Abstract
Early non-progressive horizontal radiolucent lines (RLLs) (<2 mm) under the tibial component following cemented total knee replacement (TKR) are considered to result from poor cement injection into cancellous bone. These RLLs may facilitate the entry of joint fluid and wear debris into the interface, which may proceed to ballooning osteolysis. There is currently no consensus on the preferred cementing technique (single- versus two-stage cementation) in TKR. We have prospectively analysed postoperative radiographs in 50 consecutive TKRs to compare the RLLs following single- (25 TKRs) and two-stage (25 TKRs) cementation techniques. Of the TKR radiographs studied, 26 (52%) had RLLs; nine (36%) of these were single-stage TKRs, and 17 (68%) were two-stage TKRs. This study demonstrates that single-stage cementing may be superior to the two-stage technique in terms of avoiding RLLs in immediate postoperative TKRs.
Résumé
Après prothèse du genou, un liseré (RLLs) (<2 mm) apparaît de façon très fréquente, précoce, et non évolutive, sous le plateau tibial. Celui-ci est probablement secondaire à une mauvaise pénétration du ciment à l’intérieur du tissu spongieux. Ces liserés facilitent la pénétration du liquide articulaire et des débris d’usure au niveau de l’interface et peuvent être responsables d’ostéolyses. Il n’y a pas de consensus actuellement sur la technique de cimentage (cimentation en un temps ou en deux temps). Nous avons analysé de façon prospective les radiographies de 50 prothèses totales du genou consécutives en comparant les liserés (RLLs) après cimentage en un temps ou en deux temps. 26 (52%) des prothèses totales du genou avaient un liseré, 9/25 (36%) présentaient un liseré inférieur à 2 mm dans les cimentages en un temps, 17/25 (68%) un liseré dans les cimentages en deux temps. Cette étude montre de façon claire que le cimentage en un temps est supérieur à la technique du cimentage en deux temps et évite les liserés immédiats post-opératoires.
Introduction
The technique of cementation in total knee replacement (TKR) has evolved over the last decade. Pulsed lavage followed by suction of the bony cut surfaces and pressurisation with a cement gun has vastly improved the fixation of the components. In addition, the incidence of loosening of the components has decreased following improved techniques of cementing [4, 5, 9]. However, there is still no consensus regarding the cementation technique of the two components (femoral and tibial component). Some surgeons prefer to implant both components at the same time in a single-stage approach, while others tend to implant in two stages (tibial component followed by femoral component, or vice versa).
Radiolucent lines (RLLs) are defined as radiolucent intervals (measured in millimetres) between the cement and the bone [9]. The appearance of peripheral RLLs under the tibial component is a frequent occurrence in the immediate postoperative phase. A number of studies have shown that the preparation of the bone surface has a significant effect on the occurrence of radiolucency at the cement bone interface [9, 14]. The RLLs vary in both size and location according to the technique of pressurisation [10], with progressive radiolucent lines commonly associated with early failure. Hypothesising that the appearance of RLLs depends on the cementing technique, we prospectively evaluated the two approaches to cementing (single and two stage) in terms of RLLs in the immediate postoperative phase.
Methodology
A total of 50 consecutive cemented primary TKRs for osteoarthritis were carried out in 36 patients (25 men, 11 women) between 2001 and 2004. The mean age of the patients was 72.5 years (range: 50–90 years). Posterior cruciate sparing total knee prostheses (Maxim, Biomet, UK) were implanted in all patients. The tibial component had a metal-backed, fixed-compression moulded polyethylene liner with a triangular cross-sectioned keel for tibial fixation. A matching femoro-tibial radius in the medial/lateral direction allowed maximum congruency and minimised point loading. All of the procedures were performed by the senior author (NMG).
Cementing technique
All TKRs were carried out through a midline longitudinal incision and medial parapatellar arthrotomy. The tibial cut was made at 90° to its longitudinal axis using an extramedullary jig, and the distal femoral cut was made at 5° of valgus to the femoral longitudinal axis. Following resection of the tibial plateau, the preparation of bone was same for both the types of cementation. The trabecular bone of the cut surface of the tibia was cleaned by pulsed lavage with normal saline and dried. Irrigation with normal saline opened up the cancellous spaces.
