Abstract
Increases of synaptically released zinc and intracellular accumulation of zinc in hippocampal neurons after traumatic or ischemic brain injury is neurotoxic and chelation of zinc has been shown to reduce neurodegeneration. Although our previous studies showed that zinc chelation in traumatically brain-injured rats correlated with an increase in whole-brain expression of several neuroprotective genes and reduced numbers of apoptotic neurons, the effect on functional outcome has not been determined, and the question of whether this treatment may actually be clinically relevant has not been answered. In the present study, we show that treatment of TBI rats with the zinc chelator calcium EDTA reduces the numbers of injured, Fluoro-Jade- positive neurons in the rat hippocampus 24 hours after injury but does not improve neurobehavioral outcome (spatial memory deficits) two weeks post-injury. Our data suggest that zinc chelation, despite providing short-term histological neuroprotection, fails to improve long-term functional outcome, perhaps because long-term disruptions in homeostatic levels of zinc adversely influence hippocampus-dependent spatial memory.
Keywords: traumatic brain injury, zinc chelation, behavioral outcome
Introduction
The morbidity and mortality associated with traumatic brain injury (TBI) have remained high despite decades of research into treatments for TBI patients [1] . The relative ineffectiveness of potential therapies in clinical trials of TBI [2] and reported increase in casualties suffering from TBI in current wars suggest an urgent need for research into alternative therapeutic options.
Although neurotoxic in high levels, zinc plays a key role in physiological growth and development and immune function; it is vital to the function of hundreds of enzymes, for the stabilization of DNA, and for gene expression [3]. Zinc also modulates synaptic transmission and synaptic plasticity [4–7].
Conversely, zinc is implicated in several pathological disorders; multiple studies have established that trauma-induced increases in extracellular concentrations of free zinc contribute to neurodegeneration in ischemic and TBI [8]. Dysregulation of intracellular free zinc concentrations has also been implicated in the pathophysiology of Alzheimer’s Disease and other neurodegenerative disorders [9]. Moreover, oxidative stress has been shown to contribute significantly to neurodegeneration in these disorders, with zinc implicated as a causal agent [10;11]. Disruption of homeostatic zinc levels has also been suggested as a link between oxidative stress and aging of the brain [12].
In cultured neurons, Canzoniero et al. [13] used Newport Green, a low affinity zinc-selective fluorescent dye, to demonstrate close correlation between increasing intracellular levels of ionic zinc and subsequent neuronal death. Stock et al. recently provided compelling evidence that many probes considered to be calcium-specific actually have higher affinity levels for zinc, suggesting that apparent calcium overload reported after experimental brain insults may be due to binding of these dyes to excessive levels of injury-induced concentrations of free zinc [14].
Evidence supporting the involvement of excessive levels of ionic zinc in neuronal death after brain injury is primarily inferred from observations that zinc chelating agents are neuroprotective both against direct zinc toxicity in cell culture and in various models of ischemia and TBI [8;15–17]. In rats and gerbils subjected to cerebral ischemic insults, Calderone et al. [17] showed that even late (48–60 hr post-ischemia) chelation of zinc with CaEDTA, a membrane-impermeant chelator, reduced cell death in CA1 hippocampal neurons. We reported that CaEDTA, injected intracerebroventricularly pre-TBI, reduced neuronal injury and increased neuroprotective gene expression [18]. We then questioned whether this treatment would affect neurobehavioral outcome. Thus, we designed the following study a) to confirm the protective effect of CaEDTA treatment in TBI, by determining numbers of injured, Fluoro-Jade-positive neurons in rat hippocampus 24 hours after injury [19]; and b) to determine if CaEDTA treatment improves neurobehavioral outcome after TBI.
Materials and Methods
Adult, male, Sprague-Dawley rats, 400 g to 500 g, were anesthetized with 4% isoflurane, intubated and mechanically ventilated with 1.5 – 2.0% isoflurane in room air:oxygen (80:20). For animals surviving longer than 24 hours, the right common jugular vein was sterilely cannulated for intravenous fluid administration. The tail artery was cannulated for arterial blood gas measurement and mean arterial pressure (MAP) monitoring. Protocol for moderate (2.0 atm) fluid percussion brain injury was performed as described elsewhere [20–22]. Based on preliminary dose-response results that concurred with the study by Calderone et al. [17], we used 300 mM CaEDTA for assessment of neuronal injury 24 hours after TBI. The 24-hour survival group was subdivided into three groups: eight rats received an intracerebroventricular (icv) injection of 0.9% saline 30 minutes pre-TBI; eight rats received 300 mM CaEDTA icv 30 minutes pre-TBI; and eight rats received 300 mM CaEDTA icv 30 minutes post-TBI.
