Abstract
BACKGROUND
Incomplete immunization coverage is common in low-income families and Aboriginal children in Canada.
OBJECTIVE
To determine whether child immunization coverage rates at two years of age were lower in low-income neighbourhoods of Saskatoon, Saskatchewan.
METHODS
Parents who were and were not behind in child immunization coverage were contacted to determine differences in knowledge, beliefs and opinions on barriers and solutions. A multivariate regression model was designed to determine whether Aboriginal cultural status was associated with being behind in childhood immunizations after controlling for low-income status.
RESULTS
Reviewing the past five years in Saskatoon, the six low-income neighbourhoods had complete child immunization coverage rates of 43.7% (95% CI 41.2 to 45.9) for measles-mumps-rubella, and 42.6% (95% CI 40.1 to 45.1) for diphtheria, pertussis, tetanus, polio and Haemophilus influenzae type B. The five affluent neighbourhoods had 90.6% (95% CI 88.9 to 92.3) immunization coverage rates for measles-mumps-rubella, and 78.6% (95% CI 76.2 to 81.0) for diphtheria, pertussis, tetanus, polio and H influenzae type B. Parents who were behind in immunization coverage for their children were more likely to be single, of Aboriginal or other (non-Caucasian or non-Aboriginal) cultural status, have lower family income and have significant differences in reported beliefs, barriers and potential solutions. In the final regression model, Aboriginal cultural status was no longer associated with lower immunization status.
INTERPRETATION
Child immunization coverage rates in Saskatoon’s six low-income neighbourhoods were approximately one-half the rate of the affluent neighbourhoods. The covariates with the strongest independent association with complete childhood immunization status were low income and other cultural status. Aboriginal cultural status was not associated with low child immunization rates after controlling for income status.
Keywords: Children, Ethnology, Immunization, Social class
Abstract
HISTORIQUE
Il est courant de constater une couverture vaccinale incomplète chez les enfants de familles à faible revenu et les enfants autochtones du Canada.
OBJECTIF
À déterminer si les taux de couverture vaccinale chez les enfants de deux ans étaient plus faibles dans les quartiers à faible revenu de Saskatoon, en Saskatchewan.
MÉTHODOLOGIE
Les auteurs ont pris contact avec les parents qui avaient et ceux qui n’avaient pas pris de retard dans la couverture vaccinale de leur enfant afin de déterminer les différences en matière de connaissances, de convictions et d’opinions sur les obstacles et les solutions. Ils ont conçu un modèle de régression multivariée pour déterminer si, une fois le statut de faible revenu contrôlé, le statut culturel d’autochtone s’associait à un retard de l’immunisation des enfants.
RÉSULTATS
Au cours des cinq dernières années à Saskatoon, le taux de couverture vaccinale complète des enfants des six quartiers à faible revenu s’élevait à 43,7 % (95 % IC 41,2 à 45,9) pour la rougeole, la rubéole et les oreillons, et à 42,6 % (95 % IC 40,1 à 45,1) pour la diphtérie, la coqueluche, le tétanos, la polio et l’Haemophilus influenzae de type b. Les cinq quartiers aisés présentaient un taux de couverture vaccinale de 90,6 % pour la rougeole, la rubéole et les oreillons (95 % IC 88,9 à 92,3), et de 78,6 % pour la diphtérie, la coqueluche, le tétanos, la polio et l’H influenzae de type b (95 % IC 76,2 à 81,0). Les parents qui étaient en retard dans la couverture vaccinale de leur enfant étaient plus susceptibles d’être célibataires, autochtones ou d’un autre statut culturel (non-blancs ou non-autochtones), d’avoir un revenu familial plus faible et de présenter des différences considérables en matière de convictions, d’obstacles et de solutions potentielles. Dans le modèle de régression final, le statut culturel d’autochtone ne s’associait plus à un statut d’immunisation plus faible.