The single-stage cementing technique involved vacuum mixing of two bags of cement. This was applied under pressure with a syringe gun. For the tibial surface, the cement was first delivered into the central keel area and then evenly spread from medial to lateral. The remaining cement was applied under pressure on the femoral cut surface. The tibial component was inserted first, followed by the femoral component. Following insertion of a trial liner, the knee was held in extension to pressurise the cement until it cured. The trial liner was then replaced with a polyethylene liner.
The double-stage cementing technique involved vacuum mixing of one bag of cement for each component separately. For the tibial surface, the cement was delivered in a similar fashion, and the tibial component was inserted. Sustained pressure was maintained on the component until the cement cured. A second bag of cement was vacuum mixed separately. The cement was then applied on the femoral cut surface, the femoral component inserted and sustained pressure maintained until the cement cured. Subsequently, the liner was inserted and the knee reduced.
Following the operation all patients had a drain inserted, and a pressure dressing was applied. The drains were removed after 24 h, and the dressings were reduced on the third postoperative day. All patients were allowed to mobilise the knee and weight-bear from the second postoperative day. All had X-rays on the third postoperative day. Supine anterior-posterior (AP) and lateral (Lat) view X-rays were performed without fluoroscopic positioning by a single radiographer. Any film on which the tibial implant was not in the plane of the radiograph was discarded, and a new radiograph was made. All radiographs appeared to be grossly similar.
All of the X-rays were assessed for RLLs by two of the authors independently at different times. The X-rays were blinded for the single-stage versus the two-stage cementing techniques. Although radiolucency has been previously defined as a radiolucent zone of any size between the cement and bone [2], we observed radiolucencies in the implant-cement interface as well on both the AP and Lat radiographs. The width was measured in millimetres. In condylar designs, a radiolucent zone is more frequent around the tibial than the femoral component [3]. Thus, in this study we only measured the RLLs under the tibial tray. The Knee Society Roentgenographic Evaluation system of Ewald [6] and Modified Radiographic Evaluation System of Bach et al. [2] were used to determine and assess the RLLs. In the AP view (Fig. 1a), the radiolucent zones under the tibial tray were delineated in zones 1 and 2 (medial) and 3 and 4 (lateral). The radiolucent zones 5, 6 and 7 represented the keel area. In the Lat view (Fig. 1b), radiolucent zone 1 is anterior, zone 2 is posterior and zone 3 is at the tip of the keel. We measured the RLLs present in each of the specific component zones [6] as well as the sum of the width of RLLs measured on combined AP and Lat views [2]. If the total sum of the widths of the RLLs was 4 mm or less, the category ‘narrow’ was used; if the total sum of the widths was greater than 4 mm, the category ‘wide’ was used [2].
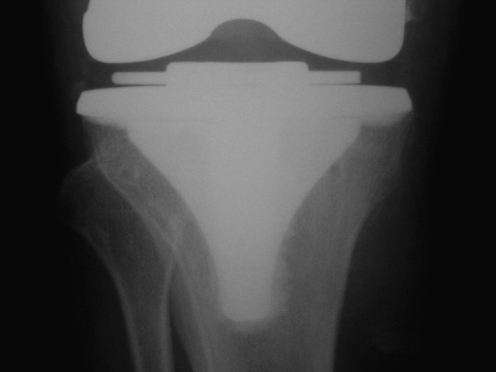
Fig. 1.
Anterior-posterior (AP) (a) and lateral (Lat) (b) views of a representative tibial component showing the zones for the radiolucent lines (RLLs). The depth of the RLLs is measured in millimetres
Results
Equal numbers (25 each) of single- and two-stage TKRs were performed. The radiographs revealed that 26 of the 50 TKRs performed (52%) had RLLs, with more RLLs at the cement-implant interface (18) than at the bone-cement interface (8) (Table 1). Of the 25 single-stage TKRS, nine (25%) had RLLs (≤2 mm), while 17 of the 25 two-stage TKRs (68%) had RLLs (≤2 mm) (Table 2).
Table 1.
Comparison of radiolucent lines (RLLs) in the bone-cement and cement-implant interfaces
| Technique | Bone cement interface only | Cement implant interface only | ||
|---|---|---|---|---|
| Anterior-posterior | Lateral | Anterior-posterior | Lateral | |
| Single stage | 1 | 1 | 2 | 5 |
| Two stage | 6 | 0 | 4 | 7 |
Table 2.
