Abstract
Background
Pay for performance (P4P) programs have shown only modest improvements in outcomes and do not target patient behaviors. Many large employers and payers are turning to pay for performance for patients (P4P4P) to reduce health costs and improve the health of their covered populations. How these programs may be perceived by patients is unknown.
Objective
To assess patients’ opinion of the acceptability of P4P4P.
Design
Cross-sectional self-administered survey.
Participants
Patients in waiting rooms in two university-based primary care clinics.
Measurements
Participants were asked their opinions about paying people to quit smoking, lose weight, control their blood pressure, or control their diabetes.
Results
Respondents were split on whether P4P4P is desirable. Thrity-six to 42% thought it was a good/excellent idea to pay smokers to quit smoking, obese people to lose weight, people with hypertension to control their blood pressure, or people with diabetes to control their blood sugar, while 41–44% of the sample thought it was a bad/very bad idea. Smokers and patients who were obese endorsed P4P4P more favorably as a means to achieving tobacco cessation and weight loss than their non-smoking and non-obese counterparts.
Conclusions
Acceptance of paying patients for performance by the general population is equivocal. Establishing the efficacy of paying patients for performance may help it gain wider acceptance.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-008-0739-1) contains supplementary material, which is available to authorized users.
KEY WORDS: pay for performance, patient acceptance of health care, financial management
“Pay for performance” (P4P) is widely used to encourage physicians and hospitals to provide higher quality care.1,2 While these efforts can change provider behavior when payments are large enough,3,4 there are limitations to this approach. Many such efforts have not been evaluated,5 and effects often have been modest.6 For example, in hospitals participating in a P4P program aimed at improving care for non-ST-segment elevation myocardial infarction, P4P was not associated with significant improvement in either care or outcomes.7 A recent study found only modestly greater improvements for multiple different measures of care in hospitals engaged in P4P compared to hospitals not engaged in P4P.8 In addition, with physician incentives much of the performance-related pay is often paid based on achieving a certain threshold of performance, meaning that many of the resources go to providers who do not actually change their behavior since they were already performing at a high level before the program was instituted.9
Perhaps the biggest limitation with P4P is that physicians and hospital-targeted P4P do not directly target patients’ health behavior, which is an extremely important driver of both health-care costs and outcomes, arguably being responsible for a much higher proportion of premature mortality than is poor quality within the health-care system.10 Recognizing the strong associations between patient behaviors such as sedentary lifestyles and smoking and health-care costs,11,12 a number of large companies within the US have begun to directly provide incentives to patients. Such “pay for performance for patients” (P4P4P) approaches include monetary and non-monetary incentives for healthy behaviors, such as losing weight or participating in wellness programs,13–16 as well as charging smokers higher health insurance premiums.13,17 For example, Blue Shield of California, IBM, and Wells Fargo and Company are providing employees with monetary incentives for activities like filling out health-risk assessment forms and exercising.13 Scotts Miracle-Gro Company is using a combination of “carrots” (e.g., free weight-loss and smoking-cessation programs, free gym membership, and prizes like vacations) and “sticks” (e.g., firing persistent smokers and higher health premiums for employees who refuse to participate in the program) to motivate behavior change in their workforce.17 Scott employees are strongly encouraged to take health-risk assessments and are charged higher health insurance premiums if they refuse or do not comply with their health coach-designed action plans.17
P4P4P is now also being used by payers such as UnitedHealth Group Inc., which has started to deposit money into medical savings accounts for selected patients with chronic conditions who adhere to prescribed regimens. Perhaps more controversial is the approach being used by the West Virginia Medicaid program, which is reducing insurance coverage when Medicaid recipients fail to follow clinical recommendations.18,19
Whether P4P4P will succeed in increasing rates of healthy behaviors in all of these settings is uncertain, though there is evidence that such approaches can significantly increase the rate of smoking cessation,20,21 abstinence from addictive drugs,22,23 utilization of preventive services,24–27 and short-term weight loss.28–30 There is also some evidence that such approaches can be cost effective,31,32 though this evidence is limited.33 Given the proliferation of such approaches, we conducted a survey of a convenience sample of 515 patients to examine how acceptable these approaches are to patients and the role of framing effects34 in how patients react to descriptions of incentive-based programs for different diseases. We also examined how reactions differed by disease condition and the patients’ own medical history and asked about the magnitude of payments subjects thought appropriate.