INTERPRÉTATION
Les taux de couverture vaccinale des enfants des six quartiers à faible revenu de Saskatoon correspondent à environ la moitié du taux des quartiers aisés. Les covariables les plus fortement associées de manière indépendante au statut de vaccination des enfants étaient le faible revenu et un autre statut culturel. Le statut culturel d’autochtone ne s’associait pas au statut de couverture vaccinale des enfants, une fois le revenu contrôlé.
Few measures in preventive medicine are of such proven value and as easy to implement as routine immunization against infectious disease (1). Unfortunately, infectious disease outbreaks were observed in Canada for measles from 1989 to 1995, mumps in British Columbia in 1997 and Quebec in 1998, and rubella in Manitoba in 1997 and in Ontario in 2005 (1,2).
Previous reports (3–11) indicate that low immunization coverage rates for children are associated with low socioeconomic status, urban dwelling, impoverished neighbourhoods, single-parent families, mobile populations and minority cultural status. A recent publication (12) from Ontario indicated that 26.6% of urban children in the lowest income neighbourhoods did not have up-to-date immunizations compared with 14.3% of children in the most affluent neighbourhoods. In contrast, a report (13) from Manitoba found high child immunization coverage rates with very small socioeconomic disparities, after the introduction of the Manitoba Immunization Monitoring System that actively tracks down and informs health care providers and parents of children who are behind in immunization coverage.
There were four objectives to the current study – to use the Saskatchewan Immunization Management System (SIMS) to determine whether child immunization coverage rates at two years of age were lower in low-income neighbourhoods of Saskatoon, Saskatchewan; to use the SIMS to identify and then contact parents who were and were not behind in child immunization coverage to determine differences in awareness, knowledge, beliefs and opinions on barriers and solutions; to build a regression model to determine which demographic covariates were associated with parents who had incomplete immunization coverage for their children; and to determine whether Aboriginal cultural status was independently associated with low child immunization coverage rates after adjusting for low-income status.
METHODS
The SIMS uses vital statistics and health insurance information to create a population database to determine the percentage of children who have the recommended number of immunizations for their age. The immunization coverage schedule specific to Saskatchewan includes the combination vaccine for measles-mumps-rubella (MMR) at 12 months and 18 months of age, and the combination vaccine for diphtheria, pertussis, tetanus, polio and Haemophilus influenzae type B (DaPTP-Hib) at two months, four months, six months and 18 months of age. The definition of complete coverage is, therefore, two MMR and four DaPTP-Hib immunizations by 18 months of age. Incomplete coverage is defined as less than six immunizations at two years of age or at least six months behind the recommended schedule. The child immunization schedule is different in each province in Canada. The present paper reviews the effectiveness of accomplishing goals specific to Saskatchewan alone. The SIMS database is, on average, more accurate and more complete than the clinical hard copies (14).
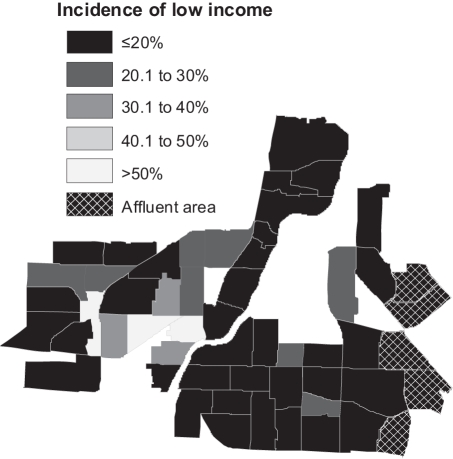
Postal code information from the 2001 census was used to identify six existing residential neighbourhoods in the city of Saskatoon that were defined as ‘low-income cut-off neighbourhoods’ by Statistics Canada (15,16). All six neighbourhoods had contiguous pre-existing municipal boundaries (Figure 1). For the first objective, the percentage of two-year-old children who had their recommended number of immunizations for MMR and DaPTP-Hib in Saskatoon’s low-income neighbourhoods (n=16,683) were compared with the rest of Saskatoon (n=184,284) and five affluent contiguous neighbourhoods (n=18,228). There was no statistically significant heterogeneity between the six low-income neighbourhoods or between the five affluent neighbourhoods in neighbourhood income, education or employment. Complete immunization coverage rates with 95% CIs were computed for the years 2001 to 2005.
