Abstract
Context
Unnecessary exposure to medical interventions can harm patients. Many hope that generalist physicians can limit such unnecessary exposure.
Objective
To assess older Americans’ perceptions of the need for tests and referrals that their personal physician deemed unnecessary.
Design
Telephone survey with mail follow-up in English and Spanish, conducted from May to September 2005 (overall response rate 62%).
Study Participants
Nationally representative sample of 2,847 community-dwelling Medicare beneficiaries. Main analyses focus on the 2,319 who had a personal doctor (“one you would see for a check-up or advice if you were sick”) whom they described as a generalist (“doctor who treats many different kinds of problems”).
Main Outcome Measure
Proportion of respondents wanting a test or referral that their generalist suggested was not necessary using 2 clinical vignettes (cough persisting 1 week after other flu symptoms; mild but definite chest pain lasting 1 week).
Results
Eighty-two percent of Medicare beneficiaries had a generalist physician; almost all (97%) saw their generalist at least once in the past year. Among those with a generalist, 79% believed that it is “better for a patient to have one general doctor who manages most of their medical problems” than to have each problem cared for by a specialist. Nevertheless, when faced with new symptoms, many would want tests and referrals that their doctor did not think necessary. For a cough persisting 1 week after flu symptoms, 34% would want to see a lung specialist even if their generalist told them they “probably did not need to see a specialist but could if they wanted to.” For 1 week of mild but definite chest pain when walking up stairs, 55% would want to see a heart specialist even if their generalist did not think it necessary. In these same scenarios, even higher proportions would want diagnostic testing; 57% would want a chest x-ray for the cough, and 74% would want “special tests” for the chest pain.
Conclusions
When faced with new symptoms, many older patients report that they would want a diagnostic test or specialty referral that their generalist thought was unnecessary. Generalists striving to provide patient-centered care while at the same time limiting exposure to unnecessary medical interventions will need to address their patients’ perceptions regarding the need for these services.
Electronic Supplementary Material
The online version of this article (doi:10.1007/s11606-008-0626-9) contains supplementary material, which is available to authorized users.
KEY WORDS: geriatrics, patient perceptions, tests and referrals, shared decision making
There is growing evidence that exposure to unnecessary diagnostic tests and specialty referrals can lead to a variety of harms. For example, patients living in regions with more aggressive medical care tend to have worse health outcomes and lower rates of patient satisfaction1, findings which may be explained by iatrogenic harms (e.g., injuries during testing, side effects of marginally effective treatments, psychological harms of labeling, medical errors). As a result, some hope that generalists will play a central role in limiting patients’ exposure to unneeded medical interventions.
While the downsides of “too much” medical care may be readily apparent to policy makers and clinicians, patients often have a different perspective. Adult patients frequently arrive at primary care visits with specific expectations that they will receive further diagnostic testing or specialty referrals. The reported prevalence of such expectations ranges from 26% to 67% for tests and 18% to 48% for referrals.2–5 Patient expectations clearly affect physician behavior.6 Nonetheless, doctors do not always meet their patients’ expectations, sometimes for good reason.7–10 For example, the physician may not believe that further action is needed.
There has been little previous work on patients’ perceptions of the need for tests and referrals that their physician does not think are necessary. In 1 national survey, more than two thirds of women said they would still want annual PAP screening even if their doctor recommended doing it less often.11 To learn more about patients’ attitudes toward “doing less,” we used clinical vignettes to ask a nationally representative sample of Medicare beneficiaries what they would do if their generalist physician said further testing or referral for a new symptom were not needed.
METHODS
The survey questions presented are part of a larger survey to assess variation in patients’ preferences for health care among Medicare beneficiaries 65 and older. The aim of the current study was to assess older Americans’ perceptions of the need for tests and referrals that their personal physician deemed unnecessary. The project was approved at the institutional review boards at Dartmouth Medical School (Hanover, NH), the University of Massachusetts, Boston, and by the Office of Research Development and Information at the Centers for Medicare and Medicaid Services (CMS).
