Abstract
An experimental study was conducted in order to evaluate biomechanical methods of single-bundle reconstruction in ACL and compare it with a new double-bundle double-tibial tunnel technique. Twenty-four porcine cadaver knees, divided into 4 groups of 6 knees each and 48 proper extensors of the fourth toe tendons, were used for the fixation techniques. In groups A and B, a double-bundle technique with a single femoral and tibial tunnel was used, fixed to a femoral and tibial post with screws and with buttons, respectively. In groups C and D, a double-bundle technique (technique Δ) with two separate tibial tunnels was used, fixed to a femoral and tibial post with screws and with buttons, respectively. A material testing system (Instron) was used for anteriorly translating the tibia until failure. The femoral and tibial post as a fixation method is superior to the conventional buttons technique. The more anatomical double-bundle reconstruction technique provided significantly higher structural properties and smaller loss of fixation compared with the single-bundle reconstruction technique. The comparison of the two techniques gave superior results to the femoral and tibial screws over the buttons. The double-bundle technique attempts to restore the anterior stability of the knee joint.
Résumé
Une étude expérimentale a été réalisée de façon à évaluer en biomécanique, la reconstruction du ligament croisé antérieur avec un faisceau en comparant celle-ci avec une reconstruction avec deux faisceaux et un double tunnel tibial. Vingt quatre cadavres de porcs ont été répartis en 4 groupes de 6 genoux chacun. Dans le groupe A et B une technique à double faisceaux a été réalisée avec un simple tunnel fémoral et tibial, par vis sur rondelle. Pour les groupes C et D, un double faisceau (technique A) a été réalisé avec deux tunnels tibiaux séparés, fixé au fémur et au tibia avec également une vis et un bouton. Le montage a été testé grâce au système Instron utilisant jusqu’à la rupture une translation antérieure du tibia. La fixation postérieure fémorale tibiale est supérieure à la fixation conventionnelle par une vis avec rondelle. La reconstruction par double faisceaux est supérieure à la reconstruction par simple faisceau. En conclusion, la comparaison de ces deux techniques montre des résultats supérieurs pour une fixation fémorale et tibiale par vis avec rondelles. La technique de double faisceaux permet de restaurer une anatomie et une stabilité antérieure de l’articulation du genou.
Introduction
Rupture of the anterior cruciate ligament (ACL) has the highest incidence among ligamentous injuries in the human knee [10].
With recent advances in the understanding of the biomechanical and biological properties of the intact ACL, a large number of surgical reconstruction techniques with various graft choices have evolved. In past years, the patellar and hamstring tendons (semitendinosus and gracilis) have become the most frequently used replacement grafts for the ruptured ACL [7, 13, 16].
Previous studies have demonstrated that the material properties of the porcine patellar and flexor digitorum profundus tendons were similar to the human patellar tendon and hamstring tendons, respectively [11]. To improve the results of ACL reconstruction under the aggressive early rehabilitation and to reproduce the complex functional anatomy of the native ACL, many authors recommend the use of double-bundle techniques [9, 13, 17].
The proposed reconstruction method uses two tendon grafts for the antero-medial and postero-lateral bundle of ACL, possessing a distance of at least 14 mm between them. This reconstruction method was named Δ technique because of the Δ shape the grafts have from the lateral view when they are positioned into their tunnels. Previous studies have demonstrated that the ACL in humans has a wide insertion in its tibial insertion varying from 18 mm to 30 mm [19].
The purpose of our experimental study is to describe and evaluate biomechanical fixation methods of the new double-bundle double-tibial tunnel technique and to compare it with single-bundle ACL reconstruction.
Materials and methods
Study design
In this study, posterior porcine legs from fully mature pigs, weighing approximately 70 kg, were used to simulate ACL reconstruction. Twenty-four porcine knees and 48 proper extensors of the fourth toe tendons, harvested from the lower limbs, were stored at −20°C. All knees and ligaments were thawed at room temperature 24 hours before use and kept moist with saline irrigation during preparation and mechanical testing. All soft-tissue structures and patella except ACL were dissected leaving a femur-ACL-tibia complex.