Figure 1.
Statistics Canada’s low-income cut-off designation for six Saskatoon (Saskatchewan) residential neighbourhoods in 2001
For the second objective, a list of names was generated for all children who had their second birthday in 2004 or 2005, and were at least six months behind in immunizations as of June 2006 when the SIMS database was accessed. The SIMS database has immunization information from all Saskatoon health care practitioners, except First Nations practitioners from the Saskatoon Tribal Council. Saskatoon children behind in their immunization coverage were manually cross-referenced with children immunized on seven reserve communities adjacent to Saskatoon (five Saskatoon children immunized in 2004 and 2005). An equal number of names were chosen at random by computer from children who were up-to-date in immunization coverage on their second birthday in 2004 and 2005. Parents or guardians of children from both groups were contacted in June and July 2006, and asked to complete a telephone survey on their awareness, knowledge, beliefs and opinions on barriers and solutions. Parents were notified if their child was up-to-date on completion of the phone survey. χ2 tests were used to assess differences between groups without correcting for multiple comparisons.
For the third objective, binary logistic regression was used to describe the relationship between the outcome variable and the explanatory demographic variables of a parent whose child was at least six months behind on childhood immunizations and a parent whose child was not behind in childhood immunizations. Stratification was used to assess for confounding and effect modification in the first step of model building (17). A hierarchical well-formulated front-wise modelling approach was used instead of a computer-generated stepwise algorithm (17). The unadjusted effect of each covariate was determined and entered one step at a time, based on changes in the −2 log likelihood and the Wald test (18). The final model includes factors with beta values for which P<0.05 (18). Confounding was tested by comparing the estimated coefficient of the outcome variable from models that contained the demographic covariates with models that did not contain the demographic covariates (18). Interaction was assessed with product terms (18). R2 was used to determine the proportion of variance in the outcome variable explained by the knowledge of the explanatory variables, but not as a measure of the appropriateness of the final model (18). Goodness-of-fit of the final model was assessed by the Hosmer-Lemeshow statistical test (18). The final results were presented as adjusted odds ratios with 95% CIs (18). All analyses were performed with an SPSS 13.0 (19) software package. The research project received ethics approval from the University of Saskatchewan Behavioural Research Ethics Board.
RESULTS
Reviewing the past five years in Saskatoon, the six low-income neighbourhoods had child immunization coverage rates of 43.7% (95% CI 41.2 to 45.9) for MMR and 42.6% (95% CI 40.1 to 45.1) for DaPTP-Hib, while the rest of Saskatoon had 69.1% (95% CI 68.2 to 70.0) for MMR and 71.9% (95% CI 71.0 to 72.8) for DaPTP-Hib. The five affluent neighbourhoods had 90.6% (95% CI 88.9 to 92.3) complete immunization coverage for MMR and 78.6% (95% CI 76.2 to 81.0) for DaPTP-Hib. Given that the coverage rates for the two immunizations were somewhat different, data are presented separately (Table 1).
TABLE 1.
Complete immunization coverage percentages of two-year-old children by neighbourhood income in Saskatoon, Saskatchewan
| Immunization coverage rates
|
|||
|---|---|---|---|
| Low-income neighbourhoods | Rest of Saskatoon | High-income neighbourhoods | |
| MMR* | |||
| Total n (2001–2005) | 678/1550 | 7327/10610 | 1012/1117 |
| 95% CI (range) | 43.7 (41.2–45.9) | 69.1 (68.2–70.0) | 90.6 (88.9–92.3) |
| DaPTP-Hib† | |||
| Total n (2001–2005) | 661/1550 | 7626/10610 | 878/1117 |
| 95% CI (range) | 42.6 (40.1–45.1) | 71.9 (71.0–72.8) | 78.6 (76.2–81.0) |
Two doses;
Four doses
The second objective was to contact parents who were behind and who were not behind in child immunization coverage to determine differences in awareness, knowledge, beliefs, and opinions on barriers and solutions. There were 1047 children in 2004 and 2005 who were behind in either MMR or DaPTP-Hib immunizations. Of those, there were 274 disconnected phone numbers, 305 wrong numbers and 110 households with no answer after 10 attempts. Of the remaining 358 parents, 271 (75.7%) agreed to participate in the survey. Parents (n= 1047) whose children were completely up-to-date in immunization coverage were chosen at random. Of those, there were 192 disconnected phone numbers, 188 wrong numbers and 121 households without any answer. Of the remaining 546 parents, 418 (76.6%) were willing to complete the phone survey. There was no statistical difference in response rate between the two groups (75.7% and 76.6%), and there was no difference between respondent and nonrespondent in terms of neighbourhood income or neighbourhood education levels.
