Abstract
In a recent article, Leigh (J Bone Joint Surg [Br] 88-B:16–18, 2006) notes that patients do not lay down memory when being counselled as to the risks involved in prospective surgery. In our article we focused on the patients’ recall of risk factors involved in elective spinal surgery. We assessed the influence of written information provided to the patients during the consenting process on their recall of operative risks. The study was a prospective randomised study. All patients having elective spinal surgery were included in our study from February 2006 to November 2006 as a consecutive series. Patients were randomised into two groups, one of which received routine consent with verbal explanations (group 1), the other received the same information supplemented by a written sheet explaining the risks of the surgery (group 2). Two weeks later we assessed patients’ recall of the risk involved in the surgery with a questionnaire and compared both groups with a Student t-test. Fifty-three patients (twenty in group 1 and twenty three in group 2) were involved. We noted a significant difference between the two groups in terms of mean number of risks recalled and number of patients recalling each risk (p < 0.001 and p < 0.005, respectively). The addition of a written sheet given to patients during the consenting process makes a significant difference in terms of their recall of the surgical risks in elective lumbar spine surgery. We advocate the routine use of written booklets during the consenting process.
Résumé
Rappel: dans un article récent, Leigh montre que les patients ne se souviennent pas très bien des indicationsqui leur ont été données en ce qui concerne l’information sur les risques avant une intervention chirurgicale. Nous avons souhaité, dans notre étude mettre l’accent sur les risques pouvant survenir dans la chirurgie rachidienne. Nous avons essayé d’évaluer l’importance de l’information écrite lors de la mise en place du consentement éclairé de ces patients. Méthode : cette étude est une étude prospective randomisée. Tous les patients devant bénéficier d’une chirurgie rachidienne ont été inclus dans notre étude sur une période s’étalant de février 2006 à novembre 2006. Tous les patients consécutifs ont été randomisés en deux groupes. Le premier groupe n’ayant que des explications par voie orale, (groupe 1) et le deuxième groupe avec un complément d’informations écrites, (groupe 2). Deux semaines après, ces patients ont été évalués avec un questionnaire et les deux groupes ont été comparés. Résultats : 53 patients dans le groupe 1 et 23 dans le groupe 2 ont été pris en compte dans cette étude. Nous avons noté une différence significative entre les deux groupes soit sur le nombre d’informations retenues par le patient ou le nombre de patients ayant pris en compte ces informations. En conclusion : outre l’information orale, une information écrite remise au patient durant le processus de consentement éclairé en chirurgie du rachis lombaire, est nécessaire avec une différence significative entre les deux groupes. Nous recommandons cette information écrite de façon routinière.
Introduction
Informed consent is a process that is now accepted as being a legal requirement prior to any medical procedure in most countries. It involves a complex balance of provision of information, understanding, confidence and trust between the clinician and his patient. This concept has evolved through the years from turning up to an operation date to complex paperwork and discussions with patients (all encompassing ‘informed consent’). The quality of informed consent is increasingly being evaluated and scrutinised with some thinking it is but a ‘myth’ [13, 19]. The explanation given to and understood by the patient is crucial. The signing of a consent form is secondary, though it may provide evidence that one obtained consent. The consent therefore relies on the very subjective ability of the patient’s recall of facts that were discussed during the consenting process prior to the operation.
In a recent article, Leigh [20] notes that patients do not lay down memory when being counselled as to the risks involved in prospective surgery and that this is of forensic importance. Denial by a patient that he or she received specific information on important topics may reflect absence of provision of such information, or that they have forgotten that it was provided. Both are difficult to prove [21]. A number of studies have shown that retention of medical information decreases over time. In our article we focus on the patients’ recall of risk factors involved in elective spinal surgery. We assess the influence of written information provided to the patients during the consenting process on their recall of operative risks. There have been previous studies looking at the potential of various other modalities (coaching [14], structured interviews [7] and written) for minor [1, 2, 18] and major operations [17]; however, to our knowledge there have been no randomised prospective studies comparing written information to verbal information for complex procedures such as elective lumbar spine surgery.