Sample Selection
Our goal was to interview a nationally representative sample of community-dwelling Medicare beneficiaries 65 and older. Our sampling frame was 20% of the 2003 Medicare denominator file (the most recent data available as of February 1, 2005) with updated addresses and phone numbers. A probability sample of 4,000 people who were Medicare beneficiaries in 2003 was drawn as well as an oversample of 800 African Americans. The selected sample identification numbers were matched to the Centers for Medicare and Medicaid Services (CMS) current beneficiary file to obtain current contact information. Those found to be in long-term care facilities or deceased were designated as not eligible and deleted from the sample.
Survey
To learn about older patients’ perceptions of the need for tests and referrals that their generalist did not consider necessary, we used 2 clinical vignettes—new chest pain when walking upstairs and a cough after the flu (exact wording shown with the results). We chose these clinical scenarios for 3 reasons: many patients have experience with these symptoms; their evaluation involves judgment calls by both physician and patient; and in both cases the generalist might appropriately manage the condition without further testing or referral.
We developed our survey in several phases. First, an expert panel wrote a draft questionnaire. We then conducted cognitive interviews with 10 patients in the target population to determine whether the terms and concepts used were clear to respondents. Cognitive interviews are intensive one-on-one interviews with people in the target population to be surveyed. These interviews are designed to learn if the terms and concepts used in the survey questions mean the same things to both respondents and investigators. The basic goal of the cognitive interview is to find out whether the questionnaire is likely to work as the survey designers intended. Cognitive testing is very useful for identifying questionnaire problems and revealing fixes for these problems before the survey goes into the field.
Finally, we conducted a telephone pretest with 17 randomly selected individuals to test the interview procedure and to identify any problems with the interviewer/respondent interactions. The final questionnaire was translated/backtranslated into Spanish. The translation was done by an academic translation center using the committee approach to translation. The complete survey is available on the JGIM website (see online appendix).
Administration
The formal data collection protocol was specified by the Centers for Medicare and Medicaid Services (CMS). The selected individuals were sent 2 pre-notification letters, 1 from CMS and 1 on Dartmouth Medical School letterhead. The initial contact with a Medicare beneficiary was the CMS letter. This letter outlined the purposes of the study, assured selected individuals that their participation was voluntary and their benefits would not be affected by their participation, and provided them with a toll-free telephone number that they could call to decline participation if they so desired. The follow-up letter from the researchers provided similar information.
Telephone numbers were matched to addresses to the fullest extent possible; interviewers called those numbers and attempted to arrange to interview the selected individual. At least 6 attempts were made to reach hard-to-reach persons. The primary obstacle to telephone contact was inability to identify correct phone numbers for 25% of the sample (despite extensive use of directory assistance, telephone matching services, and electronic directories). Also, some individuals had trouble using the phone owing to hearing problems and other logistical difficulties.
Those sampled persons for whom a good telephone number could not be found or who were not reached by telephone were sent a dual-language (English–Spanish) mail version of the same set of questions the interviewers were using. The initial mailing of the questionnaire packet contained a $5 bill as an incentive to participate. To be equitable, all those who had responded by telephone were also sent $5. Non-respondents to the mail survey were sent a reminder card and a second questionnaire.
The telephone interview took about 20 minutes on average to administer. It took a similar amount of time to complete the self-administered questionnaire. This dual-language, mixed-mode survey was fielded between March and October 2005.
Analysis
Main The main analyses include the 2,319 respondents who reported having a generalist personal physician. Because African Americans were oversampled, all analyses incorporate sampling weights so that estimates are representative of the community-dwelling Medicare population. Specifically, we used the SVY command series in STATA 8.0 (College Park, TX). We used the chi-square test to compare differences in proportions and t tests to compare means.
