Abstract
INTRODUCTION
Most clinical clerks (third-year medical students) do their paediatric rotation at the IWK Health Centre, the Dalhousie University-affiliated tertiary care paediatric institution in Halifax, Nova Scotia. Due to limited space, some clerks are sent to community hospitals in the provinces of New Brunswick and Prince Edward Island. These community hospitals are different in terms of the academic environment and the availability of paediatric subspecialty services.
OBJECTIVE
To compare performance of clinical clerks doing paediatric rotations in community hospitals (group I) with those in a university hospital (group II).
METHODS
The end-of-rotation test scores on the 45 single correct answer multiple choice questions and the three 15 min objective structured clinical examinations in group I (n=54) and group II (n=124) for two consecutive academic years were studied. The end-of-rotation comments by the clerks in group I were examined to assess the quality of their experience.
RESULTS
For the two academic years, the cumulative mean ± SD scores for multiple choice questions and objective structured clinical examinations were 82.82±7.47 and 70.82±11.37, respectively, in group I compared with 83.03±7.74 and 69.02±11.23 in group II. There were no significant differences in the results between the two groups. No difference in results was seen when the scores were analyzed separately for each of the academic years. The clerks in group I rated their experience as positive.
CONCLUSIONS
Clerks doing paediatric rotations in community hospitals perform as well and receive similar educational benefits as those at university hospitals. Community hospitals can provide a quality experience for paediatric clerkship training.
Keywords: Clinical clerks, Community hospital, Paediatric rotation, Performance, University hospital
Abstract
INTRODUCTION
La plupart des externes (les étudiants en médecine de troisième année) font leur rotation de pédiatrie au IWK Health Centre, l’établissement de pédiatrie tertiaire affilié à l’université Dalhousie de Halifax, en Nouvelle-Écosse. En raison de l’espace limité, certains externes sont envoyés dans des hôpitaux généraux du Nouveau-Brunswick et de l’Île-du-Prince-Édouard. Ces hôpitaux généraux diffèrent du point de vue du milieu universitaire et des services surspécialisés en pédiatrie.
OBJECTIF
Comparer le rendement d’externes qui font leur rotation en pédiatrie dans un hôpital général (groupe I) à ceux qui la font dans un hôpital universitaire (groupe II).
MÉTHODOLOGIE
L’auteur a étudié les résultats au test de fin de rotation, comportant 45 réponses uniques à des questions à choix multiples et aux trois examens cliniques structurés objectifs de 15 minutes dans le groupe I (n=54) et le groupe II (n=124) pendant deux années consécutives. Il a examiné les commentaires de fin de rotation des externes du groupe I afin d’évaluer la qualité de leur expérience.
RÉSULTATS
Pendant ces deux années universitaires, les résultats moyens cumulatifs ± ÉT aux questions à choix multiples et aux examens cliniques structurés objectifs étaient de 82,82±7,47 et de 70,82±11,37, respectivement, au sein du groupe I, par rapport à 83,03±7,74 et 69,02±11,23 au sein du groupe II. On n’a remarqué aucune différence significative des résultats dans les deux groupes. De plus, ils ne différaient pas lorsqu’on les calculait séparément pour chacune des deux années universitaires. Les externes du groupe I ont qualifié leur expérience de positive.
CONCLUSIONS
Les externes qui font leur rotation en pédiatrie dans un hôpital général réussissent bien et profitent du milieu d’enseignement de manière similaire à ceux qui évoluent dans un hôpital universitaire. Ainsi, les hôpitaux généraux peuvent offrir une expérience de qualité pendant la formation des externes en pédiatrie.
Despite the curriculum changes over the past decade, there are still differences in the structure of paediatric clerkships across American and Canadian medical schools (1,2). At Dalhousie University (Halifax, Nova Scotia), there are approximately 90 students in each year of medical training. The medical students do a six-week rotation in the discipline of paediatrics during their third year of medicine (clinical clerkship). This rotation consists of three weeks of inpatient ward work and three weeks of ambulatory experience consisting of outpatient clinics and paediatric emergency medicine. Most clinical clerks do their paediatric rotation at the IWK Health Centre in Halifax, Nova Scotia, which is the Dalhousie University-affiliated tertiary care paediatric institution. It is the only tertiary care paediatric hospital in the Maritimes and provides a full range of paediatric subspecialty services.