A pilot study was conducted in order to determine the mechanical properties of porcine tendons of six proper extensors of the fourth toe tendons that were 8 cm each. Each tendon graft was sutured at the distal part with two Dexon 2 bi-color sutures, leaving 1 cm of free tendon ends and a free middle part of 2 cm. The specimens were attached to a material testing system (Instron) and underwent the tensile failure test. A tensile load of 70 N was applied to the graft for 2 min, as an initial graft tension, to precondition the complex. The maximum load was 333.3 N (321–345 N) for the proper extensor of the fourth digit tendon with 3.8-mm diameter, which was used as a graft for the reconstruction procedures.
Knee specimens were randomly divided in into four groups of six specimens each. For each group, the ACL was resected. The diameter of each tendon graft was measured with a slot device with an increasing diameter of 2 mm for each slot. The diameter of the femoral and tibial tunnels was matched to the graft diameter in each knee. The four suture strands at each end of the composite graft were tied to a femoral and a tibial post (25 × 6.5-mm cancellous screw), with the knee in the appropriate position, depending on the reconstruction technique, and with the posterior femoral condyles and the posterior tibial plateau in the same coronal plane.
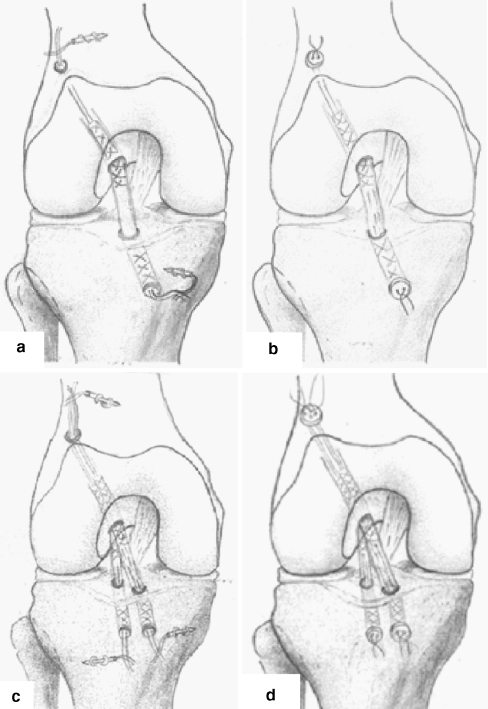
In group A, double-bundle tendon grafts were secured with the suture-post technique to a femoral and a tibial post (25 × 6.5-mm cancellous screw), with the knee in semi-flexion and with the posterior femoral and tibial condyles in the same coronal plane, using a single femoral and tibial tunnel (Fig. 1a).
Fig. 1.
The fixation techniques. a Double-bundle tendon graft single-tunnel technique, fixed with sutures tied over screws. b Double-bundle tendon graft single-tunnel technique, fixed with the sutures tied over buttons. c Double-bundle tendon graft double-tibia tunnel technique, fixed with sutures tied over screws. d Double-bundle tendon graft double-tibia tunnel technique, fixed with the sutures tied over buttons
In group B, the same technique was used, and the tendon grafts were fixed with the conventional suture tied over a button technique (Fig. 1b).
In group C, a double-bundle technique was used with two separate tibial tunnels, and the suture strands at each end of the composite graft were tied to femoral and tibial post (25 × 6.5-mm cancellous screw), with the knee in 30° of flexion for the antero-medial bundle and in 100° of flexion for the postero-lateral bundle. The first tunnel was drilled in the antero-medial border of the tibial insertion of the ACL and the second drill was positioned 14 mm postero-laterally to the first drill, at the posterior border of the ACL insertion area (Fig. 1c).
In group D the same double-bundle technique as in the previous group was used, and the tendon grafts were fixed with the suture tied over a button technique (Fig. 1d).
In all four groups, grafts were placed in the tibial and femoral tunnels, after a preconditioning of 70 N for 2 minutes.
