Abstract
The purpose of this study was to evaluate the relationship between radiological and functional results in patients with extra-articular fractures of the distal radius. We conducted a prospective study of radiological and functional assessment in 95 consecutively selected extra-articular distal radius fractures. There were two patient groups: more than 60 and less than 60 years of age. The final fracture union radiographs were analysed for their functional outcome using the Michigan Hand Outcomes Questionnaire (MHQ) and the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire. In patients with acceptable radiological results, 62% (MHQ group) and 72% (DASH group) of patients had satisfactory functional outcome. Analysing patients with satisfactory functional results, 56% (MHQ group) and 59% (DASH group) had satisfactory radiological results. There was a higher proportion of patients with better functional results, despite poor radiological results, in both of the age groups. There was a statistically significant correlation between satisfactory radial tilt and functional outcome in the younger patients. In the older age group, patients with satisfactory radiological results had satisfactory functional outcome (p < 0.05). However, in the older age group, satisfactory functional results were achieved, despite unsatisfactory radiological results.
Résumé
Le propos de cette étude est d’évaluer les relations entre les résultats radiologiques et fonctionnels des patients ayant présenté une fracture extra articulaire de l’extrémité distale du radius. Une étude prospective et radiologique a été menée chez 95 patients consécutifs présentant ce type de fractures. Ils ont été divisés en deux groupes, le groupe de plus de 60 ans et le groupe de moins de 60 ans. La consolidation finale, radiographique, a été analysée de même que le résultat fonctionnel en utilisant le score de Michigan et le questionnaire DASH. Si l’on prend les patients présentant un résultat radiologique acceptable, 62% selon le score Michigan et 72% selon le score DASH, ceux-ci ont un résultat fonctionnel satisfaisant. Si l’on analyse les patients à partir du score fonctionnel : 56% ayant un score Michigan satisfaisant et 59% un score DASH satisfaisant ceux-ci ont une consolidation radiologique également satisfaisante. Les résultats montrent qu’il existe une proportion élevée de patients ayant un score fonctionnel satisfaisant en dépit d’un résultat radiologique peu satisfaisant dans chaque groupe d’âge. De même il existe une relation statistiquement significative entre la bascule de l’extrémité distale du radius et le résultat fonctionnel chez les patients jeunes. Dans le groupe des patients âgés de plus de 60 ans ceux qui ont un résultat radiologique satisfaisant ont également un résultat cliniquement satisfaisant (p < 0.05). Cependant dans le groupe des patients les plus âgés les résultats fonctionnels satisfaisants sont observés malgré des résultats radiologiques peu satisfaisants.
Introduction
Fractures of the distal radius are the most common fractures of the upper extremity and their adequate care is occasionally overlooked [6]. Osteoporosis is a significant risk factor with respect to the occurrence of distal radius fractures in women above the age of 60 years (17% risk of sustaining fracture in their remaining lifetimes) [13].
Fractures in the younger population results in the loss of future earnings and activity limitation over a number of years [11, 15]. The overall goal should be the optimal restoration of function and anatomy of the wrist [14]. Open or closed reduction and internal fixation may be associated with wrist stiffness and the loss of function, despite good anatomical results [15].
The purpose of this study was to evaluate the relationship between radiological and functional results in patients with extra-articular fractures of the distal radius.
Patients and methods
A prospective clinical and radiological review of 102 consecutive patients, between years 2002 to 2004, with extra-articular fractures of the distal radius treated by manipulation and cast application was carried out. Ninety-five patients were eventually evaluated, as seven patients were excluded due to incomplete data. There were 79 females and 16 males in the study group, with age ranging from 22 to 94 years (average age 67 years) and an average follow-up period of 14 months (range 7 to 34 months). Ninety patients (95%) were treated within 24 h of injury and all patients within 72 h of injury. All of the patients underwent manipulation and the application of a Colles’ cast and advice on plaster care. Forty-six fractures were manipulated under haematoma block, 23 under Biers’ block and 31 under intravenous sedation. They were reviewed 7–10 days later with check radiographs. Thereafter, a well-moulded plaster was applied and regular follow-up was arranged. The length of immobilisation varied between 4–6 weeks. The final radiographic assessment of fracture union was performed at 6–8 weeks and, thereafter, discharged with physiotherapy care.
