Abstract
PURPOSE The explosion of evidence in the last decade supporting the role of spirituality in whole-person patient care has prompted proposals for a move to a biopsychosocial-spiritual model for health. Making this paradigm shift in today’s multicultural societies poses many challenges, however. This article presents 2 theoretical models that provide common ground for further exploration of the role of spirituality in medicine.
METHODS The 3 H model (head, heart, hands) and the BMSEST models (body, mind, spirit, environment, social, transcendent) evolved from the author’s 12-year experience with curricula development regarding spirituality and medicine, 16-year experience as an attending family physician and educator, lived experience with both Hinduism and Christianity since childhood, and a lifetime study of the world’s great spiritual traditions. The models were developed, tested with learners, and refined.
RESULTS The 3 H model offers a multidimensional definition of spirituality, applicable across cultures and belief systems, that provides opportunities for a common vocabulary for spirituality. Therapeutic options, from general spiritual care (compassion, presence, and the healing relationship), to specialized spiritual care (eg, by clinical chaplains), to spiritual self-care are discussed. The BMSEST model provides a conceptual framework for the role of spirituality in the larger health care context, useful for patient care, education, and research. Interactions among the 6 BMSEST components, with references to ongoing research, are proposed.
CONCLUSIONS Including spirituality in whole-person care is a way of furthering our understanding of the complexities of human health and well-being. The 3 H and BMSEST models suggest a multidimensional and multidisciplinary approach based on universal concepts and a foundation in both the art and science of medicine.
Keywords: Spirituality, theoretical models, whole-person care, education, research
INTRODUCTION
To cure sometimes,
To relieve often,
To comfort always.
Anonymous, 16th century, France
The ideal of whole-person care has long been espoused by physicians. Many have written about the role of physician as scientist and healer, who uses both objective and subjective methods to bring cure, relief, and comfort to those facing suffering, illness, and death.1,2 Since the time of this 16th century quotation, we have made tremendous advances in the ability to cure. Yet, experienced physicians realize that as we begin the 21st century, with the global burden of disease shifting to chronic illness,3 we still live in an era in which most of what we can offer consists of providing relief and comfort.
Growing evidence for the beneficial role of spirituality in health and well-being suggests promising opportunities for innovation in providing relief and comfort.4–21 The Association of American Medical Colleges (AAMC), the World Health Organization (WHO), and the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) now include spirituality in medical practice and education.22,23 In addition, many have called for an expansion of Engel’s biopsychosocial model24,25 for health care to a biopsychosocial-spiritual model,26–29 in which relief requires understanding physical, mental, and spiritual suffering, and spiritual care plays a crucial role in providing “comfort always.” Yet there still remain many challenges to incorporating spirituality into medicine. Identified barriers include the lack of a common “language” for spirituality, as well as concern regarding boundaries, ethics, and cultural and religious differences.12,30
Few comprehensive models exist that explicitly address how spirituality fits into whole-person health care. Reviewing the medical literature, Sulmasy26 concludes that specific models for patient care are lacking and proposes a biopsychosocial-spiritual model for improving quality of life for dying patients. Fitchett’s 7 × 7 model31 for spiritual assessment, tailored for those providing pastoral care, includes 7 dimensions of holistic assessment and 7 elements of spiritual assessment in a 2-column table. Wilber’s 4-quadrant integral model32–34 organizes all human phenomena into 4 domains (interiors of individuals, exteriors of individuals, interior collective, and exterior collective) and can be applied to medicine.34 Benson and Stark13 include spirituality in the self-care leg of their 3-legged therapeutic stool (pharmaceuticals, surgery, self-care). A few models for whole-person care are also described in the nursing and social work literature.29,35
Some models also exist regarding specific aspects of spirituality/religion and medicine. These models include effects of religion on health36; links between mind and spirit33; frameworks for spirituality37,38; and models for nurse education39 and counselor training.40
Although these models are helpful, few are specifically tailored to the daily patient care needs of physicians. There is also need for models that explicitly address the problem of cultural and religious diversity regarding spirituality, the role of spirituality in the therapeutic relationship, and the spiritual needs of health care professionals themselves.
This article provides a theoretical framework for the inclusion of spirituality in whole-person care in modern multicultural societies, for clinicians, educators, and researchers, through use of 2 models: the 3 H dimensions of of spirituality model (head, heart, hands) and the BMSEST model (body, mind, spirit, environment, social, transcendent). Specific goals for these models are (1) comprehensiveness, (2) applicability across belief systems (religious or secular), (3) accessibility to clinicians and learners, and (4) provision of a theoretical home for research on spirituality and health.
MODEL DEVELOPMENT
The 3 H and BMSEST models evolved from the author’s 12-year experience with curricula development regarding spirituality and medicine. This experience included extensive literature review; implementation of 4 different curricula (3 required and 1 elective) for medical students, residents, faculty, and staff at Brown University, each running 4 to 7 years41–43; and national presentations. The models were developed, tested with learners, and refined over 12 years.
Other influences on model development include 16 years as an attending family physician and educator, including 13 years as core family medicine residency faculty; lived experience with both Hinduism and Christianity since childhood, in Sri Lanka, England, the United States, and India; and a lifetime study of the world’s great spiritual traditions, including formal study of Hinduism and Christianity, and informal study of Judaism, Buddhism, Islam, Native American spirituality, Jainism, Sikhism, Zoroastrianism, and the writings of mystics and secular philosophers.
The 3 H and BMSEST models represent a synthesis of these experiences. The effects of these experiences on model development include emphasis on the practical needs of physicians, learners, and patients; attention to cultural and religious diversity; and a quest for common ground.