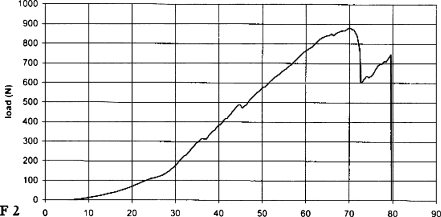
Biomechanical tests were performed on the ACL reconstructions using an Instron materials testing machine (Instron Corp.). The femur and the tibia were mounted onto the tensile tester with specially designed grips at 60° of flexion, neutral rotation, and anatomical vertical alignment. An approximately 3-mm separation of the articular surfaces was maintained to eliminate femoral-tibial shear forces. Each specimen was kept moist with saline solution during the testing. First, an anterior preload of 5 N was applied. An anterior drawer force was then applied at a cross-head speed of 20 mm/min, translating the tibia anteriorly to the femur with all other motion constrained. The applied force and the translation of the cross-head were recorded throughout the tensile failure tests done by the material testing machine, in order to obtain a load-displacement curve (Fig. 2), and transferred to a personal computer. From this curve and the recorded data, we obtained the maximum load, the stiffness and the forward displacement of the tibia. The modes of failure were also recorded. Stiffness is a parameter that best correlates with the clinical grading of joint laxity in clinical examination. The greater the stiffness is, the less the displacement for a given force and the lower the laxity grade.
Fig. 2.
The load-displacement curve of one specimen of group c
Statistical analysis was conducted with the SPSS 12 software package. In all groups non-parametric distribution of the data was found (Kolmogorow-Smirnow test). One-way analysis of variation (ANOVA) and the Mann-Whitney U Wilcoxon rank-sum test were used in the four groups for determining differences in each parameter.
Results
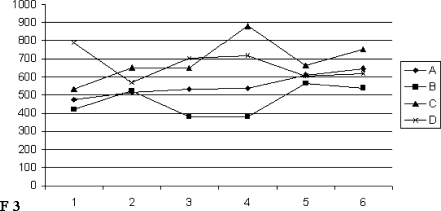
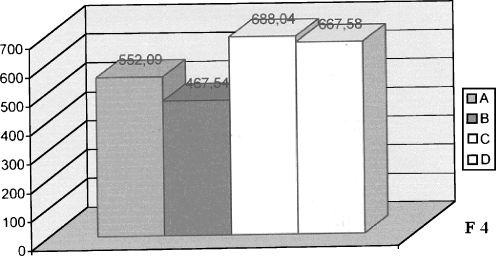
The load-deformation curves obtained from the four groups are shown in Fig. 3. Regarding the average maximum load of the groups, group C had the highest load and group D had the second highest. Group A was in the third rank, and group B had the lowest load (Fig. 4). The average maximum load (±SD) of group C (technique Δ) was 688 ± 117 N, which was significantly stronger (P < 0.03) than the ones in group A (552 ± 64 N) and group B (467 ± 82 N, P < 0.004). Group D (technique Δ with buttons) was also significantly different in strength from group A (P < 0.002) and group B (P < 0.0001), with lower values of average maximum load (667 ± 82 N). There was no significant difference either between group C and group D (P < 0.7) or between group A and group B (P < 0.08) (Table 1).
Fig. 3.
Load-deformation curves obtained from the four groups after the ACL reconstruction
Fig. 4.
Average values of groups A = 552.09, B = 467.54, C = 688.04, D = 667.58
Table 1.
Average load (N) among the four groups
| A | B | C | D | |
|---|---|---|---|---|
| Group | 552 ± 64 | 467 ± 83 | 688 ± 117 | 667 ± 82 |
| A | NS | P < 0.04 | P < 0.02 | |
| B | NS | P < 0.00 | P < 0.00 | |
| C | P < 0.04 | P < 0.00 | NS | |
| D | P < 0.02 | P < 0.00 | NS |
Group C was significantly stronger than group A and group B. Group D was also significantly different in strength from group A and group B.
Stiffness was the slope of the curve in its linear region, determined by fitting a tangential line to the load-displacement curve. As for the average stiffness of the groups, group D (22.7 ± 4 N/mm) had the highest and group C the second highest (22.2 ± 3.8 N/mm). Group B was in the third rank (18.9 ± 4.5 N/mm) and group A had the lowest value of average stiffness (17.7 ± 3 N//m). Statistical analysis showed that group C (P < 0.05) and group D (P < 0.004) were significantly stiffer than group A. There was no significant difference in average stiffness among the other groups (Table 2).
Table 2.