We previously determined that a moderate injury (2.0 atm) did not produce a functional deficit that sufficiently discriminated TBI from sham-operated rats in the Morris water maze (MWM) test. Thus, rats prepared for MWM testing were subjected to a severe fluid percussion injury (2.4 atm), which we found produced significant deficits in spatial memory in TBI rats. For MWM testing, six rats received 0.9% saline icv and sham TBI (control), six rats received 0.9% saline icv 30 min pre-TBI, six animals received 300 mM CaEDTA icv 30 min pre-Sham TBI and six received 300 mM CaEDTA icv 30 minutes pre-TBI. These animals completed MWM testing on days 11–15 and then were sacrificed.
Spatial memory function was assessed using MWM testing [23;24]. On post-injury days 11 through 15, rats were tested on four trials each day. The water maze is a 6-foot-diameter tank, filled to 2 cm above a submerged, transparent platform that is 4 inches in diameter and 26 cm in height. The water temperature is held at 26 to 27°C. The platform is stationary throughout all trials on all days. The tank is divided into four quadrants and stationary cues are marked on the wall in each quadrant. The animals’ starting points are randomly chosen daily and one trial per day is started in each quadrant. After placing the animal in the water facing the wall of the tank, the handler leaves the room. The animal is allowed two minutes to find and climb the platform and escape the water. He must then remain on the platform for 30 seconds. If the animal does not find it, the handler places him on the platform for 30 seconds before removing him from the maze. The animals are given a four-minute resting period in a warming chamber between each trial. A computer system using proprietary SMART™ software (San Diego Instruments, San Diego, CA) is used to record the animals’ path length and latency to find the platform during each trial.
For assessment of neuronal injury and gene expression analysis of apoptosis-related genes by quantitative real-time polymerase chain reaction (PCR), frozen 10 µm coronal sections of rat brains were cut on a cryostat and mounted on uncoated glass slides (Fisher Scientific, Pittsburgh, PA). Once the injury site in the hippocampus of the brain was reached, near Bregma −3.15 mm, 10 µm sections were taken every 15th section for 10 slides. The first section was mounted on a precleaned superfrost slide which was then used for LCM (laser capture microdissection). The next section was mounted on superfrost-plus slides and was used for counting. This pattern was continued through the hippocampus until approximately Bregma −4.65 mm. The slides were preserved at −20°C until sectioning was complete. Immediately after sectioning, the frozen sections mounted on the superfrost slides for LCM were thawed at room temperature for 30 sec and fixed for one minute with 75% ethanol. After fixation, the slides were briefly rinsed in RNase-free water (1 min), stained with 1% cresyl violet (1 min), rinsed in RNase-free water (1 min ×3), dehydrated in 95% ethanol (30 sec ×2), 100% ethanol (30 sec ×2) and xylene (3 min ×2), air-dried for 10 to 15 min in a hood, and stored desiccated for no more than 1 h at room temperature before LCM. All solutions were prepared with RNase-free water, and the cresyl violet was sterilely filtered just before use.
Every 15th (10 µm) coronal section through the injury site (10 sections per brain) was collected, dehydrated in graded alcohols, stained with 0.001% Fluoro-Jade for four minutes, counterstained with 1% cresyl violet and counted as described in Hellmich et al. [19].
LCM was performed using a PixCell IIe laser capture microscope with an infrared diode laser (Arcturus Engineering, Mountain View, CA). The CA3 region from the injured, ipsilateral side of the hippocampus was captured on the thermoplastic films of a CapSure LCM Cap (Arcturus Engineering, Mountain View, CA). The smallest laser spot size (7.5 µm) was used with a power setting of 90 mW and a duration of 0.8 ms. However, these settings were adjusted frequently throughout the laser capture process to optimize capture of neurons. The caps were subsequently placed tightly on 0.5 ml microfuge tubes (RNase-free) filled with lysis solution (100 µl/LCM sample) from RNAqueous-Micro kit (Ambion Inc. Austin, TX) containing guanidine thiocyanate. Each tube was vortexed and heated to 42°C for 30 min to increase the yield of RNA. The tube was spun down and the RNA sample in lysis buffer was transferred to a new RNase-free tube. Tubes were stored at −80°C for up to one week and the RNA was then extracted by using the RNAqueous-Micro kit (Ambion Inc. Austin, TX). After the RNA samples were DNAse treated, they were used directly for quantitative real-time PCR analysis.
Quantitative real-time PCR was performed on a Strategene MX3000 (La Jolla, CA), and all the Taqman reagents were ordered from Applied Biosystems (Foster City, CA). The reverse transcriptase (RT) reactions using total RNA from approximately 200 neurons acquired by LCM were performed with reagents and the recommended protocol from the Taqman Reverse Transcriptase Reagents kit (cat# N808-0234), and for the PCR the AmpliTaq Gold with Gene Amp kit was used (cat# N808-0248 buffer and Taq). The probe, forward primers and reverse primers for all genes tested were designed using BioRad (Hercules, CA) Beacon Designer (cat# 1708734). The probes were labeled by Integrated DNA Technologies (Coraville, IA) with the recommended 5’dyes (FAM, Cy5, HEX or ROX) and the 3’ quenchers (Tamra NHS Ester-Sp or Iowa Black). One reverse transcriptase reaction was completed for each DNase-treated LCM RNA sample.