Patient Characteristics We used multiple linear regression to estimate the total number of tests and referrals desired (i.e., special heart tests, heart specialist referral, chest x-ray and lung specialist referral) as a function of patient characteristics. The total number of tests/referrals desired (a number from 0 to 4) was the dependent variable. The independent variables consisted of all the personal characteristics specified in Table 2. For each level of each characteristic we calculated the adjusted total number of tests and referrals desired by substituting the sample mean for every other variable when solving the regression equation (e.g., adjusted mean number of tests and referrals desired for men was 2.36 vs 2.16 for women). For each characteristic, we designated a reference category and graphed the absolute difference (and its 95% confidence interval) between each level and the reference category (e.g., women desired 0.2 fewer tests and referrals than men).
Table 2.
Characteristics of Medicare Beneficiaries
| Medicare patients with a generalist personal doctor (N = 2,319)* | |
|---|---|
| Demographics | |
| Age in years | |
| Mean | 76 |
| Range | 65–102 |
| Men | 42% |
| Race | |
| Non-Hispanic White | 86% |
| Black | 6% |
| Hispanic | 4% |
| Other | 4% |
| Education | |
| <High school graduate | 21% |
| High school graduate | 60% |
| College graduate | 19% |
| Health status | |
| In general, how would you rate your overall health? | |
| Excellent or very good | 32% |
| Good | 40% |
| Fair or poor | 28% |
| Access to health care | |
| Visited personal doctor in the past year | 97% |
| Mean number of office visits in past year | 3.7 |
| Mean number of different doctors seen in past year | 2.6 |
| Importance of financial issues in deciding whether or not to get medical care | |
| Very important | 29% |
| Important | 25% |
| Somewhat important | 22% |
| Not important | 24% |
| Patient role in health care | |
| When you are ill, would you rate your role in managing the illness as... | |
| More important than doctor’s | 14% |
| Equally important as doctor’s | 75% |
| Less important than doctor’s | 11% |
| How important do you think it is for patients to play a large part in planning their own treatment? | |
| Very important | 54% |
| Somewhat important | 36% |
| Not important | 8% |
| Don’t know | 1% |
| How confident are you that you can manage your health conditions? | |
| Very | 48% |
| Somewhat | 43% |
| Not very | 8% |
| No health conditions | 2% |
*To provide estimates representative of the community-dwelling Medicare population, calculations were weighted to account for the oversampling of African Americans
RESULTS
Figure 1 details the steps we followed to arrive at our final sample. Two hundred and twenty-five beneficiaries were ineligible because they had either died or were living in nursing homes (and for the oversample, if they did not self-identify as African American). Out of 4,575 eligible patients, data were collected from a total of 2,847 beneficiaries. Reasons for non-response included: refusal to participate (n = 259); patient unable to complete interview (n = 89); language barrier (n = 3); and failure to reach patient by either phone or mail after numerous attempts (n = 1,377). An additional 528 were excluded because they reported that they did not have a generalist personal doctor.
Figure 1.
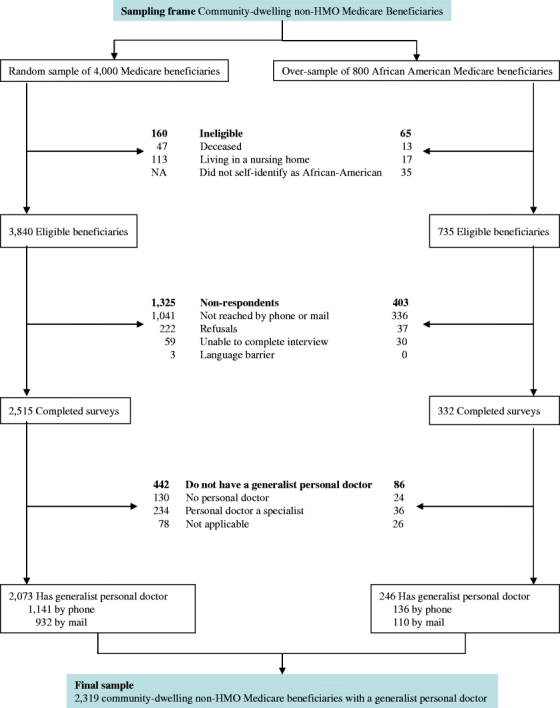
Selection of survey sample.