METHODS
Data Collection
We conducted a cross-sectional survey of patients waiting in two University of Pennsylvania primary care practice waiting rooms during the summer of 2006. Both practices serve economically diverse patient populations, virtually all of whom have some sort of health insurance. During each of the 8 weeks of data collection, study personnel were present in the waiting rooms for 9 out of 11 weekly clinic sessions. All patients were approached and asked to complete one anonymous survey. If they were interested in participating, patients were randomly assigned to receive one of two surveys (the second survey is unrelated to the results being reported in this paper). Surveys were collected from patients prior to their appointment.
The University of Pennsylvania IRB approved the study, and informed consent was not required given that the survey was anonymous. The survey was only available in English.
Survey
The survey was designed by the authors, all of whom have expertise in survey design and one of whom has extensive experience with P4P4P programs (KGV). Through an iterative process of input and editing, a final version was developed and piloted on a convenience sample of eight students. In addition to basic demographics, the survey asked patients their opinions about paying people to quit smoking, lose weight, control their blood pressure, control their diabetes, and control their cholesterol. Additional questions asked about who is to blame when a person smokes, is obese, has hypertension, or has diabetes; how much money it would be appropriate to pay patients to improve health behaviors relating to these conditions; and whether the respondent had any of these conditions. Questions were framed both positively and negatively. In total there were 36 questions, and the entire survey took between 5 and 15 min to complete. The survey is available on-line or on request of the authors.
The survey was distributed to 515 people. Of the respondents, 458 (89%) completed over half of the survey and are the focus of our analyses. The 57 people who did not complete at least half of the survey were dropped from all analyses. Due to poor formatting, 115 respondents missed a question about cholesterol, so we omitted all questions about cholesterol from our analyses. Otherwise all opinion and clinical questions were answered by at least 431 respondents. Eighty-one respondents did not provide an age, and 59 respondents did not provide an income category.
Analyses
We conducted descriptive analyses describing means and distributions using t-tests to compare mean responses between smokers and non-smokers, as well as patients with and without obesity, hypertension, and diabetes. We used logistic regression analyses to determine which variables were most strongly associated with thinking that paying patients to quit smoking or lose weight was a good or excellent idea. Potential independent variables included: demographics (age, sex, education, and income); smoking status; presence of obesity, hypertension or diabetes; and all answers pertaining to opinions about smokers or overweight people, or general attitudes about P4P4P. Income was entered as an ordinal variable with $60,000 and above as the reference category so as to include people with missing income in the analyses. To include age, which also had high levels of missing data, we broke age down into the following categories: <25, 25−<45, 45−<65, 65+, and missing age; 65+ was made the reference category. Due to their correlation with the dependent variables, questions assessing how much a person was willing to pay someone to quit smoking or lose weight were not included in the regressions. For the regressions only, all opinion questions with 5-point Likert responses were dichotomized (good/excellent idea versus all others and agree/strongly agree versus all others). Variables were entered into the regressions in a stepwise manner and retained if they were significant at p < 0.05.
RESULTS
Demographics
The respondents were 52% female. The mean age was 50 years old (SD 16, range 16–91). Thirty-one percent had a high school education or less, 28% had completed some college, and 42% had a college education or more. The median annual income was between $45,000 and $50,000 and 25% reported an annual income of less than $30,000 (21% did not respond to the income question or did not know their income). Twenty percent of the sample smoked, 25% reported being obese, 42% reported having hypertension, and 13% reported having diabetes.