WHOLE-PERSON CARE
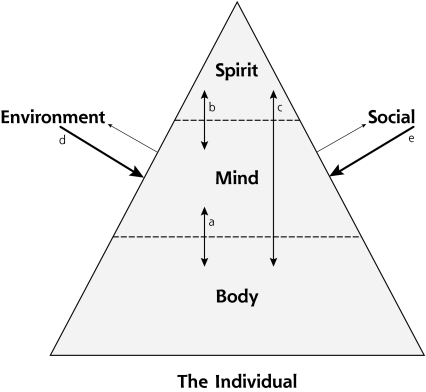
The first step in incorporating spirituality into medicine is establishing a model of the human being, composed of body (B), mind (M), and spirit (S). Figure 1 ▶, based on Maslow’s triangle44 for hierarchy of needs, illustrates this concept. Maslow’s lesser known, later work describes a state, beyond the commonly accepted pinnacle of self-actualization, termed self-transcendence, which is consistent with the inclusion of the spirit as part of the whole person.45 Dashed lines between body, mind, and spirit indicate that these are closely related rather than distinct entities. Arrows (a, b, c) represent the complex mechanisms through which these 3 facets interact. Ongoing research regarding these mechanisms includes anatomic, physiologic, biochemical, immunologic, energetic, and psychological exploration.17,32,33,46–61 Environmental (E) and social (S) influences on physical, mental, and spiritual health are also depicted in this figure and are considered separate factors, consistent with the WHO Quality of Life approach.62 In order for this model to be practical, a definition of human spirituality must be developed that is applicable to all human beings, regardless of background, just as definitions of the human body and mind are universal.
Figure 1.
BMSEST model at the individual level: the whole person plus external factors.
BMSEST = body, mind, spirit, environment, social, and transcendent.
Note: Body = cells, organs, biochemistry, genetics, physiology, possibly energy systems, etc.; mind = thoughts, emotions, cognitive function, etc.; spirit = see Table 1 ▶; environment = physical environment, occupational exposure, health care system, etc.; social = family, culture, religious organization, education, economic factors, etc.
Arrow a = interactions between body and mind.
Arrow b = interactions between mind and spirit.
Arrow c = interactions between body and spirit.
Arrow d = interactions between environmental factors and the individual.
Arrow e = interactions between social factors and the individual.
DEFINITION OF SPIRITUALITY (THE 3 H MODEL)
Defining spirituality has been a challenge for the medical profession. Yet, in order to have meaningful dialog, a common understanding of spirituality is essential. Spirituality is a complex construct. Responses from at least 800 medical students, residents, faculty, and staff in small-group teaching sessions to the question, “What does this word spirituality mean?”; a qualitative study of family medicine residents (unpublished data); and a review of the literature37,38,63–67 led to formulation of the multidimensional 3 H model of spirituality shown in Table 1 ▶.
Table 1.
The 3 H Dimensions of Spirituality, With Examples of Each Dimension
| Cognitive (Head) | Experiential (Heart) | Behavioral (Hands) |
| Beliefs | Love | Duties |
| Values | Compassion, altruism, forgiveness | Daily behavior |
| Ideals | Moral obligations | |
| Meaning | Connection, relationship with: | Choices |
| Purpose | Self | Life choices |
| Truth | Others, community | Medical choices |
| Wisdom | Environment, nature | Specific practices: |
| Faith (belief) | The transcendent | Prayer, meditation, yoga, chanting, rituals, diet, nature walks, etc |
| Inner energy Strength, resilience |
Participation in religious community | |
| Inner peace, comfort, support | ||
| Hope | ||
| Faith (trust) | ||
| Transcendence |
The 3 H’s encompass cognitive (head), experiential (heart), and behavioral (hands) aspects of the human spiritual experience. The phrase “head, heart, and hands” is used widely in other contexts68–71 but is applicable here. The cognitive, or existential, (head) aspects include search for meaning and purpose, and values and beliefs most important in one’s life. The experiential (heart) aspects encompass the human need for love, inner peace, resilience, and connection. Finally, the behavioral (hands) aspects pertain to the outward expression of spiritual beliefs and needs, such as life choices, behavior toward others, rituals, and practices. These dimensions of spirituality are applicable to all human beings irrespective of culture or belief system, whether secular or religious.
In the medical context, spiritual issues pertaining to the head include such questions as why is this happening to me (or my loved one), what will happen after I die, are these treatments consistent with my beliefs, and if God exists, where is God now? Spiritual issues related to the heart include the experiences of feeling connected vs alone when ill; feeling peace vs turmoil when facing death; or feeling hope vs despair when dealing with chronic illness. Finally, hands aspects can manifest in the medical context in a variety of ways including spiritually based treatment decisions by patients or families; patients’ requests for specific rituals, prayers, or diets; or physicians’ own needs for spiritual rituals or prayer when dealing with stressful situations.
RELATION BETWEEN SPIRITUALITY AND RELIGION
People differ widely in the way they view the relationship between spirituality and religion. For some, these terms refer to the same thing; for others, they are overlapping concepts; and for yet others, they are vastly different.64–67,72
One practical approach is to envision spirituality as addressing universal human questions and needs, and religion as providing specific (and often differing) answers to those questions, and ways of meeting those needs. Human spirituality, therefore, is often expressed in the specific language of religions or other world views. For example, to the question of what happens after death, Christianity might discuss heaven and hell, whereas Buddhism will refer to karma and rebirth. To the question of how to feel more connected and at peace, Islam might suggest specific prayers and the reading of the Koran, whereas Hinduism might recommend specific Vedic chants and mantras. Regarding how to lead a good life and make good choices, Judaism might point to the Ten Commandments and Talmudic discussions, whereas an atheist might point to certain basic human societal values to guide life’s many decisions. The questions and needs are universal, but the answers and approaches vary.
In Figure 1 ▶, organized religion is listed under social factors (S) that influence the individual. Because the combination of religious background, culture, family, and past experience shape the individual’s spirituality, members of similar religious backgrounds may have different spiritual beliefs and needs. Huston Smith asserts that in every religious community, a variety of “spiritual personality types” exist, ranging from atheists, to polytheists, to monotheists, to mystics.73 In a Jewish family, for example, one brother may be orthodox in his practices, whereas another brother may describe himself as a secular Jew; each will have different needs related to health care. Personal religiosity, therefore, is an aspect of a person’s spirit in Figure 1 ▶ (the 3 H’s) and interacts to varying degrees with organized religion.