Average stiffness of the groups
| A | B | C | D | |
|---|---|---|---|---|
| Group | 17.7 ± 3 | 19 ± 4 | 22 ± 4 | 23 ± 4 |
| A | NS | P < 0.05 | P < 0.04 | |
| B | NS | NS | NS | |
| C | P < 0.05 | NS | NS | |
| D | P < 0.04 | NS | NS |
Group C and group D were significantly stiffer than group A. There was no significant difference in average stiffness among the other groups.
There were some characteristic mechanisms of failure in each group. Suture rupture and suture-tendon disruption in graft fixation on the tibial side was the predominant mode of failure in both groups A and B. Failure occurred on the tibial fixation site in all specimens of group A and B. The grafts of groups C and D failed by rupture of the sutures, suture-tendon disruption or slippage and tear of the tendon ends from the femoral tunnel. Interestingly, the antero-medial bundle failed first, in most of the cases, either by rupture at the tendon-suture junction on the femoral site or by stretching and slippage of the femoral end of the graft.
Discussion
This study evaluated a proposed ACL reconstruction method, using double-bundle tendons with two separate tibial tunnels, in order to reproduce the kinematics effect of both the antero-medial and postero-lateral bundle of the ACL on anterior translation of the tibia, with a more anatomical reconstruction. Structural anatomy of the porcine tibia possesses a higher trabecular bone mineral density that may lead to decreased graft slippage and increased maximum failure load compared to human tissue [14]; on the other hand, functional anatomy for porcine knees demonstrates that the range of motion is 30° to 170°, while for human knees it is 0° to 140°. An anterior displacement of the porcine tibia was performed at 60° of flexion, mimicking the anterior drawer test in human knees [21, 22]. The ACL has a three-dimensional structure consisting of collagen fibrils, which respond to various shear and torsional stresses to the knee [1, 24], while the two ACL bundles present different tension parameters. Several authors have suggested that it is very difficult for the commonly used grafts to recreate the ACL properties, and reconstruction of the ACL with two bundles presents several advantages [9, 13, 20].
In the normal ACL, each antero-medial and postero-lateral portion has a different tension pattern, and there seems to be functional cooperation between the two portions [1, 24].
Both bundles, in the proposed technique, are tied either to femoral and tibial post (25 × 6.5-mm cancellous screw) or to buttons, with the knee in 30° of flexion for the antero-medial bundle and in 100° of flexion for the postero-lateral bundle. The antero-medial bundle increases in tension beyond 60°–70° of flexion; on the other hand it decreases in the postero-lateral bundle, as the knee flexes to as much as 120°. The reconstruction method we suggest uses two tendon grafts for the antero-medial and postero-lateral bundle of ACL, respectively. The first graft tendon is positioned to the anterior border of the anatomical tibial insertion site of the ACL. The second graft is positioned 14 mm postero-lateral to the first graft to the posterior border of the tibial insertion of the ACL. The insertion site, at the tibial cortex, was common for the two tibial tunnels. The femoral tunnel was also common for the two graft tendons. We used a specially designed drill system for the tunnels. We named this reconstruction method Δ technique because when the grafts are positioned into their tunnels they present a Δ shape from lateral view. Previous studies have demonstrated that ACL in humans has a wide insertion in its tibial insertion, varying from 18 mm to 30 mm [3].
In an attempt to approach an anatomical reconstruction, we believe that the Δ technique takes advantage of the wide tibial insertion of ACL and allows simulation of functional anatomy of ACL and stability of the knee joint. We performed this technique in two groups and fixed the tendon grafts with the suture-post technique to a femoral and tibial post (25 × 6.5-mm cancellous screw) and buttons at the femoral and tibial tunnel, respectively. Furthermore, we compared the Δ technique with a single-bundle ACL reconstruction method, using two different fixation methods with femoral and tibial post and a conventional suture tied over buttons, respectively.
Regarding the maximal load, groups C and D with the Δ technique had a significantly higher value than groups A and B with the single tunnel. The normal ACL provides the primary restraint to anterior posterior movement up to 90% of the anterior force [3, 15]. As it was proved in this study, the two-bundle with a double-tunnel reconstruction technique has an advantage regarding the maximum load over a double-bundle with a single-tunnel reconstruction technique, with respect to regaining a structure that morphologically and functionally resembles more closely a normal ACL.