Comparison of RLLs between the two cementing techniques (Knee Society Scoring System [6])
| Technique | Positive AP only score (no. of knees) | Positive Lat only score (no. of knees) | Positive AP + Lat score (no. of knees) | Total |
|---|---|---|---|---|
| Single stage | 1 | 6 | 2 | 9 |
| Twoe stage | 6 | 7 | 4 | 17 |
| Total | 7 | 13 | 6 | 26 |
| Single vs. two stagea | p < 0.05 (SED = 0.12) | p = 0.7 (SED = 0.14) | p = 0.4 (SED = 0.09) |
aResults of independent sample t-test
In the AP view, zones 1 (medial) (Fig. 2) and 4 (lateral) (Fig. 3) were the common sites for RLLs in both groups. In the Lat view, zone 1 (anterior) followed by zone 2 (posterior) were the most common sites of RLLs. In the AP view, there was no significant difference in the number of RLLs (Zone 4) between the two groups. The total number of RLLs in all zones (zones 1–4) was significantly lower in the single-stage group than in the two-stage group (p < 0.05) (Table 2). There was no difference between the two groups in the Lat view.
Fig. 2.
One-millimetre RLL in the bone-cement interface in AP zone 1
Fig. 3.
One-millimetre RLL in the cement-implant interface in AP zone 4
The narrow category of RLLs in the modified evaluation system were observed more frequently when the two-stage technique was used (13) than when the single-stage cementation technique was applied (9); however, this difference was not significant. There were significantly more wide category RLLs in the two-stage TKRs (4) than in the single-stage TKRs (0) (Table 3).
Table 3.
Table showing RLLs assessed by modified version of the Knee Society TKR scoring system
| Technique | Width in mm | Category of RLLs | ||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 4 | 6 | None (0 mm) | Narrow (≤4 mm) | Wide (≥ 4 mm)a | |
| Single stage (no.) | 16 | 7 | 2 | 0 | 0 | 16 | 9 | 0 |
| Double stage (no.) | 8 | 8 | 5 | 3 | 1 | 8 | 13 | 4 |
| Total RLLs (no.) | 24 | 15 | 7 | 3 | 1 | 24 | 22 | 4 |
aThe difference between the single- and two-stage TKRs in terms of wide category RLLs is significant (Spearman correlation p < 0.05).
Discussion
Fixation of the implant occurs by cement penetration into the microstructure of cancellous bone [7]. It has been postulated that the presence of RLLs at the bone–cement interface is due to faulty cementation technique [10]. Ritter et al. [9] demonstrated that the proper preparation of the cancellous bone and pressurisation of the cement reduces the initial occurrence of RLLs. The relative frequency at which RLLs appear on postoperative radiographs and their location depends on the design of the total knee prosthesis [8]. In total condylar prostheses, the RLLs are evident in the bone–cement interface under the tibial component [10]. In our series, we observed RLLs in both interfaces – the bone–cement and cement–implant interface. Other possible causes of the RLLs are thermal bone necrosis [due to heat generated during the polymerisation of polymethyl methacrylate], presence of blood or tissue debris and micromotion (leading to fibrous tissue formation at the bone–cement interface). In our study, we assessed only the immediate postoperative radiographs for RLLs, presuming that there was insufficient time for the development of a fibrous tissue film [1, 8].
Smith et al. [12] described two types of RLLs. The first type is non-progressive and results from poor cement injection. Such RLLs do not affect fixation, but they do facilitate the entry of debris to the interface. The second type is progressive, and these RLLs can quickly expand to become obvious areas of osteolysis. The development of third generation cementing techniques (low-viscosity pressure-injected cement) has been shown to improve cement penetration in the cancellous bone [3].
The two techniques of cementing in TKRs discussed in this study have been widely used without any consensus regarding the efficacy of one over the other. We presume that the presence of early RLLs in the postoperative radiographs of the knees is a result of variation in the cementing technique. We have taken meticulous measures (thorough lavage of the bone surface, suction drying [13] and pressurised cement) to remove other causes for the development of early postoperative radiographic RLLs.