Patients and method
Trial design
The study was prospective and randomised.
Patients
All patients having elective spinal surgery were included in our study from February 2006 to November 2006. Patients were selected as a consecutive series of patients coming to the pre-operative assessment clinic a few weeks before their operations. We excluded from our study patients unable to give informed consent on their own.
Assignment
Patients were individually randomised with a sealed envelope technique to one of two groups. The first group of patients (group 1) were taken through our routine consenting process which involves verbally explaining the operation, alternative treatments, intended benefits of the surgery and the risks involved in the surgery and providing them with a copy of the consent form. This process is done by the specialist registrar or by the consultant himself and takes around 20 minutes per patient. We used a check-list of risks involved in the operations in order to standardise our explanations. In addition to this consenting protocol, the second group (group 2) of patients received an informative spreadsheet that contained written explanations of the risks involved.
This information spreadsheet was an A4 size sheet containing written explanation (identical to the one provided verbally to both groups) of the risks during or after the operation. Risks included general anaesthetic risks, DVT, heart attack, pulmonary embolism, death, infection, dural tear, bleeding, transfusion, nerve damage, paralysis, loss of bowel/bladder function, failure to relieve symptoms, and worsening of the symptoms; also included were failure of metal work and donor site pain for fusions, damage to vessels, change in voice tone, and damage to wind/food pipe (trachea/oesophagus) for anterior cervical surgery. All patients involved in the study had an identical explanation of the procedure and risk factors using a spine model.
Questionnaire
An A4 size questionnaire was given to the patients the day prior to their operation, about 2 to 3 weeks after the consent process. This questionnaire assessed whether patients remembered having been told about the various risks of surgery. For each of these risks the answer was yes, no, cannot remember or not applicable. This form was filled in by the specialist registrar himself to avoid having patients using their A4 explanation sheet to fill in the questionnaire.
Statistical analysis
Statistical analysis was carried out using the Student’s t-test to compare the two groups.
Results
Fifty-three patients were involved in the study. Group 1 included patients who were consented in the traditional way (i.e. explanation of procedure, risks involved, benefits). Group 2 consisted of patients who had been consented in the traditional way plus an A4 written sheet explanation of the risk factors. Twenty patients were in group 1 and twenty three in group 2.
The average age of the patients in the groups were 62 and 57 years of age in groups 1 and 2, respectively, with no statistically significant difference noted (P = 0.22). Furthermore, there were no significant differences in terms of social class and education levels between the two groups (P = 0.1).
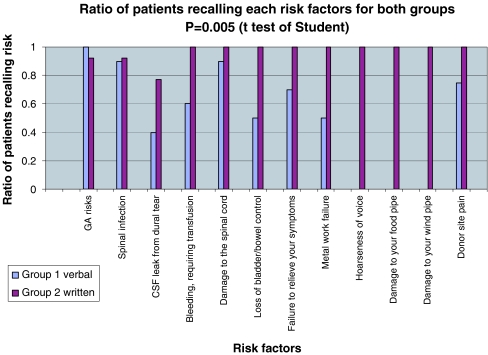
We looked at the percentage of risks recalled for each patient in each group and the number of patients remembering each risk for both groups (Fig. 1).
Fig. 1.
Ratio of patients recalling each risk factor for both groups
The mean percentage of risks recalled for each group was 72.34% and 96.09% for groups 1 and 2, respectively. The difference was significant (p < 0.001) between the two groups.
There was a statistically significant difference between patients in groups 1 and 2 in terms of ratio of patients recalling each risk with a p value of 0.005. The risks most frequently recalled by patients were general anaesthetic risks and damage to the spinal cord with paralysis. The risk that was least remembered was CSF leak from dural tear. The two groups were very similar in terms of patients recall for general anaesthetic risks and spinal infection. The biggest difference between the two groups was noted for CSF leak, bleeding requiring transfusion, loss of bladder/bowel function and failure of the metal work.