Parents who were behind in immunization coverage for their children were more likely to be divorced, separated or single, Aboriginal (First Nations, Métis or self-declared) or of other (non-Caucasian and non-Aboriginal) cultural background, and have a lower family income (Table 2).
TABLE 2.
Demographic differences between parents whose children are up-to-date in immunization coverage in comparison with parents whose children are behind in immunization coverage
| Child immunization status
|
|||
|---|---|---|---|
| Demographic information(respondent/primary caregiver) | Behind, n=271 n (%) | Up-to-date, n=418 n (%) | P |
| Sex, female | 234/265 (88.3) | 369/405 (91.1) | 0.239 |
| Marital status | 0.034 | ||
| Divorced or separated | 17/259 (6.6) | 15/401 (3.7) | |
| Married or common law | 200/259 (77.2) | 341/401 (85.0) | |
| Single | 42/259 (16.2) | 45/401 (11.2) | |
| Education level | 0.069 | ||
| Did not complete high school | 20/258 (7.8) | 20/400 (5.0) | |
| Completed high school | 59/258 (22.9) | 71/400 (17.8) | |
| University or technical diploma | 179/258 (69.4) | 309/400 (77.3) | |
| Occupation | 0.100 | ||
| Clerical, sales, service | 74/261 (28.4) | 117/400 (29.3) | |
| Homemaker | 68/261 (26.1) | 104/400 (26.0) | |
| Manual, construction, farmer, transport | 8/261 (3.1) | 29/400 (7.3) | |
| Professional, management | 75/261 (28.7) | 112/400 (28.0) | |
| Student | 11/261 (4.2) | 15/400 (3.8) | |
| Unemployed | 4/261 (1.5) | 8/400 (2.0) | |
| Other | 21/261 (8.0) | 15/400 (3.8) | |
| Cultural background | 0.000 | ||
| Caucasian | 179/258 (69.4) | 336/399 (84.2) | |
| Aboriginal | 35/258 (13.6) | 32/399 (8.0) | |
| Other | 44/258 (17.1) | 31/399 (7.8) | |
| Annual family income | 0.006 | ||
| Less than $25,000 | 54/234 (23.1) | 51/320 (15.9) | |
| $25,000 to $49,999 | 76/234 (32.5) | 80/320 (25.0) | |
| $50,000 to $99,999 | 73/234 (31.2) | 141/320 (44.1) | |
| Above $99,999 | 31/234 (13.2) | 48/320 (15.0) | |
Parents who were behind in immunization coverage were more likely to believe that immunizations weakened the immune system, natural medicines provided better and safer protection, their child would develop natural immunity and immunizations were associated with serious known and unknown side effects. In addition, parents who were behind in immunization coverage were more likely to list barriers including lack of time, no location nearby, transportation problems, childcare issues, safety concerns for their child, lack of trust with the medical community, concerns about immunizations that have not been addressed and previous negative experiences while immunizing their child (Table 3).
TABLE 3.