For the overall survey (not just our sample of those with a generalist personal doctor) 36% of surveys (n = 1,384) were completed by telephone and 29% (n = 1,131) were completed by mail for an overall response rate of 65% (calculated using the American Association for Public Opinion Research RRI formula12 that includes in the denominator all those who, despite numerous attempts, were never contacted). A total of 1,041 of the original sample were never contacted, so we have no information about whether or not they are still alive and in a private housing unit. Table 1 provides a comparison of our sample with the sampling frame.
Table 1.
Comparison of Demographic Characteristics of Survey Respondents (Community-dwelling non-HMO Medicare Beneficiaries who have A Generalist Personal Physician) with the Medicare Population (the sampling frame)
| Characteristics | Sampling frame (%) | Survey sample (%) |
|---|---|---|
| Age in years | ||
| 65–69 | 28 | 21 |
| 70–74 | 25 | 27 |
| 75–79 | 21 | 24 |
| 80–84 | 15 | 18 |
| 85+ | 11 | 10 |
| Male | 42 | 42 |
| Race | ||
| Non-Hispanic White | 86 | 86 |
| Black | 8 | 6 |
| Hispanic | 2 | 4 |
| other | 4 | 4 |
Eighty-two percent of respondents (n = 2,319) had a generalist physician, and almost all of these individuals (97%) saw their generalist at least once in the past year. The mean age was 76. Forty-two percent were men, 86% were Non-Hispanic whites, and 79% were high school graduates (Table 2). Respondents reported a wide spectrum of health status (about one third reported fair to poor health, one third reported excellent health). Most had frequent contact with the health care system (42% had at least 5 office visits in the past year). Eighty-six percent thought that their role in managing their own illness was equally or more important than the doctor’s.
Among patients with a generalist personal physician, 79% believed that it is “better for a patient to have one general doctor who manages most of their medical problems” than to have each problem cared for by a specialist. Nevertheless, when faced with new symptoms, many reported that they would want tests and referrals that their generalist doctor did not think necessary (Fig. 2). For a cough persisting 1 week after flu symptoms, 34% reported that they want to see a lung specialist even if their generalist told them they “probably did not need to see a specialist but could if they wanted to.” For 1 week of mild but definite chest pain when walking upstairs, 55% reported that they would want to see a heart specialist even if their generalist did not think it necessary. In these same scenarios, even higher proportions reported wanting diagnostic testing; 57% wanted a chest x-ray for the cough, and 74% wanted “special tests” for the chest pain.
Figure 2.
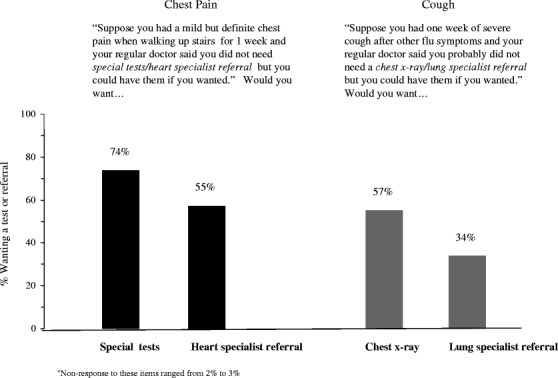
Elderly Americans with a generalist personal physician who would want a test or specialty referral that their doctor did not think was necessary (N = 2,319)*.
Patients with a prior history of heart disease were no more likely to want further heart testing (76% with heart disease wanted the test vs 73% without heart disease, p = .15). But they were more likely to desire a heart specialist referral (63% vs 53%, p < .001).
Figure 3 shows the mean number of tests and referrals desired (after adjusting for all the patient characteristics) according to patient characteristics. Men wanted more tests and referrals than women. Those with worse health reported wanting fewer than those in better health, although this difference was not statistically significant. Desire for tests and referrals also varied by race/ethnicity: the adjusted number of tests and referrals wanted was 3.12 for Hispanics who completed the Spanish version of the survey (the least acculturated group), 2.69 for Blacks, 2.45 for Hispanics completing the English survey, and 2.14 for Whites. As expected, patients with higher health care utilization in the past year—more office visits or different doctors seen—also wanted more tests and referrals (although these differences did not reach statistical significance) as did patients who perceived their role in managing their own illness as equally or more important than their doctors.
