Abstract
The Ilizarov method has been studied extensively in the management of non-union of long bones. In most cases this involves filling of defects present primarily or after débridement by bone transport. Acute docking over gaps longer than 2 cm has not been adequately studied, however. The purpose of this paper is to report the efficacy of acute peg in hole docking as a bone graft-sparing modality in the management of infected non-union of long bones.
Résumé
La méthode d’Ilizarov a été étudiée dans le traitement des pseudarthroses des os longs. Dans la plupart des cas cette perte de substance est secondaire à une mise à plat ou à un transport osseux. Cependant le traitement de perte de substance osseuse de 2 cm a pu être traité de façon extemporanée. Le propos de cette étude est de rapporter l’efficacité de tels traitements avec greffes osseuses lors de la survenue de pseudarthroses infectées des os longs.
Introduction
The problem of non-union has been known to orthopaedic surgeons since they have been treating fractures. Fractures fail to unite as a result of damage from the initial injury and mechanical instability, which are further compounded by bone loss, osteomyelitis, multiple surgical procedures, disuse osteoporosis, soft tissue atrophy and decreased arterial blood flow. Non-union of long bones with infection has always been a challenge for orthopaedic surgeons [3]. The challenge is complicated by additional factors like the presence of deformity, loss of bone, leg length discrepancy and soft tissue damage. Bone union in these situations is not obtained until infection is eradicated [3].
The presence of microbes in the fractured area limits the options available including the use of skeletal allografts, devascularised cortical struts and microvascular hook-ups [5].
Ilizarov discovered that living tissue when subjected to slow steady traction becomes metabolically activated in both the biosynthetic and proliferative pathways, a phenomenon dependent on vascularity and functional use [10]. Application of this method allows the problems of non-union, infection, shortening, deformity and osteoporosis to be addressed simultaneously [3].
Difficult or resistant infections usually require a radical débridement of the septic bone and soft tissue in addition to the application of stable fixation to enhance soft tissue healing and bone union [8, 9]. Bone defects in this situation can be filled up either by acutely shortening the bone or gradually transporting a segment to fill in the defect.
The purpose of this study was to assess the applicability of acute peg in hole docking over longer distances as a treatment modality in infected non-union of long bones.
Materials and methods
From June 2000 to July 2005, 36 cases of infected non-union of long bones were admitted in our department for management; 23 patients had been managed in our hospital from the outset whereas the other 13 had been managed elsewhere prior to their admission to our hospital. Informed consent was obtained from all patients after explaining the procedure and its advantages and potential complications.
Technical considerations
The proper application of the technique necessitated a minute and detailed study of the radiographs of the involved bone taken in the anteroposterior and lateral planes. The bone ends were classified as per the classification of Schwartsmann et al. [20]. Only those cases where at least one of the two main fragments was rhomboidal, pencil-like or trapezoidal were included in this study. This was done to prevent undue resection and sculpting during the surgical procedure. The pre-operative plan included construction of the Ilizarov frame to save operating time.
Operative technique
Intraoperatively the non-union area was approached and sinuses, sequestrate and unhealthy soft tissue débrided aggressively. The ends of the two main bone fragments were exposed. The fragment which was pre-operatively marked out as a peg was sculpted into an invaginating end (cortical peg). The other bone end was converted into a receptacle for this peg (medullary hole). The two ends were fitted into each other (peg in hole).
Stability was tested in a preliminary manner by applying manual force in bending and shear. An invagination of at least 1 cm was achieved. It was also mandatory for the base of the peg to be more than one-third of the diameter of the receiving end in both anteroposterior and lateral planes.
The preassembled Ilizarov frame was affixed and compression applied at the docking site. In all cases where the tibia was operated, a preliminary fibulectomy was done to allow docking to take place. In the lower limb bones where acute docking caused a shortening of more than 2.5 cm, a corticotomy was done in the metaphysis to allow distraction osteogenesis and equalisation of limb length.
Post-operatively any angulation at the docking site as calculated from the radiographs was corrected by differential compression and distraction of the rings. Distraction was started at the corticotomy site 7 days post-operatively and carried out four times a day in 6 hourly increments of 0.25 mm. The distraction was continued until the limb lengths were equalised. In all our cases where distraction was done, consolidation of the regenerate was the determining factor for the removal of the fixator. Docking site union was assessed by stress testing along with radiologic melting of the peg (cortical continuity).