The real-time PCR reactions were performed using 1 µl of the RT produced from the above procedure for each 25 µl PCR reaction. The PCR was performed as follows: 2.5 µl of the 10× buffer (containing 15 mM MgCl2 from the AmpliTaq Gold with Gene Amp kit cat# N808-0248), 4 µl of 25 mM MgCl2, 2.2 µl of 10 mM dNTPs (for 2- and 3-gene multiplexing sets), 0.1 µl forward and reverse primers at 25 to 75 µM (100–300 nM in final concentration), 0.1 µl of taqman dual labeled probe from IDT at 12.5 to 25 µM (50–100 nM in final concentration), and 0.125 µl of ampliTaq gold cat # N808-0248 (0.25 µl were used for a 2-gene multiplexing set and 0.375 for a 3-gene set). The final volume of the reaction was brought to 25 µl with nuclease-free water. This reaction is used for a single well in a 96-well plate. The Thermal Profile setup used for the PCR reaction was one cycle for two minutes at 50°C, then one cycle for ten minutes at 95°C, and a two-step PCR with 50 cycles each for 15 seconds at 95°C and one minute at 60°C. Each PCR reaction was performed in triplicate and standard curves were performed in triplicate for each primer and probe set and every multiplexing set using 1 µl of a 1:10 serial dilution of a 1 µg RT reaction. Standard curve points were tested with five points from 20 ng to 2 pg of input RNA per PCR reaction. Every multiplexing set has a standard curve containing at least four of the five points (detection threshold of 20 pg) with an efficiency of 90% to 110% and with an r-square value above 0.98. Every experiment contains a no template-negative control and a no RT-negative control at which the Ct values must always be at least 5 Ct values below the lowest experimental value for that specific gene. We used GAPDH as our normalizing gene for all PCRs. Probe and primer sequences were as follows: Bax, accession number NM_017059, forward primer 5’- CCCACCAGCTCTGAACAGTTC-3’, reverse primer 5’- ACACTCGCTCAGCTTCTTGG-3’; Cy5 labeled probe 5’- CATCCTGGGGCGGCT GCTCC AA-3’, Bcl-2, accession number L14680, forward primer 5’- GATGACTTCTCTCGTCGCTACC-3’, reverse primer 5’- ACCCCATCCCTGAAGAGTTCC-3’; Fam labeled probe 5’- ACCGTGGCAAAGCGTCCCCTCG-3’; caspase 3, accession number NM_012922.1, forward primer 5’- GCCGAAACTCTTCATCATTCAGG-3’, reverse primer 5’- CATATCATCGTCAGTTCCACTGTC-3’; Rox labeled probe 5’- ACCGCAGTCCAGCTCTGTACCTCG-3’; Glyceraldehyde-3-phosphate dehydrogenase, accession number NM_017008, forward primer 5’- AAGCTGGTCATCAATGGGAAAC-3’, reverse primer 5’- GAAGACGCCAGTAGACTCCACG-3’; and Hex labeled probe 5’- ATCTTCCAGGAGCGCGATCCCG-3’.
Analysis of variance or covariance of numbers of injured neurons were performed using StatView 5.0 (SAS Institute, Cary, NC). Differences in these groups were analyzed using Fisher’s protected least significant difference (PLSD) test with p<0.05 considered significant. Due to heterogeneous variances among treatment groups, real-time PCR data were assessed using the Kruskal-Wallis test at the 0.05 level of significance. Data analysis was conducted using SAS®, Release 9.1 [25]. Latency in the MWM tests was analyzed using analysis of variance for a three-factor experiment with repeated measures on time. The three factors were TBI (severe TBI and no TBI), CaEDTA (present and absent) and day (days 11–15). The first-order autoregressive covariance was used for a covariance structure. Main effects were assessed at the 0.05 and interactions of the effects were assessed at the 0.15 levels of significance as the experiment-wise error rates. Fisher’s least significant difference procedure was used for multiple comparisons with 0.005 as the comparison-wise error rate. Data analysis was conducted using PROC MIXED with LSMEANS option and Satterthwaite approximation for the denominator degrees of freedom in SAS®, Release 9.1 [25].