Figure 3.
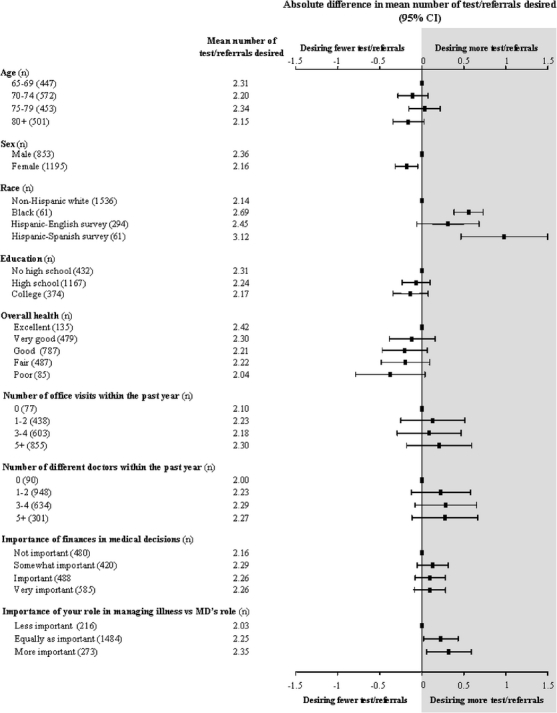
Desire for tests and referrals by patient characteristics (adjusted for all characteristics in Table 2), the mean number of the 4 possible tests or referrals desired by patient characteristics (after adjusting for all characteristics in Table 2). The absolute differences within each patient characteristic are presented graphically—this represents how many tests or referrals patients desired compared to the referent category (difference = 0).
DISCUSSION
Our findings show that elderly Americans value generalist physicians: more than 80% have a generalist physician and about the same proportion say it is better to have 1 generalist manage their problems than multiple specialists. This finding is consistent with previous work.13 At the same time, our findings suggest that older patients may hold fast to their ideas that more tests and referrals are needed even when their generalist provides advice to the contrary. In response to our vignettes, 30% to 75% of patients said they would want a diagnostic test or specialty referral that their generalist thought was unnecessary.
We think our findings reflect 2 things. First, there is a growing consensus that high-quality primary care involves shared decision making between physicians and their patients.14 A central tenet of shared decision making is that patients bring their own values and expectations to any medical encounter. Older Americans clearly endorse this view. Large majorities of Medicare beneficiaries said they see their role in managing their own illnesses as being just as important as that of their doctor, and 9 of 10 said they feel very or somewhat confident in doing so.
Second, patients seem to be predisposed to want “more” care. Studies have shown that many patients arrive at appointments with an expectation that they will receive a diagnostic test, a specialty referral, and or a prescription.Table 13,4,9 Research on patient attitudes toward cancer screening tests have shown that most Americans think standard screening tests are almost always a good idea and cannot do much harm.11,15 Further, Americans seem resistant to the idea of doing less. In a nationally representative survey of Americans, most said that “if a physician recommended you stop having or have less frequent [pap tests, mammograms, psa tests, sigmoidoscopy/colonoscopy]” they would still keep on having the tests as frequently as before.15
Another key finding in our study was that desire for tests and referrals varied significantly by gender and race. Women reported wanting fewer tests and referrals than men. Data on gender differences in patient expectations is limited. In a study of 559 audio-taped office visits of patients with a mean age of 55, women made more requests than men.16 However, this was a small study conducted among younger patients, using a different methodology. Our study also showed that compared to Whites, Blacks, and non English-speaking Hispanics reported wanting more tests and referrals. These findings are consistent with a previous study assessing patient perceptions of the urgency of seeking care among an urban population.17 However, our findings contrast with a waiting room study of 646 patients in 3 urban academic Internal Medicine practices, which found that compared to Whites, Blacks and Asians were less likely to prefer initial care by specialists.18 Differences in both measurement approach and sampling strategy may explain some of these differences.2,19
The idea that offering less care can be interpreted by patients as a withholding of valuable care (as opposed to avoiding unnecessary or even dangerous care) may in part explain why our findings varied by race and ethnicity. Previous work has shown that patients from ethnic minorities may be less likely to trust their physician.20–24 These patients may in turn be less likely to find reassurance in their doctors’ advice that further tests and referrals are not needed.