SPIRITUAL SUFFERING
Spiritual suffering can occur in any of the 3 dimensions outlined in Table 1 ▶ (head, heart, hands). A mother whose child has just died may wonder whether this is divine punishment for something she did earlier in life, thus experiencing spiritual suffering in the head dimension. A patient who is dying of cancer and has noticed family and health professionals withdrawing from him may be suffering in the heart dimension. Finally, a recent immigrant, without access to family or religious community, may be unable to perform important rituals that sustain him, thus suffering in the hands dimension. It is important to note that these 3 dimensions are closely related; thus, suffering may occur in all 3 dimensions simultaneously. The mother who is struggling with meaning (head), in the example above, may also feel disconnected from God (heart) and find herself unable to pray for help (hands). She needs assistance from someone specifically trained to address all of these issues.
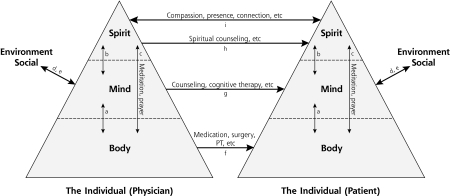
Because suffering has physical, mental, and spiritual aspects, therapeutic options should be available at all of these levels. Relief from spiritual suffering can be provided by spiritual self-care and 2 levels of therapeutic options: specialized and general spiritual care (described below). Figure 2 ▶ illustrates therapeutic approaches at the body, mind, and spirit levels (arrows f, g, h, i). Given the complexity of human suffering, multidisciplinary teams are increasingly needed to provide appropriate therapeutic interventions.
Figure 2.
Secular version of the BMSEST model for whole-person care: the physician-patient relationship.
BMSEST = body, mind, spirit, environment, social, and transcendent; PT=physical therapy.
Arrow a = interactions between body and mind.
Arrow b = interactions between mind and spirit.
Arrow c = interactions between body and spirit.
Arrow d = interactions between environmental factors and the individual.
Arrow e = interactions between social factors and the individual.
Arrow f = therapeutic approaches at the body level.
Arrow g = therapeutic approaches at the mind level.
Arrow h = therapeutic approaches at the spirit level (specialized spiritual care).
Arrow i = therapeutic effects at the spirit level (general spiritual care).
SPIRITUAL CARE
Spiritual Self-Care
Self-care of the body and mind, such as by healthy diet, exercise, and social support, has long been encouraged. Spiritual self-care can take the form of self-understanding and inquiry regarding beliefs and values, or methods for bringing peace and tranquility, such as prayer, meditation, nature walks, church attendance, or yoga. With the growing interest in the efficacy of self-management in the treatment of chronic illness, the role of spiritual self-care in health is fertile ground for exploration.
Specialized Spiritual Care
For specific struggles with head issues or hand needs, such as specific prayers or rituals, the most appropriate approach involves consulting a professional trained in spiritual care, such as a chaplain with clinical pastoral education (CPE) training or a community religious leader.74–76 In much the same way as social workers or psychologists provide the mental health components of whole-person care, chaplains are also integral to the health care team. To maintain high-quality patient care, it is critical to attend to the boundaries of role and training between physician and specialist in providing this specialized spiritual care.74–76 Physicians can identify the need and provide simple modifications in the treatment plan to accommodate specific beliefs. Chaplains, however, are trained to provide in-depth counseling and access to religious rituals and prayers (interaction h in Figure 2 ▶). In addition, it is essential for all professionals to cultivate self-awareness to avoid interference of personal beliefs and biases in ethical, patient-centered care.76
General Spiritual Care—Being a Healer
Spiritual care also attends to the heart needs (interaction i in Figure 2 ▶). The health care setting can be impersonal, leaving patients feeling vulnerable and disconnected from their usual sources of strength. This state of spiritual distress is easily overlooked because no clear religious struggle or need is articulated. The therapeutic intervention at this heart level is at once both simple and extremely difficult. It requires that health care professionals bring their humanness to the medical encounter. Elements include compassion, presence, true listening, and the encouragement of realistic hope, which have been articulated as critical elements of spiritual care.77 Unlike head and hand issues, these elements do not require doing, but rather being. These interventions do not require inquiring about specific beliefs and take no more time than a clinician’s usual duties. Rather, they require that health care professionals augment their everyday activities with presence, compassion, and positive intention. This definition of spiritual care overlaps considerably with the concept of physician as healer,1,2,78–81 who cures, relieves, and comforts always. Balint82 refers to the doctor as a potent medication, and Hippocrates2 said, “Some patients, though conscious that their condition is perilous, recover their health simply through their contentment with the goodness of the physician.” Some of these concepts are also addressed in the literature on mindfulness83 and professionalism79 in medicine, and in the research being done on listening,84 altruism and compassion,85 and the placebo effect.13
Importantly, general spiritual care does not involve emotional entanglement. There are clear distinctions between being engaged vs enmeshed. Osler, in his famous speech “Aequanimitas,”86 describes the value of clinical detachment, the “mental equilibrium of the physician…,” but advises striving for this “without at the same time hardening ‘the human heart by which we live.…” More recently, Fricchione87 describes the middle ground between separation and attachment in his neurobiologic modeling of human development and spirituality.
To achieve this critical balance, physicians need to attend to their own health and well-being, including their spiritual health. Doing so is challenging in today’s health care environment, yet is essential in the quest to be a healer and scientist. Figure 2 ▶ reminds us that every physician is also a whole person—a product of his or her own culture, family, and social institutions (including the medical industry). It also reminds us that at the level of general spiritual care, the therapeutic association (arrow i) is bidirectional—physicians have the potential to heal and be healed through their clinical interactions, as clearly illustrated by numerous physician stories.88–90
BMSEST MODELS—CULTURAL AND RELIGIOUS VARIATIONS
Figure 2 ▶ illustrates the physician-patient relationship with therapeutic options at body (B), mind (M), and spirit (S) levels within the context of environmental (E) and social (S) factors; however, many who examine this figure will argue that no discussion regarding spirituality is complete without a discussion of the transcendent (T). The figure displays a secular version of the BMSEST model, which may resonate most readily with secular humanists or atheists. In this model, spiritual factors are entirely contained within the human being, and prayer and meditation are likewise human phenomena. The transcendent, in this model, may refer to the set of societal values and needs that transcend the individual’s needs, thus guiding complex ethical decision making.