Descriptive Statistics
There were both similarities and important differences across disease conditions in respondents’ feelings about P4P4P (see Table 1). Thirty-six to 42% thought it was a good/excellent idea to pay smokers to quit smoking, obese people to lose weight, people with hypertension to control their blood pressure, or people with diabetes to control their blood sugar, while 41–44% of the sample thought it was a bad/very bad idea. However, the framing of questions affected responses. While 67% of respondents thought it was a good/excellent idea to charge non-smokers less for health insurers (framed as a reward), only 54% favored charging smokers higher premiums (framed as a punishment). Similarly, respondents were more enthusiastic about charging non-obese people less (43%) for health insurance than they were about charging obese people more (32%).
Table 1.
Opinions Regarding Financial Incentives
| Very bad/bad | Neutral | Good/ excellent | |
|---|---|---|---|
| Paying | |||
| Smokers to quit smoking | 44.1% | 17.3% | 38.6% |
| Obese people to loose weight | 40.5% | 18.1% | 42.4% |
| People with HTN to control their blood pressure | 42.8% | 21.5% | 35.7% |
| People with DM to control their blood sugar | 41.3% | 23.1% | 35.6% |
| Charging for health insurance | |||
| Charge non-smokers less | 22.8% | 10.0% | 67.2% |
| Charge smokers more | 27.8% | 17.8% | 54.4% |
| Charge non-obese less | 33.6% | 23.4% | 43.0% |
| Charge obese more | 42.2% | 25.3% | 32.4% |
| Insurance should offer incentives to reward healthy behavior | 18.8% | 18.8% | 62.4% |
| Strongly disagree/disagree | Neutral | Agree/ strongly agree | |
| People who smoke have mostly themselves to blame | 24.2% | 12.0% | 63.9% |
| People who are obese have mostly themselves to blame | 54.9% | 21.1% | 24.0% |
| People who have high blood pressure have mostly themselves to blame | 76.3% | 12.4% | 11.3% |
| People who have diabetes have mostly themselves to blame | 78.5% | 13.4% | 8.2% |
| Paying smokers to quit will lower everyone’s health costs | 37.1% | 17.4% | 45.5% |
| Paying smokers to quit is not fair to non-smokers | 37.6% | 21.6% | 40.8% |
| Paying people to quit smoking may be one of the only effective means to get people to quit | 47.0% | 20.7% | 30.3% |
| Paying people to lose weight rewards obese people | 41.1% | 23.0% | 35.9% |
| Paying people to lose weight would be an effective incentive | 38.2% | 19.3% | 42.5% |
| People should not be paid to do things they should do anyway | 28.8% | 18.4% | 53.1% |
*Five-point scale from 1 (very bad) to 5 (excellent)
**Five-point scale from 1 (strongly disagree) to 5 (strongly agree)
There were large differences in feelings about whether these behaviors are the fault of the individuals in question (Table 1). While the majority of respondents felt that smokers were to blame for their smoking (64% strongly agreed/agreed, while 24% disagreed/strongly disagreed), the vast majority of respondents disagreed/strongly disagreed with the assertion that people with hypertension (76%) or people with diabetes (79%) had themselves to blame for their illness. Respondents had more ambivalent feelings about whether obese people were to blame for their weight, with 55% or respondents disagreeing/strongly disagreeing with this assertion.
Respondents showed some ambivalence about the fairness and likely effectiveness of rewarding people for healthy behaviors. Sixty-two percent endorsed the idea that it was a good/excellent idea for their health insurance company to offer incentives to reward healthy behavior, but 53% agreed/strongly agreed that people should not be paid to do things they should do anyway. Forty-six percent of respondents agreed/strongly agreed that paying smokers to quit would lower everyone’s health-care costs, but 41% thought it would be unfair to non-smokers to do so. Thirty percent strongly agreed/agreed that paying people to quit smoking may be one of the only effective ways to help people quit smoking, while 47% disagreed/strongly disagreed with that statement. A slightly higher percentage of respondents thought that paying people to lose weight would be effective (43% agreed/strongly disagreed) as compared to 38% who strongly disagreed/disagreed. Respondents were also split fairly evenly on the question of whether paying people to lose weight rewards obese people.
