Abstract
Objective
To impute limited health literacy from commonly measured socio-demographic data and to compare it to the Short-Test of Functional Health Literacy in Adults (S-TOFHLA) for estimating the influence of limited health literacy on health status in the elderly.
Methods
The Prudential Medicare Study assesses the S-TOFHLA score, leading to a “reference standard” classification of 25% of people with inadequate literacy; the National Health Interview Survey has no such assessment. We estimated a regression of S-TOFHLA on sex, age, years of schooling, and race/ethnicity in The Prudential Medicare Study data to derive a Demographic Assessment for Health Literacy (DAHL) score, and imputed inadequate literacy to the 25% with the lowest DAHL scores. Using regression, we then examined associations between several health status measures (including hypertension, diabetes, physical and mental SF-12) and inadequate literacy (imputed or test-based).
Results
Estimates of association using imputed inadequate literacy closely approximate those obtained using S-TOFHLA-based inadequate literacy for most outcomes examined.
Conclusions
As few population surveys measure health literacy, the DAHL, a readily calculated health literacy proxy score, may be useful for expanding the scope of health literacy research in national survey data.
KEY WORDS: inadequate health literacy, health status, functional status, national surveys
With approximately 90 million American adults estimated to lack the literacy skills needed to use the health-care system1,2, an emerging literature has begun to describe the myriad health consequences of limited health literacy3. The Institute of Medicine (IOM) defines health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” Limited health literacy is an independent risk factor for worse health status, hospitalization, and mortality3,4. Virtually all health literacy research relies on data from specially designed surveys with in-person administration of a validated health literacy test – such as the Test of Functional Health Literacy in Adults (TOFHLA) and the Rapid Estimate of Adult Literacy in Medicine (REALM)5–7. To date, few surveys directly measure health literacy. Most that do are small and pertain to patients in specific clinical settings. Major national population health surveys, such as the National Health Interview Survey (NHIS), the Behavioral Risk Factor Surveillance System (BRFSS), and the National Health and Nutrition Examination Survey (NHANES), have no measure of health literacy.
Multiple reports have found high correlations between test-based health literacy measures and demographic indicators such as age, ethnicity, and years of schooling5,7–10. Imputed measures based on combinations of these indicators have been proposed11,12. Miller et al. found high construct validity by showing the correlation of their imputed measure with other indicators of health literacy12. Since large national health surveys do capture basic socio-demographic indicators, they can support an imputed health literacy measure. Such imputation will expand the scope of health literacy research to a much wider range of measures of health status, outcomes, and interventions.
Here, we propose an imputed measure of health literacy for community-living elderly, to be called the Demographic Assessment for Health Literacy (DAHL), and examine its comparative performance as a proxy for test-based measures in models to assess the influence of health literacy on health status. It is calculated from limited, broadly available data – sex, age, years of schooling and race/ethnicity. We develop the DAHL from Prudential Medicare Study data (1997), the largest population-based health literacy study to date. Our primary objective is to assess the performance of this imputed measure as a covariate in models of health status in the Prudential Study and in the National Health Interview Survey (1997 and 2005).
METHODS
The Prudential Medicare Study (1997)
The Prudential Medicare Study is an in-person survey administered to people, aged 65 or older, newly enrolled in the Medicare HMO plans of Prudential Healthcare in four locations (Cleveland, Ohio; Houston, Texas; South Florida; Tampa, Florida) between December 1996 and August 1997, excluding those who did not live in the community, with severe cognitive impairment, or who were not comfortable speaking either in English or Spanish. Among 8,409 persons in the sampling frame, 57 percent could not be contacted (938 enrollees), refused to participate (3,247), or were not eligible for interview (737). An additional 227 enrollees did not cooperate during data collection. The final respondent sample was 3,260 enrollees with an effective response rate of 47 percent, using American Association of Public Opinion Research’s definition no. 3, or 42.5 percent assuming all non-respondents were eligible.13 Non-respondents were slightly older with higher educational attainment and were more likely to be white and living in zip codes with higher median income10. Additional details of this survey have been published previously6,10,14–18. Starting with this sample of 3,260, we excluded 282 subjects with history of stroke, 55 with severe cognitive impairment (Mini-Mental State Examination Score <18), and 99 with a missing value in one of the fields examined in this study18,19, leaving a final analytic sample of 2,824.