Stiffness is a parameter that best correlates with the clinical grading of joint laxity in clinical examination. The decrease in stiffness is considered to be one of the disadvantages of the ACL reconstruction with soft tissue grafts and tissues [2]. The greater the stiffness is, the less the displacement for a given force and the lower the laxity grade.
Regarding the stiffness, statistical analysis revealed that the groups C (<0.05) and D (<0.004) were significantly stiffer than groups A and B. Other studies also suggest that the use of a good fixation in the tibia and the femur can provide the same or higher values of average failure load or average stiffness of soft tissues in ACL reconstruction compared to bone-patellar-bone graft in ACL in human knees [8, 12, 25].
The failure modes showed that the structurally weakest site for groups A and B is located at the tendon-artificial material interface and that the dominant failure site remained at the tibial tunnel. Interestingly, the weakest site in the Δ technique was the femoral site. The failure modes showed that the antero-medial of the double-bundle tendon grafts failed in the femoral site in most of the cases. To our knowledge, this is the first study that demonstrates this fact. Other studies in porcine models or human knees have also demonstrated the tibial tunnel as the dominant failure site [12, 23, 25].
The idea of using a two-bundle reconstruction of the ACL in order to recreate its normal structure is not a new one. We are in agreement with other authors as to the fact that reconstruction of the ACL with two tendons presents several advantages [13, 17, 20]. More recent studies have suggested the reconstruction of both of the two bundles in order to reproduce the functional anatomy of the ACL, not only controlling the anterior subluxation, but also providing rotatory stability [4, 5]. The preservation of one tendon’s end insertion would secure the vascular supply and could improve the neo-ligamentisation process [17, 18].
The first limitation of this study is the use of a porcine animal model. The mechanical properties of the porcine bones and tissues are not precisely the same, but similar to those of human specimens [6]. A second limitation is that it was tested only to the anterior displacement of the tibia, which was one of the purposes of this study. The third limitation is that the biomechanical properties of ACL reconstruction were studied as they would appear immediately after surgery. It is well known that in vitro tests provide only a first order evaluation of the tested techniques.
The results of this study suggest that the femoral and tibial post as a fixation method is superior to the conventional buttons technique, while the use of double-bundle tendon grafts with two separate tibial tunnels, providing wider insertion, allows better stability of the knee joint.
In clinical relevance, the results of this study suggest that this technique recreates more closely the anterior stability of the native ACL.
Acknowledgements
This study was financially supported partly by Scientific Research Programs (no.70/4/8129) by the Greek Ministry of Education.
References
- 1.Amis AA, Dawkins GPC (1991) Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. ACL replacement with polyester fibre. J Bone Joint Surg 73-B(2):260–267 [DOI] [PubMed]
- 2.Aune AK, Ekeland A, Cawley PW (1998) Intereference screw fixation of hamstrings vs. patellar tendon grafts for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:99–102 [DOI] [PubMed]
- 3.Butler DL (1989) Anterior cruciate ligament: its normal response and replacement. J Orthop Res 7:910–921 [DOI] [PubMed]
- 4.Cha PS, Brucker PU, Weat RV, Zelle BA, Yagi M, Kurosaka M, Fu FH (2005) Arthroscopic double-bundle anterior cruciate ligament reconstruction: an anatomic approach. Arthroscopy 21:1275 [DOI] [PubMed]
- 5.Ishibashi Y, Tsuda E, Tazwa K, Sato H, Toh S (2005) Intraoperative evaluation of the anatomical double-bundle anterior cruciate ligament reconstruction with the OrthoPilot navigation system. Orthopedics 28:1277–1282 [DOI] [PubMed]
