Exercise and physical activity are important to a child’s overall health and well-being. But like all children, young athletes can become ill from a variety of infections. Infection in young athletes can produce a significant dilemma, not only for the athletes, but also for the coaches and physicians because the illnesses may affect the athlete’s ability to train and compete. Is it safe for athletes with infections to continue to exercise?
CASE EXAMPLE
A 15-year-old basketball player presents with a one-week history of fatigue, sore throat, fever and swollen glands. On examination, he has a temperature of 39°C, exudative pharyngitis and bilateral cervical lymphadenopathy. Investigations include a throat swab, which is negative for group A streptococcus; a complete blood count which reveals a white blood cell count of 16×109/L with atypical lymphocytosis; and a Monospot, which is positive. You make the diagnosis of infectious mononucleosis (IM). The patient wants to know whether he can play in the city-wide basketball tournament this weekend. What do you tell him?
EXERCISE AND THE IMMUNE SYSTEM
This is an active area of research. During exercise, many physiological changes occur in the body, including the immune system. Exercise can affect the quantity and activity of the immune system (1–4). Quantitative changes include increases in neutrophils and lymphocytes because adrenaline levels rise during exercise. The neutrophil counts rise further but lymphocyte counts diminish because cortisol levels rise more steadily with continued exercise and remain elevated for longer periods following exercise. The ratio of CD4 (helper T) to CD8 (suppressor T) cells also decreases, which may contribute to infection susceptibility. The salivary immunoglobulin A concentration is suppressed with short-term exercise, and may even be diminished below baseline with long-term, high-intensity exercise (1–4).
Functional changes in the immune system with exercise include diminished neutrophil chemotaxis and phagocytosis with high-intensity endurance training. Natural killer cell activity increases with exercise and returns to baseline during recovery. These changes in the immune system, resulting in a brief period of immunosuppression after intense exercise, is referred to as the immunological ‘open window’ (2,3). This period of reduced immune function raises concerns regarding an athlete’s ability to fight off an infection during recovery following intense exercise.
ARE ATHLETES MORE SUSCEPTIBLE TO INFECTION?
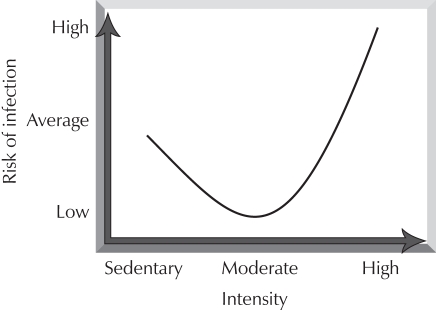
Research shows that the relationship between the amount of exercise and incidence of infection forms a ‘J’ curve (Figure 1) (2,3). It is believed that people who exercise at a moderate level have enhanced immune function and may experience fewer illnesses and shorter duration of illness, such as upper respiratory tract infections, compared with those who do not exercise at all (2,3). However, there is evidence to suggest that elite athletes training at high levels may be at greater risk of these infections. Research indicates that marathon runners have more upper respiratory tract infections during periods when mileage is increased and in the two weeks following a marathon run (2,3). Athletes also report that they have more infections during periods when they train more intensely, as well as during and after major competitions. This may be due, in part, to effects on the immune system, but may also be related to other factors, such as psychological stress, inadequate recovery time and fatigue (2). It is also recognized that exercising during an infectious illness may exacerbate symptoms, prolong the length of illness and increase the risk of potentially serious complications such as myocarditis (1,4,5).
Figure 1.
The J-curve hypothesis for training intensity and risk of infection. Reproduced with permission from reference 3
Infections causing fever can be detrimental to athletes. Fever affects the body’s ability to regulate body temperature and increases insensible fluid losses (1,5). These effects are compounded if an athlete is exercising in a hot climate, and can put athletes at greater risk of heat injury (heat stroke and heat exhaustion) and dehydration if they exercise with a fever (1,5). In addition, febrile illnesses have been shown to decrease muscle strength and endurance, reduce exercise tolerance and increase fatigue; thus, any benefits obtained by exercising during a fever are questionable (1,5).
SHOULD AN ATHLETE WITH AN INFECTION RETURN TO PLAY?