An in-person baseline survey collected data on demographic, socioeconomic, and health characteristics and administered the Short Test of Functional Health Literacy in Adults (S-TOFHLA). This test includes a 36-item reading comprehension section and a 4-item numeracy section using materials and situations likely to be encountered by the elderly in health-care settings.
Health literacy is multifaceted, with a fundamental component being reading fluency as measured by the S-TOFHLA, one of the most commonly used instruments in health literacy research5. S-TOFHLA correlates well with other tests of health literacy, tests of general literacy, and several health outcomes1,3,7. The ability to read and take action based on health-related material may be closely related to the ability to read and act on other types of materials. We refer to the construct measured by the S-TOFHLA as “health literacy,” although some authors view it as referring more narrowly to general literacy skills in the context of health care3,8.
Following others, we summarized the S-TOFHLA responses in a composite score (range: 0 to 100) and categorized scores ≤53 (the lowest quartile in the Prudential data) as “inadequate” versus a merged category of “marginal (11%) or adequate (64%).” The “marginal” group was both small and similar in all characteristics of interest to those with “adequate” literacy6,18,19.
The outcome measures are several self-reported indicators of health status – poor or fair health, hypertension, diabetes, Short Form Health measures (physical and mental SF-12)20, difficulty with IADL (Instrumental Activities of Daily Living), and ADL (Activities of Daily Living). As a marker of substandard preventive care, we used a self-reported dichotomous indicator for never having been vaccinated for flu.
National Health Interview Survey (1997, 2005)
The National Health Interview Sample (NHIS) is an in-person, nationally representative annual survey covering many health-related, demographic, and socio-economic measures21. We selected the 1997 round to match the time of the Prudential Medicare Study, focusing on the 6,972 respondents aged 65 or older. We excluded an additional 153 due to missing information on at least one study measure, resulting in a study sample of 6,819. To assess the robustness of DAHL, we also performed parallel analyses using 5,914 analogously identified respondents from NHIS 2005.
While the NHIS does not measure health literacy, NHIS data are identical or nearly identical for four of the eight outcomes captured in the Prudential Medicare Study – self-reported general health (poor/fair), hypertension, diabetes, and difficulty with ADL. Although the NHIS instrument uses a seventh item (“difficulty getting around inside the home”), the other six ADL questions in NIHS are identical to the six ADL questions used in the Prudential Medicare Study. We judged these measures to be sufficiently comparable for our study of within-cohort associations between health literacy measures and outcomes. In contrast, we viewed the NHIS and Prudential IADL measures as too different to support useful comparisons.
Defining Components of the DAHL
Our goal was to predict health literacy well from characteristics that are commonly ascertained in national surveys. Besides the DAHL, which uses four SES indicators (age, sex, race, and education), we also examined an “education only” model, as well as models that added measures to the DAHL, including difficulty in reading and understanding forms at doctor visits, seeking help for reading forms at doctor or hospital visits, frequency of reading newspapers, and current employment status. Also, following Miller, Degenholtz et al. 2007, we explored models with interactions among education, age, and race.