Results
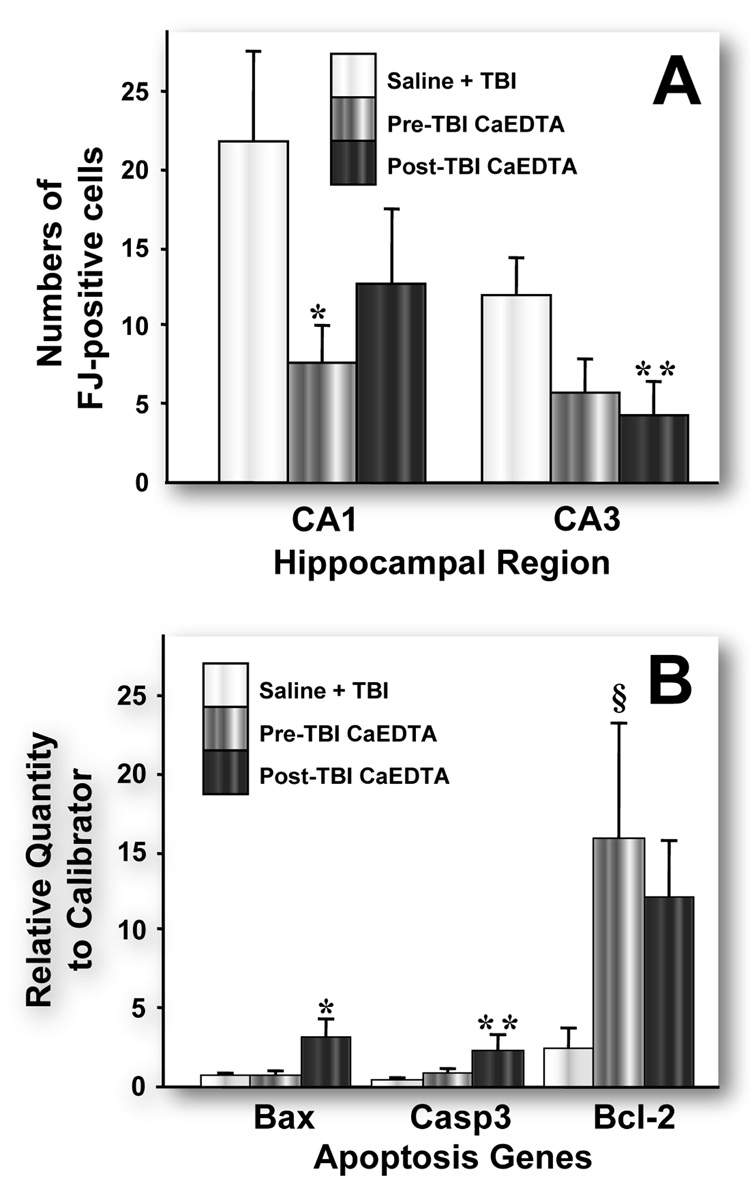
We found a significant decrease in numbers of injured, Fluoro-Jade-positive neurons in the CA1 hippocampal subfield (p<0.05) of rats pretreated with 300 µM CaEDTA compared with saline-treated TBI rats (Fig. 1A). In post-treated rats, numbers of injured, Fluoro-Jade-positive neurons were significantly reduced in the CA3 subfield compared with saline-injected TBI animals (p<0.02).
Figure 1.
A. Effects of pre- and post-TBI CaEDTA treatment on numbers of injured, Fluoro-Jade (F–J) positive neurons in rat hippocampus. Average numbers of F–J-positive neurons in the CA1 and CA3 subfields from CaEDTA treated TBI rats are compared with F–J positive neurons from saline injected TBI rats (n=8 per group). Error bars represent SEM. * p<0.05, ** p<0.02. B. Effects of pre and post-TBI CaEDTA treatment on injury-induced gene expression. Bax expression was higher in post-TBI CaEDTA treated rats, * p<0.05 compared with saline and pre-treated rats. Caspase 3 expression was higher in post-TBI CaEDTA treated rats, ** p<0.05 compared with saline treated rats only. Bcl-2 expression was higher in pre-TBI CaEDTA treated rats, § p<0.05 compared with saline treated rats. Error bars represent SEM.
Despite a clear reduction in the numbers of injured hippocampal neurons, we found few differences in injury-induced gene expression. For quantitative gene expression analysis, we chose a select group of apoptosis-related genes whose expression has been shown to be altered by TBI in our laboratory. Expression of the anti-apoptotic gene Bcl-2 was significantly greater in rats treated with CaEDTA before TBI than in saline-injected TBI rats (Fig. 1B). No other significant differences existed in Bcl-2 expression between the other groups, although Bcl-2 expression was higher in both CaEDTA-treated (pre-TBI and post-TBI) compared with untreated TBI rats. Expression of the pro-apoptotic gene Bax in rats treated with CaEDTA post-injury was significantly greater than in TBI rats pretreated with CaEDTA and TBI rats with injected with saline. Similarly, expression of caspase 3 in post-TBI rats treated with CaEDTA was significantly greater than in TBI rats injected with saline, but was not significantly different from pre-injury rats treated with CaEDTA. Caspase 3 expression was not different in saline and pre-injury injection TBI groups.