When asked how much money would be appropriate to pay patients to quit smoking, lose weight, control their blood pressure, or control their blood sugar, 51–53% responded $0, 35–40% responded $50–$500, and 10%–13% responded $1,000 or more (Fig. 1). The median response was $0 for all four health outcomes. The Pearson correlation coefficients between the four variables asking how much money patients thought should be paid for successful health outcomes (quitting smoking, losing weight, controlling blood pressure, and controlling blood sugar) ranged from 0.82–0.95. This suggests that participants did not differentiate much between the type of health outcomes considered in regards to how much to pay for succesful health outcomes, but instead approached them all similarly.
Figure 1.
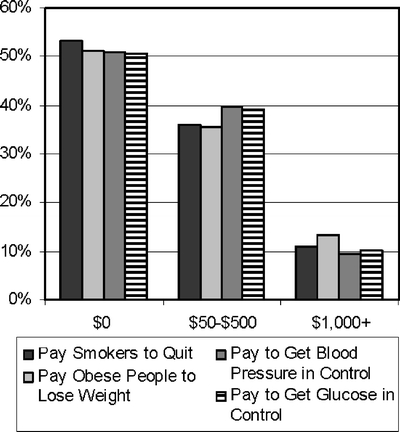
How much people are willing to pay others for health outcomes.
Comparisons Across Patients’ Medical Conditions
Smokers were more likely than non-smokers to think it was a good idea to pay smokers to quit (mean score 3.4 versus 2.7, p < 0.001), to think that paying smokers to quit will lower everyone’s health costs (mean score 3.4 versus 2.0, p = 0.029), and to think it may be one of the only effective means to increase quit rates (mean score 3.1 versus 2.6, p < 0.001) (Table 2). Smokers were less likely than non-smokers to want to charge non-smokers less for health insurance (mean score 3.1 versus 3.9, p < 0.001) or to charge smokers more for health insurance (mean score 2.8 versus 3.6, p < 0.001). Similarly, obese people were more likely than non-obese people to think it a good idea to pay obese people to lose weight (mean score 3.2 versus 2.9, p = 0.038) and to think paying people to lose weight would be an effective incentive (mean score 3.3 versus 3.0, p = 0.010). Ratings about the desirability of payments did not differ for people with hypertension compared to those without hypertension or for people with diabetes compared to those without diabetes. Of note, among patients without these conditions, mean scores for the questions relating to whether it is a good idea to pay smokers to quit, obese people to lose weight, people with hypertension to control their hypertension, or people with diabetes to control their blood sugar varied little, ranging from 2.7 to 2.9.
Table 2.