- 6.McKeon BP, Donahue BJ, Tarinelli DJ, Dalsky GP, Fulkerson JP (1999) Biomechanical evaluation of a soft-tissue interference screw in free tendon ACL graft fixation. Trans Orthop Res Soc 24:284
- 7.Maeda A, Shino K, Horibe S, Nakata K, Buccasca G (1996) Anterior cruciate ligament reconstruction with multi strand autogenous semitendinosus tendon. Am J Sports Med 24:504–509 [DOI] [PubMed]
- 8.Magen HE, Howell SM, Hull ML (1999) Structural properties of six tibial fixation methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med 27:35–43 [DOI] [PubMed]
- 9.Marcacci M, Molgora AP, Zaffagnini S, Vascellari A, Iacono F, Presti ML (2003) Anatomic double bundle anterior cruciate ligament reconstruction with hamstrings. Arthroscopy 19:540–546 [DOI] [PubMed]
- 10.Miyasaka KC, Daniel DM, Stone ML (1991) The incidence of knee ligament injuries in the general population. Am J Knee Surg 43–48
- 11.Miyata K, Yasuda K, Ishida H et al (1996) Fixation strength of the polyester tape-hamstring tendons-tape graft in anterior cruciate ligament reconstruction. Trans Orthop Res Soc 21:783
- 12.Miyata K, Yasuda K, Kondo E, Nakano H, Kimura S, Hara N (2000) Biomechanical comparisons of anterior cruciate ligament: reconstruction procedures with flexor tendon graft. J Orthop Sci 5:585–592 [DOI] [PubMed]
- 13.Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endo-buttons: operative technique and preliminary results. Arthroscopy 15:618–624 [DOI] [PubMed]
- 14.Nurmmi JT, Jarvinen TL, Kannus P et al (2002) Compaction versus extraction drilling for fixation of the hamstring tendon graft in anterior cruciate ligament reconstruction. Am J Sports Med 30:167–173 [DOI] [PubMed]
- 15.O’ Conner JJ, Zavatsky A (1993) Anterior cruciate ligament function in the normal knee. In: Arnoczky SP, Woo SL-Y, Frank CB, Simon TM (eds) The anterior cruciate ligament. Current and future conceps. Raven, New York, pp 39–52
- 16.Otero AL, Hutcheson L (1993) A comparison of the doubled semitendinosus / gracilis and central third of the patellar tendon autografts in arthroscopic anterior cruciate ligament reconstruction. Arthroscopy 9:143–148 [DOI] [PubMed]
- 17.Papachristou G, Tilentzoglou A, Efstathopoulos N, Khaldi L (1998) Reconstruction of anterior cruciate ligament using the doubled tendon technique: an experimental study in rabbits. Knee Surg Sports Traumatol Arthrosc 6:246–252 [DOI] [PubMed]
- 18.Papachristou G, Nikolaou V, Frangia K, Sourlas J, Lazarettos J, Efstathopoulos N (2005) ACL reconstruction using autologous semitendinosus tendon graft retaining the tibial insertion. Histologic study in rabbit model. Proceedings, 3rd Biomechanic Congress. IASTED, Spain
- 19.Papachristou G, Sourlas J, Magnissalis EA, Plessas Sp, Papachristou K (2006) ACL reconstruction and the implication of its tibial attachment for the stability of the joint: anthropometric and biomechanical study. Int Orthop, Aug 30 [DOI] [PMC free article] [PubMed]
- 20.Pederzini L, Adriani E, Botticella C, Tosi M (2000) Double tibial tunnel using quadriceps rendon in anterior cruciate ligament reconstruction. Arthroscopy 16:1–5 [DOI] [PubMed]
- 21.Popesko Peter (1978) Atlas of topographical anatomy of the domestic animals, 2nd edn. WB Saunders
- 22.Sacks WO (1982) Essentials of pig anatomy & Horowitz-Kramer Atlas of the musculoskeletal anatomy of the pig. Veterinary Textbooks
- 23.Scheffler SU, Sudkamp NP, Gockenjan A, Hoffman RFG, Weiler A (2002) Biomechanical comparison of hamstring and patellar tendon graft anterior cruciate ligament reconstruction techniques: the impact of fixation method under cyclic loading. Arthroscopy 18:304–315 [DOI] [PubMed]
- 24.Takai S, Woo SL-Y, Livesay GA, Adams DJ, Fu FH (1993) Determination of the in situ loads on the human anterior cruciate ligament. J Orthop Res 11:686–695 [DOI] [PubMed]
- 25.Yamanaka M, Yasuda K, Tohyama H, Nakano H, Wada T (1999) The effect of cyclic displacement on the biomechanical characteristics of ACL reconstructions. Am J Sports Med 27:772–777 [DOI] [PubMed]