Statistical Analysis
First, we used data from the Prudential Medicare Study and regression to derive the equations (scoring weights) that predict S-TOFHLA from various predictors. We then applied these weights to the values of the predictors in the NHIS data to produce an imputed literacy score (DAHL) for each Prudential and NHIS respondent. This is analogous to developing a coronary heart disease risk score with data from the Framingham Heart study (which included both risk factors and coronary heart disease outcomes) and then disseminating the scoring mechanism to predict coronary heart disease risk for people in other settings where the values of the risk factors are known, but coronary health status is not known22. Using the Prudential data and various cutoffs (for inadequate literacy) for each model, we estimated measures of agreement (sensitivity, specificity) and discrimination (area under the receiver operating characteristic, or C-statistic) as descriptors of each model’s ability to predict S-TOFHLA-based inadequate literacy23. Since DAHL is derived from coefficient estimates, its precision can be gauged from the 95% confidence interval (CI) of the predicted DAHL score at the mean level of factors. The model specification with the best trade-off between simplicity and predictive ability was selected as “the” DAHL. Its associated weights were then used to calculate DAHL scores for each person in the Prudential and NHIS samples. Within each sample, the imputed literacy indicator was defined analogously, with the bottom 25 percent classified as having inadequate literacy.
The DAHL was examined for how closely its association with the various health status measures approximates the association of the S-TOFHLA with that measure in the Prudential study. We first estimated reference effects using the S-TOFHLA-based inadequacy indicator to predict each of the eight selected health status measures in the Prudential data. Each estimate was obtained from a multivariable regression (logistic for dichotomous and linear for ordinal measures) on the test-based indicator for inadequate literacy in addition to sex, age, years of schooling, race/ethnicity, household income, and marital status.
Analogous regressions were estimated using an imputed inadequate literacy indicator, however, with only household income and marital status as additional covariates, since the DAHL is completely identified by sex, age, years of schooling, and race/ethnicity. We repeated this for all eight health status measures in the Prudential study and for the four measures in NHIS – the latter for both 1997 and 2005 data. As the NHIS survey is a multi-stage stratified sample with sampling weights differing across subgroups, we used corrective survey-adjusted weights to obtain both rates and standard errors. For the Prudential Study, we follow previous studies in treating the data as self-representative10.
Sensitivity Analysis
We evaluated the robustness of the regression estimates to the choice of threshold score for classifying those with inadequate literacy – both for the S-TOHFLA and the DAHL measures. We chose a wide range of score thresholds (from 50 to 87), while ensuring that either side of the threshold has at least 10% of sample subjects. We obtained an estimate of the association with inadequate literacy from each cut-off and compared the corresponding estimates from the two literacy measures graphically.
While all subjects in the Prudential Medicare Study are HMO enrollees, those in NHIS include Medicare HMO as well as Fee-for-Service enrollees. As these two types of NHIS enrollees may differ in terms of health literacy, socioeconomic status, and health indicators, we also examined the differences in imputed literacy scores in these cohorts separately. All statistical analyses were performed using Stata 9.224. The Institutional Review Board of Boston University School of Medicine approved the study protocol.
RESULTS
We studied 2,824 subjects from the Prudential Medicare Study and 6,819 subjects from the 1997 round of NHIS. Although the Prudential Medicare Study includes only four cities/regions, its respondents are similar to those in the NHIS sample (Table 1). The S-TOHFLA-based health literacy score ranged from 0 to 100, with a mean of 73 and standard deviation of 26 in the Prudential study,
Table 1.