Due to limited space at the university hospital, approximately one-third of the clerks are sent to community hospitals in other Maritime provinces. These off-sites include the Saint John Regional Hospital (Saint John, New Brunswick) and the Queen Elizabeth Hospital (Charlottetown, Prince Edward Island). These hospitals are the regional referral institutions for the two provinces. They are equipped with a paediatric ward and a group of primary paediatricians, but they lack most paediatric subspecialty services and dedicated paediatric emergency departments. The academic environment of a university institution is also not available in these hospitals. Each hospital has a paediatrician who acts as the clerkship coordinator for that region. The clerks are given the choice of selecting their site of rotation. If more than the desired number want to go to a particular site, the clerks decide on the final placements by mutual discussion among themselves.
Training in the community hospitals is important because that is where most medicine is practiced. This adds to the value of the experience in the long run. However, there have been concerns that learning in these community centres may not be optimal for clinical clerks, because they do not get exposure to a wide spectrum of paediatric problems due to limited number of patients available. There can be significant variations in the case mixes, and in the exposure to diagnostics and therapeutics, for students rotating through a university hospital versus a community hospital (3,4). Sometimes the students express reservations regarding their rotation at a smaller community hospital in terms of getting the necessary experience in paediatric medicine, both for learning and for passing the examinations.
OBJECTIVES
The primary purpose of the study was to compare the performance of clinical clerks doing paediatric rotations in community hospitals with those at a university hospital. The experience of clinical clerks doing rotations at the community hospitals was also assessed.
METHODS
To enter clinical clerkship, all students had successfully completed two years of undergraduate medical education at Dalhousie University and had passed all the examinations. They had all received a standard curriculum, including practical sessions and lectures on paediatric clinical skills. At the beginning of the clerkship, all students attended a one-month ‘Introduction to Clerkship’ at the university, which consisted of several seminars and lectures on a variety of topics in all specialties, including paediatrics. The objectives of the clerkship rotation were available to the coordinators at the community hospitals and the attending staff at the university hospital. They were also provided to all the clerks in advance.
The type of teaching at the university hospital included inpatient ward rounds under the paediatric medical unit, shifts in the emergency department and attendance at the outpatient ambulatory clinics, both in general paediatrics and in a variety of paediatric medical and surgical subspecialties. The teaching methods used at the community hospitals were more varied, given the difference in resources, and were left to the discretion of the attending staff, as long as they conformed to the objectives of the rotation. These included inpatient rounds, attending ambulatory clinics and seeing paediatric patients in consultation in the emergency department. The main didactic educational activity at the university hospital was a 1 h tutorial held every afternoon on a variety of paediatric topics. These were teleconferenced to the clerks rotating through the two community hospitals.
After the completion of their paediatric rotations, the clinical clerks were examined on their knowledge, skills and attitudes. The examination was comprised of two components: testing on 45 single correct answer multiple choice questions (MCQs) and three 15 min objective structured clinical examinations (OSCEs). The clinical clerks doing their rotations at the two out-of-province community hospitals (group I) and at the university hospital (group II) took the same examination. The examinations were held on a quarterly basis at Dalhousie University. The test items contained in the MCQs and the OSCEs varied each quarter, but the minimum passing marks and the methods of scoring remained unchanged. At the end of their paediatric rotations, the clinical clerks were invited to comment on their experiences. This consisted of three open-ended questions, including what the student enjoyed the most about the rotation, what needed to be improved and any other comments. The comments by the clerks were optional. The Paediatric Undergraduate Medical Education Office collected this information anonymously without identifying the names of the students.
The end-of-rotation test scores on the MCQs and the OSCEs for two consecutive cohorts of clerks (third-year medical students) for academic years 2002 to 2003 and 2003 to 2004 were obtained from the Undergraduate Medical Education Office of Dalhousie University. The data were provided with complete anonymity by removing the names of the clinical clerks or any other means of identification. The data were pooled for the two out-of-province community hospitals. The MCQ and the OSCE scores of clerks in group I were compared with the respective scores of those in group II. Student’s t test was used to examine differences between the two groups. P<0.05 was considered significant.
The end-of-rotation comments by the clinical clerks in group I were examined. These comments were collected anonymously without the student’s names appearing on the form. The handwritten comments were transcribed for review. Major themes were identified from the comments to assess the quality of experience.