Results
A total of 36 patients participated in this prospective study with an age range of 17–71 years (mean: 37.3 years). There were 22 males and 14 females. In 18 patients the tibia was involved, 9 had involvement of the femur, 6 humeri and in 3 cases both the bones of the forearm were involved (Figs. 1, 2, 3, 4). In these three cases, both the bones were assessed together rather than as individual units (Tables 1 and 2).
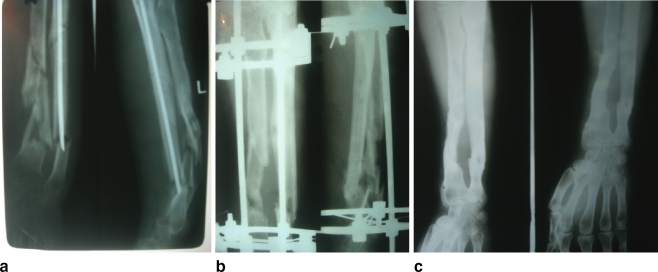
Fig. 1.
Non-union of both the forearm bones (a) managed by débridement and peg in hole docking (b). c Final result
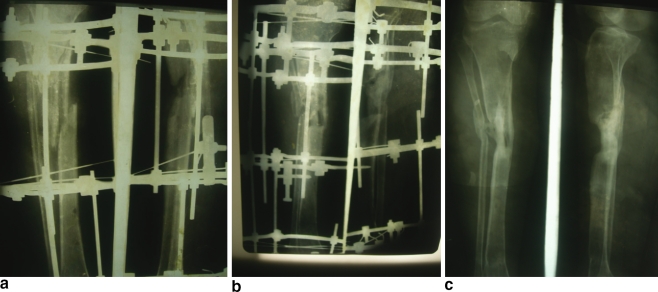
Fig. 2.
a Persistent non-union of the tibia after application of the Ilizarov frame and bone grafting. b Acute docking with peg in hole osteotomy done. c Union status 1 year after removal of the fixator. Regenerate consolidation can be appreciated distally on careful perusal
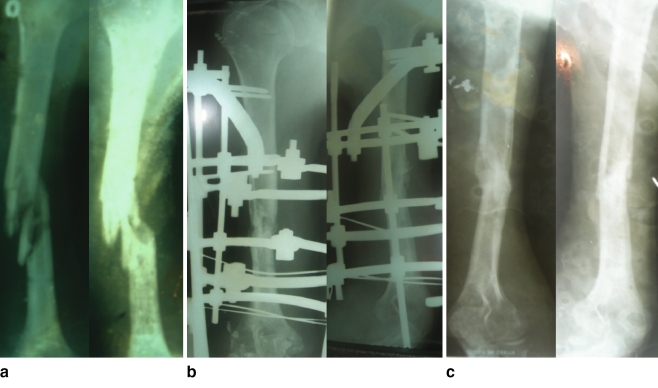
Fig. 3.
a Infected non-union of the humerus due to a firearm injury. b Acute peg in hole docking was done in an Ilizarov frame. c Complete union was achieved
Fig. 4.
The three types of bone ends (arrows). a Trapezoid. b Pencil. c Rhomboid. The peg in hole docking in the three theoretical situations is depicted by the line diagrams
Table 1.
