patterns | |||
| Open fracture type I | 2 | 2 | 0.62 |
| Transverse fractures | 9 | 6 | 0.77 |
| Oblique and spiral fractures | 28 | 15 | 0.83 |
| Comminuted fractures | 13 | 7 | 1.0 |
| Symptomatic nonunion | 4 | 2 | 1.0 |
| Demographics | |||
| Gender (F/M) | 19/37 | 12/20 | 0.82 |
| Mean age (years) | 40.1 | 38.2 | 0.56 |
| Mean body weight (kg) | 72.2 | 69.3 | 0.59 |
| Average stature (cm) | 172.3 | 170.4 | 0.65 |
All patients were reviewed at one, two, three, four, six and 12 months after surgery. The roentgenograms were taken for all patients at each follow-up appointment for the evaluation of fracture healing and implant position. Radiographic healing was interpreted by the attending surgeon at each follow-up and was verified by all of the authors of the study. Radiographic healing was defined as evidence of bridging callus across the fracture sites or the obliteration of the fracture lines.
The operating time was measured from the beginning of surgery to skin closure. The analgesic type and amount was documented for the first three postoperative days. Postoperative pain was assessed starting from postoperative day one. The visual analogue pain scale (scale 1–10) was used. Twelve months postoperatively, we evaluated the results using the shoulder scoring system of Constant and Murley [6]. In this system, the subjective and objective clinical data are included, with the maximum score being 100 points. Pain (15 points), activities of daily living (20 points), range of motion of the shoulders (40 points) and muscle power (25 points) are evaluated.
Statistics
The Chi-square test with Yates’ correction and Student’s t-test were used to compare the two groups. The SPSS 10.0 statistical software package was used to analyse the data; p values below 0.05 were considered to be significant.
Results
Fifty-six of the original 66 (84.8%) patients treated with a Knowles pin and 32 of the original 37 (86.5%) patients treated with a plate had complete follow-up. The final follow-up rate was not significantly different (p = 1.0) between the groups. Both of the groups were similar in respect of injury mechanisms, fracture types, gender and age (all p values>0.5) (Table 1). In the Knowles pin group, all of the fractures (100%) healed in six months. In the plate group, 31 of the 32 fractures (96.9%) healed in six months. Differences in union rate and healing time between the two groups were not significant (all p values>0.2). In the Knowles pin group, the mean shoulder score on Constant and Murley’s system was 95.3 ± 4.1 points (range 80–100). In the plate group, the mean score was 93.1 ± 3.8 points (range 75–100). There was no difference in the shoulder score between the two groups (p = 0.84). However, the average incision length was significantly smaller (p < 0.001) in the Knowles pin group (4.1 ± 0.31 cm) compared to the plate group (8.4 ± 1.61 cm). The operative time was also significantly less in the Knowles pin group (p < 0.001) (Table 2).
Table 2.
Clinical results of the two groups
| Knowles pin (mean±SD) | Plate (mean±SD) | p value | |
|---|---|---|---|
| Union in six months | 56/56 | 31/32 | 0.36 |
| Healing time (days) | 84.8 ± 19.1 | 92.7 ± 21.5 | 0.26 |
| Shoulder score (points) | 95.3 ± 4.1 | 93.1 ± 3.8 | 0.84 |
| Wound incision (cm) | 4.1 ± 0.31 | 8.4 ± 1.61 | <0.001 |
| Operative time (min) | 27.5 ± 10.3 | 68.4 ± 19.6 | <0.001 |
SD=standard deviation
All patients were placed on the standard protocol at our institution for analgesia, which consisted of patient-controlled meperidine (pethidine), acetaminophen and nonsteroidal anti-inflammatory drugs (NSAID) (including tiaprofenic acid and ketoprofen). For the first three days, the total values for meperidine, NSAID and acetaminophen were recorded. The total amount of meperidine used was significantly less (p<0.001) in the Knowles pin group (mean 35.7 mg, range 0–200) compared to the plate group (mean 109.4 mg, range 0–450). Tiaprofenic acid use was 714.3 mg for the Knowles pin group (range 0–1,400) and 1,437.5 mg for the plate group (range 0–2,000) (p<0.001). Ketoprofen use was 34.8 mg for the Knowles pin group (range 0–150) and 93.8 mg for the plate group (range 0–250) (p<0.001). Total acetaminophen use averaged 892.9 mg for the Knowles pin group (range 0–2,500) and 1,546.9 mg for the plate group (range 0–4,000) (p<0.001) (Table 3).
Table 3.
