Abstract
Objective
To determine if cesarean delivery for breech has increased in the United States.
Study Design
We calculated cesarean rates for term singletons in “breech / malpresentation” from 1997–2003 using National Center for Health Statistics data. We compared rates by socio-demographic groups and state. Multivariable logistic regression models were constructed to see if factors associated with cesarean delivery differed over time.
Results
Breech cesarean rates increased overall from 83.8% to 85.1%. There was a significant increase in rates for most socio-demographic groups. There was little to no increase for mothers < 30 years. There was wide variability in rates by state, 61.6%–94.2% in 1997. Higher breech incidence correlated with lower cesarean rates, suggesting potential state bias in reporting breech.
Conclusion
In the United States, breech infants are predominantly born by cesarean. There was a small increase in this trend from 1998 to 2002. There is wide variability by state, which is not explained by socio-demographic patterns, and may be due to reporting differences.
Keywords: Cesarean delivery, breech, malpresentation, United States
Introduction
Obstetricians have long debated the role of cesarean delivery for breech infants, as a potentially safer mode of delivery. However, the large majority of term breech infants in developed countries are now delivered by cesarean, and evidence generally supports this practice. The largest randomized trial to date, the Term Breech Trial whose results were published in October 2000 demonstrated improved outcome for selective cesarean delivery.(1) However, follow-up data from this trial did not demonstrate improvement in outcomes for cesarean delivery neither for infants at 2 years, nor for mothers.(2, 3) Since that time, the methodology and implications of the initial publication have been questioned.(4)
Nevertheless, the initial publication outlining the potential benefits of cesarean delivery for term breech was followed by subsequent changes in practice patterns in various countries.(1, 5, 6) In Sweden, the cesarean section rate for term breech infants increased from 75.3% to 86.0% from 1999 to 2001.(5) In the Netherlands, the cesarean section rate increased from 50% to 80% within two months after publication of the Term Breech Trial, which was associated with improvement in neonatal outcome.(6)
In the United States, there remains controversy regarding the necessity for cesarean section for all breech infants, with the latest committee opinion from the American College of Obstetricians and Gynecologists (ACOG) in July 2006 stating that vaginal breech delivery may still be a viable option with appropriate operator experience, rigorous hospital protocols and a thoroughly counseled patient.(7)
We wanted to study the patterns of cesarean section rates for breech in the United States in the years surrounding the publication of the Term Breech Trial, expecting an increase in the cesarean rate as seen in other countries. We also were interested in potential variation in cesarean rates by state and by socio-demographic factors, and changes in these variations over time. To this end, we examined births recorded in the National Center for Health Statistics (NCHS) Birth Certificate data sets for the years 1997–2003 in order to assess trends in cesarean section rates for breech infants in the United States.
Materials and Methods
This is a population study using the U.S. Birth Cohort data sets of 1997 to 2003 published by the NCHS.(8–14) In this 7-yr cohort, 1,067,989 (3.8%) of 28,012,013 total infant births were recorded as breech / malpresentation. Although we sometimes refer to the subjects of this analysis as breech infants, it is important to note that the actual item recorded on the US standardized birth certificate is “breech / malpresentation” defined as “the presentation of the fetal buttocks rather than the head, or other malpresentation.”(15–17) As such, an unspecified proportion of infants may not be true breech, but transverse lie or abnormal cephalic presentation.
To control for potential confounders in the decision to deliver by cesarean, our analysis included infants born only to U.S. residents who were singleton infants, with estimated gestational age greater than or equal to 37 weeks and less than 43 weeks. We also excluded infants born to mothers with a previous cesarean delivery or unknown method of delivery, and infants with the following congenital anomalies: anencephaly, spina bifida, hydrocephalus, microcephaly, other central nervous system anomalies, heart malformations, other circulatory / respiratory anomalies, rectal atresia, tracheoesophageal fistula, omphalocele / gastroschisis, other gastrointestinal anomalies, malformed genitalia, renal agenesis, other urogenital anomalies, diaphragmatic hernia, musculoskeletal anomalies, Down’s syndrome, and other chromosomal anomalies. Of the 560,087 eligible records, 1.7% were excluded due to anomalies. (Congenital anomalies were not reported by New Mexico and therefore potential cases with congenital anomalies from NM would not have been excluded.) This resulted in an analytic cohort of 550,773 breech infants. This study was approved by the Stanford University Institutional Review Board.