Pre-operative statistics of the patients
| S No. | Age (years) | Sex | Bone involved | Side involved | Cause of injury | Type of injury (compound/closed) | Site of injury | Culture | Type | Number of previous operations | Duration before the index procedure | Pre-operative defect (cm) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (months) | ||||||||||||
| 1 | 17 | M | Tibia | R | FAI | 2 | D | Staph. aureus | Dr | 4 | 12 | 4 |
| 2 | 28 | F | Tibia | R | FAI | 2 | MD | Pseudomonas | Dr | 5 | 13 | – |
| 3 | 31 | M | Tibia | L | Fall | 2 | MD | Mixed flora | Dr | 4 | 8 | 3 |
| 4 | 45 | M | Humerus | L | RTA | 1 | D | Staph. aureus | Dr | 1 | 5 | 2 |
| 5 | 27 | M | Humerus | L | RTA | 2 | D | Mixed flora | Q | 3 | 12 | 2 |
| 6 | 61 | M | Tibia | L | RTA | 3 | D | Staph. aureus | Q | 5 | 16 | 4 |
| 7 | 19 | M | Femur | R | FAI | 2 | M | Pseudomonas | Dr | 2 | 4 | 6 |
| 8 | 53 | F | Femur | R | FAI | 1 | M | Pseudomonas | Q | 3 | 9 | 4 |
| 9 | 55 | M | Tibia | L | FAI | 2 | D | Staph. aureus | Dr | 3 | 13 | 3 |
| 10 | 33 | F | Tibia | R | FAI | 3 | M | Staph. aureus | Q | 4 | 12 | 4 |
| 11 | 60 | M | Tibia | R | Crush | 2 | D | Staph. aureus | Q | 3 | 9 | 3 |
| 12 | 31 | F | Femur | L | RTA | 2 | D | Mixed flora | Dr | 6 | 15 | 6 |
| 13 | 32 | M | Tibia | R | FAI | 2 | M | Klebsiella | Dr | 4 | 13 | 4 |
| 14 | 19 | F | Femur | R | FAI | 2 | D | Pseudomonas | Q | 2 | 6 | 4 |
| 15 | 34 | M | Femur | L | FAI | 1 | M | Pseudomonas | Q | 5 | 9 | 12 |
| 16 | 63 | M | Tibia | R | Fall | 2 | M | Staph. aureus | Dr | 1 | 4 | 1 |
| 17 | 45 | M | FABB | L | FAI | 2 | M | Klebsiella | Dr | 2 | 3 | 3 |
| 18 | 21 | F | Femur | R | FAI | 3 | MD | Staph. aureus | Q | 2 | 6 | 2 |
| 19 | 17 | M | Tibia | R | RTA | 2 | MD | Staph. aureus | Dr | 4 | 9 | 3 |
| 20 | 31 | M | FABB | R | RTA | 2 | D | Mixed flora | Dr | 2 | 4 | 3 |
| 21 | 28 | M | Femur | L | Fall | 1 | D | Staph. aureus | Dr | 2 | 1 | 2 |
| 22 | 17 | F | Humerus | L | RTA | 3 | D | Mixed flora | Dr | 3 | 3 | 3 |
| 23 | 43 | F | Femur | R | RTA | 2 | M | Mixed flora | Dr | 4 | 4 | 6 |
| 24 | 46 | M | Humerus | L | FAI | 3 | M | Pseudomonas | Dr | 2 | 2 | 3 |
| 25 | 21 | M | FABB | L | Fall | closed | MD | Klebsiella | Dr | 3 | 3 | 3 |
| 26 | 59 | F | Humerus | R | RTA | 1 | M | Staph. aureus | Dr | 5 | 5 | 3 |
| 27 | 23 | F | Tibia | L | RTA | 2 | D | Klebsiella | Q | 6 | 6 | 3.5 |
| 28 | 67 | F | Tibia | R | FAI | 2 | M | Staph. aureus | Dr | 3 | 3 | 6 |
| 29 | 71 | M | Tibia | L | FAI | 2 | D | Pseudomonas | Dr | 4 | 4 | 6 |
| 30 | 19 | F | Tibia | R | FAI | 3 | M | Klebsiella | Dr | 2 | 2 | 2.5 |
| 31 | 27 | M | Tibia | L | RTA | 1 | D | Mixed flora | Dr | 4 | 4 | 2.5 |
| 32 | 31 | M | Femur | R | RTA | 2 | D | Mixed flora | Dr | 4 | 4 | 3 |
| 33 | 45 | M | Humerus | R | FAI | 3 | D | Staph. aureus | Dr | 3 | 3 | 2.5 |
| 34 | 53 | F | Tibia | L | FAI | 2 | MD | Staph. aureus | Dr | 2 | 2 | 4 |
| 35 | 33 | F | Tibia | L | FAI | 2 | D | Mixed flora | Dr | 1 | 1 | 4 |
| 36 | 41 | M | Tibia | R | RTA | 2 | M | Pseudomonas | Dr | 4 | 4 | 5 |
M male, F female, R right, L left, FAI firearm injury, RTA road traffic accident, D diaphyseal, M metaphyseal, MD metaphyseodiaphyseal, Dr draining, Q quiescent, FABB forearm, both bones
Table 2.