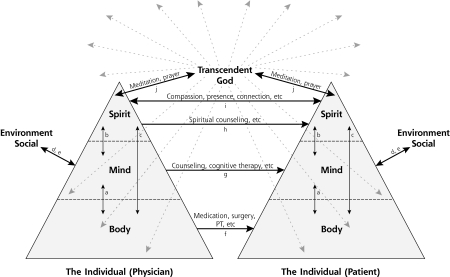
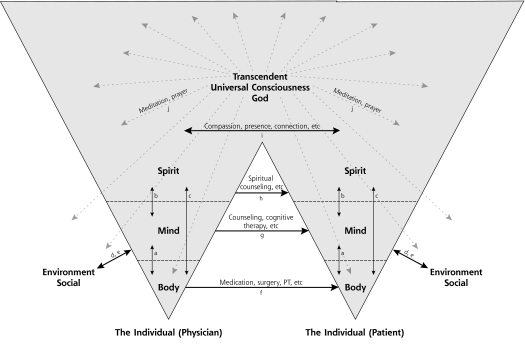
When one studies the world’s religions,73,91–96 2 major conceptual models of a divine transcendent emerge, giving rise to 2 BMSEST variations—the duality model (Figure 3 ▶) and the unity model (Figure 4 ▶). Both models exist to some degree in all the major religions; however, the duality model predominates in western religion, and the unity model predominates in eastern thought and the mystic traditions of many religions.
Figure 3.
Duality version of the BMSEST model for whole-person care.
BMSEST = body, mind, spirit, environment, social, and transcendent; PT=physical therapy.
Arrow a = interactions between body and mind.
Arrow b = interactions between mind and spirit.
Arrow c = interactions between body and spirit.
Arrow d = interactions between environmental factors and the individual.
Arrow e = interactions between social factors and the individual.
Arrow f = therapeutic approaches at the body level.
Arrow g = therapeutic approaches at the mind level.
Arrow h = therapeutic approaches at the spirit level (specialized spiritual care).
Arrow i = therapeutic effects at the spirit level (general spiritual care).
Arrow j = interactions between the individual and the Transcendent.
Figure 4.
Unity version of the BMSEST model for whole-person care.
BMSEST = body, mind, spirit, environment, social, and transcendent; PT=physical therapy.
Arrow a = interactions between body and mind.
Arrow b = interactions between mind and spirit.
Arrow c = interactions between body and spirit.
Arrow d = interactions between environmental factors and the individual.
Arrow e = interactions between social factors and the individual.
Arrow f = therapeutic approaches at the body level.
Arrow g = therapeutic approaches at the mind level.
Arrow h = therapeutic approaches at the spirit level (specialized spiritual care).
Arrow i = therapeutic effects at the spirit level (general spiritual care).
Arrow j = interactions between the individual and the Transcendent.
In the duality model (Figure 3 ▶), God is seen as separate from human beings but able to affect us on all levels. God is seen as a father or mother, and our relationship with other people is that of brothers and sisters. Prayer and meditation are methods of communicating with and attuning oneself to God, and all healing and moral guidance ultimately come from God. A variation of this model is applicable to polytheistic religions.
In the unity model (Figure 4 ▶), Maslow’s triangles are turned upside down. Here, the body is just the tip of the iceberg, and on a spiritual level, we are all one. In this model, we are part of God, as a wave is part of the ocean, and our relationship with other people is akin to limbs on the same body. Prayer and meditation are methods to connect with “God within” or the “Oneness of the universe,” and healing and ethical decisions arise from connecting with that oneness.
These 3 BMSEST models provide insight into the various ways people view spirituality and the transcendent, thus paving the way for more meaningful communication. They also emphasize that, in the clinical arena, the approaches to patient care (arrows f, g, h, i) are the same, regardless of the model variation most resonant with physician or patient. The choice of the most appropriate specific therapeutic intervention for the patient varies depending on the patient’s belief background.
SPIRITUALITY, SERVICE, AND ADVOCACY
The individual’s role in the health care system does not stop at the physician-patient relationship. The BMSEST models also illustrate the 2-way interaction between the individual and social and environmental factors (arrows d and e). Ideals and values (head), energized by inner strength and resilience (heart), can lead to profound action on a systems level (hands) to benefit the health of others. History abounds with examples of individuals, such as Mahatma Gandhi, Mother Teresa, and Martin Luther King, who harnessed spirituality to improve the social environment, with effects on many people’s health and quality of life. Research on altruism is beginning to elucidate some of the factors that influence this aspect of human experience.85
FINDING COMMON GROUND
For patient care, education, and research to successfully incorporate spirituality into whole-person care, it is essential that human spirituality be understood in universal terms, just as the human body and mind are considered universal. From the universal, we can appreciate normal variations, and from there, identify factors that affect health and well-being.
The 3 H’s (Table 1 ▶) provides a framework for understanding common spiritual themes. These themes are both explicitly and implicitly present in patients’ narratives and actions. By recognizing and responding to patients’ cues, we can allow patients to provide us with the language of spirituality that best suits them—whether religious or secular.
The BMSEST models (Figure 2 ▶, 3 ▶, 4 ▶) provide a theoretical framework for understanding the role of spirituality in whole-person care, applicable to all people. They also remind us of the existence of considerable variations in world views and images of God, while emphasizing the common therapeutic approaches available at the body, mind, and spirit levels. Optimal patient care requires a multidisciplinary team approach to navigate this complex system.
However, the true common ground and foundation for integrating spirituality into medicine lie in the healing attitude and self-awareness of the professional. Adopting a patient-centered approach, reflecting “spiritual humility,” akin to “cultural humility,”97 together with an attitude of service and advocacy, will likely yield better understanding and thus better therapeutic options than simply following established spiritual history protocols.98,99 In addition, unlike questions in other areas of medicine, many spiritual questions are unanswerable. Thus, it is often in the appreciation of the questions, rather than the provision of answers, that healing occurs.
CLINICAL AND EDUCATIONAL APPLICATIONS
The BMSEST models and the 3 H’s have many practical clinical and educational applications. The former remind clinicians of the layers of complexity in their patients’ experience of illness, and the latter provide a means for bridging cultural differences in spiritual beliefs and practices.