Discussion
In this study we focused on recall rather than comprehension because of the difficulty of assessing comprehension and the mere fact that recall is important for medico-legal purposes. So how much information is sufficient? This varies from place to place, with Britain believing in the ‘Bolam principle’, America in the ‘patient needs standard’ [4] and Australia where the Bolam principle was superseded by the judgement of Rogers vs. Whittaker 1992. In this last case an ophthalmic surgeon was found negligent in not warning of a 1 in 14,000 risk of sympathetic ophthalmia [23]. Other papers have reported that risks as low as one in two million have been required to be mentioned to the patient so as to reduce medico-legal action [12, 16, 20]. If this were to be enforced, the doctor would have to recite an endless list of risks which would range from common to ‘merely possible’. In contrast, some studies have shown that the more information provided to patients, the less is recalled and comprehended [7, 8]. It seems that the doctor is caught between ‘a rock and a hard place’—he is unable to leave out details yet too much detail would inevitably reduce recall by the patient laying the groundwork for an indemnity suit if things went ‘pear shaped’.
Despite this, the moderate approach we carried out seemed to work for our cohort of patients and the results from our study does prove that information supplied to patients via information sheets increases the recall of risk factors. This is in contrast to a previous study [25] which showed that despite reinforcement with booklets, there is no improvement in retention. The simplicity of the information sheet seemed to be favoured by most patients and previous studies have shown that a moderate approach to information sheets is favoured over a more comprehensive detailed approach [10]. Small amounts of information are being retained for longer than large amounts [15]. The sheets also help the patient to focus on the more important (medico-legal) features (risks) of the operation since many patients would know someone who has had a successful operation and may, therefore, discount the risks unless fully understood [17]. One paper did relate that the patient would tend to recall a greater number of benefits over complications [14].
Who is able to obtain informed consent? The Clinical Negligence Scheme recommends that ‘consent for elective procedures is obtained by a person capable of performing the procedure’. However, with the rapid turnover of patients, the organisation of clinics and the discontinuity of care of patients resulting from the European Working Time Directives, the GMC has proposed that a junior member of staff can obtain consent from the patient once that person ‘has sufficient knowledge of the proposed investigation or treatment and understands the risks involved’ [11]. Hence, the incorporation of information sheets in our practice would benefit both the patient and the junior staff (who under the Modernising Medical Career scheme would only be in a particular specialty for four months, at any set time in their earlier years).
We should be carrying out informed consent not merely for patient doctor interaction, but for the ever increasing litigious society in which we live. The onus is on the professional to ensure that the patient is well informed [22], so that the patient is able to make an informed decision. It was the belief (in the past) that anxiety was increased by informing patients of those complications which were of minimal risk but had catastrophic consequences (such as mortality); but some papers have shown that an increase of information before a procedure does not increase anxiety [10, 15]. The patients’ autonomy has to be recognised and supported because more and more patients are demanding to be more informed about their condition, their proposed treatment and possible complications [6, 9, 10]. Hence, the consent is a way in which patients are and can be involved with treatment decisions [5].
Cordoza stated that ‘every human being of adult years and sound mind has a right to determine what shall be done with his body, and a surgeon who performs an operation without the patient’s consent commits an assault for which he is liable in damages’ [24]. What are the legal aspects of such a situation? One paper looked at effective methods of reducing indemnity claims with regards to consent, stating that there were reductions in indemnity claims when the surgeon’s notes documented that a discussion of the risks had taken place, consent was taken in an office (rather than in the preoperative holding bay), and good communication was involved [3].
Conclusion
In our article we focussed on the patients’ recall of risk factors involved in elective spinal surgery. We assessed the influence of written information provided to the patients during the consenting process on their recall of operative risks. Fifty-three patients were involved, with group 1 receiving routine consent with verbal explanations and group 2 receiving the same information supplemented by a written sheet explaining the risks of the surgery. We noted a significant difference between the two groups in terms of mean number of risks recalled and number of patients recalling each risk (p < 0.001 and p < 0.005, respectively). The addition of a written sheet given to patients during the consenting process makes a significant difference in terms of their recall of the surgical risks in elective lumbar spine surgery. We advocate the use of written booklets routinely during the consenting process.