Overall analgesic use in the first three postoperative days
| Knowles pin | Plate | p value | |
|---|---|---|---|
| Meperidine (mg) | 35.7/i.m. | 109.4/p.o. | <0.001 |
| Tiaprofenic acid (mg) | 714.3/p.o. | 1,437.5/p.o. | <0.001 |
| Ketoprofen (mg) | 34.8/i.m. | 93.8/i.m. | <0.001 |
| Acetaminophen (mg) | 892.9/p.o. | 1,546.9/p.o. | <0.001 |
i.m.=intramuscularly, p.o.=oral
The complication rate was lower in the Knowles pin group (0%) than in the plate group (9.4%) (p=0.045). The plate group had three complications: a wound infection, a nonunion and an implant failure. A three-day regimen of intravenous antibiotics resolved the infection and wound healing occurred uneventfully. The patient with symptomatic nonunion received a secondary operation with iliac bone graft seven months postoperatively. The remaining patient, who was treated using a one-third tubular plate, suffered plate breakage one month after the operation. He was treated by replating using a dynamic compression plate and supplemental autogenous bone graft.
Four of 56 (7.1%) patients treated with a Knowles pin and 12 of 32 (37.5%) patients treated with a plate complained of symptomatic hardware problems. Symptomatic hardware problems were less frequent in the Knowles pin group (p < 0.001).
The visual analogue pain scores did not significantly differ between the two groups on the first postoperative day (p = 0.31). However, patients in the Knowles pin group had lower pain scores on days 2 and 3 when compared to the plate group (p = 0.03 and p = 0.01, respectively).
In the Knowles pin group, 48 patients (85.7%) returned to their previous work three months postoperatively. Forty patients (71.4%) were able to return to preinjury levels of activity. In the plate group, all but three cases (90.6%) returned to their previous work three months postoperatively and 24 (75%) returned to preinjury levels of activity postoperatively. There was no difference in the rate of return to work and preinjury activity levels between the groups (p > 0.7).
Discussion
Clavicle fractures are among the most common skeletal injuries [11]. The most common mechanism of injuries in adults is direct trauma or indirect injury (a fall onto the outstretched hand) [2]. Approximately 70–80% of clavicle fractures involve the middle third [2, 24]. Fractures at this location are generally treated conservatively with particularly good results (bone healing and shoulder function restoration) [9, 19]. However, various problems of conservative treatment have been reported, including: (1) pain and instability during the first three weeks after injury [24]; (2) increased tightness of the figure-of-eight bandage, resulting in the phlebostasis of arm veins [20]; and (3) high nonunion rate in high-energy trauma and severe displacement [10, 23]. Therefore, a selective surgical treatment for midclavicular fracture is recommended [11, 18, 20]. In our study, 65 of 88 patients had well-known previously reported surgical indications. The remaining 23 patients (14 in the Knowles pin group, 9 in the plate group) had intolerable pain and asked for surgical treatment. Marked pain relief was noted in these patients postoperatively. All fractures healed in three months without any complications. The shoulder scores were high (mean 97.2 points) and all patients returned to their preinjury daily activities six months postoperatively. Therefore, we recommend that intolerable pain should be considered as a selective indication for surgical treatment.
The role of an intramedullary rod for clavicular fractures lies in the internal splinting of a fracture site. The healing process of an intramedullary rod for clavicular fractures, thus, involves external bridging callus through intramembranous bone formation [12]. Although the intramedullary fixation of clavicles with Rush pins, elastic titanium nails, Kirschner wires and Kuntscher nails have been reported [8, 11, 17, 18], these operative techniques have not been widely used because of migration of the intramedullary implants [14, 15]. In our study, we determine that Knowles pinning provides stable fixation and allows an early range of motion. The interfragmental compression effect and the resistance of migration are also superior to other intramedullary implants, since the partially threaded Knowles pins with a collar can exert an axial compression force at the fracture site. This could be why Knowles pinning had a high union rate (100%) and a low implant failure rate (0%).
Plate insertion generally causes more extensive damage of the periosteum and the surrounding soft tissues than the insertion of an intramedullary rod. Poor nutrition supply impedes the fracture healing process [4, 13, 16]. Moreover, a plate may frequently require removal because of its gross prominence over skin when inserted on the superior clavicular surface. Despite good results for some series, a high complication rate has still been reported with plating for mid-third clavicular fractures. The usual complications of plating include wound infection, plate loosening, plate angulation, plate breakage, nonunion and refracture after plate removal [3]. Poigenfurst et al. [21] reported four plate breakages before union and four refractures after plate removal among 102 patients. Their total complication rate was 20%. Schwarz and Hocker [25] reported that the failure rate of plating among 36 patients was 12%. In our study, the complication rate of plating was 9.4% and for Knowles pinning, it was 0%.
Presently, Knowles pinning can offer several advantages. A shorter operation time may decrease the risk from anaesthesia. Smaller wound incision and less soft tissue dissection may reduce the postoperative pain level. In general, total analgesic use in the first three postoperative days was less in the Knowles pin group. Decreased drug use and costs may make the technique beneficial to both the patient and the hospital.