Characteristics of the Prudential Medicare Study and National Health Interview Survey (NHIS)-Elderly Samples, 1997
| Prudential Study 1997 | NHIS-Elderly 1997 | |
|---|---|---|
| (N = 2,824) | (N = 6,819) | |
| Female, % | 58 | 62 |
| Age, % | ||
| 65–69 | 37 | 27 |
| 70–74 | 28 | 27 |
| 75–79 | 19 | 22 |
| 80–84 | 11 | 15 |
| 85 | 5 | 10 |
| Race/ethnicity, % | ||
| Black | 11 | 8 |
| White | 76 | 86 |
| Hispanic | 12 | 4 |
| Other | 1 | 2 |
| Marital status, % | ||
| Married | 55 | 42 |
| Previously married | 43 | 54 |
| Never married | 2 | 5 |
| Years of schooling completed, % | ||
| 0–8 | 17 | 19 |
| 9–11 | 18 | 18 |
| 12 or GED | 34 | 32 |
| >12 | 30 | 31 |
| Annual income, % | ||
| Less than $10,000 | 20 | 25 |
| $10,001 - $15,000 | 24 | 13 |
| $15,001 - $25,000 | 35 | 29 |
| $25,001 - $35,000 | 9 | 11 |
| $35,001+ | 12 | 23 |
| Test-based literacy | ||
| S-TOHFLA health literacy score, mean (SD) | 71.3 (26.8) | NA |
| Inadequate health literacy (S-TOHFLA ≤53), % | 25 | NA |
| Self-reported health/chronic condition | ||
| General health - fair or poor, % | 24 | 26 |
| Hypertension, % | 45 | 52 |
| Diabetes, % | 14 | 13 |
| Difficulty with ADL, % | 3.3 | 5.3 |
| Difficulty with an IADL, % | 28 | NA |
| Never had flu vaccination, % | 21 | NA |
| Physical SF-12 score, mean (SD) | 45.8 (10.9) | NA |
| Mental SF-12 score, mean (SD) | 55.2 (8.5) | NA |
Note: Estimates for NHIS 1997 are weighted to adjust for the sampling design
NA = Not available in NHIS
Table 2 shows the score weights for the DAHL, calculated as the sum of the score for the reference group minus adjustments for other demographic cohorts. Specifically, white women aged 65–69 with more than 12 years of schooling (the reference group) receive a mean DAHL of 91.3, the highest possible imputed score. Less schooling, older age, and other races and ethnicities result in lower imputed health literacy. The lowest possible imputed literacy score is 15.6 among Black males 85 or older with fewer than 9 years of schooling. At the mean value of the factors determining DAHL, the predicted literacy score, which by design equals the mean of the test-based score (73.0), had a 95% confidence interval of [72.2, 73.8].
Table 2.
Obtaining the Demographic Assessment of Health Literacy (DAHL)
| (The Prudential Medicare Study 1997, N = 2,824) | ||
|---|---|---|
| Health Literacy Score | 95% CI | |
| Reference group: | ||
| DAHL for White women aged 65–69 with >12 years of schooling | 91.3 | [89.3, 93.2] |
| Adjustments for other groups: | ||
| Gender | ||
| Male | -1.8 | [-3.5, -0.27] |
| Age | ||
| 70–74 | -5.5 | [-7.5, -3.5] |
| 75–79 | -10.9 | [-13.1, -8.65] |
| 80–84 | -16.2 | [-18.9, -13.4] |
| 85+ | -27.8 | [-31.8, -23.9] |
| Race/ethnicity | ||
| Black | -15.9 | [-18.5, -13.4] |
| Hispanic | -6.7 | [-9.4, –3.9] |
| Other | -8.7 | [-15.8, -1.7] |
| Years of schooling completed | ||
| 0–8 | -30.2 | [-32.7, -27.6] |
| 9–11 | -15.9 | [-18.3, -13.6] |
| 12 or GED | -6.2 | [-8.1,-4.2] |
In the Prudential data, the S-TOHFLA and DAHL are highly correlated (ρ = 0.58), and a linear regression of DAHL on S-TOHFLA gives a coefficient estimate of 0.93. We defined “inadequate health literacy” in the Prudential Study as having an S-TOHFLA score in the lowest 25th percentile (≤53) and imputed “inadequacy” for the 25% of Prudential study persons with the lowest DAHL (≤62). With these definitions, 79% of cases are correctly classified by the DAHL, sensitivity for detecting “inadequacy” is 59%, and specificity, 84%. Using a DAHL threshold of 69 increases sensitivity to 72%, but lowers specificity to 77%. The area under the receiver operating curve (the C-statistic) is 0.81 [95% CI = (0.79, 0.83)], indicating that, overall, DAHL discriminates well among people with higher and lower S-TOFHLA scores. Adding interaction terms for education, race, and age to the DAHL left the C-statistic at 0.81, while predicting inadequate literacy from only the single best measure (“education”) is much less effective: sensitivity (58%), specificity (10%), and C-statistic = 0.72. Augmenting the DAHL with measures for difficulty in reading forms, seeking help in reading forms, newspaper reading frequency, and current employment status only modestly improves discrimination (C-statistic = 0.83).