The TKRs cemented using the two-stage technique had more RLLs in zones 1–4 (AP view) than those cemented using the single-stage technique. We postulate that the cause of these RLLs may be an unequal distribution of forces during the two-stage implantation of the tibial and femoral component, whereas the cement may be pressurised equally in all zones when the knee is extended for final pressurisation in the single-stage implantation technique. As a result, the cement may penetrate into the cancellous bone equally in all zones with the latter approach. There was no difference in terms of RLLs in the Lat view in both the anterior and posterior zones. We presume that the forces developed at the interfaces resulting from an AP toggle were similar in the two techniques.
We used the modified system of radiographic scoring in TKR proposed by Bach et al. [2] which we found to be reproducible and reliable. These authors suggested using the combined width of the RLLs present on the two radiographic views to classify narrow and wide RLLs. In their study, RLLs were commonly observed under the tibial component. Evidence suggests that the RLLs that were present at 1 year postoperative were also present at 1 month postoperative, indicating that the radiolucency was related more to the technique of cementation [9]. We support the view of others that the initial fixation of cement by adequate preparation of the bone surface is paramount to avoiding long-term failure of the tibial component. This study demonstrates that the single-stage cementing technique may be superior to the two-stage technique in avoiding RLLs in the immediate postoperative TKRs.
Complete radiolucencies tend to progress with time [5]. The presence of RLLs may result in micromotion between the implant–cement or bone–cement interface, leading to bone resorption and cement loosening [11]. Hence, the proper cementation technique is essential to ensure long-term survival of the TKRs. We recommend the use of the single-stage cementation technique for all TKRs.
References
- 1.Ahlberg A, Linden B (1977) The radiolucent zone in arthroplasty of the knee. Acta Orthop Scand 48:687–690 [DOI] [PubMed]
- 2.Bach CM, Biedermann R, Goebel G, Mayer E, Rachbauer F (2005) Reproducible assessment of radiolucent lines in total knee arthroplasty. Clin Orthop 434:183–188 [DOI] [PubMed]
- 3.DiMaio FR (2002) The science of bone cement: A historical review. Orthopaedics 25:1399–1407 [DOI] [PubMed]
- 4.Dorr LD, Conady JP, Schreiber R, Mehner DK, Hudd D (1985) Technical factors that influence mechanical loosening of the total knee arthroplasty. In: The Knee: 1st Sci Meet Knee Soc. Baltimore University Press, Baltimore, pp 121–135
- 5.Ecker ML, Lotke PA, Windsor RE, Cella JP (1987) Long term results after total condylar knee arthroplasty. Significance of radiolucent lines. Clin Orthop 216:151–158 [PubMed]
- 6.Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop 248:9–12 [PubMed]
- 7.Krause WR, Krug W, Eng B, Miller J (1982) Strength of the cement-bone interface. Clin Orthop 163:290–299 [PubMed]
- 8.Reckling FW, Asher MA, Dillon WL (1977) A longitudinal study of the radiolucent line at the bone–cement interface following total joint -replacement procedures. J Bone Joint Surg 59A:355–358 [PubMed]
- 9.Ritter MA, Herbst SA, Keating EM, Faris PM (1994) Radiolucency at the bone–cement interface in TKR. J Bone Joint Surg Am 76:60–65 [DOI] [PubMed]
- 10.Schneider R, Hood RW, Ranawat CS (1982) Radiologic evaluation of knee arthroplasty. Orthop Clin North Am 13:225–244 [PubMed]
- 11.Sherman RMP, Byrick RJ, Kay JC, Sullivan TR, Waddell JP (1983) The role of lavage in preventing hemodynamic and blood-gas changes during cemented arthroplasty. J Bone Joint Surg Am 65:500–506 [PubMed]
- 12.Smith S, Naima N, Freeman MAR (1999) The natural history of Tibial radiolucent lines in a proximally cemented stemmed total knee arthroplasty. J Arthroplasty 14:3–8 [DOI] [PubMed]
- 13.Stannage K, Shakespeare D, Bulsara M (2000) Suction technique to improve cement penetration under the tibial component in total knee arthroplasty. Knee 10:63–73 [DOI] [PubMed]
- 14.Walker PS, Soudry M, Ewald FC et al (1984) Control of cement penetration in Total Knee Arthroplasty. Clin Orthop 185:155–164 [PubMed]