We calculated national breech cesarean section rates for each year from 1997–2003 as well as state-specific rates for all 50 states and the District of Columbia. We then compared breech cesarean section rates for the years 1997 and 2003 for the following socio-demographic variables: maternal age, race, education, adequacy of prenatal care, and parity. Adequacy of care was measured by the Kessner index.(18) Adequacy was coded as a binary variable, with mothers who had intermediate, or low care classified as having inadequate prenatal care. Adequacy of care was not determined when certain variables such as the month of prenatal care initiation or number of visits were missing. We calculated percent change from 1997 to 2003 and made statistical comparisons using the chi-square statistic. While all states had uniform reporting requirements of demographic factors, various states did not have specific items on their certificate. For detailed information regarding completeness of data by state, refer to the Technical Appendix from the Vital Statistics of the United States.(15–17, 19–22)
Using the percentage of breech infants delivered by cesarean in 1997, each of the 50 states and Washington, D.C., states were assigned to a lower (< 80%), middle (80 - < 90%) or upper (>= 90%) cesarean rate performance group. These were cut-off points which allowed a division into relatively equal number of states per group. Rates were calculated for each group across years based upon the 1997 rate assignment.
We constructed multivariable logistic regression models for 1997 and 2003 to assess the impact associated with various socio-demographic and medical factors on mode of delivery, and to assess if such associations had changed between 1997 and 2003. We included the socio-demographic factors listed above, the following medical factors: maternal diabetes, hypertensive disorder, placental abruption, and precipitous delivery, and the 1997 performance group of the state in which the birth occurred. Adjusted odds ratios were calculated with 95% Wald confidence intervals. Due to the implementation of new birth certificate data forms, the states of Pennsylvania and Washington did not collect maternal education information in 2003 (n=7,200). Adequacy of prenatal care was not known for 1,547 records in the 2003 records for the remaining states and for 2,384 records in 1997. These records were not included in the logistic regression analysis.
In order to assess variation in diagnosis of breech in this database, we calculated the incidence of breech in 1997 by individual states and performed correlation analysis between incidence and breech cesarean rates. We estimated the correlation coefficient R using simple linear regression and calculated the coefficient of determination R2. We calculated 28-day mortality rates for vaginal vs. cesarean delivered breech infants according to cesarean performance group as outlined above.
All statistical analyses were computed using SAS 9.1 (SAS, Cary, NC). We used p value < 0.05 to confer statistical significance.
Results
The percentages of term breech singletons delivered by primary cesarean section over the years 1997 – 2003 are listed in Table 1. Cesarean section rates decreased from 1997 to 1998, were stable from 1998 to 1999, increased from 2000–2002, and reached a plateau in 2003. Between 1997 and 2003, the absolute increase was a modest 1.3% from 83.8% to 85.1%. There was a dip to 83.0% in 1998. Breech cesarean section rates for the 18 (35%) states with baseline rate < 80% increased from 71.5% to 73.5%. The middle group of 22 states (43%) with baseline rates from 80%- < 90% increased from 86.3% to 87.8%. The top group of 11 states (22%) with baseline rates >= 90% increased from 91.5% to 92.8%.
Table 1.
Cesarean rates for breech 1997 to 2003.
| State groups* | ||||
|---|---|---|---|---|
| Year | Overall | Low | Middle | High |
| (< 80%) | (80 - <90%) | (>= 90%) | ||
| 1997 | 83.8% | 71.5% | 86.3% | 91.5% |
| 1998 | 83.0% | 69.8% | 86.3% | 91.0% |
| 1999 | 83.1% | 69.2% | 86.2% | 91.6% |
| 2000 | 83.4% | 69.8% | 86.7% | 92.2% |
| 2001 | 84.4% | 71.0% | 87.7% | 92.7% |
| 2002 | 85.1% | 72.0% | 88.3% | 93.1% |
| 2003 | 85.1% | 73.5% | 87.8% | 92.8% |
Data source: National Center for Health Statistics.
State groups divided into those with low (n=18), middle (n=22), and high (11) baseline rates of cesarean for breech in 1997.
P values for chi-square test for overall rates and for each group were all < 0.0001.
In 1997, women who were Hispanic, > 39 years old, had 16 years or more of education or were nulliparous, had the highest breech cesarean rates. Women who were American Indian, had unknown education status, or were multiparous had the lowest rates (Table 2). The group of women with unknown education status was a small proportion (1.2%) of the cohort. There was little change in relative positions between 1997 and 2003. Cesarean rates increased from 1997 to 2003 for most socio-demographic groups investigated. There was little to no increase seen for mothers less than 30 years. Hispanic and Asian mothers and those mothers with 9–11 years of education had less significant change than other groups. The largest absolute increases were seen in women who had the lowest rates in 1997; American Indians (77.5% to 81.9%), unknown education status (77.2% to 82.5%), and para > 4 (68.7% to 74.5%).
Table 2.