Beliefs and barriers toward child immunizations between parents who are behind and those who are up-to-date in child immunizations
| Child immunization status
|
|||
|---|---|---|---|
| Beliefs and barriers | Behind, n=271 n (%) | Up-to-date, n=418 n (%) | P |
| Do you believe that your infant child is fully up-to-date with immunization coverage?, yes Beliefs about immunizations | 168/263 (63.9) | 388/406 (95.6) | 0.000 |
| Immunizations are no longer necessary because the diseases they protect against have been eliminated from society, true | 9/259 (3.5) | 8/404 (2.0) | 0.314 |
| Immunizations weaken the immune system, true | 38/243 (15.6) | 21/396 (5.3) | 0.000 |
| Natural medicines provide better and safer protection than immunizations, true | 47/235 (20.0) | 32/382 (8.4) | 0.000 |
| I believe my child will develop natural immunity if we do not immunize, true | 39/252 (15.5) | 31/388 (8.0) | 0.004 |
| I do not think you should immunize when a child has a minor illness like a cold, true | 183/251 (72.9) | 242/390 (62.1) | 0.005 |
| Immunizations are associated with serious known side effects, true | 112/250 (44.8) | 109/389 (28.0) | 0.000 |
| Immunizations are associated with serious unknown side effects, true | 78/242 (32.2) | 85/383 (22.2) | 0.007 |
| Barriers toward immunizations | |||
| I simply forget to immunize my child, yes | 91/261 (34.9) | 115/403 (28.5) | 0.087 |
| I do not have enough time in my busy day, yes | 36/262 (13.7) | 31/402 (7.7) | 0.017 |
| I do not have a location nearby, yes | 24/261 (9.2) | 15/403 (3.7) | 0.006 |
| I do not have access to transportation, yes | 28/262 (10.7) | 18/402 (4.5) | 0.003 |
| I have other children to attend to, yes | 62/261 (23.8) | 46/402 (11.4) | 0.000 |
| I would prefer another health care practitioner to perform my child’s immunization, yes | 34/260 (13.1) | 35/401 (8.7) | 0.090 |
| I fear for the safety of my child, yes | 70/262 (26.7) | 60/402 (14.9) | 0.000 |
| I do not like seeing my child in pain or crying, yes | 55/261 (21.1) | 82/401 (20.4) | 0.845 |
| I have cultural barriers that discourage immunization, yes | 11/259 (4.2) | 10/401 (2.5) | 0.257 |
| I do not trust the medical community, yes | 31/257 (12.1) | 22/401 (5.5) | 0.003 |
| I have concerns about immunizations that have not been addressed to my satisfaction, yes | 70/258 (27.1) | 64/401 (16.0) | 0.001 |
| I had a previous negative experience with immunizing my child, yes | 31/259 (12.0) | 22/401 (5.5) | 0.003 |
In terms of solutions, parents who were behind in immunization were more likely to suggest home visits by a nurse or doctor, the provision of a clinic in their neighbourhood, that only physicians immunize their child and that someone spend more time with them to talk about immunizations and the health of their child (Table 4). Solutions with strong majority support from both groups of parents to help keep their children up-to-date in immunization coverage included reminder telephone calls, reminder letters in the mail, reminders from health care practitioners when the parent is present for another matter, flexible walk-in scheduling, and extended clinical hours on weekends and evenings (Table 4).
TABLE 4.