Example 1. Medical students can use the BMSEST framework (Figure 2 ▶) to develop a holistic diagnosis and treatment plan. For example, when learning about domestic violence, rape, and incest, they can visualize potential effects on patients’ physical health (eg, bruises, sexually transmitted diseases, chronic pain); mental health (eg, posttraumatic stress disorder, depression); spiritual health (eg, search for meaning, conflicts between beliefs and treatment options); social relationships (eg, disruption of family ties, contribution of alcohol and drugs, police and legal issues); and environment (eg, safety/emergency housing). Therapeutic options may include medications for sexually transmitted diseases (arrow f) or posttraumatic stress disorder (arrows f and a); counseling by a psychologist for anxiety (arrow g); procurement of housing in a homeless shelter by a social worker (arrow d); counseling by a clinical chaplain regarding treatment options for a pregnancy resulting from rape or incest (arrow h); and a safe, compassionate, therapeutic relationship (arrow i).
The 3 H model proves a useful tool for spiritual assessment during a medical encounter, as an alternative to existing tools.98,99 It helps clinicians recognize spiritual themes in their patients’ narratives and offers a common vocabulary for open-ended questions that can reveal the specific language of spirituality that a patient uses (religious or secular).
Example 2. A 59-year old hospitalized patient with metastatic lung cancer is struggling with the decision between hospice vs more chemotherapy. Her physician is struggling to control her severe pain because the patient is reluctant to increase the amount of pain medication. A picture of Jesus on her table cues her physician to learn more about her beliefs. The 3 H’s remind him to start with general spiritual questions. He learns that although the patient believes in God as Jesus, her specific language of spirituality is from the 12-Step recovery community. Because the physician has a compassionate, respectful attitude (BMSEST arrow i), she tells him more. She believes in the afterlife and that things happen for a reason (head), and she feels loved by God and does not fear death (heart); however, she is struggling with the hospice decision and pain management (hands) because of a conflict between her fear of pain and symptoms vs her fear that taking narcotics is against the beliefs of her spiritual community. She worries that she will lose her community and die alone, “addicted” to pain medications. These concerns needed to be addressed directly, with the help of her 12-Step community, in order for her to peacefully transition to hospice care. At the end of her life, her physician realizes that attention to his own spiritual 3 H’s gave him the strength to visit her bedside, when nothing was left to do except provide his presence.
Medical students and residents in the United States have diverse spiritual beliefs, ranging from devoutly religious (in different religions), to atheist, to undecided. The 3 H’s offer the opportunity for all learners to sit at the table when discussing spirituality and medicine.
Example 3. Educators (a physician and chaplain team) have successfully used the following small group exercise as an introduction to spirituality and medicine in required medical school clerkship sessions41 and resident education43: (1) ask learners to define spirituality, (2) organize their answers using the 3 H model, (3) using small group facilitation skills, provide a safe and respectful environment for students and residents to learn from each other about the variety of world views present in their own learning community, (4) expand the conversation to stories from learners about patient encounters in which spiritual issues played a role, and (5) facilitate a conversation regarding challenges and approaches. This technique introduces the concept of spirituality as a universal human experience and promotes cross-cultural discussion.
The 3 H and BMSEST models can also be used to nurture health care professionals’ self-understanding. These models help professionals clarify their own world view and provide tools for traversing cultural differences in spiritual beliefs and practices.
Example 4. A medical student, visibly shaken, tells her advisor about an upsetting experience in her community mentor’s office. Her mentor, whom she respects, started praying with a patient while the student was present. She was taken by surprise and felt trapped, confused, and scared. Her advisor can use the 3 H and BMSEST models as tools to debrief her experience by encouraging self-understanding regarding her response (she is undecided about her beliefs, and her family has experienced religious discrimination); facilitating her understanding of the positive experiences of the patient and her mentor in this situation; and exploring strategies for responding to prayer in the clinical setting. In addition, the advisor could use the BMSEST models as training tools in cross-cultural communication for clinicians interested in including spirituality in their work.
The 3 H and BMSEST models can also help promote physician self-care by acting as springboards for physicians to discover (and rediscover) their ideals, values, and purpose, and to explore methods to rejuvenate and sustain themselves during a challenging career. These methods, aimed at reenergizing the spiritual heart, can vary widely, depending on the individual physician, from religion-based activities, to secular activities, such as nature walks, dancing, and laughing with their children. Workshops regarding spiritual self-care have been valuable additions to medical education.42,43
RESEARCH APPLICATIONS
The 3 H and BMSEST models also have research applications. Elements of these models can be tested. A variety of methods might be used to evaluate the universality of the 3 H dimensions of spirituality and the extent to which current areas of research/study have a home within the BMSEST model. BMSEST homes for published studies include the following: meditation and health (arrow a, b, c, or j)4,5,13,17,52,56; religion and health (arrow b, c, or e)8,11,12,14,16,36; compassion and altruism (arrow i, d, or e)85; biologic mediators of spirituality (arrows b and c)17,46–55; consciousness studies, in the areas of mind and spirit (arrow b)32,33,45; and human energy systems (body, arrows a and c).57–59 The BMSEST models can also help identify which of the 6 components and 10 relationships (a to j) need further study.
The various subthemes within each of the 3 H dimensions of spirituality can be used to develop scales for measuring spiritual health, well-being, and need (for use in biomedical research). The 3 H’s can add to existing scales (reviewed elsewhere26,65) by providing a framework for ensuring that measures for each dimension are included in comprehensive scales and that studies regarding the relationships between various sub-themes (eg, effects of love, hope, forgiveness, meaning) can be conceptualized in a logical way. Future research could also elucidate the contributions of physical, mental, and spiritual health to overall quality of life.
Finally, because the BMSEST models include consideration of the transcendent, which is frequently defined as being outside the realm of the physical world, they raise the question of whether effects directly related to the transcendent (eg, arrow j) can be adequately studied using methods typically used in biomedical research. Many have debated this issue.100–102 Perhaps a deeper understanding of these effects can be gleaned only through direct experience and indirectly through qualitative methods, the arts, and the humanities.
In conclusion, the 3 H and BMSEST models provide a conceptual basis for approaching spirituality as a universal human phenomenon, essential to understanding whole-person medicine. Given the complexities of the human condition, future study regarding whole-person care will require innovative multimethod research and a multidisciplinary approach, encompassing science, social science, and the humanities. Although challenging, many opportunities exist for finding common ground between differing world views and discovering better ways to provide cure, relief, and above all comfort to suffering patients.