Cesarean rate for breech by socio-demographic characteristics 1997 and 2003.
| N* | Cesarean rate | Absolute | ||||
|---|---|---|---|---|---|---|
| 1997 | 2003 | 1997 | 2003 | change | p (chi-sq) | |
| Maternal race | ||||||
| Hispanic | 10552 | 12799 | 86.46% | 87.23% | 0.8% | 0.08 |
| Asian | 3125 | 4266 | 85.15% | 86.43% | 1.3% | 0.12 |
| White | 55444 | 49304 | 83.70% | 85.91% | 2.2% | < 0.0001 |
| African American | 6359 | 6015 | 80.47% | 83.94% | 3.5% | < 0.0001 |
| American Indian | 648 | 650 | 77.47% | 81.85% | 4.4% | 0.05 |
| Maternal age | ||||||
| < 20 years | 8114 | 6460 | 83.47% | 82.60% | −0.9% | 0.16 |
| 20–29 years | 37945 | 38608 | 83.34% | 83.39% | 0.0% | 0.86 |
| 30–39 years | 28080 | 32585 | 84.43% | 87.27% | 2.8% | < 0.0001 |
| >= 40 years | 1959 | 2581 | 85.66% | 89.31% | 3.7% | 0.0002 |
| Maternal education† | ||||||
| 0–8 years | 3345 | 3541 | 82.30% | 84.61% | 2.3% | 0.01 |
| 9–11 years | 9431 | 8164 | 82.46% | 83.51% | 1.1% | 0.06 |
| 12 years | 23965 | 20097 | 83.58% | 85.02% | 1.4% | < 0.0001 |
| 13–15 years | 17410 | 16007 | 82.92% | 84.63% | 1.7% | < 0.0001 |
| >= 16 years | 20997 | 24466 | 85.27% | 88.00% | 2.7% | < 0.0001 |
| Unknown | 950 | 759 | 77.16% | 82.48% | 5.3% | 0.007 |
| Adequacy of PNC†† | ||||||
| Adequate | 58141 | 56811 | 84.85% | 86.95% | 2.1% | < 0.0001 |
| Inadequate | 15573 | 14773 | 80.23% | 82.33% | 2.1% | < 0.0001 |
| Parity | ||||||
| Nulliparous | 46043 | 47654 | 88.92% | 89.50% | 0.6% | 0.005 |
| Para 1–4 | 28878 | 31265 | 76.30% | 78.83% | 2.5% | < 0.0001 |
| Para > 4 | 1177 | 1315 | 68.65% | 74.52% | 5.9% | 0.001 |
| Performance group | ||||||
| Bottom | 20585 | 20716 | 71.6% | 73.9% | 2.3% | < 0.0001 |
| Middle | 33615 | 37799 | 86.3% | 86.8% | 0.5% | 0.05 |
| Top | 21898 | 21719 | 91.5% | 92.8% | 1.3% | < 0.0001 |
| TOTAL | 76098 | 80234 | 83.82% | 85.09% | 1.3% | < 0.0001 |
Data source: National Center for Health Statistics.
N – number of infants in breech / malpresentation.
Maternal education information not available for Pennsylvania and Washington 2003 (n=7200).
For some records (n=11304), adequacy of prenatal care was not able to be ascertained due to missing information.
We used multivariable logistic regression to assess the impact of various factors on cesarean delivery of breech term infants for 1997 and 2003 (Table 3). Of the medical factors considered, precipitous delivery was the highest risk factor for not having a cesarean delivery. Of the sociodemographic factors, African American race, age less than 20, unknown educational level, and multiparity had the lowest odds ratios for breech cesarean delivery in 1997. In general, the models were similar for both time periods with similar magnitude of odds ratios and 95% confidence intervals. The impact of maternal education lessened from 1997 to 2003, with mothers having less than 8 years of education having increased risk of vaginal delivery in 1997 (OR 0.89, 95% CI 0.80, 0.99), but no increased risk in 2003. The influence of parity was always significant, but the magnitude of the odds ratios decreased over time, particularly for parity > 4. After controlling for socio-demographic and medical factors, the bottom performance group had a 4-fold decrease, and the middle group an almost 2 fold decrease in the odds of Cesarean delivery compared to the top performance group in both years.
Table 3.
Multivariable logistic regression models for cesarean delivery for breech over time.