Solutions listed by parents to increase child immunization coverage rates
| Child immunization status
|
|||
|---|---|---|---|
| Solutions and preferences | Behind, n=271 n (%) | Up-to-date, n=418 n (%) | P |
| Solutions to keep children up-to-date | |||
| Reminder telephone calls, yes | 216/262 (82.4) | 349/401 (87.0) | 0.117 |
| Reminder letters in mail, yes | 208/262 (79.4) | 345/401 (86.0) | 0.032 |
| Home visits by nurse or doctor, yes | 97/261 (37.2) | 101/398 (25.4) | 0.002 |
| Reminded by my doctor or nurse when I am present for another matter, yes | 189/260 (72.7) | 335/402 (83.3) | 0.001 |
| General advertising, yes | 117/261 (44.8) | 232/400 (58.0) | 0.001 |
| Flexible walk-in scheduling, yes | 186/260 (71.5) | 319/402 (79.4) | 0.025 |
| Extended clinical hours on weekends, yes | 187/260 (71.9) | 316/402 (78.6) | 0.051 |
| Extended clinical hours at night, yes | 198/261 (75.9) | 316/401 (78.8) | 0.391 |
| Reduced waiting times in clinic, yes | 153/260 (58.8) | 208/401 (51.9) | 0.079 |
| Provide child with other health services at same time as immunization, yes | 176/259 (68.0) | 261/401 (65.1) | 0.500 |
| Provide a clinic in your neighbourhood, yes | 160/261 (61.3) | 205/401 (51.1) | 0.011 |
| Provide transportation to nearest clinic, yes | 79/261 (30.3) | 106/402 (26.4) | 0.288 |
| Provide babysitting at clinic, yes | 96/259 (37.1) | 145/400 (36.3) | 0.869 |
| Preferences to keep children up-to-date | |||
| Prefer only public health nurses to immunize my child, yes | 89/261 (34.1) | 127/403 (31.5) | 0.498 |
| Prefer only physicians to immunize my child, yes | 62/261 (23.8) | 70/403 (17.4) | 0.047 |
| Prefer only paediatricians to immunize my child, yes | 48/260 (18.5) | 55/403 (13.6) | 0.100 |
| Prefer someone spend more time with me to talk about child immunizations during my appointment, yes | 109/259 (42.1) | 134/401 (33.4) | 0.026 |
| Prefer that someone spend more time with me to talk about health of my child during immunization appointment, yes | 138/258 (53.5) | 168/401 (41.9) | 0.004 |
| Prefer that someone spend more time with me to talk about my health during child immunization appointment, yes | 63/258 (24.4) | 78/402 (19.4) | 0.144 |
It is of particular interest that 63.9% of parents whose child was behind in immunization coverage believed that their child was fully up-to-date (Table 3). Of the parents who believed their child was up-to-date, 27.7% indicated that they simply forgot to immunize their child in comparison with 47.4% of the parents who did not believe their child was up-to-date (P=0.002). In other words, most parents did not forget that their child was behind – they simply did not know that their child was not fully immunized. Of the same parents whose child was behind in immunization coverage but the parent believed their child was up-to-date, 91.0% would have liked a reminder telephone call, 87.3% would have liked a reminder letter and 81.2% would have liked to have been reminded by their doctor or nurse while present for another matter.
It is also of interest to review the parents who were behind in immunization coverage but knew their child was behind. The greatest barrier is that 44.8% believe immunizations are associated with serious known side effects and 32.2% believe that immunizations are associated with serious unknown side effects.
For the third objective, binary logistic regression was used to determine whether any demographic variable had an independent effect on the outcome of a child falling behind on immunization coverage. Variables with the strongest unadjusted association during model building included parent cultural status (Aboriginal and other), lower household income status and being a single parent. In the final regression model, Aboriginal cultural status no longer had a statistically significant association with the outcome, but other cultural status remained (OR=2.259; 95% CI 1.306 to 3.909). Low income acted as a confounder for Aboriginal cultural status. Lower income status remained statistically significant in the final model (OR=1.721; 95% CI 1.164 to 2.545) (Table 5). The variable of single parenthood lost its statistical significance after controlling for other covariates. There was no effect modification. The R2 of the final model was 0.390, suggesting reasonable explanation of the proportion of variance in the outcome variable explained by the knowledge of the explanatory variables. The goodness-of-fit test result (P=0.975) suggests that the final model is appropriate and that the predicted values are accurate representations of the observed values.
TABLE 5.
Independent variables associated with parents whose child was not up-to-date in immunization coverage
| Independent variables | Beta | SE | Unadjusted OR | Adjusted OR (95% CI) | P |
|---|---|---|---|---|---|
| Cultural status of parent | |||||
| Caucasian* | |||||
| Aboriginal | 0.348 | 0.293 | 2.053 | 1.417 (0.797–2.517) | 0.235 |
| Other (non-Caucasian or non-Aboriginal) | 0.815 | 0.280 | 2.664 | 2.259 (1.306–3.909) | 0.004 |
| Income of family | |||||
| More than $100,000 per year* | |||||
| Less than $50,000 per year | 0.543 | 0.200 | 1.917 | 1.721 (1.164–2.545) | 0.007 |
| $50,000 to $99,999 per year | 0.225 | 0.274 | 1.247 | 1.252 (0.732–2.143) | 0.412 |
Dependent variable – child behind in immunization coverage (n=689).