Operative and post-operative statistics
| S No. | Procedure | Distraction lengthening | Regenerate consolidation | Complications | Docking union | Result grading | |||
|---|---|---|---|---|---|---|---|---|---|
| (cm) | Problems | Obstacles | True complications | (weeks) | Bone | Functional | |||
| 1 | Do+T | 5 | Normal | PTI, depression | 8 | Excellent | Excellent | ||
| 2 | Do | – | – | PTI, pain | 8 | Excellent | Excellent | ||
| 3 | Do+T | 3 | Normal | PTI, pain | 10 | Excellent | Good | ||
| 4 | Do | – | – | Dysthesia | 8 | Good | Excellent | ||
| 5 | Do | – | – | – | 8 | Good | Excellent | ||
| 6 | D+T | 4 | Delayed | PTI, pain, oedema, | Delayed consolidation | 12 | Excellent | Good | |
| 7 | Do+T | 2 | Premature | PTI | Premature consolidation | 8 | Good | Fair | |
| 8 | Do+T | 5 | Normal | PTI | 8 | Good | Fair | ||
| 9 | Do+T | 4 | Normal | PTI, pain | 10 | Good | Fair | ||
| 10 | Do+T | 6 | Normal | Pain | 8 | Excellent | Good | ||
| 11 | Do+T | 4 | Normal | PTI, pain | 10 | Excellent | Excellent | ||
| 12 | Do+T | 6 | Normal | PTI, pain | 10 | Fair | Fair | ||
| 13 | Do+T | 4 | Normal | PTI, oedema | 10 | Excellent | Good | ||
| 14 | Do+T | 5 | Normal | Pain | 10 | Good | Fair | ||
| 15 | Do+T | 10 | Delayed | PTI, pain | Delayed consolidation | Angulation of the regenerate | 14 | Poor | Poor |
| 16 | Do | – | – | Pain | 10 | Excellent | Excellent | ||
| 17 | Do | – | – | PTI, pain | RSOD | 8 | Fair | Poor | |
| 18 | Do | – | – | – | PTI | 8 | Good | Good | |
| 19 | Do+T | 3 | Normal | PTI | 8 | Excellent | Excellent | ||
| 20 | Do | – | – | Pain, dysthesia | 8 | Good | Fair | ||
| 21 | Do | – | – | PTI | 8 | Fair | Good | ||
| 22 | Do | – | – | Pain | 8 | Good | Excellent | ||
| 23 | Do+T | 7 | Normal | PTI, pain | 10 | Good | Fair | ||
| 24 | Do | – | – | PTI, pain | 8 | Good | Excellent | ||
| 25 | Do | – | – | Pain | 8 | Good | Fair | ||
| 26 | Do | – | – | Metal allergy | 10 | Good | Excellent | ||
| 27 | Do+T | 4 | Delayed | PTI, pain | Delayed consolidation | 8 | Excellent | Good | |
| 28 | Do+T | 7 | Normal | PTI | 10 | Excellent | Excellent | ||
| 29 | Do+T | 7 | Delayed | PTI, pain | Delayed Consolidation | 10 | Excellent | Good | |
| 30 | Do+T | 2.5 | Normal | PTI, pain | 8 | Excellent | Excellent | ||
| 31 | Do+T | 3 | Delayed | Pain, oedema | Delayed consolidation | 10 | Excellent | Good | |
| 32 | Do+T | 3 | Delayed | PTI | Delayed consolidation | 12 | Fair | Fair | |
| 33 | Do | – | – | Pain | 8 | Good | Good | ||
| 34 | Do+T | 5 | Normal | PTI | 12 | Excellent | Excellent | ||
| 35 | Do+T | 5 | Normal | PTI, oedema | 10 | Excellent | Good | ||
| 36 | Do+T | 5 | Normal | PTI, dysthesia | Ring sequestrum | 14 | Fair | Fair | |
Do docking, T transport, PTIpin tract infection, RSOD reflex sympathetic osteodystrophy
The primary cause of injury was a firearm injury (FAI) in 18 cases, road traffic accident (RTA) in 13, fall from a height in 4 and a crush injury due to a collapsing wall in 1. The original injury was type 1 compound in 6 cases, type 2 compound in 22 cases and type 3 compound in 7 cases [7]. One case had a closed fracture initially. Before the application of the peg in hole modality of treatment the number of surgical interventions ranged from 1 to 6 with a mean of 3.25 interventions per patient. The duration of treatment before application of the final procedure was 1–16 months (mean: 6.4 months). At the time of the surgery 10 patients had a quiescent infection (Q) and 26 had a draining infection (Dr).