| 1997 | 2003 | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||||
| Gestational Age* | 0.86 | 0.85 | 0.88 | 0.82 | 0.80 | 0.83 | |
| Race | |||||||
| Hispanic | 1.10 | 1.02 | 1.18 | 1.04 | 0.97 | 1.12 | |
| Asian | 0.93 | 0.83 | 1.04 | 0.86 | 0.78 | 0.95 | |
| White | 1.00 | (reference) | 1.00 | (reference) | |||
| African American | 0.81 | 0.75 | 0.87 | 0.86 | 0.79 | 0.93 | |
| Amer. Indian | 0.96 | 0.79 | 1.18 | 1.11 | 0.89 | 1.38 | |
| Maternal age | |||||||
| <=19 y | 0.72 | 0.67 | 0.78 | 0.69 | 0.63 | 0.75 | |
| 20–29 y | 1.00 | (reference) | 1.00 | (reference) | |||
| 30–39 y | 1.23 | 1.18 | 1.29 | 1.46 | 1.38 | 1.53 | |
| >= 40 y | 1.55 | 1.35 | 1.79 | 1.88 | 1.62 | 2.18 | |
| Maternal education | |||||||
| 0–8 y | 0.89 | 0.80 | 0.99 | 0.97 | 0.87 | 1.09 | |
| 9–11 y | 1.00 | 0.93 | 1.07 | 1.01 | 0.93 | 1.09 | |
| 12 y | 1.00 | (reference) | 1.00 | (reference) | |||
| 13–15 y | 0.92 | 0.87 | 0.98 | 0.96 | 0.90 | 1.02 | |
| >= 16 y | 0.85 | 0.80 | 0.90 | 0.87 | 0.81 | 0.92 | |
| unknown | 0.74 | 0.61 | 0.89 | 0.74 | 0.59 | 0.91 | |
| Inadequate prenatal care | 0.92 | 0.87 | 0.97 | 0.87 | 0.83 | 0.92 | |
| Parity | |||||||
| Nulliparous | 1.00 | (reference) | 1.00 | (reference) | |||
| Para 1–4 | 0.36 | 0.35 | 0.38 | 0.39 | 0.37 | 0.40 | |
| Para > 4 | 0.22 | 0.19 | 0.25 | 0.33 | 0.28 | 0.39 | |
| Diabetes | 1.12 | 0.99 | 1.26 | 1.00 | 0.89 | 1.12 | |
| Placental abruption | 0.87 | 0.62 | 1.22 | 0.95 | 0.64 | 1.41 | |
| Hypertensive disorder | 0.89 | 0.81 | 0.97 | 0.87 | 0.79 | 0.96 | |
| Precipitous delivery | 0.09 | 0.07 | 0.10 | 0.11 | 0.09 | 0.13 | |
| Performance group (1997) | |||||||
| Bottom | 0.23 | 0.22 | 0.25 | 0.21 | 0.20 | 0.23 | |
| Middle | 0.58 | 0.54 | 0.61 | 0.56 | 0.53 | 0.60 | |
| Top | 1.00 | (reference) | 1.00 | (reference) | |||
Data source: National Center for Health Statistics.
OR, odds ratio; CI, confidence interval. Odds ratios > 1 favor cesarean delivery.
OR for gestational age reflects increment of 1 week increase in gestational age.
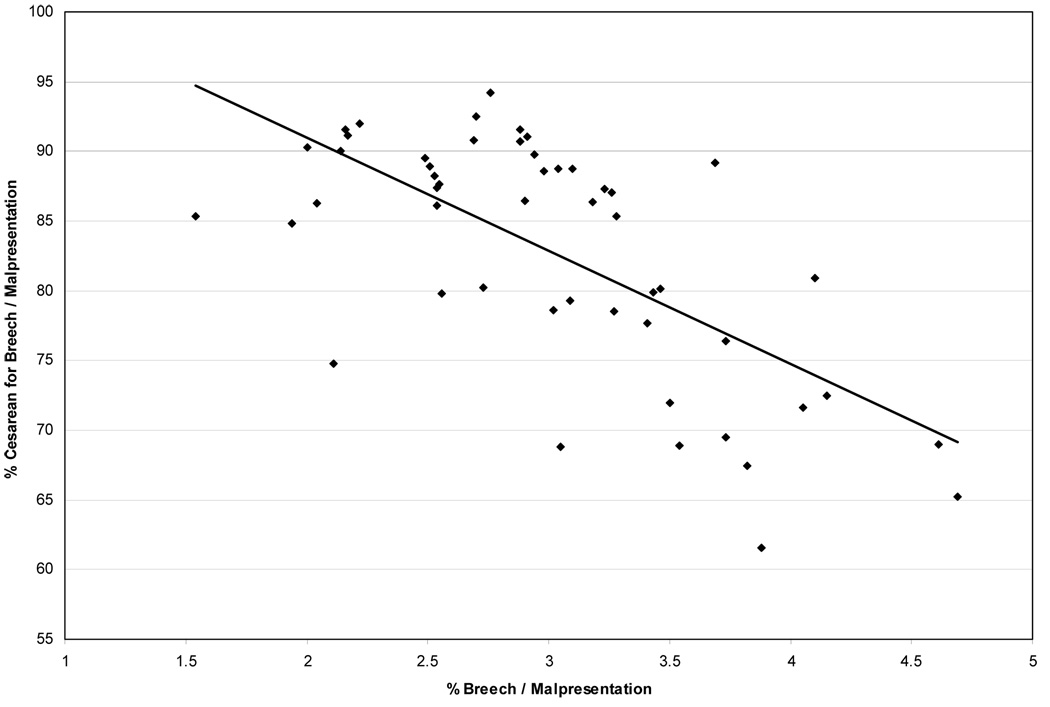
Table 4 lists the states rank ordered by the percentage of term breech infants delivered by cesarean ranging from 94.2% to 61.6% in 1997 (adjustment for socio-demographic factors gave similar results with a range of 60.2% to 94.2% in 1997 and are available on request). Across the study period, states tended to maintain their relative position. There was an unexpected relationship between breech cesarean rate and state reporting of breech incidence. States in the highest performance group (>= 90% cesarean rates) had incidence of breech of 2.5%, the middle group (80 - < 90% cesarean rates) had breech incidence of 2.8%, and the lowest group (< 80% cesarean rates) had breech incidence of 3.5%. The higher incidence of breech was correlated with lower incidence of breech cesarean rates (R = −0.66, R2 = 0.44) suggesting the possibility that part of the variability in the percent cesarean for breech may be the result of regional differences in assessing and reporting the number of breech infants (Figure 1). As we were unsure of the validity of comparing state-by-state breech incidence using this database, the names of the states in Table 4 are masked.