Acknowledgments
I thank the many medical students, residents, and colleagues who, over 11 years, have engaged in frank conversations about spirituality and health. I thank Denise Leclair, MD, Roger Mennillo, MD, the Brown Family Medicine Scholarship Promotion Committee, Jeffrey Borkan, MD, PhD, and Kohar Jones, MD, for reviewing this manuscript.
Conflicts of interest: none reported
REFERENCES
- 1.Lown B. The Lost Art of Healing. New York, NY: Ballantine Books; 1999.
- 2.Dixon DM, Sweeney KG, Pereira Gray DJ. The physician healer: ancient magic or modern science? Br J Gen Pract. 1999;49(441): 309–312. [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Global mortality, disability and the contribution of risk factors: global burden of disease study. Lancet. 1997;349(9063):1436–1442. [DOI] [PubMed] [Google Scholar]
- 4.Benson H, Malvea BP, Graham JR. Psysiologic correlates of meditation and their clinical effects in headache: an ongoing investigation. Headache. 1973;13(1):23–24. [DOI] [PubMed] [Google Scholar]
- 5.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation. Gen Hosp Psychiatry. 1982;4(1):33–47. [DOI] [PubMed] [Google Scholar]
- 6.Millison MB. A review of the research on spiritual care and hospice. Hosp J. 1995;10(4):3–18. [DOI] [PubMed] [Google Scholar]
- 7.Williams AL. Perspectives on spirituality at end of life: a meta-summary. Palliat Support Care. 2006;4(4):407–417. [DOI] [PubMed] [Google Scholar]
- 8.Matthews DA, McCullough ME, Larson DB, Koenig HG, Swyers JP, Milano MG. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med. 1998;7(2):118–124. [DOI] [PubMed] [Google Scholar]
- 9.Levin JS, Larson DB, Puchalski CM. Religion and spirituality in medicine: research and education. JAMA. 1997;278(9):792–793. [DOI] [PubMed] [Google Scholar]
- 10.Larimore WL, Parker M, Crowther M. Should clinicians incorporate positive spirituality into their practices? What does the evidence say? Ann Behav Med. 2002;24(1):69–73. [DOI] [PubMed] [Google Scholar]
- 11.Mueller PS, Plevak DJ, Rummans TA. Religious involvement, spirituality and medicine: implications for clinical practice. Mayo Clin Proc. 2001;76(12):1225–1235. [DOI] [PubMed] [Google Scholar]
- 12.Koenig HG. Religion, spirituality and medicine: implications for clinical practice. South Med J. 2004;97(12):1194–1200. [DOI] [PubMed] [Google Scholar]
- 13.Benson H, Stark M. Timeless Healing: The Power and Biology of Belief. New York, NY: Scribner; 1996.
- 14.Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. New York, NY: Oxford University Press; 2001.
- 15.Weaver AJ, Flannelly KJ, Oppenheimer JE. Religion, spirituality and chaplains in the biomedical literature 1965–2000. Int J Psychiatry Med. 2003;33(2):155–161. [DOI] [PubMed] [Google Scholar]
- 16.Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: linkages to physical health. Am Psychol. 2003;58(1):36–52. [DOI] [PubMed] [Google Scholar]
- 17.Seeman TE, Dublin LF, Seeman M. Religion/spirituality and health: a critical review of the evidence for biologic pathways. Am Psychol. 2003;58(1):53–63. [DOI] [PubMed] [Google Scholar]
- 18.Thoresen CE, Harris AHS. Spiritulity and health: what’s the evidence and what’s needed? Ann Behav Med. 2002;24(1):3–13. [DOI] [PubMed] [Google Scholar]
- 19.Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen-Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med. 1999;159(15):1803–1806. [DOI] [PubMed] [Google Scholar]
- 20.McCord G, Gilchrist VJ, Grossman SD, et al. Discussing spirituality with patients: a rational and ethical approach. Ann Fam Med. 2004;2(4):356–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oyama O, Koenig HG. Religious beliefs and practices in family medicine. Arch Fam Med. 1998;7(5):431–435. [DOI] [PubMed] [Google Scholar]
- 22.Learning objectives for medical student education—guidelines for medical schools: report I of the Medical School Objectives Project. Acad Med. 1999;74(1):461–462. [DOI] [PubMed] [Google Scholar]
- 23.WHOQOL SRPB Group. A cross-cultural study of spirituality, religion and personal beliefs as components of quality of life. Soc Sci Med. 2006;62(6):1486–1497. [DOI] [PubMed] [Google Scholar]
- 24.Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137(5):535–544. [DOI] [PubMed] [Google Scholar]
- 25.Borrell-Carrio F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice and scientific inquiry. Ann Fam Med. 2004;2(6):576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sulmasy DP. A biopsychosocial-spiritual model for the care of patients at the end of life. Gerontologist. 2002;42(Spec No 3):24–33. [DOI] [PubMed] [Google Scholar]
- 27.McKee DD, Chappel JN. Spirituality and medical practice. J Fam Pract. 1992;35(2):201, 205–208. [PubMed] [Google Scholar]
- 28.Ben-Arye E, Bar-Sela G, Frenkel M, Kuten A, Hermoni D. Is a biopsychosocial-spiritual approach relevant to cancer treatment? A study of patients and oncology staff members on issues of complementary medicine and spirituality. Support Care Cancer. 2006;14(2):147–152. [DOI] [PubMed] [Google Scholar]
- 29.Hutchinson ED. A working model. In: Hutchinson ED, Matto HC, Harrigan MP, Charlesworth LW, Viggiani PA. Challenges of Living: A Multidimensional Working Model for Social Workers. Thousand Oaks, CA: Sage Publications, Inc; 2007.
- 30.Ellis MR, Vinson DC, Ewigman B. Addressing the spiritual concerns of patients: family physicians’ attitudes and practices. J Fam Pract. 1999;48(2):105–109. [PubMed] [Google Scholar]
- 31.Fitchett G. Assessing Spiritual Needs: A Guide for Caregivers. Lima, OH: Academic Renewal Press; 2002.
- 32.Wilber K. Integral Psychology: Consciousness, Spirit, Psychology, Therapy. Boston, MA: Shambhala Publications; 2000.
- 33.Wilber K. Waves, Streams, States and Self: A Summary of My Psychological Model. Boston, MA: Shambhala Publications; 2000.