The defects on the basis of pre-operative roentgenograms ranged from 0 to 12 cm (mean: 3.6 cm). In the forearm bones, the radiologically larger defect was added to the clinical limb length discrepancy to calculate the defect.
Acute peg in hole docking was done in all the cases and 23 cases required concomitant distraction osteogenesis to re-establish the limb length. The mean distraction length in these cases was 4.76 cm. In 16 of these cases the regenerate consolidated normally, prematurely in 1 and in 6 cases it was delayed.
The time to docking site union averaged 9.4 weeks. This was ascertained clinically by stress testing and radiologically by observing the melting of the clear margins of the peg. We encountered a total of 64 complications with 54 being problems, 7 obstacles and 3 true complications [18]. The three true complications were reflex sympathetic dystrophy (RSOD), premature consolidation and formation of a ring sequestrum around an olive wire which continued to drain at the completion of treatment.
The bone results were assessed according to the protocol laid down by the association for the study and application of the method of Ilizarov [17]. An excellent result was defined as union, no infection, deformity of less than 7° and leg length inequality of less than 2.5 cm; a good result was defined as union and any two of the other three criteria; a fair result was defined as union and one of the other criteria; and a poor result was defined as non-union or refracture, or as union in the absence of any of the other three criteria.
Accordingly we had 16 excellent, 14 good, 5 fair and 1 poor result. In cases where both the bones of the forearm (radius and ulna) were managed with this modality, the bone of the forearm with the poorer result was represented. The poor result occurred in a femoral defect docked over 12 cm where the regenerate angulated. The patient had a functionally poor result due to stiffness of the knee. He refused further intervention and manages his routine activities with a shoe raise.
The functional result was based on five criteria: a noteworthy limp, stiffness of adjacent joints (loss of more than 15° of motion), soft tissue sympathetic dystrophy (RSOD), pain that reduced activity or disturbed sleep and inactivity. The functional result was considered excellent if the patient was active and none of the other four criteria were applicable, good if the patient was active but one or two of the other criteria were applicable, fair if the patient was active but three or four of the other criteria were applicable and poor if the patient was inactive [3]. On this basis we had 13 excellent, 11 good, 10 fair and 2 poor results. The follow-up of the first poor result has been mentioned earlier. The other poor result occurred in a case where both bones of the forearm were docked. The patient developed reflex sympathetic dystrophy which was managed by physiotherapy.
Discussion
The purpose of reporting this study was to reinforce the fact that acute docking over longer distances with a peg in hole invagination contact is possible without compromising the final result and it gives advantages that are lacking with the conventional transport and bone grafting techniques.
Infected non-union of long bones remains a management challenge, due to its association with deformity, loss of bone, leg length discrepancy and soft tissue damage [3].
In the process of débriding the infected tissue, significant defects at the non-union site are often created. Golyakhovsky et al. classified a gap of more than 3 cm as a large bone loss [4].
Successful treatment of infected non-union often combines radical débridement of the septic bone and soft tissue in addition to application of stable fixation to enhance soft tissue healing and bone union [8].
Various modalities of treatment have been used from time to time including the use of cancellous bone grafts, vascularised free tissue transfer and electrical stimulation [14].
Papineau et al. presented their series where infected non-union was treated by débridement, external fixation and bone grafting. The high amount of graft loss and the requirement that it be kept moist make the procedure unsuitable for defects larger than 4 cm [19].
Microsurgical composite osteomyocutaneous free tissue transfer has been used in the reconstruction of bone defects. These often fail due to the short vascular pedicle that prohibits anastomosis outside the zone of injury [21]. Besides this the occurrence of fatigue fracture, high non-union rate and donor site morbidity are considerations when offering this procedure to the patient.
Electricity in the form of direct current is contraindicated in the presence of draining osteomyelitis, besides causing immobilisation and rehabilitation problems [25].