This can be a tricky issue, particularly at critical moments during an athlete’s competitive season. In general, decisions about whether to continue exercising during an illness can be made using a ‘neck check’ (3–5). If symptoms are confined to above the neck, such as a runny nose, nasal congestion or sore throat, athletes may continue to participate as long as they feel able. An infected athlete should attempt to exercise at mild to moderate intensity for 10 min to 15 min; if symptoms worsen, the athlete should stop and rest. If symptoms do not worsen, the athlete can continue to participate (3–5).
If an athlete has systemic symptoms, however, such as fever, myalgias, diarrhea or an elevated resting heart rate, they should refrain from exercising until symptoms have resolved for a period of seven to 14 days, because of the risk of dehydration, prolonged illness or more serious complications. Once recovered, athletes should ease back into sports gradually, taking one to two days for every training day missed to build back up to preillness levels (3–5).
Another issue to consider when athletes have an infection is the contagiousness of the illness. If participation imparts a risk to teammates or other people involved in the sport, the athlete should not participate until they have fully recovered (5).
Specific illnesses such as IM require special considerations. Splenomegaly associated with IM results from lymphocytic infiltration, which distorts the splenic architecture, making the spleen fragile and prone to rupture. Physical examination alone is notoriously unreliable for detecting splenomegaly (6). Although one series (6) demonstrated that the spleen was palpably enlarged in only 17% of patients, 100% of patients had an enlarged spleen demonstrated by ultrasound. Therefore, it should be assumed that any patient with IM has splenomegaly. Ultrasound is the test of choice to determine spleen size.
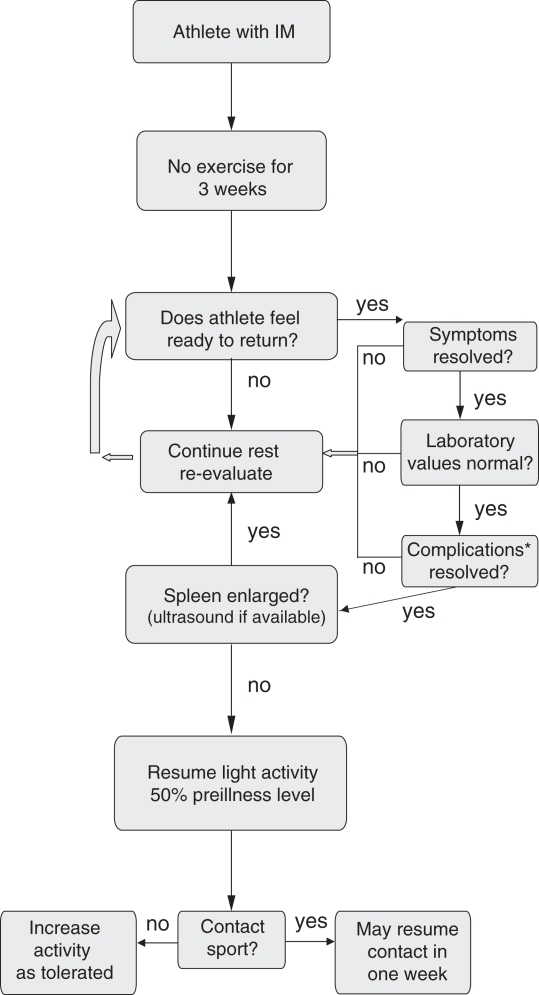
Splenic rupture is the single most important complication of IM in the athletic population, particularly those participating in contact sports (7,8). The risk of splenic rupture, which is often spontaneous, is approximately 0.1% to 0.5% and is highest in the first three weeks of illness (day four to 21). Splenic rupture after 28 to 35 days is very rare. Therefore, athletes with IM should be excluded from sport participation for a minimum period of three weeks beginning from the onset of symptoms or from the time of diagnosis if the timing of onset is not clear (7,8). After the minimum three-week disqualification period, athletes may resume low-impact, noncontact training at 50% of preillness level, as long as the following criteria are met:
Resolution of symptoms (including fever, fatigue, lymphadenopathy and pharyngitis);
Normalization of all laboratory markers;
Resolution of splenomegaly, confirmed ideally by ultrasound; and
Resolution of any and all complications (including fatigue, airway obstruction secondary to enlarged tonsils and hepatitis).