Reference category. SE Standard error
DISCUSSION
Child immunization coverage rates are routinely lower in Saskatoon’s six low-income neighbourhoods in comparison with the rest of the city, and are approximately one-half the rate of the affluent neighbourhoods. Although this trend is consistent with other jurisdictions in Canada, the magnitude of the disparity is disproportionate (12). Similar to other reports, Saskatoon parents who were behind in immunization coverage for their children were more likely to be divorced, separated or single; Aboriginal or other culture; have lower family income, and list barriers including risk of adverse effects, access problems, distrust of the medical community, lack of knowledge about immunizations and a desire for clinicians to spend more time with them (3-11,20,21). The authors caution that some of the relative differences observed are small.
Perhaps surprisingly, 63.9% of parents with children who were at least six months behind in immunization coverage believed their children were up-to-date. This is a new finding that suggests the need to use a reminder system in Saskatoon. Approximately 90% of those behind in coverage who believed their children were up-to-date would have liked a reminder phone call or letter to keep them up-to-date. This request from Saskatoon parents is evidence based. A meta-analysis on patient reminder systems to improve immunization rates in children found these systems to be effective (OR=1.45; 95% CI 1.28 to 1.66) (4). A report from Manitoba indicates that their electronic monitoring system has actually been used to remind parents and practitioners to track down children with incomplete coverage to reduce socioeconomic disparities in childhood immunization (13).
Previous reports (22) indicate that Aboriginal children in Canada are more likely to be behind in immunization coverage, but the authors were not able to find a study that statistically controlled for potential confounding variables such as low-income status. Although Aboriginal cultural status was initially strongly associated with child immunization status, in our study, Aboriginal culture did not have a statistically significant association with incomplete immunization coverage in children after adjusting for low-income status. This is a new finding and is important because it invalidates the negative stereotype that it is more difficult to immunize Aboriginal children. Aboriginal children in Alaska (USA) routinely have immunization coverage rates in excess of 90%, despite traditional risk factors such as poverty, a higher proportion of uneducated mothers and remote access. High child immunization coverage rates in Alaska is the result of the utilization of an electronic monitoring system, collaboration between the state government and local tribal councils, willingness of public health nurses to perform home visits and making vaccination delivery a high priority (23,24).
A limitation of our study was that majority of parents were not able to be contacted. This introduces a potential selection bias that we were unable to control for in our analysis. Once parents were contacted, response rates were similar. This finding does suggest, however, that more efforts are required to keep telephone numbers current if telephone reminders are to be used to keep parents and their children up-to-date in immunization coverage. The only question with a response rate below 80% was income status of parents with children who were up-to-date. Using neighbourhood income as a proxy for individual income did not significantly influence the final regression model.
Future research should evaluate whether a reminder system in Saskatoon is effective in increasing overall immunization coverage rates up to the national goal of 95% (1).
Acknowledgements
The authors thank Dr Bill Bingham, Gary Beaudin, Janice Chomyn, Terry Dunlop, Lynne Warren, Judith Wright, Michelle Flamont and Tanis Kershaw for their assistance.