The performance of the imputed inadequate health literacy (i-IL) as a proxy for the S-TOHFLA-based “gold-standard” indicator (IL) to quantify associations with various measures of health status is shown in Table 3. Test-based IL was associated with poorer health for all eight health-status measures, although in one case (hypertension) it was not statistically significant at the 5% level. For each of the six dichotomous and two continuous measures of health, the 95% confidence intervals for the i-IL and IL associations in the Prudential Study overlap each other. Furthermore, for the four dichotomous outcomes that are also available in NHIS, the 95% confidence interval for the i-IL association in NHIS overlaps each of the other two confidence intervals. Several point estimates are quite similar in all three situations, for example, estimated odds ratios (ORs) for self-reported poor/fair general health were 1.77 for IL and 1.78 for i-IL in the Prudential Medicare Study, and 1.70 in NHIS. In one instance (diabetes), however, the estimated ORs varied substantially (being 1.37, 1.08, and 1.29, respectively), with the association of i-IL in the Prudential study being not significant, while the other two are significant at the 5% level. The only other large difference was observed for the Mental SF-12, where the effect estimates for inadequate literacy were -2.46 when measured using IL versus -1.27 when using i-IL in the Prudential Medicare Study. This difference may be large enough to be meaningful, although even here, the confidence intervals overlap.
Table 3.
Association of Inadequate Literacy With Self-reported Health and Chronic Conditions
| Prudential Study Sample, N = 2,824 | NHIS 1997, N = 6,819 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| S-TOFHLA-based inadequate health literacy | DAHL inadequate health literacy | DAHL inadequate health literacy | |||||||
| 95% CI | 95% CI | 95% CI | |||||||
| OR | Low | High | OR | Low | High | OR | Low | High | |
| Dichotomous outcome measures | |||||||||
| Poor/fair general health | 1.77 | 1.42 | 2.21 | 1.78 | 1.45 | 2.19 | 1.70 | 1.49 | 1.94 |
| Hypertension | 1.08 | 0.88 | 1.33 | 1.15 | 0.96 | 1.39 | 1.07 | 0.95 | 1.21 |
| Diabetes | 1.37 | 1.04 | 1.81 | 1.08 | 0.83 | 1.40 | 1.29 | 1.08 | 1.54 |
| Difficulty with ADL | 1.91 | 1.17 | 3.13 | 2.57 | 1.62 | 4.08 | 2.47 | 1.91 | 3.19 |
| Difficulty with IADL | 1.77 | 1.41 | 2.22 | 1.52 | 1.25 | 1.86 | NA | ||
| Flu vaccination, never | 1.31 | 1.03 | 1.67 | 1.42 | 1.14 | 1.77 | NA | ||
| 95% CI | 95% CI | 95% CI | |||||||
| Coefficient | Low | High | Coefficient | Low | High | Coefficient | Low | High | |
| Continuous outcome measures | |||||||||
| Physical SF12 | -1.70 | -2.78 | -0.63 | -2.34 | -3.34 | -1.33 | NA | ||
| Mental SF12 | -2.46 | -3.31 | -1.62 | -1.27 | -2.05 | -0.49 | NA | ||
NA = Not available in NHIS
These results are based on using a threshold that categorizes 25 percent of the population as having inadequate literacy; in Figure 1 we illustrate the corresponding estimates for a range of threshold scores. For all the measures except “difficulty with an ADL” we found considerable stability in the OR estimates associated with S-TOFHLA-based inadequate literacy across the entire spectrum of threshold choice from 50 to 87. This stability was matched well by the estimate based on the DAHL across most of the spectrum – except at the lowest threshold scores, possibly due to small numbers (only 14% of the Prudential study has i-IL <55). A similar pattern was found for the corresponding associations in the NHIS (1997) sample – here based only on the imputed inadequate literacy indicator (Fig. 2).
Figure 1.