Our study should be interpreted in light of several limitations. First, as with any survey, there is the possibility of non-response bias. Our findings could be biased if the most passive patients—people who would accept physician recommendations without question—were overrepresented among non-respondents. Our response rate of 62% (65% for the national random sample and 45% for the African-American oversample) mitigates this concern, and it should be noted that this is quite a good response rate for a national survey. In addition, the demographic characteristics of our sample are very close to those of the sampling frame—20% of the 2004 Medicare denominator file (see Table 1), suggesting that non-response was a random phenomenon (at least with regards to these characteristics).
Second, some readers may be concerned about the use of clinical vignettes to measure patients’ desire for tests and referrals. We could not logistically study actual responses in a real-time situation—and even if we could, contextual differences would make it extremely difficult to interpret the results. In fact, this is the distinct advantage of using vignettes: all respondents are exposed to the same situation, controlling for differences in context.25 Further, it is reassuring that responses to the vignettes demonstrated construct validity—more patients reported a desire for tests and referrals for the potentially serious symptom (chest pain) than for the relatively minor symptom (cough after the flu). The combination of large sample size and use of the clinical vignette allowed us to construct a robust statistical model to make valid between-group comparisons, e.g., non-Hispanic White vs Black vs Hispanic.
Good physicians help patients get the care they need, neither more nor less. Our findings suggest that generalists striving to provide patient-centered care while at the same time limiting exposure to unnecessary medical interventions will face a difficult balancing act. It is not hard to understand where patients’ enthusiasm for medical interventions comes from. A host of sources, including disease promotion campaigns, direct to consumer drug ads (and, increasingly, ads from academic medical centers), and a media eager to tout the newest health risk or miracle cure bombards them with the message that more care is always better. All these forces push in the direction of doing more. Generalists have the opportunity to act as a countervailing force by working in a shared decision-making mode to address their patients’ expectations explicitly and by highlighting for their patients that good medical decision making almost always involves considering both the benefits and harms of interventions. If generalists want patients to do less, they will need to do more.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 102 KB)
Acknowledgments
The authors would like to thank Jennifer Snide for her assistance with manuscript preparation. Dr. Herndon had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. This study was supported by a grant from the National Institute on Aging (PO1 AG19783) and from a Research Enhancement Award from the Department of Veterans Affairs. Dr. Herndon was supported by a faculty development grant from the Department of Medicine at Dartmouth-Hitchcock Medical Center. Drs. Woloshin and Schwartz were supported by Robert Wood Johnson Generalist Faculty Scholar Awards. The views expressed herein do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
Conflict of Interest None disclosed.
Footnotes
Electronic Supplementary Material
The online version of this article (doi:10.1007/s11606-008-0626-9) contains supplementary material, which is available to authorized users.