We measured the radiological parameters of radial height/length, radial angle/inclination and radial tilt (Fig. 1). The radiological criteria of acceptable fracture union were measured as per Graham [8]. Functional results were assessed using the Michigan Hand Outcomes Questionnaire (MHQ) [3] and the Disabilities of the Arm, Shoulder and Head (DASH) questionnaire [21]. The functional and radiological results were analysed using Fisher’s exact probability test, the Mann-Whitney U-test and the Chi-squared test for the two age groups separately and in combination.
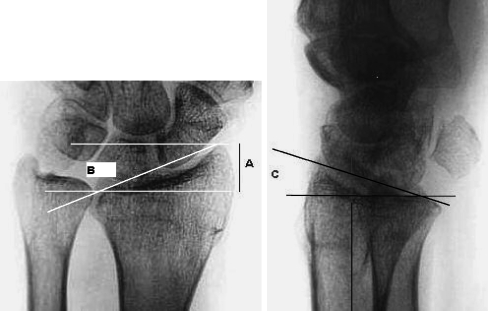
Fig. 1.
Radiographs of the distal radius showing the measurements taken on the anterior–posterior (AP) and lateral views where A is the radial height/length, B is the radial angle/inclination and C is the radial tilt
Results
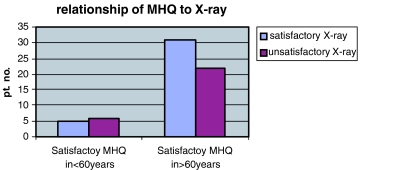
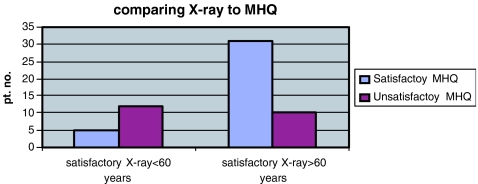
There were 95 patients in this study; 58 patients had satisfactory radiological results and 64 patients (based on the MHQ) and 71 patients (based on the DASH questionnaire) had satisfactory functional results. Figures 2 and 3 compare patients with satisfactory functional results with the radiological results in the two age groups: below and above 60 years of age. In patients under 60 years of age, 11 patients had satisfactory functional results (based on the MHQ and DASH questionnaire), with only five of them having satisfactory radiological results (45%, p > 0.05). In the patient group above 60 years of age, satisfactory functional results were seen in 53 (MHQ group) and 60 patients (DASH group). Thirty-one (58%) and 37 (62%) of patients (in the MHQ group and the DASH group, respectively) had satisfactory radiological results also (no correlation, p > 0.05).
Fig. 2.
Relationship between functional and radiological outcome using the Michigan Hand Outcomes Questionnaire (MHQ)
Fig. 3.
Relationship between functional and radiological outcome using the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire
Figures 4 and 5 compare the acceptable radiological results to the functional results. Seventeen patients (under 60 years of age) had acceptable radiological parameters. Only five patients in the MHQ group (30%) and six patients in the DASH group (35%) had satisfactory functional results (no correlation, p > 0.05). However, in over the 60 years of age group, 41 patients had acceptable radiological results. Of these, 31 (76%) and 37 patients (90%) in the MHQ and DASH groups, respectively, had a good functional outcome (p < 0.05).
Fig. 4.
Comparison of the radiological results to functional outcome using the MHQ
Fig. 5.
Comparison of the radiological results to functional outcome using the DASH questionnaire
On combining both age groups, 58 patients had satisfactory radiological results. Of these, 36 (62% in the MHQ group) and 42 (72% in the DASH group) had satisfactory functional outcome. Of the 37 patients who had unacceptable radiological results, only nine (24% in the MHQ group) and eight patients (22% in the DASH group) had unsatisfactory functional outcome as well. On evaluating patients having satisfactory functional results, we found 56% (MHQ group) and 59% (DASH group) of patients had good radiological results at fracture union. Amongst the unsatisfactory functional outcome group, the percentage of patients with unsatisfactory radiological results were 29 (MHQ group) and 33 (DASH group).