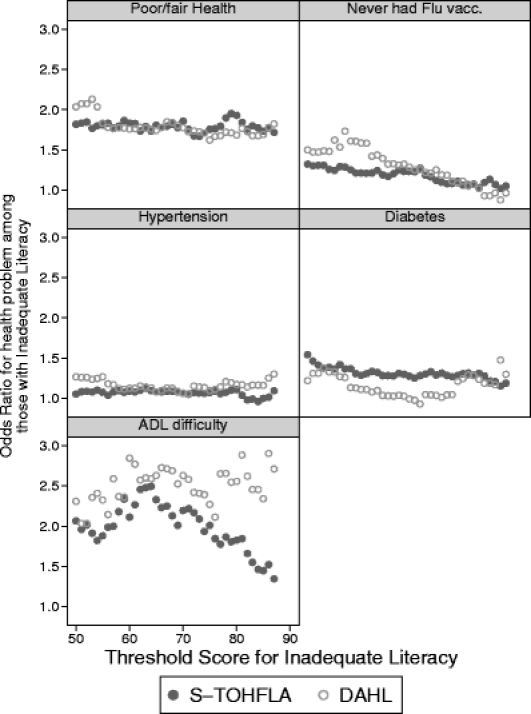
Association of self-reported health with inadequate literacy based on S-TOHFLA and DAHL Prudential Study 1997 (N = 2,824). Note: Each point corresponding to a threshold score denotes the effect associated with S-TOHFLA-based or DAHL-based inadequate literacy from a separate logistic regression.
Figure 2.
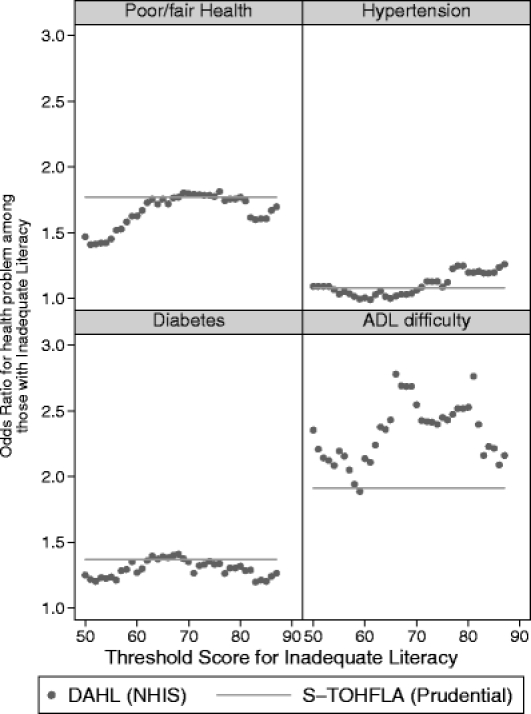
Association of self-reported Health with inadequate literacy based on DAHL – NHIS elderly 1997 (N = 6,819). Note: Each point corresponding to a threshold score denotes the effect associated with DAHL-based inadequate literacy from a separate logistic regression. The NHIS estimate based on imputed (DAHL) inadequate literacy is compared with the S-TOFHLA-based estimate from Prudential study using the 25 percentile threshold score of 53.
While the Prudential Medicare Study sample includes only HMO enrollees, the NHIS sample includes both HMO and Fee-for-Service enrollees. Comparing these two cohorts in the NHIS sample, we found that while the HMO enrollees were more likely to be younger, better educated, and have higher income, these differences were small, and the derived rates of inadequate literacy were not statistically significant.
DISCUSSION
This study examines the performance of an imputed measure of inadequate health literacy among elderly subjects as a proxy for test-based measures commonly used in the literature. We used the S-TOHFLA-based measure of health literacy in the Prudential Medicare Study to develop scoring weights for a parsimonious model that includes four widely available demographic indicators – sex, age, years of schooling, and race/ethnicity. Using these weights we evaluated the performance of the imputed literacy measure, the DAHL, to estimate the association with a variety of health status measures obtained in the Prudential Medicare Study (1997) as well as the elderly in the 1997 and 2005 rounds of the National Health Interview Survey (NHIS). For most of the eight health measures examined, we found similar estimates of the influence of inadequate health literacy using the imputed and test-based measures. Similarity in the estimates for the Prudential Medicare Study and NHIS is noteworthy because, while the two samples are rather similar, they differ significantly in some characteristics – for example, the NHIS elderly sample is older and less poor than the Prudential study sample.