Table 4.
Singleton term breech cesarean rate and breech incidence by state.
| Breech cesarean rate (%) | Breech incidence (%) | ||||
|---|---|---|---|---|---|
| State | 1997 | 2003 | 1997 | 2003 | |
| 1 | 94.2 | 93.9 | 2.76 | 2.55 | |
| 2 | 92.5 | 94.6 | 2.70 | 2.33 | |
| 3 | 92.0 | 94.6 | 2.22 | 1.96 | |
| 4 | 91.5 | 93.2 | 2.16 | 1.91 | |
| 5 | 91.5 | 92.6 | 2.88 | 2.88 | |
| 6 | 91.2 | 93.9 | 2.17 | 2.26 | |
| 7 | 91.1 | 87.5 | 2.91 | 2.73 | |
| 8 | 90.8 | 90.9 | 2.69 | 2.83 | |
| 9 | 90.7 | 93.6 | 2.88 | 2.80 | |
| 10 | 90.3 | 96.2 | 2.00 | 1.70 | |
| 11 | 90.1 | 90.9 | 2.14 | 2.25 | |
| mean | 2.50 | 2.38 | |||
| 12 | 89.7 | 93.7 | 2.94 | 2.87 | |
| 13 | 89.5 | 91.2 | 2.49 | 2.24 | |
| 14 | 89.1 | 79.2 | 3.69 | 3.27 | |
| 15 | 88.9 | 81.0 | 2.51 | 2.84 | |
| 16 | 88.7 | 92.1 | 3.04 | 3.19 | |
| 17 | 88.7 | 91.3 | 3.10 | 2.47 | |
| 18 | 88.6 | 87.9 | 2.98 | 3.29 | |
| 19 | 88.2 | 96.5 | 2.53 | 2.59 | |
| 20 | 87.6 | 92.7 | 2.55 | 2.65 | |
| 21 | 87.4 | 91.0 | 2.54 | 2.18 | |
| 22 | 87.3 | 89.1 | 3.23 | 4.13 | |
| 23 | 87.1 | 87.9 | 3.26 | 3.13 | |
| 24 | 86.4 | 86.7 | 2.90 | 2.71 | |
| 25 | 86.4 | 92.8 | 3.18 | 2.56 | |
| 26 | 86.3 | 89.0 | 2.04 | 1.61 | |
| 27 | 86.1 | 77.3 | 2.54 | 3.34 | |
| 28 | 85.4 | 88.8 | 3.28 | 2.86 | |
| 29 | 85.3 | 97.0 | 1.54 | 1.97 | |
| 30 | 84.9 | 93.0 | 1.94 | 2.30 | |
| 31 | 80.9 | 84.1 | 4.10 | 4.27 | |
| 32 | 80.2 | 80.2 | 2.73 | 2.85 | |
| 33 | 80.2 | 87.4 | 3.46 | 2.73 | |
| mean | 2.84 | 2.82 | |||
| 34 | 79.9 | 62.0 | 3.43 | 4.02 | |
| 35 | 79.8 | 81.8 | 2.56 | 1.91 | |
| 36 | 79.3 | 76.0 | 3.09 | 2.93 | |
| 37 | 78.6 | 81.0 | 3.02 | 2.54 | |
| 38 | 78.5 | 78.5 | 3.27 | 3.29 | |
| 39 | 77.7 | 87.3 | 3.41 | 2.68 | |
| 40 | 76.4 | 82.7 | 3.73 | 3.55 | |
| 41 | 74.7 | 90.2 | 2.11 | 3.14 | |
| 42 | 72.4 | 83.6 | 4.15 | 3.02 | |
| 43 | 71.9 | 82.2 | 3.50 | 2.68 | |
| 44 | 71.6 | 81.3 | 4.05 | 3.28 | |
| 45 | 69.5 | 77.4 | 3.73 | 4.64 | |
| 46 | 68.9 | 69.1 | 4.61 | 4.60 | |
| 47 | 68.9 | 48.4 | 3.54 | 5.12 | |
| 48 | 68.8 | 73.8 | 3.05 | 4.15 | |
| 49 | 67.4 | 66.7 | 3.82 | 4.26 | |
| 50 | 65.2 | 78.4 | 4.69 | 2.97 | |
| 51 | 61.6 | 69.7 | 3.88 | 3.84 | |
| mean | 3.54 | 3.48 | |||
Data source: National Center for Health Statistics.