If athletes continue to improve in the first week of graded return to activity with no relapse of symptoms, they may be fully cleared to return to sport participation, including contact sports (Figure 2). If ultrasound is not available to document spleen size, extra caution should be exercised before allowing an athlete who is recovering from IM to return to sport, particularly contact sports. Consideration should be given to delaying return to play for another week or two to avoid potentially late splenic rupture (3,7).
Figure 2.
Return to play for an athlete with infectious mononucleosis (IM). *Complications can include fatigue, airway obstruction and hepatitis, among others. Adapted with permission from references 3 and 7
PREVENTION
The best way to avoid missing training or competition is to prevent illness (2). Athletes can reduce their risk of infection by maintaining a healthy lifestyle and by ensuring the following:
Eat a well-balanced diet;
Get adequate sleep;
Avoid overtraining and fatigue;
Allow adequate recovery time following intense exercise;
Avoid contact with people who are ill;
Wash hands frequently;
Do not share water bottles or towels;
Reduce life stressors; and
Get appropriate immunizations (measles, mumps and rubella, hepatitis A and B, influenza and tetanus).
BACK TO THE CASE
On presentation, our athlete had been symptomatic for one week with a fever, fatigue and lymphadenopathy. He had an enlarged spleen on examination and was diagnosed with IM. Regardless of the etiology, the athlete fails the neck check and, therefore, should not be exercising (3–5). In addition, splenomegaly and the diagnosis of IM precludes him from participating in sports for a minimum of three weeks from the time of onset of symptoms to reduce his risk of splenic rupture. Therefore, he should not participate in the tournament on the upcoming weekend. An ultrasound to document resolution of splenomegaly may be helpful to guide the athlete’s return to sport after the minimum three-week exclusion period.
Footnotes
PAEDIATRIC SPORTS AND EXERCISE MEDICINE SECTION
Executive: Drs Laura Purcell, London Health Sciences Centre, London, Ontario (President); Merrilee Zetaruk, Winnipeg, Manitoba (Vice President); Michelle McTimoney, IWK Health Centre, Halifax, Nova Scotia (Secretary); John Philpott, Toronto, Ontario (Member at Large); Claire LeBlanc, Edmonton, Alberta (Member at Large)
Principal author: Dr Laura Purcell, London Health Sciences Centre, London, Ontario
The recommendations in this article do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking into account individual circumstances, may be appropriate.
REFERENCES
- 1.Stricker PR. Acute illnesses. Sullivan JA, Anderson SJ, editors. Care of the Young Athlete. American Academy of Orthopedic Surgeons and American Academy of Pediatrics. 2000:213–8. [Google Scholar]
- 2.Nieman DC. Is infection risk linked to exercise workload? Med Sci Sports Exerc. 2000;32(7 Suppl):S406–11. doi: 10.1097/00005768-200007001-00005. [DOI] [PubMed] [Google Scholar]
- 3.Metz JP. Curr Sports Med Rep. Vol. 2. 2003. Upper respiratory tract infections: Who plays, who sits? pp. 84–90. [DOI] [PubMed] [Google Scholar]
- 4.Eichner ER. Infection, immunity and exercise: What to tell patients? Phys Sportsmed. 1993;21:125–35. doi: 10.1080/00913847.1993.11710319. [DOI] [PubMed] [Google Scholar]
- 5.Primos WA., Jr Sports and exercise during acute illness: Recommending the right course for patients. doi: 10.3810/psm.1996.01.1199. < www.physsportsmed.com/issues/1996/01_96/primos.htm> (Version current at October 17, 2007) [DOI] [PubMed]
- 6.Dommerby H, Stangerup SE, Stangerup M, Hancke S. Hepatosplenomegaly in infectious mononucleosis, assessed by ultrasonic scanning. J Laryngol Otol. 1986;100:573–9. doi: 10.1017/s0022215100099680. [DOI] [PubMed] [Google Scholar]
- 7.Kinderknecht JJ. Infectious mononucleosis and the spleen. Curr Sports Med Rep. 2002;1:116–20. doi: 10.1249/00149619-200204000-00009. (Philadelphia: Current Medicine Group, LLC, 2002) [DOI] [PubMed] [Google Scholar]
- 8.MacKnight JM. Infectious mononucleosis: Ensuring a safe return to sport. Phys Sportsmed. 2002;30:27–41. doi: 10.3810/psm.2002.01.137. [DOI] [PubMed] [Google Scholar]