References
- 1.Fisher, ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending: Part 2. Health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–99. [DOI] [PubMed]
- 2.Kravitz RL. Measuring patients’ expectations and requests. Ann Intern Med. 2001;134:881–8. [DOI] [PubMed]
- 3.Peck BM, Ubel PA, Roter DL, Goold SD, Asch DA, Jeffreys AS, Grambow SC, Tulsky JA. Do unmet expectations for specific tests, referrals, and new medications reduce patients’ satisfaction? J Gen Intern Med. 2004;19:1080–7. [DOI] [PMC free article] [PubMed]
- 4.Van Bokhoven MA, Pleunis-van Empel MCH, Koch H, Grol RPTM, Dinant G, van der Weijden T. Why do patients want to have their blood tested? A qualitative study of patient expectations in general practice. BMC Fam Pract. 2006;7:75–82. [DOI] [PMC free article] [PubMed]
- 5.Keitz SA, Stechuchak KM, Grambow SC, Koropshak CM, Tulsky JA. Behind closed doors—management of patient expectations in primary care practices. Arch Intern Med. 2007;167:445–2. [DOI] [PubMed]
- 6.Little P, Dorward M, Warner G, Stephens K, Senior J, Moore M. Importance of patient pressure and perceived pressure and perceived medical need for investigations, referrals, and prescribing in primary care: nested observational study. BMJ. 2004;328:444–7. [DOI] [PMC free article] [PubMed]
- 7.Kravitz RL, Callahan EJ, Paterniti D, Antonius D, Dunham M, Lewis CE. Prevalence and sources of patients’ unmet expectations for care. Ann Intern Med. 1996;125:730–7. [DOI] [PubMed]
- 8.Kravitz RL, Callahan EJ. Patients’ perceptions of omitted examinations and tests. J Gen Intern Med. 2000;15:38–45. [DOI] [PMC free article] [PubMed]
- 9.Jackson JL, Kroenke K. The effect of unmet expectations among adults presenting with physical symptoms. Ann Intern Med. 2001;134:889–97. [DOI] [PubMed]
- 10.Bell RA, Kravitz RL, Thom D, Krupat E, Azari R. Unsaid but not forgotten. Patients’ unvoiced desires in office visits. Arch Intern Med. 2001;161:1977–84. [DOI] [PubMed]
- 11.Sirovich BE, Woloshin S, Schwartz LM. Screening for cervical cancer: will women accept less? Am J Med. 2005;118:151–8. [DOI] [PubMed]
- 12.American Association for Public Opinion Research. Standard Definitions: Final Dispositions for Case Codes and Outcome Rates for Surveys,. Lenexa, KS: AAPOR; 2004.
- 13.Lewis CL, Wickstrom GC, Kolar MM, et al. Patient preferences for care by general internists and specialists in the ambulatory setting. J Gen Intern Med. 2000;15:75–83. [DOI] [PMC free article] [PubMed]
- 14.Institute of Medicine. Crossing the Quality Chasm. Washington DC: National Academy Press; 2001.
- 15.Schwartz LM, Woloshin S, Fowler F, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291:71–8. [DOI] [PubMed]
- 16.Kravitz RL, Bell RA, Azari R, Kelly-Reif S, Krupat E, Thom DH. Direct observation of requests for clinical services in office practice. What do patients want and do they get it? Arch Int Med. 2003;163:1673–81. [DOI] [PubMed]
- 17.Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Ethnicity, socio-economic position and gender—do they affect reported heath-care seeking behavior? Soc Sci Med. 2003;57:895–904. [DOI] [PubMed]
- 18.Wong MD, Asch SM, Andersen RM, Hays RD, Shapiuro MF. Racial and ethnic differences in patients’ preferences for initial care by specialists. Am J Med. 2004;116:613–20. [DOI] [PubMed]
- 19.Kravitz RL, Callahan EJ, Azari R, Antonius D, Lewis CE. Assessing patients’ expectations in ambulatory medical practice. Does measurement approach make a difference? J Gen Intern Med. 1997;12:67–72. [DOI] [PMC free article] [PubMed]
- 20.Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Med Care. 1998;36:180–9. [DOI] [PubMed]
- 21.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–63. [DOI] [PubMed]
- 22.Blanchard J, Lurie N. R-E-S-P-E-C-T: Patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004;53:721–30. [PubMed]
- 23.Sheppard VB, Zambrana RE, O’Malley AS. Providing health care to low-income women: a matter of trust. Fam Pract. 2004;21:484–91. [DOI] [PubMed]
- 24.Halbert CH, Armstrong K, Gandy OH, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166:896–901. [DOI] [PubMed]
- 25.King G, Murray CJL, Salomon JA, Tandon A. Enhancing the validity and cross-cultural comparability of survey research. Am Polit Sci Rev. 2004;97:567–83.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(PDF 102 KB)