The individual radiological parameters, radial height, radial angle and radial tilt, were assessed with the functional outcome in the two age groups (Tables 1, 2 and 3). There was a significant correlation between satisfactory radial (volar) tilt and having good functional outcome in patients under the age of 60 years (p < 0.05).
Table 1.
Comparison of radial height to functional results in the different age groups
| Satisfactory MHQ in patients <60 years old | Satisfactory MHQ in patients >60 years old | Satisfactory DASH in patients <60 years old | Satisfactory DASH in patients >60 years old | |
|---|---|---|---|---|
| Satisfactory radial height | 9 | 55 | 9 | 48 |
| Unsatisfactory radial height | 2 | 11 | 3 | 11 |
Table 2.
Comparison of radial tilt to functional results in the different age groups
| Satisfactory MHQ in patients <60 years old | Satisfactory MHQ in patients >60 years old | Satisfactory DASH in patients <60 years old | Satisfactory DASH in patients >60 years old | |
|---|---|---|---|---|
| Satisfactory radial tilt | 12 | 48 | 14 | 57 |
| Unsatisfactory radial tilt | 0 | 7 | 0 | 12 |
Table 3.
Comparison of radial angle to functional results in the different age groups
| Satisfactory MHQ in patients <60 years old | Satisfactory MHQ in patients >60 years old | Satisfactory DASH in patients <60 years old | Satisfactory DASH in patients >60 years old | |
|---|---|---|---|---|
| Satisfactory radial angle | 9 | 43 | 9 | 47 |
| Unsatisfactory radial angle | 2 | 12 | 3 | 12 |
Discussion
Smaill stressed the importance of patient satisfaction in the assessment of end results [16]. It is widely believed that accurate reduction and superior radiological results produce good functional outcome [1, 11, 14, 17, 18]. Frykman showed that intra-articular fractures led to deformity and poor functional results [7]. Steward et al. reported a direct correlation between good anatomical and functional results [19]. However, Cassebaum concluded that good function ensued, despite poor anatomical results [2]. Some authors have shown that there is no correlation between functional outcome and satisfactory radiological results [23, 24].
We compared functional outcome to the radiological results and found that patients had better functional results, despite unsatisfactory radiological results in both of the age groups. Amongst patients with satisfactory radiological results (in both age groups), 62% (MHQ group) and 72% (DASH group) of patients had satisfactory functional outcome. Analysing the other way round, amongst patients with satisfactory functional results, 56% (MHQ group) and 59% (DASH group) had satisfactory radiological results at fracture union.
The younger patients require more anatomical alignment for satisfactory functional outcome [11, 15, 19]. The criteria of satisfactory radiological results given by Graham [8] may not be adequate in younger patients. This could have resulted in lower functional scores, despite acceptable radiological results (29% in the MHQ and 35% in the DASH groups). However, in the older age group, there was a statistically significant correlation between satisfactory radiological results and functional outcome.
Cooney et al. [4], Hove et al. [9] and Villar et al. [20] showed that the loss of radial length was associated with poor functional outcome. A combination of radial shortening over 5 mm, radial angle of less than 15° and dorsal tilt of over 15° are associated with poor results [8]. Some authors have shown the importance of restoring the radial tilt for optimum wrist and hand function [12]. Our study design was prospective but not randomised and, therefore, has its limitations. However, we found that satisfactory radial tilt was associated with superior functional outcome in the younger age group of patients (p < 0.05). Dias et al. [5] and Kaukonen et al. [10] also showed the direct relationship of inadequate radial tilt to poor functional outcome. The MHQ and DASH questionnaires are reliable and consistent predictors of functional outcome [3, 22]. We also found a statistically significant relationship between satisfactory radiological results and functional outcome in the older age group.
Conclusion
We conclude that the restoration of anatomical radial tilt results in better functional outcome in young patients. In older patients, there was a statistically significant correlation between an acceptable radiological outcome and good functional results, but the same was not true the other way round. We found that the satisfactory functional results were obtained, despite unsatisfactory radiological results in the older age group.