Conventionally non-unions have been treated by converting an infected draining non-union into a non-draining non-union and then promoting union by bone grafting. This usually involves three operations conducted in three separate sittings, i.e. saucerisation of the wound with fixation, skin grafting and bone grafting. Weber et al. and Judet et al. reported an active method of treating infected non-unions which involves restoration of bony continuity, osteoperiosteal grafting, fixation and use of suction irrigation drains. They reported a 15% failure rate [12, 23].
Calhoun et al. treated this problem with the use of antibiotic impregnated polymethyl methacrylate beads [2]. However, significant immobilisation and rehabilitation problems were encountered.
Ilizarov spoke of a discovery of a number of common biologic regularities that encourage both the repetitive and formative processes of regeneration and growth not only of bone tissue, but also of soft tissue in damaged and diseased locomotor systems [11].
These revolutionary techniques devised by Ilizarov have created a new potential for the salvage and reconstruction of the residuals of non-union and chronic osteomyelitis [1].
Difficult or resistant infections usually require radical débridement of the septic bone and soft tissue in addition to the application of stable fixation to enhance soft tissue healing and bone union [8]. This débridement usually leads to the creation of a defect.
Use of the Ilizarov circular frame allows resection of the infected bone, repair of the defect and stabilisation to consolidation while maintaining or restoring the length of the limb. The defects resulting from bone loss can be filled by one of the two methods.
Acutely shortening the bone and then gradually lengthening it to restore length
Bone transport to fill in the defect [6]
Transporting a bone fragment often throws up obstacles that require surgical intervention. This includes non-union of the transported fragment and docking site refracture [4, 15].
Also because the healing of the target site does not begin until intercalary lengthening of the fragment is complete, patients requiring bone transport are maintained in the external fixator longer than those needing comparable limb elongation [8].
In a majority of lax pseudoarthrosis, the bone ends are usually osteopaenic. The osteopaenia progresses during the distraction period. Therefore, at the end of distraction, when the constant tension stress is no longer present, stable fixation of the bone ends may become significantly compromised [20].
Acute docking as a treatment modality has not been studied in any large series in the literature. Docking acutely under vision allows compression and does not rely on transformational osteogenesis. In order to achieve an adequate area of bone contact or to increase stability by appropriate sculpting of the contact surfaces, the shape of the bone ends must be considered [20]. Usually bone ends are resected in order to accomplish end-to-end contact and compression. This usually, in our experience, increases the resultant defect. Improved contact with less bone resection as well as improved fracture stability may be obtained by using the peg in hole osteotomy whereby the end of one fragment is invaginated into the end of the other main fragment. Results of our series show that acute docking circumvents several problems that afflict conventional bone grafting and internal bone transport.
In the 39 bones that were docked in 36 patients, bone grafting was not required in any case. In studies carried out by Marsh et al., Yokoyama et al. and Thirumal et al., additional procedures like bone grafting were required in 10, 50 and 50% of their cases, respectively [16, 22, 24]. The statistical difference with our series is significant.
The time from surgery to union at the docking site averaged 9.4 weeks in our series. According to Dendrinos et al. the time taken for an intercalary segment to unite at the docking site after conventional internal transport is 24 weeks [3]. Again the difference is statistically significant.
Shortened treatment time. This is especially noticed in upper limb bones as according to Kocaoglu et al., a shortening of 4–5 cm can be tolerated without any functional or cosmetic disability [13]. In the lower limb bones length equalisation was the limiting factor as the docking site union progressed rapidly.
At the latest follow-up none of our cases had sustained a refracture at the docking site. Maini et al. reported a refracture rate of 10% in their series [15].
Adjustment of axial alignment post-operatively as the peg does not allow displacement at the docking site.
Reduction in the number of reoperations as the docking site does not need to be freshened. Only one case in our entire series required an additional surgical procedure for the débridement of a ring sequestrum.
The technique is versatile and applicable to all limb bones as our series shows. The results of this series encourage application of this method more widely as possible complications of oedema due to kinking of vessels and lymphatics which occurs in acute docking of greater than 2 cm was hardly encountered.
Conclusion
Acute peg in hole docking in infected non-union of long bones addresses the basic principles of axial alignment, vascularity, stability and function simultaneously.