In conclusion, the fixation of midclavicular fractures by Knowles pins is a safe and simple technique. We have demonstrated that this technique is another option that can provide good results.
References
- 1.Ali Khan MA, Lucas HK (1978) Plating of fractures of the middle third of the clavicle. Injury 9(4):263–267 [DOI] [PubMed]
- 2.Bigliani LU, Craig EV, Butters KP (1991) Fractures of the shoulder. In: Rockwood CA Jr, Green DP, Bucholz RW (eds) Rockwood and Green’s fractures in adults, 3rd edn. Lippincott-Raven, Philadelphia, Pennsylvania, pp 871–1019
- 3.Bostman O, Manninen M, Pihlajamaki H (1997) Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma 43(5):778–783 [DOI] [PubMed]
- 4.Bradbury N, Hutchinson J, Hahn D, Colton CL (1996) Clavicular nonunion. 31/32 healed after plate fixation and bone grafting. Acta Orthop Scand 67(4):367–370 [DOI] [PubMed]
- 5.Chu CM, Wang SJ, Lin LC (2002) Fixation of mid-third clavicular fractures with Knowles pins: 78 patients followed for 2–7 years. Acta Orthop Scand 73(2):134–139 [DOI] [PubMed]
- 6.Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164 [PubMed]
- 7.Crenshaw AH Jr (2003) Fractures of shoulder, arm, and forearm. In: Canale ST (ed) Campbell’s operative orthopaedics, vol 3, 10th edn. Mosby, Philadelphia, Pennsylvania, pp 2985–3069
- 8.Enneking TJMQ, Hartlief MT, Fontijne WPJ (1999) Rushpin fixation for midshaft clavicular nonunions: good results in 13/14 cases. Acta Orthop Scand 70(5):514–516 [DOI] [PubMed]
- 9.Grassi FA, Tajana MS, D’Angelo F (2001) Management of midclavicular fractures: comparison between nonoperative treatment and open intramedullary fixation in 80 patients. J Trauma 50(6):1096–1100 [DOI] [PubMed]
- 10.Hill JM, McGuire MH, Crosby LA (1997) Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 79(4):537–539 [DOI] [PubMed]
- 11.Jubel A, Andermahr J, Schiffer G,Tsironis K,Rehm KE (2003) Elastic stable intramedullary nailing of midclavicular fractures with a titanium nail. Clin Orthop Relat Res 408:279–285 [DOI] [PubMed]
- 12.Kernek CB, Robb JA (1986) External callus formation of closed femoral shaft fractures treated by medullary fixation. Orthopedics 9(1):45–51 [DOI] [PubMed]
- 13.Kitsis CK, Marino AJ, Krikler SJ, Birch R (2003) Late complications following clavicular fractures and their operative management. Injury 34(1):69–74 [DOI] [PubMed]
- 14.Leppilahti J, Jalovaara P (1999) Migration of Kirschner wires following fixation of the clavicle—a report of 2 cases. Acta Orthop Scand 70(5):517–526 [DOI] [PubMed]
- 15.Lyons FA, Rockwood CA Jr (1990) Migration of pins used in operations on the shoulder. J Bone Joint Surg Am 72(8):1262–1267 [PubMed]
- 16.Neviaser RJ (1987) Injuries to the clavicle and acromioclavicular joint. Orthop Clin North Am 18(3):433–438 [PubMed]
- 17.Ngarmukos C, Parkpian V, Patradul A (1998) Fixation of fractures of the midshaft of the clavicle with Kirschner wires. Results in 108 patients. J Bone Joint Surg Br 80(1):106–108 [DOI] [PubMed]
- 18.Niemier U, Zimmermann HG (1990) Kuntscher’s open intramedullary nailing of the clavicle. An alternative in the treatment of an old clavicular fracture (in German). Chirurg 61(6):464–466 [PubMed]
- 19.Nordqvist A, Petersson CJ, Redlund-Johnell I (1998) Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma 12(8):572–576 [DOI] [PubMed]
- 20.Petracic B (1983) Efficiency of a rucksack bandage in the treatment of clavicle fractures (in German). Unfallchirurgie 9(1):41–43 [PubMed]
- 21.Poigenfurst J, Rappold G, Fischer W (1992) Plating of fresh clavicular fractures: results of 122 operations. Injury 23(4):237–241 [DOI] [PubMed]
- 22.Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elbow Surg 11(5):452–456 [DOI] [PubMed]
- 23.Robinson CM (1998) Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 80(3):476–484 [DOI] [PubMed]
- 24.Rowe CR (1968) An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res 58:29–42 [DOI] [PubMed]
- 25.Schwarz N, Hocker K (1992) Osteosynthesis of irreducible fractures of the clavicle with 2.7-mm ASIF plates. J Trauma 33(2):179–183 [DOI] [PubMed]