Figure 1.
To investigate if there was a difference in survival of breech infants born by cesarean vs. vaginal route, we compared neonatal mortality by mode of delivery. For the entire cohort, the relative risk of death was 2.0 (95% CI 1.7, 2.4) for vaginal compared to cesarean delivery. The 28-day mortality rate for cesarean delivered breech infants was similar at 1.4, 1.5, and 1.4 per 1,000 births for the highest, middle, and lowest cesarean performance groups. In contrast, the mortality rate for vaginally delivered infants varied considerably, at 5.4, 3.5, and 1.4 per 1,000 live births for the highest, middle, and lowest performance groups, respectively. The relative risks of death for a breech infant for vaginal vs. cesarean delivery were 3.8, 2.3, and 1.0 for these three groups respectively. States that reported the highest breech incidence reported the lowest cesarean rates for breech infants (Fig. 1) and had the least difference in the mortality of their breech infants by mode of delivery. It is possible that these differences may not represent true differences in outcome of breech by mode of delivery, as it may actually reflect differences in the proportion of infants incorrectly labeled as breech or malpresentation,
Comment
In 2001, the ACOG recommended cesarean delivery for the term singleton breech.(23) This recommendation was based largely on the results of The Term Breech Trial which found that cesarean section was associated with both reduced mortality and serious morbidity in the newborn period.(1) Subsequently, the two year outcomes of surviving children whose mothers were enrolled in the Term Breech Trial were no different between groups.(3) Methodological aspects of the trial have also been questioned.(4) In 2006 the ACOG recommendation was amended due to a continuing controversy regarding the true long term risks of term vaginal breech delivery, and the importance of operator experience, strict protocols and patient counseling in any decision to pursue a breech vaginal delivery were emphasized.(7)
We found that in 1997, most U.S. singletons in breech position were delivered by cesarean. Although there was an increase from 83.8 to 85.1% over the next 6 years, it was relatively small for the nation as a whole. Time trends shown in Table 1 suggest that this increase may have been influenced by the publication of the Term Breech Trial and following ACOG committee opinion.(1, 23) If this was the case, the influence of the Trial in the United States was comparatively insignificant compared to corresponding increases seen in other countries soon after these publications, such as in the Netherlands and Sweden.(5, 6) Although those countries had an even larger percentage increase in cesarean sections; both had baseline rates that were significantly lower than the U.S. and even after the increase, did not go to levels much higher than those seen at baseline in the U.S. The medico-legal environment in the United States may have had an influence on cesarean rates for breech even prior to the Term Breech Trial.
It is possible that the modest increase in the delivery of breech infants by cesarean seen in the U.S. was not influenced by the publications, but was a reflection of a general trend in increased cesarean delivery. In looking at the U.S. cohort of singleton term vertex infants without severe congenital anomalies, we found that their primary cesarean delivery rate increased from 10.8% to 14.7% from 1997 to 2003 (full details upon request).
Clinical decision making is based on the physician’s assessment of both the clinical situation and the constellation and weight given to a patient’s medical and socio-demographic risk factors. These weights are dependent upon one’s experience, published findings, and professional recommendations / guidelines. We constructed logistic models and used the odds ratio as a proxy for the weight given specific risk factors towards the decision to deliver a breech infant vaginally. In general, the direction and extent to which most factors such as precipitous delivery, inadequate prenatal care, and maternal age influenced decision making was similar across years (Table 3). Several groups which had a higher risk for vaginal delivery in 1997, such as women with low education and multiparous mothers, had decreased risk for vaginal delivery in 2003, suggesting an increase in the decision to deliver them by cesarean. On the other hand Hispanics and older gestational age developed a higher risk of being delivered vaginally.
Although most states saw a modest increase in cesarean rates from 1997 to 2003, we did not find a dramatic difference between those states which had started out with lower and higher cesarean rates. Typically, the lower performers in a quality of care measure improve the most after an intervention.(24) There was a suggestion of this phenomenon in our data; while the cesarean rate for the states with lowest initial rates increased from 71.6% to 73.9% (absolute difference of 2.3%), the states with highest initial rates increased from 91.5% to 92.8% (absolute difference of 1.3%).