References
- 1.Broos PL, Fourneau IA, Stoffelen DV (2001) Fractures of the distal radius. Current concepts for treatment. Acta Orthop Belg 67(3):211–218 [PubMed]
- 2.Cassebaum WH (1950) Colles’ fracture. A study of end results. J Am Med Assoc 143(11):963–965 [DOI] [PubMed]
- 3.Chung KC, Hamill JB, Walters MR, Hayward RA (1999) The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg 42(6):619–622 [DOI] [PubMed]
- 4.Cooney WP 3rd, Dobyns JH, Linscheid RL (1980) Complications of Colles’ fractures. J Bone J Surg Am 62(4):613–619 [PubMed]
- 5.Dias JJ, Wray CC, Jones JM (1987) The radiological deformity of Colles’ fractures. Injury 18(5):304–308 [DOI] [PubMed]
- 6.Fernandez DL, Martin CJ (2001) Classification and conservative treatment of distal radius fractures. In: Watson HK, Weinzweig J (eds) The wrist. Lippincott Williams & Wilkins, Philadelphia, Pennsylvania, pp 277–298
- 7.Frykman G (1967) Fracture of the distal radius including sequelae–shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand 108(Suppl):1–155 [DOI] [PubMed]
- 8.Graham TJ (1997) Surgical correction of malunited fractures of the distal radius. J Am Acad Orthop Surg 5(5):270–281 [DOI] [PubMed]
- 9.Hove LM, Fjeldsgaard K, Skjeie R, Solheim E (1995) Anatomical and functional results five years after remanipulated Colles’ fractures. Scand J Plast Reconstr Surg Hand Surg 29(4):349–355 [DOI] [PubMed]
- 10.Kaukonen JP, Porras M, Karaharju E (1988) Anatomical results after distal forearm fractures. Ann Chir Gynaecol 77(1):21–26 [PubMed]
- 11.McQueen M, Caspers J (1988) Colles’ fracture: does the anatomical result affect the final function? J Bone Joint Surg Br 70(4):649–651 [DOI] [PubMed]
- 12.McQueen MM, MacLaren A, Chalmers J (1986) The value of remanipulating Colles’ fractures. J Bone Joint Surg Br 68(2):232–233 [DOI] [PubMed]
- 13.Platt H (1932) Colles’ fracture. Br Med J 2:288–292 [DOI] [PMC free article] [PubMed]
- 14.Porter ML, Stockley I (1984) Functional index: a numerical expression of post-traumatic wrist function. Injury 16(3):188–192 [DOI] [PubMed]
- 15.Rosenthal AH, Chung KC (2002) Intrafocal pinning of distal radius fractures: a simplified approach. Ann Plast Surg 48(6):593–599 [DOI] [PubMed]
- 16.Smaill BG (1965) Long-term follow-up of Colles’s fracture. J Bone Joint Surg Br 47(1):80–85 [PubMed]
- 17.Smilovic J, Bilic R (2003) Conservative treatment of extra-articular Colles’ type fractures of the distal radius: prospective study. Croatian Med J 44(6):740–745 [PubMed]
- 18.Stein H, Volpin G, Horesh Z, Hoerer D (1990) Cast or external fixation for fracture of the distal radius. A prospective study of 126 cases. Acta Orthop Scand 61(5):453–456 [DOI] [PubMed]
- 19.Steward HD, Innes AR, Burke FD (1985) Factors affecting the outcome of Colles’ fracture: an anatomical and functional study. Injury 16(5):289–295 [DOI] [PubMed]
- 20.Villar RN, Marsh D, Rushton N, Greatorex RA (1987) Three years after Colles’ fracture. A prospective review. J Bone J Surg Br 69(4):635–638 [DOI] [PubMed]
- 21.Wakefield AE, McQueen MM (2000) The role of physiotherapy and clinical predictors of outcome after fracture of the distal radius. J Bone Joint Surg Br 82(7):972–976 [DOI] [PubMed]
- 22.Westphal T, Piatek S, Schubert S, Schuschke T, Winckler S (2002) Reliability and validity of the upper limb DASH questionnaire in patients with distal radius fractures (in German). Z Orthop Ihre Grenzgeb 140(4):447–451 [DOI] [PubMed]
- 23.Young CF, Nanu AM, Checketts RG (2003) Seven-year outcome following Colles’ type distal radial fracture. A comparison of two treatment methods. J Hand Surg Br 28(5):422–426 [DOI] [PubMed]
- 24.Young BT, Rayan GM (2000) Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am 25(1):19–28 [DOI] [PubMed]