References
- 1.Aronson J, Johnson E, Harp JH (1989) Local bone transportation for treatment of intercalary defects by the Ilizarov technique. Biomechanical and clinical considerations. Clin Orthop Relat Res 243:71–79 [PubMed]
- 2.Calhoun JH, Henry SL, Anger DM, Cobos JA, Mader JT (1993) The treatment of infected nonunions with gentamicin-polymethylmethacrylate antibiotic beads. Clin Orthop Relat Res 295:23–27 [PubMed]
- 3.Dendrinos GK, Kontos S, Lyritsis E (1995) Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg Am 77(6):835–846 [DOI] [PubMed]
- 4.Golyakhovsky V, Frankel VH (1991) Ilizarov bone transport in large bone loss and in severe osteomyelitis. Bull Hosp Jt Dis Orthop Inst 51(1):63–73 [PubMed]
- 5.Green S (1994) Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res 301:111–117 [PubMed]
- 6.Gugenheim JJ Jr (1998) The Ilizarov method. Orthopedic and soft tissue applications. Clin Plast Surg 25(4):567–578 [PubMed]
- 7.Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 58(4):453–458 [PubMed]
- 8.Heppenstall RB (1984) The present role of bone graft surgery in treating nonunion. Orthop Clin North Am 15(1):113–123 [PubMed]
- 9.Hosny G, Shawky MS (1998) The treatment of infected non-union of the tibia by compression-distraction techniques using the Ilizarov external fixator. Int Orthop 22(5):298–302 [DOI] [PMC free article] [PubMed]
- 10.Ilizarov GA (1990) Clinical application of the tensionstress effect for limb lengthening. Clin Orthop Relat Res 250:8–26 [PubMed]
- 11.Ilizarov GA (1997) The principles of the Ilizarov method. Bull Hosp Jt Dis 56(1):49–53 [PubMed]
- 12.Judet PR, Patel A (1972) Muscle pedicle bone grafting of long bones by osteoperiosteal decortication. Clin Orthop Relat Res 87:74–80 [DOI] [PubMed]
- 13.Kocaoglu M, Eralp L, Tomak Y (2001) Treatment of humeral shaft non-unions by the Ilizarov method. Int Orthop 25(6):396–400 [DOI] [PMC free article] [PubMed]
- 14.Lenoble E, Lewertowski JM, Goutallier D (1995) Reconstruction of compound tibial and soft tissue loss using a traction histogenesis technique. J Trauma 39(2):356–360 [DOI] [PubMed]
- 15.Maini L, Chadha M, Vishwanath J et al (2000) The Ilizarov method in infected nonunion of fractures. Injury 31(7):509–517 [DOI] [PubMed]
- 16.Marsh JL, Prokuski L, Bierman JS (1994) Chronic infected tibial nonunions with bone loss. Conventional techniques versus bone transport. Clin Orthop Relat Res 301:139–146 [PubMed]
- 17.Paley D, Catagni MA, Argnani F (1989) Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 241:146–165 [PubMed]
- 18.Paley D (1990) Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 250:81–104 [PubMed]
- 19.Papineau LJ, Alfageme A, Dalcourt JP et al (1979) Osteomyelit chronique; eccision et griffe de spongieuz a l’air libre après mises a plat extensives. Int Orthop 3:165–176 [DOI] [PubMed]
- 20.Schwartsman V, Choi SH, Schwartsman R (1990) Tibial nonunions. Treatment tactics with the Ilizarov method. Orthop Clin North Am 21(4):639–653 [PubMed]
- 21.Schwartz WM, Mears DC (1985) The role of free-tissue transfers in lowerextremity reconstruction. Plast Reconstr Surg 76:364–373 [DOI] [PubMed]
- 22.Thirumal M, Shong HK (2001) Bone transport in the management of fractures of the tibia. Med J Malaysia 56(1):44–52 [PubMed]
- 23.Weber BG, Cech O (1976) Pseudoarthrosis, pathology, biomechanics, therapy, results. Hans Huber, Bern, Switzerland
- 24.Yokoyama K, Itoman M, Nakamura K et al (2001) Free vascularized fibular graft vs. Ilizarov method for post-traumatic tibial bone defect. J Reconstr Microsurg 17(1):17–25 [DOI] [PubMed]
- 25.Youdas JW, Wood MB, Calahan TD et al (1988) A quantitative analysis of donor site morbidity after vascularized fibula transfer. J Orthop Res 6:621–629 [DOI] [PubMed]