REFERENCES
- 1.Health Canada. 6th edn. Ottawa: Health Canada; 2002. Canadian Immunization Guide. [Google Scholar]
- 2.Public Health Agency of Canada. Infectious diseases news brief, May 7, 2005. < http://www.phac-aspc.gc.ca/bid-bmi/dsd-dsm/nb-ab/2005/nb2105_e.html> (Version current at November 12, 2007)
- 3.Szilagyi PG, Schaffer S, Shone L, et al. Reducing geographic, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics. 2002;110:e58. doi: 10.1542/peds.110.5.e58. [DOI] [PubMed] [Google Scholar]
- 4.Jacobson VJ, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev. 2005;(3):CD003941. doi: 10.1002/14651858.CD003941.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briss PA, Rodewald LE, Hinman AR, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18:97–140. doi: 10.1016/s0749-3797(99)00118-x. [DOI] [PubMed] [Google Scholar]
- 6.Kendrick D, Hewitt M, Dewey M, et al. The effect of home visiting programmes on uptake of childhood immunization: A systematic review and meta-analysis. J Public Health Med. 2000;22:90–8. doi: 10.1093/pubmed/22.1.90. [DOI] [PubMed] [Google Scholar]
- 7.Agbley D, Campbell H. London: Health Education Authority; 1998. Summary of factors affecting immunization uptake levels. Childhood Immunization in England: Issues from the Research. [Google Scholar]
- 8.Marsh GN, Channing DM. Comparison in use of health services between a deprived and an endowed community. Arch Dis Child. 1987;62:392–6. doi: 10.1136/adc.62.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reading R, Colver A, Openshaw S, Jarvis S. Do interventions that improve immunization uptake also reduce social inequalities in uptake? BMJ. 1994;308:1142–4. doi: 10.1136/bmj.308.6937.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lynch M. Effect of practice and patient population characteristics on the uptake of childhood immunizations. Br J Gen Pract. 1995;45:205–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Fleming DM, Charlton JR. Morbidity and healthcare utilisation of children in households with one adult: Comparative observational study. BMJ. 1998;316:1572–6. doi: 10.1136/bmj.316.7144.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guttmann A, Manuel D, Dick PT, To T, Lam K, Stukel TA. Volume matters: Physician practice characteristics and immunization coverage among young children insured through a universal health plan. Pediatrics. 2006;3:595–602. doi: 10.1542/peds.2004-2784. [DOI] [PubMed] [Google Scholar]
- 13.Gupta S, Roos LL, Walld R, Traverse D, Dahl M. Delivering equitable care: Comparing preventive services in Manitoba. Am J Public Health. 2003;93:2086–92. doi: 10.2105/ajph.93.12.2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atcheson W, Palmer C, Tuchschere R. Regina: Saskatchewan Health; 2006. Saskatchewan immunization management system validity study. [Google Scholar]
- 15.Statistics Canada. Ottawa: Statistics Canada; 2005. 2001 population census. [Google Scholar]
- 16.Statistics Canada. Low income cut-offs from 1994–2003 and low income measures from 1992–2001. < http://www.statcan.ca/english/research/75F0002MIE/75F0002MIE2004002.pdf> (Version current at November 12, 2007)
- 17.Rothman KJ, Greenland S. 2nd edn. Philadelphia: Lippincott Williams and Wilkins; 1998. Modern Epidemiology. [Google Scholar]
- 18.Hosmer DW, Lemeshow S. New York: Wiley; 1989. Applied Logistic Regression. [Google Scholar]
- 19.SPSS. Chicago: SPSS Inc; 2000. version 10.0. [Google Scholar]
- 20.Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol. 2005;58:1081–8. doi: 10.1016/j.jclinepi.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Tarrant M, Gregory D. Exploring childhood immunization uptake with First Nations mothers in north-western Ontario, Canada. J Adv Nurs. 2003;41:63–72. doi: 10.1046/j.1365-2648.2003.02507.x. [DOI] [PubMed] [Google Scholar]
- 22.Health Canada. A statistical profile on the health of First Nations in Canada. Ottawa: Health Canada; 2005. Health Status; pp. 48–54. [Google Scholar]
- 23.Centers for Disease Control and Prevention. Vaccination coverage levels among Alaska Native Children aged 19–35 months – National Immunization Survey, United States, 2000–2001. MMWR. 2003;52:710–3. [PubMed] [Google Scholar]
- 24.Strine TW, Mokdad AH, Barker LE, et al. Vaccination coverage of American Indian/Alaska native children aged 19 to 35 months: Findings from the national immunization survey 1998–2000. Am J Public Health. 2003;93:2046–9. doi: 10.2105/ajph.93.12.2046. [DOI] [PMC free article] [PubMed] [Google Scholar]