Health-specific Opinions as a Function of the Type of Health Problem
| Non-smokers mean ± SD | Smokers mean ± SD | T-test p value | |
|---|---|---|---|
| Pay smokers to quit? | |||
| Is it a good idea to pay smokers to quit smoking? | 2.7 ± 1.6 | 3.4 ± 1.6 | <0.001 |
| Charging for health insurance | |||
| Charge non-smokers less | 3.9 ± 1.5 | 3.1 ± 1.6 | <0.001 |
| Charge smokers more | 3.6 ± 1.5 | 2.8 ± 1.6 | <0.001 |
| Smoking specific attitudes | |||
| Paying smokers to quit will lower everyone’s health costs | 3.0 ± 1.3 | 3.4 ± 1.3 | 0.029 |
| Paying smokers to quit is not fair to non-smokers | 3.1 ± 1.3 | 2.9 ± 1.1 | 0.218 |
| Paying people to quit may be one of the only effective means to increase quit rates | 2.6 ± 1.2 | 3.1 ± 1.2 | <0.001 |
| People who smoke have mostly themselves to blame | 3.6 ± 1.3 | 3.4 ± 1.3 | 0.125 |
| General attitudes | |||
| Insurance should offer incentives to reward healthy behavior | 3.8 ± 1.6 | 3.6 ± 1.4 | 0.239 |
| People should not be paid to do things they should do anyway | 3.4 ± 1.3 | 3.4 ± 1.9 | 0.700 |
| Not obese mean ± SD | Obese mean ± SD | T-test p value | |
| Pay obese people to lose weight? | |||
| Is it a good idea to pay obese people to lose weight? | 2.9 ± 1.6 | 3.2 ± 1.6 | 0.038 |
| Charging for health insurance | |||
| Charge non-obese less | 3.2 ± 1.6 | 3.1 ± 1.5 | 0.709 |
| Charge obese more | 2.8 ± 1.5 | 2.6 ± 1.4 | 0.279 |
| Weight-specific attitudes | |||
| Paying people to lose weight rewards obese people | 2.9 ± 1.2 | 2.9 ± 1.2 | 0.833 |
| Paying people to lose weight would be an effective incentive | 3.0 ± 1.3 | 3.3 ± 1.3 | 0.010 |
| People who are obese have mostly themselves to blame | 2.5 ± 1.2 | 2.5 ± 1.2 | 0.701 |
| General attitudes | |||
| Insurance should offer incentives to reward healthy behavior | 3.71.4 | 3.7 ± 1.4 | 0.950 |
| People should not be paid to do things they should do anyway | 3.5 ± 1.3 | 3.3 ± 1.2 | 0.176 |
Five-point scale from 1 (strongly disagree or very bad idea) to 5 (strongly agree to excellent idea)
Regression Analysis
In multivariate logistic regression (Table 3), the following variables were associated with an increased odds of holding the opinion that paying patients to quit smoking was a good or excellent idea: being a current smoker; thinking that paying smokers to quit will lower everyone’s health costs and might be one of the only effective means of getting people to quit; and thinking incentives to reward healthy behavior are a good/excellent idea. Variables that were negatively associated with increased odds of agreeing that paying patients to quit smoking was a good or excellent idea included male gender, having diabetes, rating charging smokers more for health insurance as a good/excellent idea; expressing the view that paying smokers to quit is unfair; and agreeing or strongly agreeing that others should not be paid to do things they should do anyway.
Table 3.
Odds of Thinking Paying Patients for Health Outcome is a Good/Excellent Idea
| OR (95% CI)* | |
|---|---|
| Quit smoking | |
| Men | 0.51 (0.29–0.90) |
| Smokers | 2.73 (1.34–5.59) |
| Patients with diabetes | 0.23 (0.09–0.55) |
| Thinks charging smokers more for health insurance is a good/excellent idea | 0.47 (0.25–0.90) |
| Agrees/strongly agrees paying smokers to quit will lower everyone’s costs | 4.76 (2.63–8.63) |
| Agrees/strongly agrees paying smokers to quit is not fair to non-smokers | 0.31 (0.16–0.60) |
| Agrees/strongly agrees paying people to quit may be one of the only effective means to increase quit rates | 5.72 (2.90–11.28) |
| Thinks insurance offering incentives to reward healthy behavior is a good/excellent idea | 7.16 (3.50–14.64) |
| Agrees/strongly agrees people should not be paid to do things they should do anyway | 0.23 (0.13–0.43) |
| Lose weight | |
| Agrees/strongly agrees paying people to lose weight rewards obese people | 0.51 (0.28–0.91) |
| Agrees/strongly agrees paying people to lose weight would be an effective incentive | 11.89 (6.92–20.42) |
| Thinks insurance should offer incentives to reward healthy behavior is a good/excellent idea | 5.61 (3.12–9.92) |
| Agrees/strongly agrees people should not be paid to do things they should do anyway | 0.23 (0.13–0.39) |
*Odds ratios (95% confidence intervals) are from multivariate logistic regression, which adjusts for all the other variables presented in this Table
In the regression evaluating weight loss (Table 3) agreeing or strongly agreeing that paying people rewards obese people and that people should not be paid to do things they should do anyway were assciated with a lower odds of thinking it was a good/excellent idea to pay people to lose weight. Agreeing/strongly agreeing that incentives might be effective and thinking incentives to reward healthy behavior are a good/excellent idea were associated with an increased odds of thinking it was a good/excellent idea.