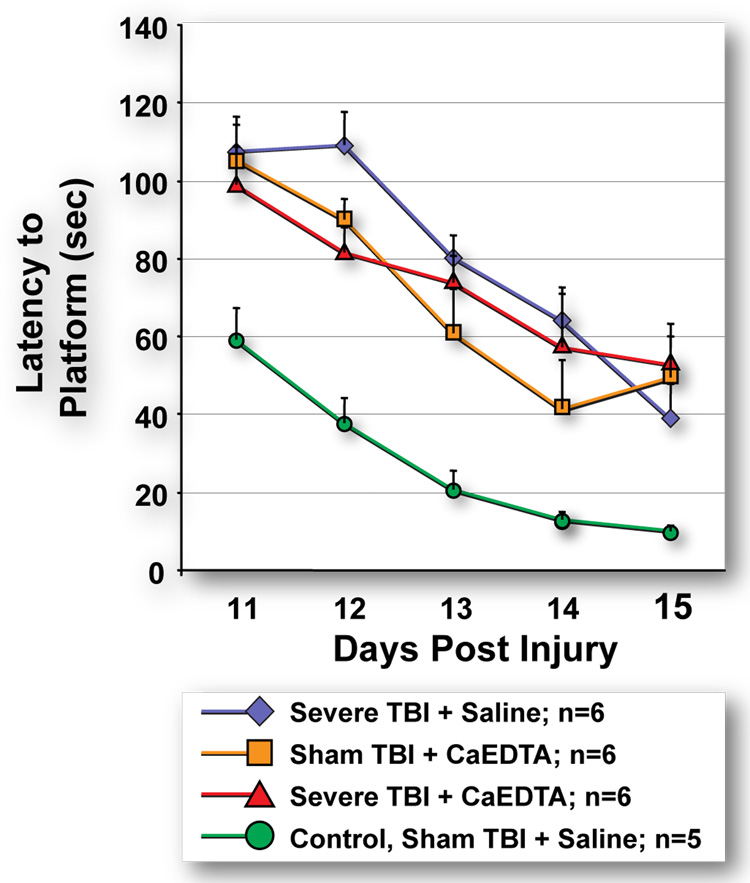
Despite clear reductions in acutely injured neurons associated with CaEDTA treatment, we observed no beneficial effect of CaEDTA treatment on neurobehavioral outcome after TBI (Fig. 2). More surprisingly, CaEDTA treatment of sham-operated controls reduced MWM performance compared with untreated sham-operated control rats. When compared with the untreated sham-operated control group (no TBI + no CaEDTA), mean latencies of three groups (severe TBI + CaEDTA, severe TBI + saline, and sham TBI + CaEDTA) were significantly greater than the control group from days 11 to 15 but were not statistically significantly different from each other.
Figure 2.
Assessment of spatial memory deficits using Morris Water Maze. CaEDTA treatment does not improve spatial memory in TBI rats and CaEDTA-treated sham-operated rats have pronounced spatial memory deficits which are not significantly different from TBI rats with and without CaEDTA treatment. Error bars represent SEM.
Discussion
The acute neuroprotective effect of CaEDTA treatment in experimental brain injury has been reported by various groups [8;15;18;26;27]. The primary goals of our study were to determine if this protective effect could be correlated with a significant decrease in neuronal injury and concomitant changes in expression of known apoptosis-related genes, Bax, caspase 3 and Bcl-2, and to determine if acute CaEDTA treatment had a beneficial effect on neurobehavioral outcome. To date, there are no reports of the long-term influence of CaEDTA treatment on functional outcome after TBI. Thus, we sought to determine the effect of zinc chelation on spatial memory deficits after TBI. Zinc chelation therapy has also been proposed for the treatment of other neurodegenerative disorders; since zinc has been implicated as a causative agent in the oxidative stress that contributes to neurodegeneration in Alzheimer’s disease [28], chelation of zinc with clioquinol has been proposed as a therapeutic treatment for Alzheimer’s disease patients [29].
We recently showed that we can quantify the severity of hippocampal neuronal injury by counting the numbers of degenerating Fluoro-Jade-positive neurons in the rat hippocampal subfields after TBI [19]. In a subsequent study [30], we found that the distribution and numbers of injured, Fluoro-Jade-positive neurons were similar to that of zinc-positive neurons after TBI, thus providing evidence that excessive accumulation of zinc in neurons contributed to cell death. Lavoie et al. [31] also showed a strong correlation between dying, TUNEL-positive neurons and zinc-positive neurons (stained with the high-affinity zinc dye TSQ) in the hippocampus following kainic acid-induced seizures.