We found great variability in individual state cesarean section rates for breech / malpresentation, ranging from 61.6% to 94.2% in 1997. Even after risk adjustment the range remained quite broad from 60.2% to 94.2% (Table 3 - details of risk adjusted results not shown). It is possible that some of these differences may be explained by regional differences in care provided by public vs. private hospitals as well as teaching hospitals or in differences according to patient insurance status. While our dataset did not contain data on type of hospital or payer source, the potential role of these factors in determining mode of delivery also deserves further study. Although both the observed and adjusted variability remained quite broad from 1997 to 2003, the relative rates for each state were quite consistent over time (Table 3).
An unexpected finding was the relationship between breech / malpresentation incidence and corresponding cesarean rates suggesting the possibility of an over-reporting bias in the reporting of breech / malpresentation. Over-reporting the number of such births could lead to a systematic underestimation of the percentage of breech delivered by cesarean as most non-breech term infants are delivered vaginally. For example, if the true state incidence of breech / malpresentation was 4%, with a cesarean rate of 80% (based upon the actual number of breech infants delivered by cesarean divided by the actual number of infants with breech / malpresentation) and there was an overestimation of breech incidence to 5% (with the additional 1% having a cesarean rate of 15%), the observed cesarean rate for breech would be erroneously decreased from 80% to 67%.
There is evidence of such over-reporting of “breech / malpresentation” infants in our findings on mortality by mode of delivery. While the cesarean delivered breech infants had similar mortality rates regardless of breech incidence, vaginally delivered breech / malpresentation infants had widely varying mortality rates depending on performance group of cesarean rates. Those states with the highest cesarean rates for breech had the lowest incidence of breech and a vaginal vs. cesarean relative risk of mortality of 3.8. Those states with the lowest cesarean rates for breech had the highest breech incidence and vaginal mortality rates equal to cesarean mortality rates, suggesting that the “breech / malpresentation” infants in this cohort included a significant number of low mortality risk vertex infants.
It is unclear what accounts for this potential over-reporting of “breech / malpresentation”. We, as well as other investigators have previously used US vital records to perform analyses of breech deliveries using the “breech / malpresentation” code in NCHS datasets.(25–28) In fact, the latest ACOG committee opinion regarding mode of delivery for breech relies upon this data.(7) In doing these studies, analyses have been based on the assumption that the reporting of breech / malpresentation is primarily indicative of breech presentation or other presentations such as transverse lie in which vaginal delivery may be associated with adverse outcome. However, it may be the case that reporting of “breech / malpresentation” may not be consistent across regions. The source of inconsistency may be differences in the assessment and reporting of malpresentation. We believe that the large differences in the incidence of breech and corresponding variation in breech cesarean rates according to state are likely due to differences in assessment and reporting, as well as variations in clinical decision making. We conclude that it is impossible to estimate the true incidence of breech for the nation as a whole or at the regional level. We can only say that the reported breech incidence for term singletons without congenital anomalies ranged from 1.5 to 4.7% by individual state in 1997 and from 1.6% to 4.6% in 2003. Furthermore, it is not possible to make conclusions about the potential benefit of cesarean for breech to prevent mortality from this data, due to the variability of reporting and the inability to exclude confounding factors.
Although the rates of cesarean delivery for breech that are presented here may not be precise, the reporting of cesarean for breech appear stable over time (i.e. reliable), making the relatively small change observed likely to reflect actual extent of change over this time period.
The 2003 revision of the US birth certificate, which has been undergoing implementation across states over the past several years, has been modified and the line for “breech / malpresentation” is now worded as “non-vertex presentation”, which includes shoulder, brow, and face presentations along with breech and transverse lie.(29) We suggest that a more specific coding for breech would better serve the obstetric community in tracking trends as well as for research purposes. Until we can be assured that assessment and reporting of breech is valid, it will be difficult to use epidemiologic studies based on vital records data to add to the discourse on the benefit of cesarean for breech. Such studies could be quite relevant considering the ongoing debate over the Term Breech Trial .(4, 30)
Acknowledgements
Henry Lee is supported by NIH Training Grant 2T32 HD 07249-23. All authors have no financial conflicts of interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This research was presented at the Pediatric Academic Societies Annual Meeting in Toronto, Ontario, Canada, May 5–8, 2007.
Condensation In the United States, breech infants are predominantly born by cesarean with variation by state; cesarean rates increased modestly from 1997–2003.