Income and education were not independently associated with whether a person thought it was a good or excellent idea to pay smokers to quit smoking or obese people to lose weight. All variables retained in either regression had a Pearson’s correlation coefficient of 0.47 or less.
DISCUSSION
We believe this is the first survey done on patients’ opinions of the acceptability of paying for performance for patients (P4P4P). Respondents were almost evenly split on whether this is desirable, with 36–42% describing it as good/excellent idea, while 40–44% thought it was a bad/very bad idea. The framing of questions appears to matter, with respondents replying more favorably when statements were framed as rewards as opposed to punishments. While paying patients for performance may be an effective means to reduce the rate of unhealthy behaviors within the US population, opinions about such approaches are mixed. Given the relative lack of improvement in quality observed to date through provider-targeted P4P, these findings have potentially important implications for companies that are beginning to embrace the use of financial incentives for healthy behaviors as a potential way to reduce health-care costs and improve productivity in their workforce, as well as for insurers and policy makers considering wider spread use of P4P4P.7–9
The survey questions focused on rewards for change in behavior (losing weight), though most existing P4P programs reward absolute achievement (getting weight below some pre-set threshold). We did this because we feel that tying incentives to changes in behavior is more likely to increase the rate of healthy behaviors than if such programs focus on absolute achievement. Differences in ratings of desirability of P4P4P for different health problems appears to be driven in part by smokers and obese people more enthusiastically endorsing the concept that payments may lead to positive outcomes. This could be because patients who have these conditions have found changing the behavior in question (smoking, losing weight) difficult and are more eager to consider a new means of achieving their goals than people without these conditions who have not experienced these difficulties. If this is true, further evidence that P4P4P is effective in improving patient health outcomes could lead to wider support for these programs.
If further tests of P4P4P indicate that this approach is effective and cost effective, it will be important to assess how to best target such programs. They may be more effective in lower income populations because the same dollar amount would conceivably have greater influence; if so, such approaches could help ameliorate health disparities; however, ethical consideration will need to be given to whether these programs are unduly coercive for lower income populations. Consideration will also be needed of how to appropriately frame such interventions to maximize fairness and minimize gaming.
The main limitation of this study is that it was based on a convenience sample, and we have no information about the people who refused to participate and how they may have been systematically different from survey respondents. In addition our sample was derived from only two university-based practices, both of which are in West Philadelphia, and thus is geographically limited. The generalizability of our results is therefore unknown, though this population would be similar to other populations cared for in many of the academic medical centers in the US.
Our data reveal some mixed support of widespread use of incentives to change behavior, though resistance was expressed less in terms of the general idea and more directly in terms of only moderate enthusiasm for specific initiatives. When programs were framed in terms of health insurance premiums, respondents were more willing to endorse them, especially when they rewarded good behaviors, such as charging non-smokers less for health insurance, rather than penalizing smokers by charging more. Ultimately if these programs are to become more widespread, determining how best to design them, both in regards to the types of incentives as well as the targets of the incentives, will be important. As the first study of its kind, this study provides a benchmark by which to assess the acceptability of P4P4P among insured populations who have so far been the target of these programs.
Given the prevalence of unhealthy behaviors within the US population, serious consideration needs to be given to any approach that may effectively motivate improvements in the rate of healthy behavior.