RESULTS
There were 27 clinical clerks in group I and 62 in group II for each of the academic years studied. For the two years, a total of 54 clerks were in group I (39 clerks in Saint John, New Brunswick, and 15 clerks in Charlottetown, Prince Edward Island) and 124 in group II (Halifax, Nova Scotia). Tables 1 and 2 show the results of the MCQs and the OSCEs, respectively, for each of the academic years for the two groups. The scores for the two groups were not significantly different for either the MCQs or the OSCEs.
TABLE 1.
Results of multiple choice questions for each academic year according to group
| Group I (n=27) | Group II (n=62) | P | |
|---|---|---|---|
| Academic year 2002 to 2003 | |||
| Score (mean ± SD) | 82.91±7.32 | 84.16±8.64 | 0.51 |
| Range | 67.39–95.45 | 58.70–100 | |
| Academic year 2003 to 2004 | |||
| Score (mean ± SD) | 82.74±7.76 | 81.91±6.61 | 0.60 |
| Range | 63.04–95.56 | 66.67–95.45 | |
Group I – community hospital;
Group II – university hospital;
TABLE 2.
Results of objective structured clinical examinations for each academic year according to group
| Group I (n=27) | Group II (n=62) | P | |
|---|---|---|---|
| Academic year 2002 to 2003 | |||
| Score (mean ± SD) | 69.14±10.98 | 67.01±11.25 | 0.41 |
| Range | 40.48–88.89 | 38.10–92.11 | |
| Academic year 2003 to 2004 | |||
| Score (mean ± SD) | 72.97±11.59 | 71.60±10.72 | 0.59 |
| Range | 42.11–100 | 34.21–94.44 | |
Group I – community hospital;
Group II – university hospital;
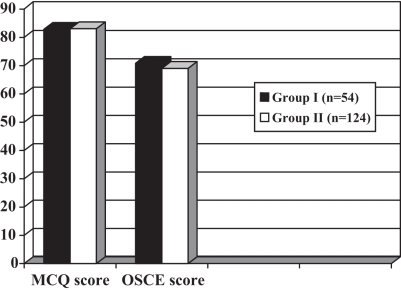
Figure 1 shows the cumulative results of the MCQs and the OSCEs for the two academic years. The mean ± SD score of the MCQs were 82.82±7.47 (range 63.04 to 95.56) for group I and 83.03±7.74 (range 58.70 to 100) for group II. The mean ± SD score of the OSCEs were 70.82±11.37 (range 42.11 to 100) for group I and 69.02±11.23 (range 34.21 to 94.44) for group II. There was no difference in the scores of either the MCQs (P=0.86) or the OSCEs (P=0.32) between the two groups.
Figure 1.
Cumulative results of the multiple choice question (MCQ) examination and the objective structured clinical examination (OSCE) groups for two academic years. Group I – community hospital; Group II – university hospital
Two students failed the MCQs and the OSCEs. Both of these students were from group II.
The end-of-rotation comments were available from 28 clerks (52%) doing rotations in the community hospitals (group I). The comments were variable but generally positive. Most clerks believed that the opportunity for patient care was adequate. The teaching by the staff was described as satisfactory. Things that needed improvement included more exposure to inpatient care opportunities and better structured teaching. The presence of a paediatric resident was thought to be important for supervised clinical care. Overall, the clerks found it to be an enjoyable experience.
DISCUSSION
The performance of clinical clerks receiving training at the community hospitals has been assessed in several disciplines of medicine and surgery (5–18). In paediatrics, studies looking at the performance of clinical clerks in community versus university institutions have provided variable results. Some studies (19–21) have found no difference in the performance between the two groups, while others (22) report differences in learning experience and a higher failure rate in students doing ambulatory rotations in the community. These conflicting results could be due to several factors, including the lack of standardized curriculum, differences in measuring performance outcome and variations in assessing the learning experience. No data are available on this subject from Canadian medical schools.
The student performance can be assessed using a variety of tools, including in-training evaluation reports, MCQs and OSCEs. At our institution, the students receive a pass or fail on their in-training evaluation reports; thus, this nongraded tool would not provide a comparative measure between different groups. The MCQ and OSCE results were studied because these were thought to be the best objective measures of student performance. The present study shows that clerks in community hospitals perform as well as their colleagues in the university hospital. Two cohorts of clerks were studied to ensure that the findings of the first cohort were true and sustained. The results were remarkably consistent for the two academic years studied, providing further validity to the findings.