- 34.Astin JA, Astin AW. An integral approach to medicine. Altern Ther Health Med. 2002;8(2):70–75. [PubMed] [Google Scholar]
- 35.Friedmann ML, Mouch J, Racey T. Nursing the spirit: the framework of systemic organization. J Adv Nurs. 2002;39(4):325–332. [DOI] [PubMed] [Google Scholar]
- 36.Koenig HG, Hays JC, George LK, Blazer DG, Larson DB, Lander-man LR. Modeling the cross-sectional relationship between religion, physical health, social support and depressive symptoms. Am J Geriatr Psychiatry. 1997;5(2):131–144. [PubMed] [Google Scholar]
- 37.Buck HG. Spirituality: concept analysis and model development. Holist Nurs Pract. 2006;20(6):288–292. [DOI] [PubMed] [Google Scholar]
- 38.Miner-Williams D. Putting the puzzle together: making spirituality meaningful for nursing using an evolving theoretical framework. J Clin Nurs. 2006;15(7):811–821. [DOI] [PubMed] [Google Scholar]
- 39.Narayanasamy A. ASSET: a model for actioning spirituality and spiritual care education and training in nursing. Nurse Educ Today. 1999;19(4):274–285. [DOI] [PubMed] [Google Scholar]
- 40.Purdy M, Dupey PA. Holistic flow model of spiritual wellness. Couns Values. 2005;49(2):95–106. [Google Scholar]
- 41.Anandarajah G, Mitchell M, Stumpff J. Evaluation of a required spirituality and medicine teaching session in the family medicine clerkship. Fam Med. 2007;39(5):311–312. [PubMed] [Google Scholar]
- 42.Anandarajah G, Mitchell M. A spirituality and medicine elective for senior medical students: 4 years’ experience, evaluation and expansion to the family medicine residency. Fam Med. 2007;39(5):313–315. [PubMed] [Google Scholar]
- 43.Anandarajah G, Long R, Smith M. Integrating spirituality and medicine into the residency curriculum. Acad Med. 2001;76(5):519–520. [DOI] [PubMed] [Google Scholar]
- 44.Maslow AH. Motivation and Personality. 2nd ed. New York, NY: Harper and Row; 1970.
- 45.Koltko-Rivera ME. Rediscovering the later version of Maslow’s hierarchy of needs: self-transcendence and opportunities for theory, research, and unification. Rev Gen Psychol. 2006;10(4):302–317. [Google Scholar]
- 46.Borg J, Andree B, Soderstrom H, Farde L. The serotonin system and spiritual experience. Am J Psychiatry. 2004;160(11):1965–1969. [DOI] [PubMed] [Google Scholar]
- 47.Kurup RK, Kurup PA. Hypothalamic digoxin, hemispheric chemical dominance and spirituality. Int J Neurosci. 2003;113(3):383–393. [DOI] [PubMed] [Google Scholar]
- 48.McCain NL. Psychoneuroimmunology, spirituality and cancer. Gynecol Oncol. 2005;99(3 Suppl 1):S121. [DOI] [PubMed] [Google Scholar]
- 49.Sephton SE, Koopman C, Schaal M, Thoresen C, Spiegel D. Spiritual expression and immune status in women with metastatic breast cancer: an exploratory study. Breast J. 2001;7(5):345–353. [DOI] [PubMed] [Google Scholar]
- 50.Austin J. Zen and the Brain. Cambridge, MA: MIT Press; 1998.
- 51.Newberg A, D’Aquili E, Rause V. Why God Won’t Go Away: Brain Science and the Biology of Belief. New York, NY: Ballantine Books; 2001.
- 52.Lazar SW, Bush G, Gollub RL, Fricchione GL, Khelsa G, Benson H. Functional brain mapping of the relaxation response and meditation. Neuroreport. 2000;11(7):1581–1585. [PubMed] [Google Scholar]
- 53.Fricchione G, Daly R, Rogers MP, Stefano GB. Neuroimmunologic influences in neuropsychiatric and psychophysiologic disorders. Acta Pharmacol Sin. 2001;22(7):577–587. [PubMed] [Google Scholar]
- 54.Fricchione G, Stefano GB. Placebo neural systems: nitric oxide, morphine and dopamine brain reward and motivation circuitries. Med Sci Monit. 2005;11(5):MS54–MS65. [PubMed] [Google Scholar]
- 55.Koenig HG, Cohen HJ. The Link Between Religion and Health: Psychoneuroimmunology and the Faith Factor. New York, NY: Oxford University Press; 2002.
- 56.Stefano GB, Esch T. Integrative medical therapy: examination of meditation’s therapeutic and global medical outcomes via nitric oxide [review]. Int J Mol Med. 2005;16(4):621–630. [PubMed] [Google Scholar]
- 57.Rubik B. The biofield hypothesis: its biophysical basis and role in medicine. J Altern Complement Med. 2002;8(6):703–717. [DOI] [PubMed] [Google Scholar]
- 58.Rein G. Bioinformation within the biofield: beyond bioelectromagnetics. J Altern Complement Med. 2004;10(1):59–68. [DOI] [PubMed] [Google Scholar]
- 59.Bell IR, Baldwin CM, Schwartz GE. Translating a nonlinear systems theory model for homeopathy into empirical tests. Altern Ther Health Med. 2002;8(3):58–66. [PubMed] [Google Scholar]
- 60.Jung CG. Psychology and Religion. New Haven, CT: Yale University Press; 1938.
- 61.Fowler JW. Stages of Faith: The Psychology of Human Development and the Quest for Meaning. San Francisco, CA: HarperCollins; 1981.
- 62.Division of Mental Health and Prevention of Substance Abuse. World Health Organization. WHOQOL. Measuring Quality of Life. http://www.who.int/mental_health/media/68.pdf. Accessed Aug 20, 2008.