Electronic supplementary material
Electronic supplementary material
(PDF 53.4 KB)
Acknowledgements
The work in this paper was supported by a grant from the Commonwealth of Pennsylvania, titled Collaboration to Reduce Disparities in Hypertension, grant no. ME-02-382.
The Commonwealth bears no responsibility for the content of this article. This paper was presented as a poster at the Society of General Internal Medicine 2007 National Meeting in Toronto, Canada, 2007.
Conflict of Interest Drs. Long and Helweg-Larsen have no conflicts of interest in relationship to this work. Dr. Volpp received an honorarium from Astra Zeneca for convening a conference on medication adherence as well as receiving investigator initiated grant support from Pfizer for ongoing patient follow-up for a randomized controlled trial of copayment reductions that was initiated through the grant that also supported this work (the Commonwealth of Pennsylvania sponsored Collaboration to Reduce Disparities in Hypertension, grant no. ME-02-382).
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-008-0739-1) contains supplementary material, which is available to authorized users.
References
- 1.Galvin R. Evaluating the performance of pay for performance. Med Care Res Rev. 2006;63(1):126S–130S. [DOI] [PubMed]
- 2.Epstein AM, Lee TH, Hammel MB. Paying physicians for high-quality care. New Engl J Med. 2004;350(4):406–410. [DOI] [PubMed]
- 3.Epstein AM. Paying for performance in the United States and abroad. New Engl J Med. 2006;355(4):406–408. [DOI] [PubMed]
- 4.Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. New Engl J Med. 2006;355(4):375–384. [DOI] [PubMed]
- 5.Chassin MR. Does paying for performance improve the quality of health care? Med Care Res Rev. 2006;631(1):22S–125S. [DOI] [PubMed]
- 6.Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Annals Int Med. 2006;145(4):265–272. [DOI] [PubMed]
- 7.Glickman SW, Ou FS, DeLong ER, et al. Pay for performance, quality of care, and outcomes in acute myocardial infarction. JAMA. 2007;297(21):2373–2380. [DOI] [PubMed]
- 8.Lindenauer PK, Remus D, Roman S, Rothberg MB, Benjamin EM, Ma A, Bratzler DW. Public reporting and pay for performance in hospital quality improvement. New Engl J Med. 2007;356(5):486–496. [DOI] [PubMed]
- 9.Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: from concept to practice. JAMA. 2005;294(14):1788–1793. [DOI] [PubMed]
- 10.Schroeder SA. Shattuck Lecture. We can do better - improving the health of the American People. New Engl J Med. 2007;357(12):1221–1228. [DOI] [PubMed]
- 11.Centers for Disease Control and Prevention. Annual smoking-attributable mortality, years of potential life lost, and economic costs- United States, 1995–1999. MMWR Morb Mortal Wkly Rep. 2002;51(14):300–303. [PubMed]
- 12.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who’s paying? Health Aff (Millwood). Jan–Jun 2003;Suppl Web Exclusives:W3-219-226. http://content.healthaffairs.org/cgi/content/full/hlthaff.w3.219v1/DC1 Last Accessed July 2, 2008 [DOI] [PubMed]
- 13.Yi D. For Many Employees, Fitness has its Prize. Los Angeles Times, March 12 2007.
- 14.Mcqueen MP. Wellness plans reach out to the healthy. Wall Street Journal Abstracts, 2007;March 28: D1.
- 15.Jordan S. Financial carrot is a healthy incentive, more companies use enticing benefits to lure workers into wellness programs. Omaha World Herald, 2007;March 25:A1.
- 16.Song KM. New health-benefits plan prompts county workers to diet and head for the gym. The Seattle Times, 2006;July 22:A1.