Here, we have presented data that are consistent with previous studies: CaEDTA treatment significantly reduced the numbers of injured neurons in rat the hippocampus 24 hours after TBI. However, our studies also show that manipulating excess TBI-induced zinc levels by chelation treatment did not positively influence long-term functional outcome after TBI. Unexpectedly, we found that CaEDTA treatment of control rats actually worsened spatial memory performance in the MWM test, making their latencies comparable to both injured, untreated rats and TBI rats treated with CaEDTA and significantly exceeding those of sham controls. This may occur because zinc-chelating agents dysregulate homeostatic zinc levels that are critical for normal physiological function [3;7]. Daumas et al. [32] also showed that infusion of CaEDTA into the CA3 region of the hippocampus impaired episodic-like memory in mice. Due to zinc’s importance in the make-up of many vital proteins, prolonged reductions of intracellular zinc levels could have important adverse consequences, including impaired response to stress, affective depression and other neurodegenerative diseases [33–35].
One of the limitations of our study is that CaEDTA is a highly potent zinc chelator that also exerts local osmotic effects. Even though CaEDTA is a cell-impermeant chelator, there is some evidence that high extracellular levels can reduce intracellular zinc levels [36]. Lavoie et al. suggested that osmotic imbalances caused by high (100–300 mM) levels of intraventricularly injected CaEDTA may have permeabilized the cells that would allow the chelator to further deplete intracellular levels of zinc [31]. Because zinc chelators differ in the avidity with which they deplete zinc, we suspect that it may be prudent to study zinc chelators that bind zinc less avidly than CaEDTA. Canzoniero et al. reported that direct zinc toxicity in neuronal cultures was attenuated by both the high-affinity zinc chelator, TPEN, and the lower affinity chelator pyrithione; however, TPEN was intrinsically neurotoxic whereas the lower affinity chelator was nontoxic [16].
The pro- and anti-apoptotic gene expression data at first appear contradictory. There was increased expression of the anti-apoptotic gene Bcl-2 after TBI, but concurrently there were increases in expression of Bax and caspase 3, two pro-apoptotic genes. It is possible that neuronal survival requires a favorable balance between the expression of pro-survival and pro-apoptotic genes and that the increases in Bax and caspase 3 were more than compensated by significant increases in expression of Bcl-2. In a previous study [37] we found that neuronal survival correlated with up-regulation of neuroprotective genes but not with changes in expression of apoptosis-related genes. Further studies are required to enhance our understanding of the correlation between TBI-induced gene expression, neurodegeneration, neuronal survival and neurobehavioral outcome.
Acknowledgments
This study was supported in part by National Institutes of Health grant 1R01 NS042849-01A1 (Dr. Donald S. Prough). We thank Andrew Hall, Jeffrey Meserve and Laurie Bolding for their editorial assistance and Christy Perry for assistance with the figures.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21:544–548. doi: 10.1097/00001199-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Cernak I. Recent advances in neuroprotection for treating traumatic brain injury. Expert. Opin Investig. Drugs. 2006;15:1371–1381. doi: 10.1517/13543784.15.11.1371. [DOI] [PubMed] [Google Scholar]
- 3.Frassinetti S, Bronzetti G, Caltavuturo L, Cini M, Croce CD. The role of zinc in life: a review. J Environ Pathol. Toxicol. Oncol. 2006;25:597–610. doi: 10.1615/jenvironpatholtoxicoloncol.v25.i3.40. [DOI] [PubMed] [Google Scholar]
- 4.Lin DD, Cohen AS, Coulter DA. Zinc-induced augmentation of excitatory synaptic currents and glutamate receptor responses in hippocampal CA3 neurons. J Neurophysiol. 2001;85:1185–1196. doi: 10.1152/jn.2001.85.3.1185. [DOI] [PubMed] [Google Scholar]