Overall, the results support using the DAHL as a proxy for a test-based determination of inadequate health literacy in models to predict health outcomes. First, the DAHL can capture most of those who would be classified by the S-TOFHLA as having inadequate literacy. Second, even though about 20% of the sample is classified differently by the two measures, the similar magnitude and direction of associations between various health outcomes and inadequate literacy defined either way point to the underlying robustness of these associations.
The basis for the DAHL is the strong association between test-based health literacy (S-TOFHLA) and the four socioeconomic status (SES) indicators – years of schooling, age, sex, and race/ethnicity. This association is not surprising – some of these factors are causal (years of schooling, age), while others are important mediators (age, race/ethnicity, and sex). Indeed, while variation in the DAHL is dictated completely by differences in these four SES indicators, the S-TOFHLA score is obviously affected by other factors. Our findings indicate that these four SES factors capture most of the variation in S-TOFHLA, while avoiding the need for difficult to measure covariates, such as “difficulty in reading forms” that would limit a proxy measure’s range of applicability.
An important implication of our sensitivity analyses is that the relationship between literacy and health outcomes appears quite stable across the range of scores. For most of the health measures examined, the odds ratio of reporting a health problem seems to be stable for much of the spectrum of both the test-based as well as imputed literacy scores. In other words, for the outcomes measured, there appear to be no particular threshold scores that identify particularly vulnerable population subgroups. Instead, the relationship appears to be linear, with potential health benefit from improved health literacy at all “levels” of literacy.
The DAHL is parsimonious in its specification compared to the imputed measure in Miller et al.12, even though both used the same underlying socio-demographic indicators. While the measure in Miller et al. allowed for interaction of schooling with age, Black race, and Hispanic ethnicity, the DAHL involves no interaction terms. Nevertheless, there is no loss in its discriminatory power in identifying those with inadequate health literacy, as measured by the S-TOFHLA.
Several limitations should be noted. First, the present study is limited to self-reported general health status. Analyses of other health measures should be conducted. Of the eight measures available in the Prudential Medicare Study, only four could be compared in the NHIS. Second, for health status indicators with low prevalence (such as the 3.3% prevalence for difficulty with ADL), estimates based on the imputed measure may not be stable. Future research should further evaluate this hypothesis and possibly identify a prevalence threshold that could be used as a guide for conducting analyses using the DAHL. Third, the sampling framework of the Prudential Medicare Study restricted the range of potentially important demographic characteristics that could be included in an imputed measure. For example, it is possible that including a variable for being born outside the US would improve the predictive capacity of the DAHL; however, since this variable was not collected in the Prudential Medicare Study, it could not be evaluated. There are other differences between the Prudential Medicare Study and the NHIS. First, the Prudential sample includes only Medicare HMO enrollees, while the NHIS (and other national surveys) includes both HMO and Fee-for-Service enrollees. Second, the Prudential sample includes new enrollees during an 8-month period ending August 1997; the NHIS represents the Medicare population throughout 1997. Finally, the ADL measure differs slightly across the two surveys.
To date, direct measures of health literacy require in-person evaluation, which is not done in most national health surveys. Our findings suggest that the DAHL may serve as a good proxy for estimating associations in national surveys where test-based health literacy measures are absent. Compared to the limited size and scope of the existing surveys with test-based health literacy measures, readily available national surveys, such as Medical Expenditure Panel Survey (MEPS) and Behavioral Risk Factor Surveillance System (BRFSS), offer considerably richer settings for evaluating associations of inadequate health literacy with hitherto unexamined health outcomes and utilization. These larger surveys enable examination of less common health outcomes and utilization (including, heart attacks and cardiac revascularization). In addition, longitudinal analyses on health literacy have been rare to date due to the limited availability of relevant data. Several available data sets provide the immediate opportunity to examine longitudinal hypotheses with the DAHL. Indeed, a broad range of new health literacy research questions can now be studied.