The examination results studied provided a measure of performance in the short term because the testing was held close to the end of the rotation, when the knowledge and skills acquired were relatively fresh. It is not known whether this performance is maintained in the longer term in later testing, including the national licensing examinations. Also, the effect on actual clinical practice in later years is unknown.
Recently, with increased enrolments in the medical schools and limited funding, there is tremendous pressure on the resources of university-affiliated hospitals. Over time, this pressure is expected to increase and more clerks will have to be sent to other sites for their clinical rotations. More importantly, most medicine is practiced in the community, and training in such a setting is invaluable. It provides the students with hands-on experience, because they are exposed to both common and complex problems in a real-life setting. Community-based educational experiences have been recommended for the paediatric curriculum (23) and may also positively affect the student’s decision to take up paediatrics as a career choice (24). For these reasons, it is desirable to send more clinical clerks to community hospitals for training.
The present study reveals that where the clerks are placed for their rotations has little influence on their final performance. To maintain consistency in performance, the focus should be on defining the objectives of the curriculum and supervision by qualified staff. The didactic and structured teaching sessions should be shared with the remote sites using technologies for distributed learning. The end-of-rotation comments and suggestions made by clerks should be used to make necessary changes in their training to further improve their educational experience. Of note, all of the clerks in the study shared the same curriculum in the two preclerkship years. They were exposed to similar opportunities of knowledge acquisition, and this consistency may also account for the comparable performance on examination after the clinical rotation.
The results of the present study are also a source of reassurance to the clinical clerks going to community hospitals for their paediatric rotations in that, despite being in a different learning environment, their performance is comparable with their colleagues in a larger academic centre. The vast majority of them also seemed to enjoy the community learning experience. Since the present study, the Department of Paediatrics at Dalhousie University has expanded its sites of clerkship rotation to three other community hospitals in Nova Scotia and one more in Prince Edward Island.
The study was limited to a defined geographical area involving specific institutions. The preclerkship curriculum was also standardized for all students. The results may not be generalizable to other institutions with different resources and curriculum.
CONCLUSIONS
When measured on standard examination techniques, the clinical clerks doing paediatric rotations in community hospitals performed as well as those at university hospitals and also found the experience enjoyable. Community hospitals can provide a quality experience for paediatric clerkship training.
Acknowledgements
The author thanks Bernice MacLellan (Paediatric Undergraduate Medical Education Office) for her help in organizing some of the material for the study.
REFERENCES
- 1.Olson AL, Woodhead J, Berkow R, Kaufman NM, Marshall SG. A national general pediatric clerkship curriculum: The process of development and implementation. Pediatrics. 2000;106:216–22. [PubMed] [Google Scholar]
- 2.Kumar A, Gera R, Shah G, Godambe S, Kallen DJ. Student evaluation practices in pediatric clerkships: A survey of the medical schools in the United States and Canada. Clin Pediatr (Phila) 2004;43:729–35. doi: 10.1177/000992280404300807. [DOI] [PubMed] [Google Scholar]
- 3.Rattner SL, Louis DZ, Rabinowitz C, et al. Documenting and comparing medical students’ clinical experiences. JAMA. 2001;286:1035–40. doi: 10.1001/jama.286.9.1035. [DOI] [PubMed] [Google Scholar]
- 4.McCurdy FA, Sell DM, Beck GL, Kerber K, Larzelere RE, Evans JH. A comparison of clinical pediatric patient encounters in university medical center and community private practice settings. Ambul Pediatr. 2003;3:12–5. doi: 10.1367/1539-4409(2003)003<0012:acocpp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 5.Carney PA, Eliassen MS, Pipas CF, Genereaux SH, Nierenberg DW. Ambulatory care education: How do academic medical centers, affiliated residency teaching sites, and community-based practices compare? Acad Med. 2004;79:69–77. doi: 10.1097/00001888-200401000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Greer T, Schneeweiss R, Baldwin LM. A comparison of student clerkship experiences in community practices and residency-based clinics. Fam Med. 1993;25:322–6. [PubMed] [Google Scholar]