- 5.Molnar P, Nadler JV. Synaptically-released zinc inhibits N-methyl-D-aspartate receptor activation at recurrent mossy fiber synapses. Brain Res. 2001;910:205–207. doi: 10.1016/s0006-8993(01)02720-2. [DOI] [PubMed] [Google Scholar]
- 6.Ruiz A, Walker MC, Fabian-Fine R, Kullmann DM. Endogenous zinc inhibits GABA(A) receptors in a hippocampal pathway. J Neurophysiol. 2004;91:1091–1096. doi: 10.1152/jn.00755.2003. [DOI] [PubMed] [Google Scholar]
- 7.Hirzel K, Muller U, Latal AT, Hulsmann S, Grudzinska J, Seeliger MW, Betz H, Laube B. Hyperekplexia Phenotype of Glycine Receptor alpha1 Subunit Mutant Mice Identifies Zn(2+) as an Essential Endogenous Modulator of Glycinergic Neurotransmission. Neuron. 2006;52:679–690. doi: 10.1016/j.neuron.2006.09.035. [DOI] [PubMed] [Google Scholar]
- 8.Choi DW, Koh JY. Zinc and brain injury. Annu. Rev. Neurosci. 1998;21:347–375. doi: 10.1146/annurev.neuro.21.1.347. [DOI] [PubMed] [Google Scholar]
- 9.Mocchegiani E, Bertoni-Freddari C, Marcellini F, Malavolta M. Brain, aging and neurodegeneration: role of zinc ion availability. Prog Neurobiol. 2005;75:367–390. doi: 10.1016/j.pneurobio.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Barnham KJ, Masters CL, Bush AI. Neurodegenerative diseases and oxidative stress. Nat Rev Drug Discov. 2004;3:205–214. doi: 10.1038/nrd1330. [DOI] [PubMed] [Google Scholar]
- 11.White AR, Barnham KJ, Bush AI. Metal homeostasis in Alzheimer's disease. Expert. Rev Neurother. 2006;6:711–722. doi: 10.1586/14737175.6.5.711. [DOI] [PubMed] [Google Scholar]
- 12.Frazzini V, Rockabrand E, Mocchegiani E, Sensi SL. Oxidative stress and brain aging: is zinc the link? Biogerontology. 2006;7:307–314. doi: 10.1007/s10522-006-9045-7. [DOI] [PubMed] [Google Scholar]
- 13.Canzoniero LMT, Turetsky DM, Choi DW. Measurement of intracellular free zinc concentrations accompanying zinc-induced neuronal death. J. Neurosci. 1999;19:1–6. doi: 10.1523/JNEUROSCI.19-19-j0005.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stork CJ, Li YV. Intracellular zinc elevation measured with a "calcium-specific" indicator during ischemia and reperfusion in rat hippocampus: a question on calcium overload. J Neurosci. 2006;26:10430–10437. doi: 10.1523/JNEUROSCI.1588-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suh SW, Chen JW, Motamedi M, Bell B, Listiak K, Pons NF, Danscher G, Frederickson CJ. Evidence that synaptically-released zinc contributes to neuronal injury after traumatic brain injury. Brain Res. 2000;852:268–273. doi: 10.1016/s0006-8993(99)02095-8. [DOI] [PubMed] [Google Scholar]
- 16.Canzoniero LM, Manzerra P, Sheline CT, Choi DW. Membrane-permeant chelators can attenuate Zn2+-induced cortical neuronal death. Neuropharmacology. 2003;45:420–428. doi: 10.1016/s0028-3908(03)00171-0. [DOI] [PubMed] [Google Scholar]
- 17.Calderone A, Jover T, Mashiko T, Noh KM, Tanaka H, Bennett MV, Zukin RS. Late calcium EDTA rescues hippocampal CA1 neurons from global ischemia-induced death. J Neurosci. 2004;24:9903–9913. doi: 10.1523/JNEUROSCI.1713-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hellmich HL, Frederickson CJ, DeWitt DS, Saban R, Parsley MO, Stephenson R, Velasco M, Uchida T, Shimamura M, Prough DS. Protective effects of zinc chelation in traumatic brain injury correlate with upregulation of neuroprotective genes in rat brain. Neurosci Lett. 2004;355:221–225. doi: 10.1016/j.neulet.2003.10.074. [DOI] [PubMed] [Google Scholar]
- 19.Hellmich HL, Capra B, Eidson K, Garcia J, Kennedy D, Uchida T, Parsley M, Cowart J, DeWitt DS, Prough DS. Dose-dependent neuronal injury after traumatic brain injury. Brain Res. 2005;1044:144–154. doi: 10.1016/j.brainres.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 20.Dixon CE, Lyeth BG, Povlishock JT, Findling RL, Hamm RJ, Marmarou A, Young HF, Hayes RL. A fluid percussion model of experimental brain injury in the rat. J. Neurosurg. 1987;67:110–119. doi: 10.3171/jns.1987.67.1.0110. [DOI] [PubMed] [Google Scholar]
- 21.Mathew BP, DeWitt DS, Bryan RM, Jr, Bukoski RD, Prough DS. Traumatic brain injury reduces myogenic responses in pressurized rodent middle cerebral arteries. J. Neurotrauma. 1999;16:1177–1186. doi: 10.1089/neu.1999.16.1177. [DOI] [PubMed] [Google Scholar]