Acknowledgements
The findings of this study were presented at the 2007 Annual Meetings of both the Society of General Internal Medicine (April 25–28, Toronto) and the AcademyHealth (June 3–5, Orlando, FL).
Potential conflicts of interest None disclosed.
References
- 1.Nielsen-Bohlman L, Panzer A, Hamlin B, Kindig D. (National Academies Press). Health literacy: a prescription to end confusion. 2004. [PubMed]
- 2.Kutner M, Greenberg E, Jin Y, Paulsen C. (US Department of Education, National Center for Education Statistics). The health literacy of america's adults: results from the 2003 national assessment of adult literacy. 2006.
- 3.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. A systematic review of the literature. J Gen Intern Med.. 2004;19(12):1228–1239. [DOI] [PMC free article] [PubMed]
- 4.Sudore RL, Yaffe K, Satterfield S, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006;21(8):806–812. [DOI] [PMC free article] [PubMed]
- 5.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20(2):175–184. [DOI] [PMC free article] [PubMed]
- 6.Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92(8):1278–83. [DOI] [PMC free article] [PubMed]
- 7.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–5. [PubMed]
- 8.DeWalt DA, Pignone MP. Reading is fundamental: The relationship between literacy and health. Arch Intern Med. 2005;165(17):1943–1944. [DOI] [PubMed]
- 9.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–41. [DOI] [PubMed]
- 10.Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281(6):545–551. [DOI] [PubMed]
- 11.Paasche-Orlow M, Hanchate A. Modeling literacy with sociodemographic characteristics and literacy activities. J Gen Intern Med. 2005;21(S4):88.
- 12.Miller MJ, Degenholtz HB, Gazmararian JA, Lin CJ, Ricci EM, Sereika SM. Identifying elderly at greatest risk of inadequate health literacy: A predictive model for population-health decision makers. Res Social Adm Pharm. 2007;3(1):70–85. [DOI] [PubMed]
- 13.The American Association for Public Opinion Research. (AAPOR). Standard definitions: final dispositions of case codes and outcome rates for surveys, 4th edition. 2006.
- 14.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40(5):395–404. [DOI] [PubMed]
- 15.Howard DH, Sentell T, Gazmararian JA. Impact of health literacy on socioeconomic and racial differences in health in an elderly population. J Gen Intern Med. 2006;21(8):857–861. [DOI] [PMC free article] [PubMed]
- 16.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21(12):1215–1221. [DOI] [PMC free article] [PubMed]
- 17.Baker DW, Gazmararian JA, Williams MV, et al. Health literacy and use of outpatient physician services by Medicare managed care enrollees. J Gen Intern Med. 2004;19(3):215–220. [DOI] [PMC free article] [PubMed]
- 18.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165(17):1946–52. [DOI] [PubMed]
- 19.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40(5):395–404. [DOI] [PubMed]
- 20.Ware J. The MOS 36-item short-form health survey (SF-36). In: Sederer L, Dickey B, eds. Outcomes assessment in clinical practice. Baltimore, MD: Williams & Wilkins; 1996:61–64.
- 21.U. S. Department of Health and Human Services. NATIONAL HEALTH INTERVIEW SURVEY, 1997 [Computer file] 2nd ICPSR version. Hyattsville, MD: US Dept. of Health and Human Services, National Center for Health Statistics [producer], 1996. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2001.
- 22.Brindle P, Emberson J, Lampe F, et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ. 2003;327(7426):1267. [DOI] [PMC free article] [PubMed]
- 23.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. [DOI] [PubMed]
- 24.StataCorp. Stata Statistical Software: Release 9 College Stataion, TX: StataCorp LP; 2005.