- 17.Conlin M. Get healthy _ or else. inside one company’s all-out attack on medical costs. Business Week Online, 2007;February 26. Available at http://www.businessweek.com/magazine/content/07_09/b4023001.htm Last Accessed July 2, 2008
- 18.Steinbrook R. Imposing personal responsibility for health. New Engl J Med. 2006;355(8):753–756. [DOI] [PubMed]
- 19.West Virginia’s Medicaid State Plan Amendment (SPA) 06-02, approved by the Centers for Medicare & Medicaid Services, Department of Health and Human Services, May 3, 2006. Available at http://www.wvdhhr.org/bms/oAdministration/bms_admin_WV_SPA06-02_20060503.pdf Last Accessed July 2, 2008
- 20.Donatelle RJ, Hudson D, Dobie S, Goodall A, Hunsberger M, Oswald K. Incentives in smoking cessation: status of the field and implications for research and practice with pregnant smokers. Nicotine & Tobacco Research. 2004;9(Supplement 2):S163–S179. [DOI] [PubMed]
- 21.Volpp KG, Gurmankin Levy A, Asch DA, et al. A randomized controlled trial of financial incentives for smoking cessation. Cancer Epidemiol Biomarkers Prev. 2006;15(1):12–18, Jan. [DOI] [PubMed]
- 22.Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2005;101:102–203. [DOI] [PubMed]
- 23.Higgins ST, Silverman K, eds. Motivating Behavior Change Among Illicit Drug Abusers: Research on Contingency Management Interventions. Washington, DC: American Psychological Association; 1999.
- 24.Marcus AC, Kaplan CP, Crane LA, et al. Reducing loss-to-follow-up among women with abnormal Pap smears. Results from a randomized trial testing an intensive follow-up protocol and economic incentives. Med Care. 1998;36(3):397–410, Mar. [DOI] [PubMed]
- 25.Stevens-Simon C, O’Connor P, Bassford K. Incentives enhance postpartum compliance among adolescent prenatal patients. J Adolesc Health. 1994;15(5):396–399, Jul. [DOI] [PubMed]
- 26.Malotte CK, Rhodes F, Mais KE. Tuberculosis screening and compliance with return for skin test reading among active drug users. Am J Public Health. 1998;88(5):792–796, May. [DOI] [PMC free article] [PubMed]
- 27.Seal KH, Kral AH, Lorvick J, McNees A, Gee L, Edlin BR. A randomized controlled trial of monetary incentives vs. outreach to enhance adherence to the hepatitis B vaccine series among injection drug users. Drug Alcohol Depend. 2003;71(2):127–131, Aug 20. [DOI] [PubMed]
- 28.Jeffery RW, Thompson PD, Wing RR. Effects on weight reduction of strong monetary contracts for calorie restriction or weight loss. Behav Res Ther. 1978;16(5):363–369. [DOI] [PubMed]
- 29.Finkelstein EA, Linnan LA, Tate DF, Birken BE. A pilot study testing the effect of different levels of financial incentives on weight loss among overweight employees. J Occup Environ Med. 2007;49(9):981–989, Sep. [DOI] [PubMed]
- 30.Jeffery RW, Gerber WM, Rosenthal BS, Lindquist RA. Monetary contracts in weight control: effectiveness of group and individual contracts of varying size. J Consult Clin Psychol. 1983;51(2):242–248, Apr. [DOI] [PubMed]
- 31.Sindelar J, Elbel B, Petry NM. What do we get for our money? Cost-effectiveness of adding contingency management. Addiction. 2007;102(2):309–316, Feb. [DOI] [PubMed]
- 32.Sindelar JL, Olmstead TA, Peirce JM. Cost-effectiveness of prize-based contingency management in methadone maintenance treatment programs. Addiction. 2007;102(9):1463–1471, Sep. [DOI] [PMC free article] [PubMed]
- 33.Kane RL, Johnson PE, Town RJ, Butler M. A structured review of the effect of economic incentives on consumers’ preventive behavior. Am J Prev Med. 2004;27(4):327–352. [DOI] [PubMed]
- 34.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Electronic supplementary material
(PDF 53.4 KB)