- 22.Shimamura M, Garcia JM, Prough DS, Hellmich HL. Laser capture microdissection and analysis of amplified antisense RNA from distinct cell populations of the young and aged rat brain: effect of traumatic brain injury on hippocampal gene expression. Mol Brain Res. 2004;17:47–61. doi: 10.1016/j.molbrainres.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 23.Hamm RJ, Temple MD, Pike BR, O'Dell DM, Buck DL, Lyeth BG. Working memory deficits following traumatic brain injury in the rat. J Neurotrauma. 1996;13:317–323. doi: 10.1089/neu.1996.13.317. [DOI] [PubMed] [Google Scholar]
- 24.Morris RG, Garrud P, Rawlins JN, O'Keefe J. Place navigation impaired in rats with hippocampal lesions. Nature. 1982;297:681–683. doi: 10.1038/297681a0. [DOI] [PubMed] [Google Scholar]
- 25.SAS/STAT® 9.1 User's Guide. Cary, NC: SAS Institute; 2004. [Google Scholar]
- 26.Lee JM, Zipfel GJ, Choi DW. The changing landscape of ischaemic brain injury mechanisms. Nature. 1999;399:A7–A14. doi: 10.1038/399a007. [DOI] [PubMed] [Google Scholar]
- 27.Koh JY. Zinc and disease of the brain. Mol. Neurobiol. 2001;24:99–106. doi: 10.1385/MN:24:1-3:099. [DOI] [PubMed] [Google Scholar]
- 28.Cherny RA, Atwood CS, Xilinas ME, Gray DN, Jones WD, McLean CA, Barnham KJ, Volitakis I, Fraser FW, Kim Y, Huang X, Goldstein LE, Moir RD, Lim JT, Beyreuther K, Zheng H, Tanzi RE, Masters CL, Bush AI. Treatment with a Copper-Zinc Chelator Markedly and Rapidly Inhibits beta-Amyloid Accumulation in Alzheimer's Disease Transgenic Mice. Neuron. 2001;30:665–676. doi: 10.1016/s0896-6273(01)00317-8. [DOI] [PubMed] [Google Scholar]
- 29.Cuajungco MP, Faget KY, Huang X, Tanzi RE, Bush AI. Metal chelation as a potential therapy for Alzheimer's disease. Ann. N. Y. Acad. Sci. 2000;920:292–304. doi: 10.1111/j.1749-6632.2000.tb06938.x. [DOI] [PubMed] [Google Scholar]
- 30.Hellmich HL, Eidson KA, Capra BA, Garcia JM, Boone DR, Hawkins BE, Uchida T, DeWitt DS, Prough DS. Injured Fluoro-Jade-positive hippocampal neurons contain high levels of zinc after traumatic brain injury. Brain Res. 2006;1127:119–126. doi: 10.1016/j.brainres.2006.09.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lavoie N, Peralta MR, III, Chiasson M, Lafortune K, Pellegrini L, Seress L, Toth K. Extracellular chelation of zinc does not affect hippocampal excitability and seizure-induced cell death. J Physiol. 2007;578:275–289. doi: 10.1113/jphysiol.2006.121848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daumas S, Halley H, Lassalle JM. Disruption of hippocampal CA3 network: effects on episodic-like memory processing in C57BL/6J mice. Eur J Neurosci. 2004;20:597–600. doi: 10.1111/j.1460-9568.2004.03484.x. [DOI] [PubMed] [Google Scholar]
- 33.Hao Q, Maret W. Imbalance between pro-oxidant and pro-antioxidant functions of zinc in disease. J Alzheimers Dis. 2005;8:161–170. doi: 10.3233/jad-2005-8209. [DOI] [PubMed] [Google Scholar]
- 34.Bodnar LM, Wisner KL. Nutrition and depression: implications for improving mental health among childbearing-aged women. Biol Psychiatry. 2005;58:679–685. doi: 10.1016/j.biopsych.2005.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen WQ, Cheng YY, Zhao XL, Li ST, Hou Y, Hong Y. Effects of zinc on the induction of metallothionein isoforms in hippocampus in stress rats. Exp Biol Med (Maywood. ) 2006;231:1564–1568. doi: 10.1177/153537020623100917. [DOI] [PubMed] [Google Scholar]
- 36.Frederickson CJ, Suh SW, Koh JY, Cha YK, Thompson RB, LaBuda CJ, Balaji RV, Cuajungco MP. Depletion of intracellular zinc from neurons by use of an extracellular chelator in vivo and in vitro. J Histochem. Cytochem. 2002;50:1659–1662. doi: 10.1177/002215540205001210. [DOI] [PubMed] [Google Scholar]
- 37.Hellmich HL, Garcia JM, Shimamura M, Shah SA, Avila MA, Uchida T, Parsley MA, Capra BA, Eidson KA, Kennedy DR, Winston JH, DeWitt DS, Prough DS. Traumatic brain injury and hemorrhagic hypotension suppress neuroprotective gene expression in injured hippocampal neurons. Anesthesiology. 2005;102:806–814. doi: 10.1097/00000542-200504000-00017. [DOI] [PubMed] [Google Scholar]