References
- 1.Armstrong AP, Cole AA, Page RE (1997) Informed consent: are we doing enough? Br J Plast Surg 50:637–640 [DOI] [PubMed]
- 2.Askew G, Pearson KW, Cryer D (1990) Informed consent: can we educate patients? J R Coll Surg Edinb 35:308–310 [PubMed]
- 3.Bhattacharyya T, Yeon H, Harris M (2005) The medical-legal aspects of informed consent in orthopaedic surgery. J Bone Joint Surg Am 87:2395–2400 [DOI] [PubMed]
- 4.Canterbury v Spence (1972) 464 F 2d 772. US Court of Appeals
- 5.Cassileth BR, Zupkis RV, Sutton-Smith K, March V (1980) Informed consent- why are its goals imperfectly realised? N England J Med 302:896–900 [DOI] [PubMed]
- 6.Courtney MJ (2001) Information about surgery: what does the public want to know? Aust NZ J Surg 71:24–26 [DOI] [PubMed]
- 7.Dawes PJD, O’Keefe L, Adcock S (1993) Informed consent: using a structured interview changes patients’ attitudes toward informed consent. J Laryngol Otol 107:775–779 [DOI] [PubMed]
- 8.Epstein LC, Lasagna L (1969) Obtaining informed consent. Form or substance. Arch Intern Med 123:682–688 [DOI] [PubMed]
- 9.Farnhill D, Inglis S (1993) Patients desire for information about anaesthesia- Australian attitudes. Anaesthesia 48:162–164 [DOI] [PubMed]
- 10.Garden AL, Merry AF, Holland RL, Petre KJ (1996) Anaesthesia information - what patients want to know. Anaesth Intensive Care 24:594–598 [DOI] [PubMed]
- 11.General Medical Council (1998) Seeking patients’ consent: the ethical consideration. GMC, London
- 12.Hekkenberg RJ, Irish JC, Rotstein LE, Brown DH, Gullane PJ (1997) Informed consent in head and neck surgery: how much do patients actually remember? J Otolaryngol 26:155–159 [PubMed]
- 13.Herz Da, Looman JE, Lewis SK (1992) Informed consent: is it a myth? Neurosurgery 30:453–458 [DOI] [PubMed]
- 14.Hutson MM, Blaha JD (1991) Patients’ recall of pre-operative instruction for informed consent for an operation. J Bone Joint Surg Am 73:160–162 [PubMed]
- 15.Inglis S, Farnhill D (1993) The effects of providing preoperative statistical anaesthetic-risk information. Anaesth Intensive Care 21:799–805 [DOI] [PubMed]
- 16.Knapp TA, Huff RL (1976) Emerging trends in the physician’s duty to disclose: an update of Canterbury v Spence. J Leg Med (Chicago) 1:41–45 [PubMed]
- 17.Langdon IJ, Hardin R, Learmonth ID (2002) Informed consent for total hip arthroplasty: Does a written information sheet improve recall by patients? Ann R Coll Surg Engl 84(6):404–408 [DOI] [PMC free article] [PubMed]
- 18.Layton S, Korsen J (1994) Informed consent in oral and maxillofacial surgery: a study of the value of written warnings. Br J Oral Maxillofac Surg 32:34–36 [DOI] [PubMed]
- 19.Leeb D, Bowers DG, Lynch JB (1976) Observations on the myth of ‘informed consent’. Plast Reconstr Surg 58:280–282 [DOI] [PubMed]
- 20.Leigh B (2006) Consent - an event or a memory? J Bone Joint Surg [Br] 88–B:16–18 [DOI] [PubMed]
- 21.Lemaire R (2006) Informed consent - a contemporary myth? J Bone Joint Surg [Br] 88:2–7 [DOI] [PubMed]
- 22.Murphy JFA (2000) Informed consent. Ir Med J 93:68 [PubMed]
- 23.Rogers v Whittaker (1992) 67 ALJR 47. Australian High Court
- 24.Schloendorf v Society of New York Hospital (1914) 10 NE 92
- 25.Turner P, Williams C (2002) Informed consent: patients listen and read, but what information do they retain? N Z Med J 115(1164):U218 [PubMed]