References
- 1.Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet. 2000;356(9239):1375–1383. doi: 10.1016/s0140-6736(00)02840-3. [DOI] [PubMed] [Google Scholar]
- 2.Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):917–927. doi: 10.1016/j.ajog.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Whyte H, Hannah ME, Saigal S, Hannah WJ, Hewson S, Amankwah K, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):864–871. doi: 10.1016/j.ajog.2004.06.056. [DOI] [PubMed] [Google Scholar]
- 4.Glezerman M. Five years to the term breech trial: the rise and fall of a randomized controlled trial. Am J Obstet Gynecol. 2006;194(1):20–25. doi: 10.1016/j.ajog.2005.08.039. [DOI] [PubMed] [Google Scholar]
- 5.Alexandersson O, Bixo M, Hogberg U. Evidence-based changes in term breech delivery practice in Sweden. Acta Obstet Gynecol Scand. 2005;84(6):584–587. doi: 10.1111/j.0001-6349.2005.00534.x. [DOI] [PubMed] [Google Scholar]
- 6.Rietberg CC, Elferink-Stinkens PM, Visser GH. The effect of the Term Breech Trial on Medical Intervention Behavior and Neonatal Outcome in The Netherlands: An Analysis of 35,453 Term Breech Infants. Obstet Gynecol Surv. 2005;60(5):289–290. doi: 10.1111/j.1471-0528.2004.00317.x. [DOI] [PubMed] [Google Scholar]
- 7.ACOG Committee Opinion No. 340. Mode of term singleton breech delivery. Obstet Gynecol. 2006;108(1):235–237. doi: 10.1097/00006250-200607000-00058. [DOI] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Hyattsville, Maryland: National Center for Health Statistics; Birth Cohort Linked Birth and Infant Death Data Set. 1999
- 9.National Center for Health Statistics. Hyattsville, MD: National Center for Health Statistics; Birth Cohort Linked Birth and Infant Death Data Set. 2000
- 10.National Center for Health Statistics. Hyattsville, MD: National Center for Health Statistics; Birth Cohort Linked Birth and Infant Death Data Set. 1997
- 11.National Center for Health Statistics. Hyattsville, MD: National Center for Health Statistics; Birth Cohort Linked Birth and Infant Death Data Set. 1998
- 12.National Center for Health Statistics. Hyattsville, MD: National Center for Health Statistics; Birth Cohort Linked Birth and Infant Death Data Set. 2001
- 13.National Center for Health Statistics. Hyattsville, MD: National Center for Health Statistics; Natality public-use tape and CD-ROM. 2002
- 14.National Center for Health Statistics. Hyattsville, MD: National Center for Health Statistics; Natality public-use tape and CD-ROM. 2003
- 15.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Technical Appendix from Vital Statistics of the United States 1999 Natality.
- 16.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Technical Appendix from Vital Statistics of the United States 1997 Natality.
- 17.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Technical Appendix from Vital Statistics of the United States 1998 Natality.
- 18.Kessner DMK, C W. Contrasts in Health Status. Washington, DC: Institute of Medicine, National Academy of Sciences; 1973. Infant Death: An Analysis by Maternal Risk and Health Care. [Google Scholar]
- 19.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Technical Appendix from Vital Statistics of the United States 2000 Natality.
- 20.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Technical Appendix from Vital Statistics of the United States 2001 Natality.
- 21.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Technical Appendix from Vital Statistics of the United States 2002 Natality.
- 22.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Documentation of the Detail Natality Public Use File for 2003.
- 23.ACOG committee opinion: number 265, December 2001. Mode of term single breech delivery. Obstet Gynecol. 2001;98(6):1189–1190. doi: 10.1016/s0029-7844(01)01708-2. [DOI] [PubMed] [Google Scholar]
- 24.Lindenauer PK, Remus D, Roman S, Rothberg MB, Benjamin EM, Ma A, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007;356(5):486–496. doi: 10.1056/NEJMsa064964. [DOI] [PubMed] [Google Scholar]
- 25.Kontopoulos EV, Ananth CV, Smulian JC, Vintzileos AM. The impact of route of delivery and presentation on twin neonatal and infant mortality: a population-based study in the USA, 1995-97. J Matern Fetal Neonatal Med. 2004;15(4):219–224. doi: 10.1080/14767050410001668707. [DOI] [PubMed] [Google Scholar]
- 26.Lee HC, El-Sayed YY, Gould JB. Delivery mode by race for breech presentation in the US. J Perinatol. 2007;27(3):147–153. doi: 10.1038/sj.jp.7211668. [DOI] [PubMed] [Google Scholar]
- 27.Lee KS, Khoshnood B, Sriram S, Hsieh HL, Singh J, Mittendorf R. Relationship of cesarean delivery to lower birth weight-specific neonatal mortality in singleton breech infants in the United States. Obstet Gynecol. 1998;92(5):769–774. doi: 10.1016/s0029-7844(98)00291-9. [DOI] [PubMed] [Google Scholar]
- 28.Muhuri PK, Macdorman MF, Menacker F. Method of delivery and neonatal mortality among very low birth weight infants in the United States. Matern Child Health J. 2006;10(1):47–53. doi: 10.1007/s10995-005-0029-z. [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. Hyattsville, Maryland: Centers for Disease Control and Prevention; Guide to Completing the Facility Worksheets for the Certificate of Live Birth and Report of Fetal Death (2003 revision)
- 30.Bewley S, Shennan A. Peer review and the Term Breech Trial. Lancet. 2007;369(9565):906. doi: 10.1016/S0140-6736(07)60447-4. [DOI] [PubMed] [Google Scholar]