- 63.McBrien B. A concept analysis of spirituality. Br J Nurs. 2006;15(1): 42–45. [DOI] [PubMed] [Google Scholar]
- 64.Miller WR, Thoresen CE. Spirituality, religion and health: an emerging research 3 eld. Am Psychol. 2003;58(1):24–35. [DOI] [PubMed] [Google Scholar]
- 65.Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality: implications for physical and mental health research. Am Psychol. 2003;58(1):64–74. [DOI] [PubMed] [Google Scholar]
- 66.Zinnbauer BJ, Pargament KI, Cole B, et al. Religion and spirituality: unfuzzing the fuzzy. J Sci Study Relig. 1997;36(4):549–564. [Google Scholar]
- 67.Shea J. Spirituality and Health Care: Reaching Towards a Holistic Future. Chicago, IL: Park Ridge Center; 2000.
- 68.Sathya Sai. Education in Human Values. Philosophy of SSEHV. http://www.ssehvusa.org/phil.html. Accessed Aug 20, 2008.
- 69.Head, Heart, Hands Diversity Leadership [Web site]. http://www.Headhearthands.com/main.phtml. Accessed Aug 20, 2008.
- 70.Head, Heart, Hands Framework. Singapore Ministry of Education. National Education Branch. http://www.ne.edu.sg/hhh_framework.htm. Accessed Aug 20, 2008.
- 71.Head, Heart & Hand Art Studio [Web site]. http://www.head-heart-hand.com/. Accessed Aug 20, 2008.
- 72.Hall DE, Koenig HG, Meador KG. Conceptualizing “religion”: how language shapes and constrains knowledge in the study of religions and health. Perspect Biol Med. 2004;47(3):386–401. [DOI] [PubMed] [Google Scholar]
- 73.Smith H. Why Religion Matters: The Fate of the Human Spirit in an Age of Disbelief. San Francisco, CA: HarperSanFrancisco; 2001.
- 74.Handzo G, Koenig HG. Spiritual care: whose job is it anyway? South Med J. 2004;97(12):1242–1244. [DOI] [PubMed] [Google Scholar]
- 75.Puchalski CM, Lunsford B, Harris MH, Miller RT. Interdisciplinary spiritual care for seriously ill and dying patients: a collaborative model. Cancer J. 2006;12(5):398–416. [DOI] [PubMed] [Google Scholar]
- 76.Post SG, Puchalski CM, Larson DB. Physician and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med. 2000;132(7):578–583. [DOI] [PubMed] [Google Scholar]
- 77.O’Connor PM. Spiritual elements of hospice care. Hosp J. 1986; 2(2):99–108. [PubMed] [Google Scholar]
- 78.Cassel CK. The patient-physician covenant: an affirmation of Asklepios. Conn Med. 1996;60(5):291–293. [PubMed] [Google Scholar]
- 79.Cruess RL, Cruess SR. Teaching medicine as a profession in the service of healing. Acad Med. 1997;72(11):941–952. [DOI] [PubMed] [Google Scholar]
- 80.Novack DH, Epstein RM, Paulsen RH. Towards creating physician-healers: fostering medical students’ self-awareness, personal growth and well-being. Acad Med. 1999;74(5):516–520. [DOI] [PubMed] [Google Scholar]
- 81.Miller WL, Crabtree BF. Healing landscapes: patients, relationships, and creating optimal healing places. J Altern Complement Med. 2005;11(Suppl 1):S41–S49. [DOI] [PubMed] [Google Scholar]
- 82.Balint M. The Doctor, His Patient and the Illness. London, England: Pitman Medical; 1952.
- 83.Epstein RM. Mindful practice. JAMA. 1999;282(9):833–839. [DOI] [PubMed] [Google Scholar]
- 84.Frank AW. Asking the right questions about pain: narratives and phronesis. Lit Med. 2004;23(2):209–225. [DOI] [PubMed] [Google Scholar]
- 85.Post SG, Underwood LG, Schloss JP, Hurlbut WB, eds. Altruism and Altruistic Love: Science, Philosophy, and Religion in Dialogue. New York, NY: Oxford University Press; 2002.
- 86.The Alan Mason Chesney Medical Archives of the Johns Hopkins Medical Institutions. Osler W. Aequanimitas. http://www.medica-larchives.jhmi.edu/osler/aequessay.htm. Accessed Aug 20, 2008.
- 87.Fricchione GL. Separation, attachment and altruistic love: the evolutionary basis for medical caring. In: Altruism and Altruistic Love. New York, NY: Oxford University Press; 2002.
- 88.Remen RN. Kitchen Table Wisdom: Stories That Heal. New York, NY: Riverhead Books; 1996.
- 89.Scannell K. Writing for our lives: physician narratives and medical practice. Ann Intern Med. 2002;137(9):779–781. [DOI] [PubMed] [Google Scholar]
- 90.Borkan JM, Reis S, Medalie JH, Steinmetz D. Patients and Doctors: Life-Changing Stories From Primary Care. Madison, WI: University of Wisconsin Press; 1999.
- 91.Smith H. The World’s Religions: Our Great Wisdom Traditions. San Francisco, CA: HarperCollins; 1991.
- 92.Jung CG. Psychology and the East. Princeton, NJ: Princeton University Press; 1978.
- 93.Jung CG. Psychology and Western Religion. Princeton, NJ: Princeton University Press; 1984.
- 94.James W. The Varieties of Religious Experience. New York, NY: New American Library; 1958.
- 95.Campbell J. The Hero With a Thousand Faces. Princeton, NJ: Princeton University Press; 1990.
- 96.Eliade M. The Sacred and Profane: The Nature of Religion. Orlando, FL: Harcourt, Inc; 1959.
- 97.Tervalon M, Murray-Carcia J. Cultural humility vs. cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117–125. [DOI] [PubMed] [Google Scholar]
- 98.Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician. 2001;63(1):81–88. [PubMed] [Google Scholar]
- 99.Puchalski C, Romer AL. Taking a spiritual history allows clinicians to understand patients more fully. J Palliat Med. 2003;3(1):129–137. [DOI] [PubMed] [Google Scholar]
- 100.Turner DD. Just another drug? A philosophical assessment of randomized controlled studies on intercessory prayer. J Med Ethics. 2006;32(8):487–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Halperin EC. Should academic medical centers conduct clinical trials of the efficacy of intercessory prayer? Acad Med. 2001;76(8):791–797. [DOI] [PubMed] [Google Scholar]
- 102.Olshansky B, Dossey L. Retroactive prayer: a preposterous hypothesis? BMJ. 2003;327(7429):1465–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]