- 7.Carney PA, Pipas CF, Eliassen MS, et al. An analysis of students’ clinical experiences in an integrated primary care clerkship. Acad Med. 2002;77:681–7. doi: 10.1097/00001888-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Packman CH, Krackov SK, Groff GD, Cohen J. The Rochester practice-based experience. An experiment in medical education. Arch Intern Med. 1994;154:1253–60. [PubMed] [Google Scholar]
- 9.Butterfield PS, Libertin AG. Learning outcomes of an ambulatory care rotation in internal medicine for junior medical students. J Gen Intern Med. 1993;8:189–92. doi: 10.1007/BF02599265. [DOI] [PubMed] [Google Scholar]
- 10.Leone-Perkins M, Schnuth RL, Lipsky MS. Students’ evaluations of teaching and learning experiences at community- and residency-based practices. Fam Med. 1999;31:572–7. [PubMed] [Google Scholar]
- 11.Prislin MD, Fitzpatrick CF, Radecki S. A comparison of family medicine clerkship student performance across multiple teaching sites. Fam Med. 1998;30:279–82. [PubMed] [Google Scholar]
- 12.Williams M, Ambrose M, Carlin AM, Tyburski JG, Steffes CP. Evaluation of academic and community surgery clerkships at a Midwestern medical school. J Surg Res. 2004;116:11–3. doi: 10.1016/s0022-4804(03)00312-3. [DOI] [PubMed] [Google Scholar]
- 13.Kroot LJ, Barlow W, Murphy-Spencer A. Comparison and evaluation of the clinical experience of fourth-year medical students in a mandatory emergency medicine clerkship at university and community hospitals. Med Teach. 2001;23:310–12. doi: 10.1080/01421590120048148. [DOI] [PubMed] [Google Scholar]
- 14.deLahunta EA, Bazarian J. University and community hospital medical student emergency medicine clerkship experiences. Acad Emerg Med. 1998;5:343–6. doi: 10.1111/j.1553-2712.1998.tb02717.x. [DOI] [PubMed] [Google Scholar]
- 15.Potts M. Rural community health agencies as primary care clerkship sites for medical students. Fam Med. 1994;26:632–7. [PubMed] [Google Scholar]
- 16.Fincher RM, Case SM, Ripkey DR, Swanson DB. Comparison of ambulatory knowledge of third-year students who learned in ambulatory settings with that of students who learned in inpatient settings. Acad Med. 1997;72:S130–2. doi: 10.1097/00001888-199710001-00044. [DOI] [PubMed] [Google Scholar]
- 17.Calhoun JG, Davis WK, Erlandson EE, Maxim BR. A multisite comparison of student activities in the surgery clerkship. Surgery. 1982;91:622–7. [PubMed] [Google Scholar]
- 18.Talbert LM, Stritter FT, Riddle MH. A clinical clerkship in a multicenter setting: An appraisal. J Reprod Med. 1981;26:421–4. [PubMed] [Google Scholar]
- 19.McCurdy FA, Beck GL, Kollath JP, Harper JL. Pediatric clerkship experience and performance in the Nebraska Education Consortium: A community vs university comparison. Arch Pediatr Adolesc Med. 1999;153:989–94. doi: 10.1001/archpedi.153.9.989. [DOI] [PubMed] [Google Scholar]
- 20.White CB, Thomas AM. Students assigned to community practices for their pediatric clerkship perform as well or better on written examinations as students assigned to academic medical centers. Teach Learn Med. 2004;16:250–4. doi: 10.1207/s15328015tlm1603_5. [DOI] [PubMed] [Google Scholar]
- 21.Satran L, Harris IB, Allen S, Anderson DC, Poland GA, Miller WL. Hospital-based versus community-based clinical education: Comparing performances and course evaluations by students in their second-year pediatrics rotation. Acad Med. 1993;68:380–2. doi: 10.1097/00001888-199305000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Malloy MH, Speer A. A comparison of performance between third-year students completing a pediatric ambulatory rotation on campus vs in the community. Arch Pediatr Adolesc Med. 1998;152:397–401. doi: 10.1001/archpedi.152.4.397. [DOI] [PubMed] [Google Scholar]
- 23.Scheiner AP. Guidelines for medical student education in community-based pediatric offices. American Academy of Pediatrics Council on Pediatric Education Subcommittee on Medical Student Curriculum. Pediatrics. 1994;93:956–9. [PubMed] [Google Scholar]
- 24.Jospe N, Kaplowitz PB, McCurdy FA, Gottlieb RP, Harris MA, Boyle R. Third-year medical student survey of office preceptorships during the pediatric clerkship. Arch Pediatr Adolesc Med. 2001;155:592–6. doi: 10.1001/archpedi.155.5.592. [DOI] [PubMed] [Google Scholar]